Abstract
Background
Subxiphoid incisional hernias are notoriously difficult to repair and are prone to recurrence. The few reports on subxiphoid hernia published over the last two decades have not fully addressed the etiology, pathology, treatment, and outcome of this problem. This review was performed to analyze the published experience and increase the understanding of these difficult hernias.
Methods
We reviewed the extensive literature, including the Medline and Current Contents computerized database searches, and searched the available bibliographies.
Results
Seven retrospective studies of a total of 113 patients who had clinical subxiphoid hernias after median sternotomy were found. An additional surgical technique describing a modified median sternotomy preventing the hernia, and a single review article on selected technical considerations of subxiphoid ventral repair were also found.
Conclusions
The incidence of subxiphoid hernia after median sternotomy can be possibly reduced by paraxiphoid extension of the sternotomy, reinforcement near the xiphoid end of the incision, or by optimizing closure of the distal sternotomy and the linea alba. Abdominal wall reinforcement by open-mesh closure or laparoscopic transperitoneal prosthetic repair can effectively deal with the defect. Long-term outcome analyses are not yet available.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subxiphoid incisional hernias after median sternotomy typically occur in the epigastrium, where the incision extends into the abdomen. They are notoriously difficult to repair and are prone to recurrence. Although their reported incidence is between 1% and 4.2% [1–9], their true incidence is difficult to estimate for at least two reasons. First, most subxiphoid hernias are small and asymptomatic. Thus, many patients do not seek medical attention. Second, long-term follow-up of a large group of patients with median sternotomies sufficient to make this assessment has not been described [8]. A recently published study from the Cleveland Clinic reported 117 repaired hernias among 24,000 patients who underwent median sternotomy (0.5%). However, the authors could not calculate the true incidence because of the significant number of national and international referrals in the patient population studied [9].
The few reports on subxiphoid hernia published over the last two decades have not fully addressed the etiology, pathology, treatment, and outcome of this problem. This review was performed to analyze the published experience and increase the understanding of these difficult hernias.
Review of the literature
The data reported herein are based on a literature review including the Medline and Current Contents computerized database searches. The following subject headings were searched and combined into search sets: sternum, hernia, anatomy, surgical wound dehiscence, and wound healing. Search sets of the following key words were used in addition to the subject heading terms: sternum, median sternotomy, hernia, subxiphoid hernia, subxiphoid space, anatomy, sternotomy closure, surgical wound dehiscence, xiphoid process, and wound closure. All variant combinations of subject headings and key words were checked. Finally, the existing bibliographies were explored for articles pertaining to the review.
The search of the literature and available bibliography revealed seven retrospective studies of a total of 113 patients who had clinical subxiphoid hernias after median sternotomy [1–3, 5–7, 9]. An additional surgical technique describing a modified median sternotomy in 2,500 patients very briefly reported a zero incidence of this hernia [4]. We were able to locate a single review article on the technical considerations of subxiphoid ventral repairs [8]. Of interest, the first of all xiphoid hernia series [1] was published 88 years after the first known description of median sternotomy [12], and 28 years after the incision was popularized as a contemporary approach to the heart and great vessels [13].
The clinical series of subxiphoid hernia are summarized in Table 1. Two articles focused on different aspects of the presentation and treatment of the same 20 patients [2, 3]. Overall, many of the demographic and technical details were not uniformly reported among the studies. Collectively, the majority of patients were male and their age ranged between 30 and 86 years. All patients had undergone median sternotomy extended to the midline epigastric area. The diameter of the defects identified varied from 2 cm to 15 cm. Between 35% and 100% of the hernias were symptomatic [1, 2]. Only one group provided details of their sternal closure method, which did not include suture of the xiphoid process [1]. Two studies reported that the linea alba was closed with absorbable material [1, 2]. Only two studies included patients with previously repaired hernias [1, 5]. Finally, only two studies reported on the postoperative time of detection, ranging from 3 days to 7 years [1], with a peak at 3–4 years [9].
Discussion
Surgical anatomy of the subxiphoid region
The borders of the subxiphoid space are created by the sternum and ribs superiorly, the rectus abdominis muscles and linea alba anteriorly, and the diaphragm posteriorly and inferiorly. The region’s musculofascial structures are all anchored to the upper, osseous, or cartilaginous border, in the angle of which the xiphoid process emerges as a quite variable structure. Its multiple anatomic variants can be grouped into three main categories based upon the shape of the xiphoid. The xiphoid process may be categorized as small, long, or broad [8]. The rectus muscles and anterior rectus sheaths wrap up the front of the xiphoid region; the diaphragm, posterior rectus sheaths, and linea alba attach to the sternum and xiphoid process, thus, forming the boundary of the abdominal cavity.
The xiphoid process is incompletely ossified and is composed of cartilage in the majority of patients. It is firmly attached to four structures in the region: (1) the linea alba attaches to its anterior aspect; (2) the costoxiphoid ligament attaches its ventral and dorsal aspects to the 7th costal cartilages; (3) the transverse muscles of the thorax attach it to the 6th rib; and (4) the sternal portion of the diaphragm attaches to its posterior surface [1]. The arterial blood supply of the xiphoid process is limited when compared with that of the proximal sternum. In 61.3% of patients, blood is supplied by the so-called xiphoid artery, a terminal branch of the internal thoracic artery. This artery is found on the right side in 30.7%, on the left in 21%, and is bilateral in 9.7% of patients [14]. If the xiphoid artery is not present, the area is supplied by branches of the superior epigastric artery. Collateral blood supply to the area may be compromised if the internal thoracic or superior epigastric arteries are damaged or used as conduits in bypass procedures [14].
The preperitoneal space extends in a cranial direction behind the xiphoid process and forms the so-called retroxiphoid space, which is filled with fatty tissue. The sternal portion of the diaphragm, which is easily detachable by blunt-finger dissection, separates the retroxiphoid space and the lower anterior mediastinum, which also contains fatty tissue. The above-described relationship suggests how blunt-finger dissection behind the sternum can create a pocket which extends as far as the surgeon’s index finger can reach. It must be noted that, in the majority of patients undergoing heart surgery, the myocardium is adherent to the posterior sternum. This limits the extent of blunt dissection because of a significant risk of myocardial injury.
Biomechanical considerations
The true etiology and pathogenesis of subxiphoid hernia after median sternotomy has not been fully elucidated. Both patient-related factors, such as impaired collagen metabolism, obesity, and older age, and technical factors, such as wound infection, absorbable suture material, and inadequate incisions and closures, may contribute to the genesis of this problem [15]. Recent studies of sternal biomechanics after median sternotomy suggest that the closure may start to fail at or near the xiphoid end of the incision in association with lateral traction forces caused by breathing or coughing [16, 10]. This suggests that separation of the lower sternum and xiphoid process may contribute to the hernia’s etiology.
The linea alba is an area across which the tendinous aponeurotic fibers of the flat abdominal muscles (external, internal, and transverse) pass from one side to the other. This triple pattern crossing (also described using the term “decussation” [16]) is thought to specifically provide additional strength to the midline aponeurosis. Herniation has been described more frequently when only one layer (as opposed to three) of decussating fibers is present [11]. The aponeurotic fibers are oriented in oblique planes, forming a dynamic fabric that allows the fibers’ configuration to change in response to movement of the trunk. This is exemplified by the absence of folds in the linea alba during flexion of the trunk while folds do occur in the skin, and the above-described adaptive function of the aponeurosis is lost as a result of post-surgical scarring [11].
During respiration and coughing, the abdominal muscles, fibers of the linea alba, costoxiphoid ligaments, transverse thoracic muscles, and the diaphragm all exert lateral distracting forces which, ultimately, result in increased fascial tension and possible fascial dehiscence [1, 11]. Biomechanical experiments using both human cadaveric and plastic surrogate sterna where most or all of the muscles were absent have demonstrated that lateral distracting forces transmitted through the ribs first cause sternal dehiscence at the xiphoid end of the incision [16, 10], suggesting that the distraction is mediated by the region’s osseous geometry. One study found that the defects’ distal border was formed by a bifid xiphoid process in all patients, supporting the theory of an early bony non-union [1].
Treatment of subxiphoid hernia
Subxiphoid hernia after median sternotomy is, in fact, a specific variety of incisional hernia. The contemporary treatment of the hernia follows a series of basic principles that are, or should be, common to all types of repair, whether open or laparoscopic, based upon extrapolation to this specific hernia of modern understanding of optimal hernia repair. These principles emphasize tension-free repair with permanent, well fixed, overlapping underlay prosthetic material, and are summarized in Table 2.
Open repair
The retrospective nature of the reported series, small numbers, heterogeneous population, and the lack of detailed descriptions and statistical analysis all make it difficult for one to conclude how to best manage these hernias. Reinforcement of a subxiphoid defect through an anterior approach is technically challenging because of two reasons: (1) at the cranial aspect, the insertion of the posterior rectus sheath in front of and near the xiphoid process inhibits a sound overlap of the osseous border and (2) adhesion of the heart to the scar potentially increases the risk of myocardial injury as the dissection proceeds cranially.
Suture closure of the defect brings together the fibrotic, retracted fascial margins, and, thus, contradicts the principles of “tension-free” repair. Indeed, such closure has reportedly been associated with high recurrence rates, between 43% and 80% [1, 9]. Repair using permanent mesh has been reported to yield lower recurrence rates ranging from 0% to 32% [1, 3, 5, 9].
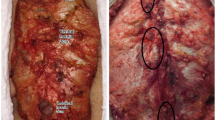
Open repair of subxiphoid hernia typically proceeds through the old incision and can be performed using various approaches, depending on the anatomy and the surgeon’s preference. The hernia sac can be relatively easily dissected from the defect margins and reduced. A tension-free endogenous repair has used linea alba-based, overlapping flaps from the anterior rectus abdominis sheaths [3] (Fig. 1a–c). The literature provides no data on whether using a permanent prosthesis might be a better option [17].
Prosthetic repairs can proceed in one of several ways, including use of the preperitoneal space. The mesh can be anchored to the posterior rectus abdominis sheath and left either exposed in the subcutaneous space [1] (Fig. 2a) or covered with the external oblique aponeurosis, which has been relaxed by multiple incisions and approximated in the midline [5] (Fig. 2b), also known as the Clotteau method. The upper margin of the defect consists mainly of cartilage, which poses technical problems for reliable mesh fixation. Partial or complete resection of the scarred xiphoid process may be required to optimize exposure for the repair. Perichondral strips of mesh at the costal margin, although extremely painful, have provided very satisfactory attachment, with excellent long-term results in difficult hernias for which other repair methods were not available [18]. It must be noted that the costal perichondrium is very well innervated; encircling the ribs with foreign material can cause persistent pain and, therefore, should be avoided [8].
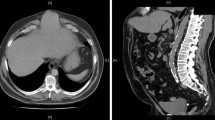
An effective sublay augmentation of the region requires an adequate cephalad overlap. The posterior rectus abdominis sheath must be transected at the costal margin in order to open the space between the peritoneum and the diaphragm. The maneuver helps to achieve a wide overlap cranial aspect of the defect, down to the hepatic veins and the esophagus (Fig. 3). Failure to achieve the overlap in the cephalad aspect approximates an onlay repair and carries a much higher recurrence risk.
Cross-sectional schematic diagram (sagittal right parasternal view) showing the topography of a sublay augmentation of the defect with adequate cephalad overlap. C = costal arch, M = rectus abdominis muscle, S = posterior rectus abdominis sheath, V = vena cava, L = liver, F = falciform ligament, P = peritoneal cavity, the arrow indicates the cut in the posterior rectus abdominis sheath through which the retromuscular prosthesis enters the preperitoneal space
The onlay method is, perhaps, the easiest and most reproducible technique for repair (Fig. 4). The ability to stay superficially in the subcutaneous plane, obtain good visibility, and achieve tissue overlap of 5 cm or more are among the claimed advantages of this technique. A 20% laxity has been recommended to compensate for shrinkage of the mesh [19, 20]. The literature suggests that using suprafascial mesh is associated with increased seroma formation and risk of infection, which cannot be fully eliminated by antibiotics and prophylactic drainage [21].
Laparoscopic repair
The laparoscopic treatment of subxiphoid hernia was pioneered in 2000 when a screen of bi-layer permanent composite (Composix™, C.R. Bard, Inc., Murray Hill, NJ) was brought up against the undersurface of the defect using four transmural corner stitches and tacked to the posterior rectus abdominis sheath all around the defect’s margins [6]. An analogous method of fixation was used in two subsequently published laparoscopic series, with reported recurrence rates of 10% and 33%, respectively [7, 9]. The authors claimed improved visibility of the defect margins [9].
The laparoscopic repair of subxiphoid hernia after sternotomy is based on most of the principles described by the recently published major trials of minimally invasive vental hernia repair [22–25]. An important technical point concerning the laparoscopic repair is the necessity to dissect the falciform ligament up to the hepatic veins. By doing this, the mesh overlap can extend to the hepatic veins and the esophagus (Fig. 5). The tissue overlap around the prosthesis must be at least 4 cm and, ideally, close to 5 cm [23, 25]. A sheet of mesh with low adhesive potential (Dual Mesh, W. L. Gore & Associates, Flagstaff, AZ) is typically rolled into a cigar-shape, introduced intraabdominally, unfolded, and stretched to lie parallel to the abdominal wall by pulling previously placed anchoring sutures through all abdominal layers. Once the patch is firmly held in place, endoscopic tackers are used around the edges to fix the prosthesis. The placement of additional full-thickness abdominal wall stitches circumferentially every 3–6 cm is considered to be mandatory [22–25]. Mesh fixation only with spiral tacks is not recommended, since most tacks do not penetrate more than 2 mm beyond the mesh [23]. A recent porcine experimental study demonstrated that the tensile strength of sutures used to fix intraabdominal prostheses was up to 2.5 times greater than that produced by the tacks [26]. The cranial overlap of the prosthesis will be fixed by the liver and the stomach when desufflating the pneumoperitoneum. This technique is routinely used by laparoscopic surgeons when repairing hernias after midline incisions. The good exposure, tension-free placement of the prosthesis, and wide coverage beyond the defect’s margin all contribute to a lower recurrence rate compared with open repairs [26].
Cross-sectional schematic diagram (sagittal right parasternal view) showing the topography of an intraperitoneal augmentation of the defect with adequate cephalad overlap. C = costal arch, M = rectus abdominis muscle, S = posterior rectus abdominis sheath (which was left intact), V = vena cava, L = liver, F with arrows = mobilized falciform ligament ventral and dorsal to the prosthesis, P = peritoneal cavity
It is considered sufficient to fix the mesh at or below the costal arch. Placement of endoscopic tacks right under the ribs and through the costochondral junction, along the edge of the sternum at the xiphoid, improves the closure, but creates chronic severe pain that often requires injection therapy in the office. Placing tackers beyond the costal chondral margin can cause life-threatening complications, such as pericarditis or even acute cardiac tamponade [27]. In addition, the limited accumulated experience with this method does not provide sufficient data regarding the influence of a prosthetic material anchored to the diaphragm on respiratory physiology [8].
Conclusions
The incidence of subxiphoid hernia after median sternotomy can be possibly reduced by paraxiphoid extension of the sternotomy [4], reinforcement near the xiphoid end of the incision, or by optimizing closure of the distal sternotomy and the linea alba. Non-absorbable aponeurotic suture of the epigastrium may further improve the closure’s stability. The repair of an established subxiphoid hernia is technically demanding, with no procedural standardization. It must be based on sound scientific principles (Table 2). Abdominal wall reinforcement by open-mesh closure or laparoscopic transperitoneal prosthetic repair can effectively deal with the defect (Table 3). Long-term outcome analyses comparing laparoscopic and open repair are not yet available.
References
Cohen MJ, Starling JR (1985) Repair of subxiphoid incisional hernias with marlex mesh after median sternotomy. Arch Surg 120:1270–1271
Davidson BR, Bailey JS (1986) Incisional herniae following median sternotomy incisions: their incidence and aetiology. Br J Surg 73:995–996
Davidson BR, Bailey JS (1987) Repair of incisional hernia after median sternotomy. Thorax 42:549–550
Barner HB (1987) A technical modification of median sternotomy to eliminate subxiphoid incisional hernias. Arch Surg 122:843
Bouillot JL, Badawy A, Alexandre JH (1997) Incisional abdominal hernia after median sternotomy. Repair with the use of Dacron mesh. Hernia 1:129–130
Muscarella P, Needleman BJ, Goldstein AH, Steinberg SM (2000) Laparoscopic repair of a subxiphoid incisional hernia following median sternotomy. Surg Rounds 23:605–611
Landau O, Raziel A, Matz A, Kyzer S, Haruzi I (2001) Laparoscopic repair of poststernotomy subxiphoid epigastric hernia. Surg Endosc 15:1313–1314
Conze J, Prescher A, Kisielinski K, Klinge U, Schumpelick V (2005) Technical consideration for subxiphoidal incisional hernia repair. Hernia 9:84–87
Mackey RA, Brody FJ, Berber E, Chand B, Henderson JM (2005) Subxiphoid incisional hernias after median sternotomy. J Am Coll Surg 201:71–76
Milton H (1897) Mediastinal surgery. Lancet 1:872–875
Julian OC, Lopez-Belio M, Dye WS, Javid H, Grove WJ (1957) The median sternal incision in intracardiac surgery with extracorporeal circulation: a general evaluation of its use in heart surgery. Surgery 42:753–761
Lachman N, Satyapal KS (1999) Origin and incidence of xiphoid branch of the internal thoracic artery. Surg Radiol Anat 21:351–354
Yahchouchy-Chouillard E, Aura T, Picone O, Etienne JC, Fingerhut A (2003) Incisional hernias. I. Related risk factors. Dig Surg 20:3–9
Dasika UK, Trumble DR, Magovern JA (2003) Lower sternal reinforcement improves the stability of sternal closure. Ann Thorac Surg 75:1618–1621
Losanoff JE, Collier AD, Wagner-Mann CC, Richman BW, Huff H, Hsieh F-H, Diaz-Arias A, Jones JW (2004) Biomechanical comparison of median sternotomy closures. Ann Thorac Surg 77:203–209
Askar OM (1977) Surgical anatomy of the aponeurotic expansions of the anterior abdominal wall. Ann R Coll Surg Engl 59:313–321
Bendavid R (2004) The unified theory of hernia formation. Hernia 8:171–176
Merrell RC, Than-Trong T (1985) Osseous and chondral fixation of polypropylene mesh. Am J Surg 149:816–818
Amid PK (2003) The Lichtenstein repair in 2002: an overview of causes of recurrence after Lichtenstein tension-free hernioplasty. Hernia 7:13–16
Freund HR, Charuzi I (2003) Laparoscopic and open repair of post-sternotomy incisional hernia of the subxiphoid region. In: Morales-Conde S (ed) Laparoscopic ventral hernia repair. Springer, Paris, France, pp 375–382
White TJ, Santos MC, Thompson JS (1998) Factors affecting wound complications in repair of ventral hernias. Am Surg 64:276–280
Ramshaw BJ, Esartia P, Schwab J, Mason EM, Wilson RA, Duncan TD, Miller J, Lucas GW, Promes J (1999) Comparison of laparoscopic and open ventral herniorrhaphy. Am Surg 65:827–831
Heniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Ann Surg 238:391–400
McKinlay RD, Park A (2004) Laparoscopic ventral incisional hernia repair: a more effective alternative to conventional repair of recurrent incisional hernia. J Gastrointest Surg 8:670–674
Novitsky YW, Cobb WS, Kercher KW, Matthews BD, Sing RF, Heniford BT (2006) Laparoscopic ventral hernia repair in obese patients: a new standard of care. Arch Surg 141:57–61
van’t Riet M, de Vos van Steenwijk PJ, Kleinrensink GJ, Steyerberg EW, Bonjer HJ (2002) Tensile strength of mesh fixation methods in laparoscopic incisional hernia repair. Surg Endosc 16:1713–1716
Park A, Heniford BT, LeBlanc KA, Voeller GR (2001) Laparoscopic repair of incisional hernias. Part 2: surgical technique. Contemp Surg 57:225–238
Acknowledgments
This material is the result of work supported with the resources and by the use of the facilities at the John D. Dingell VA Medical Center, Detroit, MI, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Losanoff, J.E., Basson, M.D., Laker, S. et al. Subxiphoid incisional hernias after median sternotomy. Hernia 11, 473–479 (2007). https://doi.org/10.1007/s10029-007-0258-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-007-0258-8