Abstract
Background/purpose
Many laparoscopic surgical techniques were described for management of inguinal hernia in pediatric patients. This prospective study was conducted to compare laparoscopic purse–string suture of hernia sac at the internal ring at one side, leaving the distal sac intact (technique I) and disconnection of the hernia sac with intra-corporeal suture of proximal part at the internal ring (technique II) in the other side in the same case.
Patients and methods
Thirty three patients with bilateral congenital inguinal hernia (66 repairs) were included in this study. The outcome variables were operative time, intraoperative complications, post-operative complications and recurrence rate.
Results
This study included 28 males and 5 females. The age of the patients ranged from 1 to 72 month with a mean of (15.27 ± 19.09). The operative time was shorter in technique I than in technique II and this difference was statistically significant. No intraoperative complications were reported. Five cases (15%) developed hydrocele and two cases (6%) developed recurrence in technique I during the follow up period.
Conclusion
Laparoscopic repair of congenital inguinal hernia using laparoscopic disconnection of the sac and closure of the internal ring has lower recurrence rate and hydrocele formation but longer operative time compared to laparoscopic purse–string closure alone. Due to the high rate of recurrence in technique I, there is definite superiority of technique II as a surgical option.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia is one of the most common disorders in pediatric patients and its incidence was reported to occur in 0.8–4.4% of children. It is more common in neonates and premature infants [1].
Management of this condition is performed by high ligation of the hernia sac at the internal inguinal ring (IIR) either through open or laparoscopic techniques [2].
Laparoscopic repair of congenital inguinal hernia has a wide acceptance and there are many centers routinely performing this approach nowadays. The documented advantages include excellent exposure of the both internal rings with detection and repair of contralateral patent processus vaginalis (PPV), minimal traumatic dissection to tissues, less complications, faster recovery, accepted recurrence rates and aesthetic results if compared to the open approach [3].
With advances of the minimal invasive surgery in pediatric patients, many improvements were developed to enhance results and outcome. These improvements involve laparoscopic instruments, number of the ports used, types of sutures and knots and the mode of dissection at the internal ring [4]. At our institution, different laparoscopic techniques are used to repair congenital inguinal hernia including needlescopic repair, laparoscopic purse–string suture at the internal ring with or without disconnection of the hernia sac.
The aim of this study is to compare two laparoscopic techniques in management of bilateral cases: Laparoscopic purse–string suture of hernia sac at the internal ring leaving the distal sac intact (technique I) versus disconnection of the hernia sac with intra-corporeal suture of proximal part at the internal ring (technique II). Both techniques will be applied to each case, one at each side.
Patients and methods
This prospective study was conducted on 33 patients presented with bilateral congenital inguinal hernia in the period between Feb 2015 and Sept 2019. Recurrent inguinal hernia, hernia with undescended testicles and neonates less than one month were excluded. Approval was obtained from the institute's Research Ethics committee with approval code 2977/12/14. Parents of each patient were informed about all steps in this study including the operative idea and post-operative follow up. An informed consent was taken from parents of each patient included in the study. All patients were subjected to thorough history taking, clinical examination, and routine laboratory investigations.
For each case, laparoscopic purse–string suture of hernia sac at the internal ring leaving the distal sac intact was done at the left side hernia (technique I) and laparoscopic disconnection of the hernia sac with intra-corporeal suture of proximal part at the internal ring was done at the right side hernia (technique II).
Operative procedure
Under general anesthesia, open technique was used to insert a 5-mm umbilical port for 5-mm 0°/30° scope. Additional 3-mm/5-mm trocars were inserted at the right and left midclavicular lines at both sides of the umbilicus. In infants and small babies, the working ports were inserted higher than the level of umbilicus.
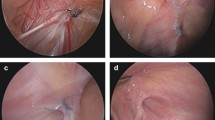
For the hernia on the left side, laparoscopic purse- string suture of the hernia sac at the internal ring was performed using 2/0 or 3/0 non-absorbable sutures with intra-corporeal ligation. The testicular vessels and the vas deference were visualized and secured during performing the suture. The peritoneum alone was included in the stitch along the inferior margin of the internal ring and the fascia transversalis and peritoneum were included at the superior margin of the ring (Fig. 1a, b).
For the hernia on the right side, a circumferential incision of the peritoneum at the internal ring was performed. The vas deference and the testicular vessels were dissected away under vision and then the peritoneum posterior to the internal ring was divided followed by anterior dissection then the peritoneal defect was closed by intra-corporeal 2/0 or 3/0 non-absorbable sutures (Fig. 2a–d). Finally, the abdomen was deflated and the abdominal incisions were closed.
All patients were discharged on the same day. They were followed up in the outpatient clinic 2 weeks, 3 months and 6 months after the operation and parents were advised to contact the department of pediatric surgery, if there were any concerns in the immediate post-operative period. Patient assessment in post-operative visits was based on clinical examination of the operative site and ipsilateral testis to detect recurrence or testicular atrophy. On doubtful condition of the testis, an ultrasonography and duplex were used for further assessment.
The two operative techniques were compared as regard to the operative time, the intraoperative complications, the post-operative complications and the recurrence rate.
Data were collected and tabulated. Statistical analysis was conducted using SPSS™ ver. 20 (IBM SPSS, NY, USA). Student t test was used to analyze numerical variables whereas Fisher’s exact test was used to analyze categorical variables and Chi square was used to assess the homogeneity of the two groups regarding demographics and confounding factors. P value less than 0.05 was considered statistically significant.
Results
This study included 33 patients with bilateral congenital inguinal hernia yielding 66 hernia repairs.
Two laparoscopic procedures were performed in the same patient. Patient’s demographics were illustrated in Table 1. Hernia characteristics regarding type, content and duration was compared in Table 2. Cases in both techniques were homogenous regarding these confounding factors, with no significant statistical difference.
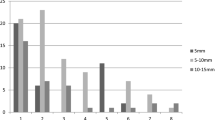
The operative time of both techniques was calculated from the start of the technique to its end, omitting the time of trocar insertion, insufflation and wound closure. The mean operative time for both techniques was compared separately for males vs. females, and cases < 12 months vs. cases > 12 months, due to the natural differences in time consumption among these groups; Table 3. The operative time was shorter in technique I than technique II and this difference was statistically significant. No intraoperative complications (bleeding, injury to vas, vessels or bowels) were reported.
Five hernias operated with technique I (15%) developed hydrocele which resolved spontaneously while; no hernias operated with technique II had post-operative hydrocele. This difference was statistically significant (p = 0.02). Scrotal hematoma developed in one hernia (3%) operated with technique II, which resolved spontaneously without surgical intervention. Two hernias (6%) operated with technique I developed recurrence during the follow up period Table 4. The 1st case was a 3 months old male, recurrence was noticed on the 2nd post-operative day on the right side. Open repair was done and the patient discharged on the same day. Follow up for 6 months revealed no recurrence. The 2nd case was a one month old male with recurrence occurred at the right side on the 5th post-operative day; open repair was done and the patient discharged at the same day. Follow up for 9 months revealed no recurrence. No recurrence was reported in hernias repaired with technique II. This difference was not statistically significant. There were no cases with testicular atrophy or retraction of the testis up to the groin during the follow up period. All cases were completed laparoscopically without conversion to open surgery. All of them achieved full recovery, started oral feeding 4 h after the operation and discharged on the same day.
Discussion
Many surgical techniques were described in the literature for laparoscopic repair of congenital inguinal hernia in pediatric patients, these techniques can be summarized as: intra-corporeal, extracorporeal and percutaneous approaches [5]. Laparoscopic intra-corporeal purse–string suture at the internal ring using non-absorbable stitches for repair of congenital inguinal hernia was first described by Philippe Montupet in 1993 [6]. Several modifications of the technique were described and published, including Z suture, flip flap technique, interrupted or continuous sutures. However, these techniques were not devoid of high recurrence rate due to the skip area which left over the vas deference and testicular vessels [7, 8]. For that reason, many techniques were introduced in which the peritoneum was transected or disconnected at the internal ring aiming at making some trauma and scarring which improves healing [9]. The recurrence rate was decreased to reach 0–4% in many series using these techniques [10,11,12,13].
This study included 33 patients with bilateral congenital inguinal hernia, for whom we compared two laparoscopic repair techniques in each patient, one in each side: purse–string suturing of the internal ring (technique I) versus disconnection of the hernia sac and repair of the peritoneal defect (technique II). Comparing two techniques in the same patient carries the advantage of elimination of all confounding factors that may affect the results, including age, sex, obesity and general status of the patient.
In this study, closure of peritoneal defect was done using absorbable sutures: polyglactin (vicryl™, Ethicon, NJ, USA) after disconnection of the sac in technique II. The peritoneal trauma due to dissection, diathermy heat & subsequent scarring are supposed to be the main factors responsible for the better healing, Other studies reported using vicryl suture to perform intra-corporeal purse–string suture after disconnection of hernia sac and that the use of absorbable sutures is justified in this technique [14, 15].
Laparoscopic techniques for congenital inguinal hernia repair are known to consume a longer operative time than the traditional open technique ranging from 25 to 47 min in the literature. This time decreases gradually with advancement in laparoscopic training [16, 17]. In this study, the mean operative time was 22.50 ± 8.16 min and 37.68 ± 8.22 min in males in technique I and II respectively, and 20.0 ± 5.0 min and 31.0 ± 5.48 min in females in technique I and II respectively. This difference was statistically significant. Hasanin et al. reported that the mean operative time was 13.9 ± 1.7 min in group (closure with purse–string without disconnection) and was 16.0 ± 2.8 min in group II (disconnection of the hernia sac and purse sting suture) [18]. In Oshiba et al. study, the mean duration of surgery was 32.50 ± 6.18 min in group I and 34.0 ± 7.88 min in group II [19]. The median operating time was 19 min in Montupet and Esposito study who disconnect the peritoneum distally and performing a purse–string suture around the proximal peritoneum using a 4–0 non-absorbable suture [20]. The mean operative time was 42 min in Tsai et al. study who performed disconnection and purse–string suture at the internal ring [21].
No intraoperative complications occurred in this study and this may be due to the meticulous dissection of the hernia sac and the careful sweeping of the vas and testicular vessels during manipulation of the peritoneum. Similar results were also reported in many other studies [14, 21, 22].
One of the main criticisms of the laparoscopic techniques for repair of pediatric inguinal hernias is the recurrence rate. It ranged from 0.7 to 4.5% in most series [23,24,25,26]. It could possibly be due to closure of the internal ring under tension, broken purse–string suture, large size hernia and the missed area of the peritoneum over the vas deference and the testicular vessels making skip area susceptible for recurrence [27]. Two hernias (6%) in technique I developed recurrence during the follow up period while no recurrence was reported in hernias in technique II. This difference was not statistically significant.
During the follow up period, five hernias (15.15%) developed scrotal hydrocele (operated with technique I) which resolved spontaneously over six months. Scrotal hydrocele incidence was less in cases operated with technique II which may be attributed to disconnection of hernia sac. On the other hand, scrotal hematoma appeared in one case (3.03%) in technique II which resolved with conservative treatment. Shalaby et al., in their study on laparoscopic repair using purse–string alone, reported that 4% of their cases developed scrotal hydrocele and they were managed conservatively without surgery [7]. Tam et al. reported that post-operative hydrocele occurred in 1% of their cases which were repaired using laparoscopic purse–string sutures without disconnection and resolved spontaneously without treatment [28]. In another study of Shalaby et al., they reported 4 cases with hematoma (0.57%), one case required percutaneous aspiration, while the other cases successfully responded to conservative treatment [29]. Similar results were also reported in other series [11, 19, 30] and these results proved that post-operative hydrocele and hematoma are acceptable complications after laparoscopic techniques for hernia repair as they resolve spontaneously. Testicular atrophy and iatrogenic retracted testis were not reported in this study during the follow up period. Shalaby et al., supported the same result in their study [29]. One case of cryptorchidism and another case of testicular atrophy were reported by Tam et al. in their study which included 433 cases [28]. No conversion to open technique was reported in this study. Esposito et al. [31] and Shehata et al. [32] reported similarly, no conversion in their studies.
The current study is the first study to compare laparoscopic purse–string suture alone with laparoscopic peritoneal disconnection with ligation techniques in bilateral congenital inguinal hernia in the same patients, and this will make most confounding variables fixed (age, sex and weight) but still the size of the IIR is different between the two sides and may affect the results.
Conclusion
Laparoscopic repair of congenital inguinal hernia using laparoscopic purse–string closure at the IIR alone or with disconnection of the sac and purse–string closure at the IIR are effective, safe and feasible techniques.
Laparoscopic disconnection of the hernia sac and purse–string closure at the internal ring had minimal post-operative complications, lower recurrence rate and hydrocele formation but longer operative time compared to laparoscopic purse–string closure alone.
There is definite superiority of laparoscopic disconnection purse–string closure over purse–string closure alone considering the high recurrence rate of the later (6%).
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- IIR:
-
Internal inguinal ring
- PPV:
-
Patent processus vaginalis
References
Chan KL, Tam PK (2004) Technical refinements in laparoscopic repair of childhood inguinal hernias. Surg Endosc 18(6):957–960
Turial S, Enders J, Krause K, Schier F (2011) Laparoscopic inguinal herniorrhaphy in babies weighing 5 kg or less. Surg Endosc 25(1):72–78
Saranga Bharathi R, Arora M, Baskaran V (2008) Minimal access surgery of pediatric inguinal hernias: a review. Surg Endosc 22(8):1751–1762
Esposito C, Montinaro L, Alicchio F, Savanelli A, Armenise T, Settimi A (2010) Laparoscopic treatment of inguinal hernia in the first year of life. J Laparoendosc Adv Surg Tech A 20(5):473–476
Ostlie DJ, Ponsky TA (2014) Technical options of the laparoscopic pediatric inguinal hernia repair. J Laparoendosc Adv Surg Tech A 24(3):194–198
Esposito C, Escolino M, Farina A, Settimi A (2014) Two decades of history of laparoscopic pediatric inguinal hernia repair. J Laparoendosc Adv Surg Tech A 24(9):669–670
Shalaby R, Ismail M, Dorgham A, Hefny K, Alsaied G, Gabr K et al (2010) Laparoscopic hernia repair in infancy and childhood: evaluation of 2 different techniques. J Pediatr Surg 45(11):2210–2216
Schier F (2006) Laparoscopic inguinal hernia repair-a prospective personal series of 542 children. J Pediatr Surg 41(6):1081–1084
Marte A, Sabatino MD, Borrelli M, Parmeggiani P (2009) Decreased recurrence rate in the laparoscopic herniorrhaphy in children: comparison between two techniques. J Laparoendosc Adv Surg Tech A 19(2):259–262
Boo YJ, Han HJ, Ji WB, Lee JS (2012) Laparoscopic hernia sac transection and intracorporeal ligation show very low recurrence rate in pediatric inguinal hernia. J Laparoendosc Adv Surg Tech A 22(7):720–723
Becmeur F, Philippe P, Lemandat-Schultz A, Moog R, Grandadam S, Lieber A et al (2004) A continuous series of 96 laparoscopic inguinal hernia repairs in children by a new technique. Surg Endosc 18(12):1738–1741
Koivusalo AI, Korpela R, Wirtavuori K, Piiparinen S, Rintala RJ, Pakarinen MP (2009) A single-blinded, randomized comparison of laparoscopic versus open hernia repair in children. Pediatrics 123(1):332–337
Chan KL, Hui WC, Tam PK (2005) Prospective randomized single-center, single-blind comparison of laparoscopic vs open repair of pediatric inguinal hernia. Surg Endosc 19(7):927–932
Pant N, Aggarwal SK, Ratan SK (2014) Laparoscopic repair of hernia in children: comparison between ligation and nonligation of sac. J Indian Assoc Pediatr Surg 19(2):76–79
Riquelme M, Aranda A, Riquelme QM (2010) Laparoscopic pediatric inguinal hernia repair: no ligation, just resection. J Laparoendosc Adv Surg Tech A 20(1):77–80
Schier F (1998) Laparoscopic herniorrhaphy in girls. J Pediatr Surg 33(10):1495–1497
Darzi A, Nduka CC (1997) Endoscopically guided percutaneous repair of inguinal hernia through a 2-cm incision. Minihernia repair Surg Endosc 11(7):782–784
Hasanein ARM, Fathi M, El Sayed A (2017) Laparoscopic purse-string suture sac closure is appropriate procedure for children with unilateral indirect inguinal hernia: comparative study versus laparoscopic sac excision and closure procedure. Egypt J Surg 36(4):394
Oshiba AAK, Aboheba M, Shehata S, Shalaby R (2016) Comparative study between purse–string suture and peritoneal disconnection with ligation techniques in the laparoscopic repair of inguinal hernia in infants and children. Ann Pediatr Surg 12(4):137–141
Montupet P, Esposito C (2011) Fifteen years experience in laparoscopic inguinal hernia repair in pediatric patients. Results and considerations on a debated procedure. Surg Endosc 25(2):450–453
Tsai YC, Wu CC, Ho CH, Tai HC, Yang SS (2011) Minilaparoscopic herniorrhaphy in pediatric inguinal hernia: a durable alternative treatment to standard herniotomy. J Pediatr Surg 46(4):708–712
Shehata SM, El Attar AA, Attia MA, Hassan AM (2013) Laparoscopic herniotomy in children: prospective assessment of tertiary center experience in a developing country. Hernia 17(2):229–234
Shah R, Arlikar J, Dhende N (2013) Incise, dissect, excise and suture technique of laparoscopic repair of paediatric male inguinal hernia. J Minim Access Surg 9(2):72–75
Kumar A, Ramakrishnan TS (2013) Single port laparoscopic repair of paediatric inguinal hernias: our experience at a secondary care centre. J Minim Access Surg 9(1):7–12
Ponsky TA, Nalugo M, Ostlie DJ (2014) Pediatric laparoscopic inguinal hernia repair: a review of the current evidence. J Laparoendosc Adv Surg Tech A 24(3):183–187
Shalaby R, Abd Alrazek M, Elsaied A, Helal A, Mahfouz M, Ismail M et al (2018) Fifteen years experience with laparoscopic inguinal hernia repair in infants and children. J Laparoendosc Adv Surg Tech A 28(1):101–105
Treef W, Schier F (2009) Characteristics of laparoscopic inguinal hernia recurrences. Pediatr Surg Int 25(2):149–152
Tam YH, Lee KH, Sihoe JD, Chan KW, Wong PY, Cheung ST et al (2009) Laparoscopic hernia repair in children by the hook method: a single-center series of 433 consecutive patients. J Pediatr Surg 44(8):1502–1505
Shalaby R, Ismail M, Samaha A, Yehya A, Ibrahem R, Gouda S et al (2014) Laparoscopic inguinal hernia repair; experience with 874 children. J Pediatr Surg 49(3):460–464
Giseke S, Glass M, Tapadar P, Matthyssens L, Philippe P (2010) A true laparoscopic herniotomy in children: evaluation of long-term outcome. J Laparoendosc Adv Surg Tech A 20(2):191–194
Esposito C, Escolino M, Cortese G, Aprea G, Turra F, Farina A et al (2017) Twenty-year experience with laparoscopic inguinal hernia repair in infants and children: considerations and results on 1833 hernia repairs. Surg Endosc 31(3):1461–1468
Shehata SM, Attia MA, Attar AAE, Ebid AE, Shalaby MM, ElBatarny AM (2018) Algorithm of laparoscopic technique in pediatric inguinal hernia: results from experience of 10 years. J Laparoendosc Adv Surg Tech A 28(6):755–759
Funding
This study had no funding from any resource.
Author information
Authors and Affiliations
Contributions
HAA gave the idea and collected the patients’ data and analyzed them. MAS wrote the paper with revision and the corresponding author. MAM put study design and followed the patients postoperatively.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest or financial ties to disclose. Content have not published elsewhere, and the paper not being submitted elsewhere.
Ethical approval
This study was approved by the Review Board of the Department of General Surgery, Faculty of Medicine, Tanta University, Egypt, on 31th December 2014. All patients included in this study gave written informed consent to participate in this research. If the patient was less than 16 years’ old or unconscious at the time of the study, written informed consent for their participation was given by their parent or legal guardian. The committee’s reference number: 2977/12/14.
Informed consent
All patients included in this research gave written informed consent to publish the data contained within this study. If the patient was less than 16 years’ old, deceased or unconscious when consent for publication was requested, written informed consent for the publication of this data was given by their parent or legal guardian.
Rights and permissions
About this article
Cite this article
Almetaher, H.A., Hassan, H.S., Effat, A. et al. Laparoscopic repair of congenital inguinal hernia: a comparative study between purse–string suture and peritoneal disconnection with ligation techniques in bilateral cases. J Ped Endosc Surg 2, 83–89 (2020). https://doi.org/10.1007/s42804-020-00052-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42804-020-00052-y