Abstract
Objectives
The purpose of this in vitro study was to compare the precision of fit of frameworks milled from semi-sintered regular zirconia and high-translucent (HT) zirconia blanks, fabricated with two different CAD/CAM systems.
Material and methods
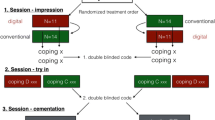
Three-unit, posterior fixed dental prostheses (FDP) frameworks were fabricated for standardized dies (n = 11) with two different laboratory computer-aided design (CAD)/computer-aided manufacturing (CAM) systems (Cercon/Ceramill). The replica technique was used to evaluate the marginal and internal fit under an optical microscope. Evaluation of the data was performed according to prior studies at a level of significance of 5%.
Results
The systems showed a statistically significant influence on the internal fit of the frameworks (p ≤ 0.001) and on the marginal fit (p < 0.001). The type of material showed no influence on the marginal fit for the Cercon system (p = 0.636) and on the marginal fit (p = 0.064) and the internal fit (p = 0.316) for the Ceramill system, while regular zirconia from Cercon showed higher internal values than HT zirconia (p = 0.016).
Conclusions and clinical relevance
Both investigated systems showed clinically acceptable values within the limitations of this in vitro study. However, one showed less internal accuracy when regular zirconia was used.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With growing awareness of biocompatibility and esthetics, patients prefer metal-free restorations for posterior fixed dental prostheses (FDP). Especially in this area of the mouth, where the biting forces are at a maximum, the requirement of the ceramics for FDP fabrication regarding strength and fracture toughness has come into the focus of preclinical and clinical interventions. Different high-strength ceramics are now available [1], in which yttria-stabilized zirconia has evolved as the material of choice for the clinical use of posterior FDPs [1–3]. Zirconia unites many positive characteristics of dental ceramics such as biocompatibility, low plaque retention, absence of allergies, and no metallic conduction, but shows a high opacity being a disadvantage regarding the esthetic outcome with high clinical relevance. Recent studies by Stawarczyk et al. showed the influence of the sintering temperature on the translucency of zirconia [4]. High-translucent materials are suitable for anterior restorations, as achieving natural esthetics is easier than that with regular opaque zirconia.
Fully sintered blanks were fabricated from a process known as hot isostatic pressing (HIP). These blanks stand out due to excellent fitting because a second sintering is not required [5–7]. Mentionable disadvantages are the extended milling time and the increased wear of the milling burs in computer-aided manufacturing (CAM) machines [5–7]. Another method uses semi-sintered blanks. These blanks have a chalk-like consistency so that they show less resistance during the milling process [1, 6, 8–10]. In this approach, the substructure or monolithic restoration is sintered to full density after the first sintering process. A relevant disadvantage of this concept, the sinter shrinkage observed after the second sintering, which amounts to 15–30%, can influence the fit of the framework significantly [2, 11]. Studies working with milling densely sintered blanks reported no secondary caries [7, 12]. So, it might be concluded that compensation of the sinter shrinkage leads to a clinical problem of early systems milling pre-sintered blanks [2, 11].
The internal and especially the marginal adaption of FDPs are of paramount importance for the long-term clinical success of a restoration. There is a consensus between various authors that marginal openings below 120 μm in in vivo studies are clinically acceptable [13–16]. Some authors postulate marginal gap widths of 50–75 μm [17, 18], although gaps of less than 80 μm are difficult to detect in clinical practice. For in vitro studies, the obtained results should be better than those in in vivo studies, because they offer ideal conditions. A poor fit could increase plaque accumulation which might lead to periodontal disease and therefore to bone loss [2, 11, 19–24] or an increased risk for secondary caries. The internal fit is also important for the durability of the restoration. The fracture strength is significantly reduced by cement layers above 70 μm, which Tuntiprawon examined for aluminous porcelain jacket crowns [25].
The fitting of pre-sintered zirconia FDPs showed clinically acceptable results [11, 26], but, to the authors’ best knowledge, there is no data on the accuracy of high-translucent zirconia.
The null hypothesis of this study is that both computer-aided design (CAD)/CAM systems produce marginal gap widths below 120 μm and that there is no difference between both systems and materials.
Material and methods
A standardized cast model with a missing mandibular right first molar was used (Fig. 1). The second premolar and the second molar had a 360° chamfer preparation. Forty-six impressions were made (Adisil blau, Siladent Dr. Boehme und Schoeps GmbH, Goslar, Germany) and poured in class IV resin-reinforced die stone (ResinRock, Whip Mix Corp, Louisville, KY). This die stone had an improved surface smoothness and an increased resistance to abrasion, which was necessary for this study.
The models were tested for defects. If there was a defect, a new model was produced. Forty-four models were consecutively numbered; two models were used for prestudies.
The appropriate cement space thickness of each CAD/CAM system was determined as follows:
Three frameworks were designed with each of the CAD/CAM systems having three different cement spaces. After milling and sintering, the frameworks were returned to their respective dies and internal impressions were made (Xantopren L blau, Heraeus Kulzer GmbH, Hanau, Germany) and evaluated visually. The frameworks with the best fitting under finger pressure were chosen for the study. For the CAD/CAM system, Cercon, a virtual cement space of 50 μm was selected, while Ceramill required a virtual cement space of 40 μm. The same calibrated investigator fabricated all specimens.
A technician with more than 15 years CAD/CAM experience instructed the investigator in prestudies to manufacture FDPs in the same quality.
Laboratory CAD/CAM systems
Cercon (DeguDent)
The procedure was described in previous studies [27]:
A laser scanner (Cercon eye, DeguDent, Hanau, Germany) performed the digitalization of the dies, and the frameworks were designed in the CAD program of the system (Cercon art, DeguDent). A wall thickness of 0.5 mm, which was the minimum for zirconium oxide frameworks and preinstalled at the program, and a virtual cement layer of 50 μm were used. The connector cross section was set at least at 9 mm2.
Twenty-two pieces of the designed framework were fabricated—11 from regular zirconia and 11 from HT zirconia—using the CAM unit of the system (Cercon Brain). The chemical compositions are stated in Tables 1 and 2.
The frameworks were milled from semi-sintered zirconia blanks (Cercon base disk 20, DeguDent) and semi-sintered HT zirconia blanks (Cercon HT, DeguDent). Every framework was milled from a separate disk. The milled, enlarged frameworks were sintered to full density at a temperature of 1623 K for zirconia for 8 h and 1773 K for HT zirconia for 8.5 hours.
Ceramill (Amann Girrbach)
A laser scanner (Ceramill map 300, Amann Girrbach, Koblach, Austria) performed the digitalization of the dies and the CAD program of the system helped design the frameworks (Ceramill mind, Amann Girrbach). A wall thickness of 0.5 mm and a virtual cement layer of 40 μm were used. The surface area of the connector cross section was set at least at 9 mm2.
Twenty-two frameworks, 11 of zirconia and 11 of HT zirconia, were fabricated using the laboratory CAM unit of the system (Ceramill motion). The chemical compositions are stated in Tables 3 and 4.
The frameworks were milled from semi-sintered zirconia blanks (Ceramill Zi, Amann Girrbach) and semi-sintered HT zirconia blanks (Ceramill Zolid, Amann Girrbach). Every framework was milled from a separate disk. The milled, enlarged frameworks were sintered to full density at temperature of 1723 K for both materials resulting in shrinkage to the desired dimensions. To calculate the shrinkage, the CAD/CAM program required a special factor for each material. Ceramill Zi needed a factor of 4.0, while Ceramill Zolid needed a factor of 7.0, which was stated on the blanks.
After this, all frameworks were examined for deformity and debris, then steam-cleaned (Triton SLA, Bego, Bremen, Germany). An experienced dental technician adapted the frameworks to the dies. To identify areas that needed correction, color (Bite-X Articulating Paste, Asami Tanaka Dental Enterprises Europe GmbH, Friedrichsdorf, Germany) was applied onto the die, and the framework was placed without force [28]. The technician removed the red spots with a diamond rotary cutting instrument (Komet 8801014, Brasseler) with water-cooling spray and he kept on until the spots disappeared and the restoration had a good clinical seat and a correct marginal closure without imperfections. Time for adaption was recorded (t < 5 min).
To measure the marginal and internal fit of the FDP, the replica technique described by Reich et al. was applied [11, 29, 30]:
The frameworks were filled with a light-body silicone (President light body green, Coltène, Konstanz, Germany) and the FDP substructure was placed on its die with finger pressure. After the light-body silicone was set, the framework was removed and the thin silicone film stabilized by injecting a heavy-body silicone (President heavy body, Coltène) (Figs. 2, 3). After removing the replicas, they were sectioned with a scalpel (Feather disposable scalpel blade no.11, Feather Safty Razor Co., Ltd., Osaka, Japan): premolar replicas were divided into four pieces by a mesio-distal and a bucco-lingual section, and molar replicas were divided into six pieces by further bucco-lingual section (Fig. 4). With a microscope (Axioskop 2 Mat, Zeiss, Oberkochen, Germany), the gap width between the FDP and die was measured at a magnification of 50:1. A digital camera (D 100, Nikon, Tokyo, Japan) was connected with the microscope and the photographs were transferred to the imaging data program (Optimas 6.5, Media Cybernetics, Silver Spring, MD, USA) (Fig. 5).
The measurement was provided by an employee for technology and materials. The principal investigator was calibrated in a prestudy to achieve a precision of 90% and a trueness of 5 μm as described in prior studies [31]:
A series of points was set manually with the mouse of the computer on the junction between the light- and heavy-body silicone to get the first reference line. To establish the second line, a series of points was placed on the junction of light-body silicone and the abutment. The computer program connected two points from one side, and a perpendicular line was dropped from a point of the opposite border. The length of the perpendicular line corresponded to the cement gap in microns (μm).
For a better comparison, the measurements were divided into four different areas of interest: marginal gap, chamfer area, axial area, and occlusal area according to prior publications [28, 31].
Marginal gap: Closest distance between die and framework.
Chamfer area: The internal adaptation of the framework at the point of the biggest diameter.
Axial area: The internal adaptation of the crown walls at the midpoint of the axial wall (2 mm occlusal to the margin of the die).
Occlusal area: The internal adaptation of the inner surface of the framework to the die at the midpoint from the facial and proximal area.
Statistics
The statistical analysis was performed using SPSS version 21.0 (SPSS Germany, Munich, Germany). Descriptive statistics was calculated. Data were tested for normal distribution by the Shapiro-Wilk test. The medians of the gap dimensions of each group were statistically analyzed with a non-parametric test (Mann-Whitney U test) as the data were not normally distributed. The level of significance was set at 5%.
Results
Tables 5 and 6 show the number (N) of measure points at M and CAO, the lower quartile (Q0.25), the median (Q0.5), and the upper quartile (Q0.75) in micrometers (Figs. 6, and 7).
The median adaptation gap dimensions for Cercon were 27 μm (marginal M) and 57 μm (chamfer area, axial, occlusal CAO). Regular zirconia from Cercon showed a median of 27 μm (M) and 59 μm (CAO) and that of HT zirconia of 26 μm (M) and 55 μm (CAO).
Ceramill frameworks showed median adaptation gap dimensions of 21 μm (M) and 43 μm (CAO). Regular Ceramill zirconia showed a median of 20 μm (M) and 42 μm (CAO) and HT that of zirconia of 22 μm (M) and 44 μm (CAO).
The median internal and marginal gap widths of both systems were significantly different (p < 0.001).
The median marginal gap widths for Cercon showed no significant difference between zirconia and HT zirconia (p = 0.636). Also, the median marginal gap values for Ceramill showed no significant difference between the examined materials (p = 0.064) just like the internal fit (p = 0.316), while the median internal gap values for Cercon were significantly different between the two materials (p = 0.016). Regular zirconia from Cercon showed higher internal values than HT zirconia. To the authors’ best knowledge, there are no data on the accuracy of high-translucent zirconia so that no comparison can be drawn.
The median internal fit for Cercon between both tested materials was significantly different, while no differences between the materials by Ceramill were detected.
Discussion
The consensus between various authors is that a clinically acceptable marginal opening is below 120 μm for in vivo studies. Weaver et al. [18] postulated an acceptable marginal gap width for full crowns of 70 (±10) μm, while Hung et al. suggested 50–75 μm [17]. For CAD/CAM-fabricated all-ceramic crowns, marginal gap widths of 23–74 μm were reported in the literature [19, 32, 33]. Both systems and materials tested in the present in vitro study showed a clinically acceptable marginal median gap dimension of 20–27 μm, so that the null hypothesis can be accepted.
Ceramill showed lower values than Cercon, but the difference was so low (≤17 μm) that it presumably does not affect clinical use. Also, the differences (≤10 μm) between the materials of one system were scarcely of any importance in daily clinical use. The median internal adaption (CAO) also showed acceptable results, but the values were lower than in those further studies [27, 28, 31]. Tuntiprawon and Wilson examined the fracture strength of aluminous porcelain jacket crowns [25]. Their study showed that cement layers between 73 and 122 μm at the axial wall reduce the compressive strength without any significant improvement of seating. In this in vitro study, the values were lower, but the present data did not indicate any contact between the die and framework, which might have been visible in the replicas. To increase the cement layer, a higher spacer parameter had to be set, which directly increases the internal gap width. Further studies are needed to examine the fitting and the fracture strength of both systems and materials in vivo and in vitro, because the Tuntiprawon study does not directly refer to zirconia. Another aspect is that thin cement layers (80 μm) in the occlusal area are more favorable for mechanical stability [34] and a higher precision in internal fit can reduce the risk for veneering fracture [35]. Both systems and materials could fulfill this requirement.
In vitro studies offer standardized and optimized conditions. Only one cast model was used so that the preparation design was the same for all the examined frameworks. Therefore, the results of the present study show the fit of CAD/CAM systems under ideal conditions. CAD/CAM technologies involve scanning, software, and machine procedures. Each single step could lead to inaccuracy of fitting such as an inadequate spacer parameter or inadequate calculated sinter shrinkage. To avoid this, prestudies were done to find out the right spacer parameter for each system. Both tested CAD/CAM systems used the same preparation model, but a different laser scanner, different CAD software, different semi-sintered zirconia blanks, and different milling machines were involved; significant differences can be caused through every step of manufacturing. Further studies are needed to examine whether a change in the design settings can bring the internal values for Cercon regular zirconia in line with high-translucent zirconia.
The limitations of the present study were the following: (1) To avoid inaccuracies, all frameworks were adapted with a standardized protocol by an experienced technician. The fit was controlled by two experienced examiners and the replica technique where only intact replicas were used. (2) The gap dimensions were measured using the replica technique. As a result, the precision was just measured at a few defined areas per framework, which might not present the complete fit. (3) All frameworks were produced and tested under ideal conditions, which might not reflect the fitting in daily clinical use. Further studies are needed to confirm the results of this study for different spans of FDP and more available systems.
Conclusions
According to the results of this study, the following conclusions can be drawn:
-
1.
Both CAD/CAM systems showed in vitro acceptable marginal openings.
-
2.
The internal fit of both systems showed acceptable results.
-
3.
Translucent zirconia exhibited the same accuracy as regular substructure zirconia.
References
Tinschert J, Natt G, Mohrbotter N, Spiekermann H, Schulze KA (2007) Lifetime of alumina- and zirconia ceramics used for crown and bridge restorations. J Biomed Mater Res B Appl Biomater 80(2):317–321. doi:10.1002/jbm.b.30599
Sailer I, Feher A, Filser F, Gauckler LJ, Luthy H, Hammerle CH (2007) Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont 20(4):383–388
Tinschert J, Natt G, Mautsch W, Augthun M, Spiekermann H (2001) Fracture resistance of lithium disilicate-, alumina-, and zirconia-based three-unit fixed partial dentures: a laboratory study. Int J Prosthodont 14(3):231–238
Stawarczyk B, Emslander A, Roos M, Sener B, Noack F, Keul C (2014) Zirconia ceramics, their contrast ratio and grain size depending on sintering parameters. Dent Mater J 33(5):591–598
Vult von Steyern P, Carlson P, Nilner K (2005) All-ceramic fixed partial dentures designed according to the DC-Zirkon technique. A 2-year clinical study. J Oral Rehabil 32(3):180–187. doi:10.1111/j.1365-2842.2004.01437.x
Beuer F, Schweiger J, Edelhoff D (2008) Digital dentistry: an overview of recent developments for CAD/CAM generated restorations. Br Dent J 204(9):505–511. doi:10.1038/sj.bdj.2008.350
Edelhoff D, Florian B, Florian W, Johnen C (2008) HIP zirconia fixed partial dentures—clinical results after 3 years of clinical service. Quintessence Int 39(6):459–471
Sachs C, Groesser J, Stadelmann M, Schweiger J, Erdelt K, Beuer F (2014) Full-arch prostheses from translucent zirconia: accuracy of fit. Dental materials: official publication of the Academy of Dental Materials 30(8):817–823. doi:10.1016/j.dental.2014.05.001
Stawarczyk B, Ozcan M, Hallmann L, Ender A, Mehl A, Hammerlet CH (2013) The effect of zirconia sintering temperature on flexural strength, grain size, and contrast ratio. Clinical oral investigations 17(1):269–274. doi:10.1007/s00784-012-0692-6
Kohorst P, Herzog TJ, Borchers L, Stiesch-Scholz M (2007) Load-bearing capacity of all-ceramic posterior four-unit fixed partial dentures with different zirconia frameworks. Eur J Oral Sci 115(2):161–166. doi:10.1111/j.1600-0722.2007.00429.x
Reich S, Wichmann M, Nkenke E, Proeschel P (2005) Clinical fit of all-ceramic three-unit fixed partial dentures, generated with three different CAD/CAM systems. Eur J Oral Sci 113(2):174–179. doi:10.1111/j.1600-0722.2004.00197.x
Tinschert J, Schulze KA, Natt G, Latzke P, Heussen N, Spiekermann H (2008) Clinical behavior of zirconia-based fixed partial dentures made of DC-Zirkon: 3-year results. Int J Prosthodont 21(3):217–222
Belser UC, MacEntee MI, Richter WA (1985) Fit of three porcelain-fused-to-metal marginal designs in vivo: a scanning electron microscope study. J Prosthet Dent 53(1):24–29
Karlsson S (1993) The fit of Procera titanium crowns. An in vitro and clinical study. Acta Odontol Scand 51(3):129–134
McLean JW, von Fraunhofer JA (1971) The estimation of cement film thickness by an in vivo technique. Br Dent J 131(3):107–111
Sulaiman F, Chai J, Jameson LM, Wozniak WT (1997) A comparison of the marginal fit of In-Ceram, IPS Empress, and Procera crowns. Int J Prosthodont 10(5):478–484
Hung SH, Hung KS, Eick JD, Chappell RP (1990) Marginal fit of porcelain-fused-to-metal and two types of ceramic crown. J Prosthet Dent 63(1):26–31
Weaver JD, Johnson GH, Bales DJ (1991) Marginal adaptation of castable ceramic crowns. J Prosthet Dent 66(6):747–753
Bindl A, Mormann WH (2005) Marginal and internal fit of all-ceramic CAD/CAM crown-copings on chamfer preparations. J Oral Rehabil 32(6):441–447. doi:10.1111/j.1365-2842.2005.01446.x
Holmes JR, Bayne SC, Holland GA, Sulik WD (1989) Considerations in measurement of marginal fit. J Prosthet Dent 62(4):405–408
Schaerer P, Sato T, Wohlwend A (1988) A comparison of the marginal fit of three cast ceramic crown systems. J Prosthet Dent 59(5):534–542
Felton DA, Kanoy BE, Bayne SC, Wirthman GP (1991) Effect of in vivo crown margin discrepancies on periodontal health. J Prosthet Dent 65(3):357–364
Sorensen JA (1989) A rationale for comparison of plaque-retaining properties of crown systems. J Prosthet Dent 62(3):264–269
Sorensen SE, Larsen IB, Jorgensen KD (1986) Gingival and alveolar bone reaction to marginal fit of subgingival crown margins. Scand J Dent Res 94(2):109–114
Tuntiprawon M, Wilson PR (1995) The effect of cement thickness on the fracture strength of all-ceramic crowns. Aust Dent J 40(1):17–21
Beuer F, Neumeier P, Naumann M (2009) Marginal fit of 14-unit zirconia fixed dental prosthesis retainers. J Oral Rehabil 36(2):142–149. doi:10.1111/j.1365-2842.2008.01908.x
Beuer F, Korczynski N, Rezac A, Naumann M, Gernet W, Sorensen JA (2010) Marginal and internal fit of zirconia based fixed dental protheses fabricated with different concepts. Clin Cosmet Investig Dent 2:5–11
Beuer F, Naumann M, Gernet W, Sorensen JA (2009) Precision of fit: zirconia three-unit fixed dental prostheses. Clinical oral investigations 13(3):343–349. doi:10.1007/s00784-008-0224-6
Boening KW, Wolf BH, Schmidt AE, Kastner K, Walter MH (2000) Clinical fit of Procera AllCeram crowns. J Prosthet Dent 84(4):419–424. doi:10.1067/mpr.2000.109125
Molin M, Karlsson S (1993) The fit of gold inlays and three ceramic inlay systems. A clinical and in vitro study. Acta Odontol Scand 51(4):201–206
Beuer F, Aggstaller H, Edelhoff D, Gernet W, Sorensen J (2009) Marginal and internal fits of fixed dental prostheses zirconia retainers. Dental materials: official publication of the Academy of Dental Materials 25(1):94–102. doi:10.1016/j.dental.2008.04.018
Tinschert J, Natt G, Mautsch W, Spiekermann H, Anusavice KJ (2001) Marginal fit of alumina- and zirconia-based fixed partial dentures produced by a CAD/CAM system. Oper Dent 26(4):367–374
Coli P, Karlsson S (2004) Precision of a CAD/CAM technique for the production of zirconium dioxide copings. Int J Prosthodont 17(5):577–580
Rekow ED, Harsono M, Janal M, Thompson VP, Zhang G (2006) Factorial analysis of variables influencing stress in all-ceramic crowns. Dental materials: official publication of the Academy of Dental Materials 22(2):125–132. doi:10.1016/j.dental.2005.04.010
Rekow D, Thompson VP (2005) Near-surface damage—a persistent problem in crowns obtained by computer-aided design and manufacturing. Proc Inst Mech Eng H J Eng Med 219(4):233–243
Acknowledgements
DeguDent and Amann Girrbach supported this study with materials. The authors would like to thank the laboratory staff of the prosthodontic department of Munich Dental School for their support, especially to Josef Schweiger and John Meinen.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
No funding was obtained for this study.
Ethical approval
This article does not contain any studies with animals or human participants performed by any of the authors.
Informed consent
For this kind of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Schönberger, J., Erdelt, KJ., Bäumer, D. et al. Marginal and internal fit of posterior three-unit fixed zirconia dental prostheses fabricated with two different CAD/CAM systems and materials. Clin Oral Invest 21, 2629–2635 (2017). https://doi.org/10.1007/s00784-017-2064-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-017-2064-8