Abstract
Introduction
Incisional hernias to the subxiphoid region are rare and anatomically challenging, with bony and cartilaginous structures attaching, as well as conflating abdominal fascia. The repair of hernias in this region is, therefore, difficult and prone to recurrence. The surgical treatment can be done by open or laparoscopic repair but very little is known about which method is superior. We, therefore, reviewed our data of patients undergoing repair of subxiphoid hernias.
Methods
Between January 2010 and June 2015 twenty-eight patients were treated by laparoscopic (n = 8) or open (n = 20) hernia repair due to an incisional hernia in the subxiphoid region. Patients with ventral hernias with an origin more distal than the M1-area only extending into the subxiphoid region and those undergoing suture hernia repair were excluded.
Results
The hernia sizes, in terms of length, width and EHS classification, did not vary between open and laparoscopic repair. The duration of laparoscopic surgery was significantly shorter than the mean operative time for an open subxiphoid hernia repair (168.1 min vs. 96.1 min, respectively; p = 0.012). The groups did not differ significantly in terms of overall postoperative complications (p = 0.568) but the grade (Clavien–Dindo) of complications was higher following open repair leading to three reoperations. Within the follow-up time, we diagnosed significantly (p = 0.031) more subxiphoid hernia recurrences after laparoscopic repair (37.5%, n = 3) than after open repair (0%).
Conclusion
Laparoscopic and open repair of subxiphoid incisional hernias are both technically challenging compared to other midline hernias. Referring to our results laparoscopic repair has shorter operative times, lower postoperative morbidity with a higher recurrence rate compared to open repair but the sample size is too small for an overall conclusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subxiphoid incisional hernias are uncommon midline hernias with a fascial defect in the epigastric region directly caudal to the xiphoid process. According to the classification of primary and incisional abdominal wall hernias by Muysoms et al. subxiphoidal incisional hernias are classified as M1 [1]. Incisional hernias to this region may occur as a proximal defect of large abdominal midline laparotomies extended to the xiphoid process or after median sternotomy. The reported incidence of subxiphoid incisional hernias after median sternotomy ranges up to 4.2% [2,3,4]. However, some authors assume that the true incidence might be higher because most hernias are small and asymptomatic due to the prevention of intestinal incarceration by the underlying liver [4, 5].
The subxiphoid area is anatomically a complex region with bony and cartilaginous structures attaching as well as conflating abdominal fascia. The repair of hernias in this region is, therefore, difficult and prone to recurrence. Results of conventional hernia repair with primary midline approximation of the fascia are poor with reported recurrence rates up to 80% [6, 7]. The implementation of meshes has, therefore, become the standard procedure with lower recurrence rates from 0 to 32% [3, 6,7,8,9]. Laparoscopic repair with the usage of a composite mesh offers a feasible alternative to open repair [3, 10].
Despite these facts, it is still difficult to decide how to manage these hernias, mainly due to a small number of reported series with a retrospective nature, a very heterogeneous population and the lack of long-term data regarding recurrence rates.
We, therefore, reviewed our Management and data of the surgical repair of subxiphoidal incisional hernias with a special focus on the long-term success of the treatment.
Patients and methods
Patients and methods
Between January 2010 and June 2015 a total of 864 ventral incisional hernias underwent operative treatment in our surgical department. 85 (9.8%) of the patients were identified from our database with a subxiphoid incisional hernia (M1). Fifty five of these patients were excluded due to ventral hernias with an origin more distal than the M1-area only extending into the subxiphoid region. Patients undergoing suture repair were also excluded from the analysis (n = 2). A total of 28 patients were included in the analysis with 20 patients (71.4%) that underwent open repair and eight patients (28.6%) after laparoscopic repair. Hernias were mainly diagnosed by a primary general physician and referred to our outpatient clinic, were we confirmed the diagnosis by physical and sonography examination or computed tomography (Fig. 1). All patients showed a subxiphoid bulging (Fig. 2) mainly with complaints, but no patient presented with signs of incarceration.
Principles of surgical treatment and perioperative management
The surgical treatment of subxiphoid hernia repair, whether open or laparoscopic, followed basic principles of modern hernia repair. The main principle is a mesh augmentation of the hernia defect, and therefore, the creation of a mesh-tissue compound to prevent a hernia recurrence [5]. These general fundamentals also emphasize a tension-free repair with a well fixed mesh and an adequate overlap of the mesh of at least 5 cm in all directions [4, 5].
All patients undergoing open or laparoscopic repair of a subxiphoid hernia received a single-shot of intravenous cephalosporin and metronidazole shortly before the time of incision. An abdominal binder was fitted to all patients at the end of the operation and patients were strongly recommended to carry the binder for 4–6 weeks postoperatively.
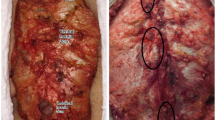
Open repair
Open repair started by proceeding through the old incision and dissection of the hernia sac. To achieve an adequate cranial overlap for a mesh augmentation in the retromuscular (sublay) layer the posterior lamina of the rectus sheath had to be completely detached from the costal arch. Following this, a retroxiphoid space between the peritoneum and the diaphragm was created by blunt dissection of the fatty tissue that reaches 5 cm or more behind the xiphoid process (Fig. 3). In patients who underwent a primary median sternotomy, cardiac surgery care was applied to possible adhesions of the heart to the scar to limit the risk of myocardial injury. After achieving an adequate hernia overlap of at least 5 cm around all edges, the peritoneum and the posterior rectus sheath were closed with a running suture (PDS, Ethicon; USA) and a lightweight mesh was cut to size. We chose an Ultrapro mesh (Ethicon; USA) in 14 patients, a Vypro mesh (Ethicon; USA) in 4 cases and in two patients an Optilene mesh (B.Braun; Germany) was used. Mesh fixation was performed along all edges with interrupted sutures (Vicryl, Ethicon; USA). When using wound drainages, redon’s suction drainages were inserted above the mesh, usually subcutaneously. The anterior rectus sheath was also closed with a running suture (PDS, Ethicon; USA).
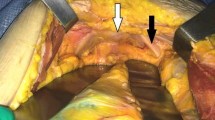
Laparoscopic repair
The main principles of laparoscopic repair of subxiphoid hernia are based on the guidelines for laparoscopic ventral and incisional hernia repair [11]. In all patients undergoing laparoscopic repair, the pneumoperitoneum was established using a Veress needle or by mini Laparotomy in the left upper quadrant. After complete adhesiolysis and dissection of the hernia content, one of the major steps was to completely take down the falciform ligament. In this way, the mesh position can cranially extend up to the hepatic veins and the esophagus to assure an adequate overlap. The hernia defect was not primarily closed by sutures. After introducing and unfolding the mesh, intraabdominally anchoring sutures were placed to fix the mesh parallel to the abdominal wall. We used a Composite Mesh in all patients (Parietex composite, Medtronic; USA). Endoscopic tacks (AbsorbaTack, Medtronic; USA) were placed in a double-crown around the hernia defect and the edges of the mesh wherever positioning was safe. Whenever a positioning of endoscopic tacks was unsafe we did not rely on the non-fixation but rather used a combination of fibrin glue in the far cranial region and tacks as far as possible for mesh fixation. In all cases, it was at least possible to complete the inner crown around the hernia defect with endoscopic tacks.
Follow-up and statistical analysis
During December 2016, a questionnaire on suspicion of hernia recurrence based on the patient-reported outcomes by Baucom et al. was sent to all included patients [12]. This ventral hernia recurrence inventory is a simple patient-reported outcome measurement to determine hernia recurrence. Main contents are two questions regarding the patient´s hernia operation: “Do you feel or see a bulge?” and “Do you have physical symptoms or pain at the site”. Non-responders were contacted by a surgeon by phone calls up to three times. If there was still no response, patients were classified as lost to follow-up. Participants reporting a new bulge at the hernia site or with suspicion of a hernia recurrence were invited to our outpatient clinic for a clinical examination. All examinations were performed by two experienced surgeons and inconclusive clinical findings were completed with a dynamic abdominal sonography or a CT scan.
Statistical analysis was performed using SPSS Version 22 (IBM, USA). To compare the open and laparoscopic approach, the Chi-square test was used for categorical analysis and the Student´s t-test or a single factor variance analyses for continuous data. The significance was defined as p value of lower than 0.05.
Results
Twenty-eight patients had undergone surgical repair of a subxiphoid hernia between January 2010 and June 2015. Twenty of these patients (71.4%) were treated with an open approach and a retromuscular mesh repair and 8 patients received a laparoscopic IPOM repair. Patients’ gender, age and body-mass-index (BMI) did not differ significantly between the two treatment-groups. The mean length of hospital stay was longer after open repair (11.5 vs. 7.0, respectively) but without reaching statistical significance (p = 0.464). Both groups included patients with thoracic and abdominal previous operations as (Table 1).
As shown in Table 2 the hernia sizes in terms of length, width and EHS classification did not vary in their treatment by open or laparoscopic repair. All patients were treated by a planned elective operation. The mean duration of laparoscopic surgery was significantly more than 1 h shorter than the mean operative time for an open subxiphoid hernia repair (168.1 min vs. 96.1 min, respectively; p = 0.012). In 95.0% of the open operations (n = 19) a wound-drainage mechanism was used as compared to none after laparoscopic repair (p < 0.001). The groups did not differ significantly in terms of overall postoperative complications (p = 0.568) but patients following open hernia repair more often developed severe complications (≥ Grade III) according to the classification of Clavien and Dindo (p = 0.223). Following open repair postoperative morbidity included a prolonged wound drain due to high amounts of fluid secretion and three patients with bleeding complications. After laparoscopic repair one patient showed gastrointestinal symptoms with nausea and vomiting and another patient developed a minor surgical side infection at one of the trocar sites. Three patients (15.0%) of the open group needed a reoperation and none after laparoscopic repair. In one case the bleeding was subcutaneous with a consecutive surgical side infection and in the second case the patient developed a bleeding from the muscle with an insufficiency of the closure of the anterior fascia diagnosed by ultrasound. These reoperations were performed on postoperative day 5 and 6. One patients showed an acute bleeding from the muscle layer at the drain insertion site and needed a reoperation within the first postoperative night. This patient also developed an acute on chronic renal failure. All three patients undergoing reoperations were preoperatively classified as ASA III and all under antiplatelet therapy (Asperin 100 mg).
The median follow-up time after open repair was 48.8 months (8–76 months) and 32.5 months (4–68 months) after laparoscopic repair (p = 0.123) as shown in Table 3. 40% of the patients after open repair were lost to follow-up, 12.5% after laparoscopic repair. Four patients (n = 3 open; n = 1 laparoscopic) died within the follow-up time as reason for lost to follow-up. Within the follow-up time, we diagnosed significantly (p = 0.031) more subxiphoid hernia recurrences after laparoscopic repair (42.9%, n = 3) than after open repair (0%).
Discussion
Incisional hernias to the subxiphoid region are rare and the repair of these hernias is a surgical challenge mainly due to the complexity of the anatomic region. We, therefore, reviewed our experiences and results with the open and laparoscopic repair of isolated subxiphoid hernias.
Laparoscopic and open repair are both feasible treatment options for subxiphoid hernias. The laparoscopic repair offers the advantage of shorter operative times and a tendency to lower postoperative morbidity compared to the open hernia repair. In our case, the operative time of laparoscopic repair was almost an hour shorter than the open repair. One of the main reasons for the shorter operative time of laparoscopic repair is an excellent visualization of the hernia defect and an easier anatomic preparation of the hernia site. Besides these facts, the previous incision can be avoided and the tissue trauma is minimal [10]. In our opinion, the only crucial technical point during the laparoscopic repair is the mesh fixation to the cranial side. It is necessary to completely dissect the falciform ligament down to the hepatic veins for an adequate overlap to the cranial side. With the diaphragm on the cranioventral side of the mesh, tack fixation might penetrate and injure vital thoracic structures and should, therefore, be avoided on this side of the mesh. Some authors describe a non-fixation of the cranial mesh overlap with the idea of the intraabdominal pressure exerted by the liver and the stomach fixing the prosthesis after desufflating the pneumoperitoneum [3, 4, 7]. Others report a fixation using a combination of tacks and transfascial or intracorporeal nonabsorbable sutures [9, 10]. Whenever possible we preferred creating a fixation with endoscopic tacks while being cautious of the diaphram. For the eight patients we treated laparoscopically we did not rely on the method of non-fixation to the cranial side, and therefore, used fibrin glue for an additional fixation of the mesh to the diaphragm. But in conclusion, this technical problem remains the unsolved weak spot of laparoscopic repair of subxiphoid hernias.
For open hernia repair Conze et al. accurately described the preparation of the retroxiphoid space and the opening of the “fatty triangle” in their anatomic study: By transecting the posterior rectus sheath from the costal margins the retroxiphoid space can be entered [5]. Blunt dissection of the fatty tissue directly behind the xiphoid process creates an open space without injuring the peritoneum to achieve a wide cranial overlap of the hernia defect (Fig. 3). This large tissue trauma might be one of the reasons for the higher postoperative morbidity following open hernia repair in our study. Even though the difference of postoperative morbidity between the two operative groups did not achieve statistical significance, it cannot be left unmentioned that patients in this study after open repair had more severe complications according to the grading of Clavien and Dindo. Three of these patients also required a reoperation all due to bleeding complications. In one of these cases an acute bleeding was probably caused by the inserted drain and led to a reoperation within the first postoperative night. Drains were placed in 19 of 20 open hernia repairs (95%) and none after laparoscopic repair. In both other cases undergoing a reoperation the bleeding was not indicated by the drain. Drains were mainly removed within the first two postoperative days, only in one patient prolonged fluid secretion required a therapy by leaving the drainage for 7 days. According to a recent Cochrane review there is not enough evidence to make a final decision whether wound drains after incisional hernia repair are associated with improved or even worse outcomes [13]. But also due to our present results, we are a lot more reserved in terms of using wound drains after open hernia repair or at least pay more attention to bleeding from the inserted site.
Initial descriptions of subxiphoid hernia repair using a suture closure by bringing together the retracted fascial margins reported a high recurrence rate of up to 80% [6, 7]. With the usage of a permanent mesh the recurrence rates after open hernia repair have been reported to be around 30% [6, 7, 14] and after laparoscopic repair to be between 10 and 30% [3, 7, 10]. We found an overall recurrence rate of 15.8% after a median follow-up time of 3.8 years (46.2 months). Even though the laparoscopic hernia repair has a significantly higher recurrence rate in our study these results should be viewed with caution. The sample size is obviously not large enough to achieve an adequate statistical power as shown in the exemplary power calculation at the appendix of Table 3. Furthermore, our recurrence rate after open repair could be underestimated due to the higher rate of lost to follow-up. We are, therefore, not able to make a reliable conclusion regarding the comparison of recurrence rates after laparoscopic and open repair of subxiphoid hernias.
The small sample size and the retrospective design are obviously the main limitation to the present study. But as subxiphoid hernias are rare this makes prospective or even randomized controlled trials challenging. More observational studies or registry data evaluation with larger sample sizes are, therefore, desirable.
References
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Hidalgo Pascual M, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RK, Simons MP, Smietanski M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414. https://doi.org/10.1007/s10029-009-0518-x
Davidson BR, Bailey JS (1986) Incisional herniae following median sternotomy incisions: their incidence and aetiology. Br J Surg 73(12):995–996
Landau O, Raziel A, Matz A, Kyzer S, Haruzi I (2001) Laparoscopic repair of poststernotomy subxiphoid epigastric hernia. Surg Endosc 15(11):1313–1314. https://doi.org/10.1007/s004640090011
Losanoff JE, Basson MD, Laker S, Weiner M, Webber JD, Gruber SA (2007) Subxiphoid incisional hernias after median sternotomy. Hernia 11(6):473–479. https://doi.org/10.1007/s10029-007-0258-8
Conze J, Prescher A, Kisielinski K, Klinge U, Schumpelick V (2005) Technical consideration for subxiphoidal incisional hernia repair. Hernia 9(1):84–87. https://doi.org/10.1007/s10029-004-0239-0
Cohen MJ, Starling JR (1985) Repair of subxiphoid incisional hernias with Marlex mesh after median sternotomy. Arch Surg 120(11):1270–1271
Mackey RA, Brody FJ, Berber E, Chand B, Henderson JM (2005) Subxiphoid incisional hernias after median sternotomy. J Am Coll Surg 201(1):71–76. https://doi.org/10.1016/j.jamcollsurg.2005.01.025
de Mesquita GHA, Iuamoto LR, Suguita FY, Essu FF, Oliveira LT, Torsani MB, Meyer A, Andraus W (2017) Simple technique of subxiphoid hernia correction carries a low rate of early recurrence: a retrospective study. BMC Surg 17(1):51. https://doi.org/10.1186/s12893-017-0249-3
Ghanem OM, Zahiri HR, Devlin S, Sibia U, Park A, Belyansky I (2016) Laparoscopic subxiphoid hernia repair with intracorporeal suturing of mesh to the diaphragm as a means to decrease recurrence. J Laparoendosc Adv Surg Tech A 26(2):129–132. https://doi.org/10.1089/lap.2015.0518
Eisenberg D, Popescu WM, Duffy AJ, Bell RL (2008) Laparoscopic treatment of subxiphoid incisional hernias in cardiac transplant patients. JSLS 12(3):262–266
Silecchia G, Campanile FC, Sanchez L, Ceccarelli G, Antinori A, Ansaloni L, Olmi S, Ferrari GC, Cuccurullo D, Baccari P, Agresta F, Vettoretto N, Piccoli M (2015) Erratum to: laparoscopic ventral/incisional hernia repair: updated consensus development conference based guidelines. Surg Endosc 29(9):2485. https://doi.org/10.1007/s00464-015-4470-9
Baucom RB, Ousley J, Feurer ID, Beveridge GB, Pierce RA, Holzman MD, Sharp KW, Poulose BK (2016) Patient reported outcomes after incisional hernia repair-establishing the ventral hernia recurrence inventory. Am J Surg 212(1):81–88. https://doi.org/10.1016/j.amjsurg.2015.06.007
Gurusamy KS, Allen VB (2013) Wound drains after incisional hernia repair. Cochrane Database Syst Rev 12:CD005570. https://doi.org/10.1002/14651858.CD005570.pub4
Davidson BR, Bailey JS (1987) Repair of incisional hernia after median sternotomy. Thorax 42(7):549–550
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that no conflict of interest exists.
Ethical approval
Ethical approval from the institutional review board was not required for this study.
Human and animal rights
As a retrospective review, no experimental conditions were implemented. All human participants received standard of care treatments and; thus, no rights were violated. No animals were involved in this study.
Informed consent
As a retrospective review, formal consent was not required.
Rights and permissions
About this article
Cite this article
Raakow, J., Schulte-Mäter, J., Callister, Y. et al. A comparison of laparoscopic and open repair of subxiphoid incisional hernias. Hernia 22, 1083–1088 (2018). https://doi.org/10.1007/s10029-018-1815-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-018-1815-z