Abstract
Objectives
The purpose of this study was to evaluate the clinical performance of removable dental prostheses (RDP) supported by either electroplated (EP-RDP) or cast (C-RDP) double crowns.
Material and methods
Fifty-four participants received a total of 60 RDP. Two hundred and seventeen abutment teeth were provided with double crowns. The participants were randomly assigned to two groups (EP-RDP or C-RDP). Re-evaluations took place after 6 months and then once a year up to 6 years. Primary endpoint was survival time for RDP and abutment teeth; secondary endpoints were failure of facing, decementation of primary crown, and post-prosthetic endodontic treatment. T, U, and chi-squared tests were used to assess the homogeneity of the EP-RDP and C-RDP groups. Survival differences were analyzed with log-rank tests and Cox regression models; secondary endpoints were assessed by the use of logistic regression.
Results
Six-year survival was 77 % for EP-RDP and 97 % for C-RDP. Cumulative survival of abutment teeth was 85 % for EP-RDP and 91 % for C-RDP; differences between survivals in the two groups did not reach statistical significance. Survival of abutment teeth depended on tooth vitality. Failures of facings, decementations, or post-prosthetic endodontic treatments were not different between groups.
Conclusions
To identify possible differences between different double crown systems, longer follow-up periods and/or larger numbers of patients are needed.
Clinical relevance
Survival of teeth supporting double crown-retained RDP is affected by their vitality. Clinical performance was acceptable for both RDP supported by electroplated or cast double crowns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Double crown-retained removable dental prostheses (RDP) have been clinically proven to be a successful treatment option in the prosthetic dentistry [1–16]. The versatility and advantages of double crown retainers for RDP have recently been emphasized once again [17]. In spite of the increasing use of dental implants, double crown-retained RDP are still a reasonable alternative to fixed dental prostheses for the rehabilitation of partially edentulous patients, particularly with regard to combined tooth- and implant-borne RDP.
The manufacture of double crowns by casting requires highly skilled dental technicians, however. In the 1990s, the fabrication of electroplated double crown systems, with cast primary crowns and electroplated secondary crowns, was described for the first time [18, 19]. In 2000, Weigl et al. reported on the clinical use of double crown-retained RDP with all-ceramic primary crowns in combination with secondary crowns made of electroplated gold [20, 21].
The fabrication of electroplated secondary crowns, a largely automated process (so-called electroplating or electroforming), does not require special technical skills and ensures optimum fit between primary and secondary crowns. In contrast with cast double crowns, electroplated double crown systems depend, predominantly, on the principle of hydraulic adhesion resulting from the film of saliva between primary and secondary crowns and seem to have favorable tribological properties [20, 22]. Recent in vitro studies have dealt with retentive force measurements and the wear behavior of electroplated double crown systems [23–26]. One study reported slightly lower retentive forces for electroplated double crowns than for cast double crowns [26], whereas another study found the opposite [24]. Factors affecting retentive force measured in vivo were the material of the primary crowns, abutment height, the taper, and the number of wear cycles [23–26].
Numerous reports are available on the survival of RDP, survival of abutment teeth, and complications of cast double crown-retained RDP [1–16]. The current dental literature, however, does not provide sufficient information about the clinical performance of RDP retained by electroplated double crown systems. Randomized clinical trials are lacking.
The objectives of this prospective, randomized clinical trial were to quantify and compare the clinical performance of cast double crown-retained RDP (C-RDP) and electroplated double crown-retained RDP (EP-RDP). We investigated the survival of the RDP, survival of the abutment teeth, and common technical and biological complications in both groups after 6 years of clinical use. We have already reported the oral health-related quality of life (OHRQoL) of the participants during the first year after treatment; we found that OHRQoL was not significantly different [27]. The clinical performance of these prostheses after being worn for 3 years was also found to be comparable [28].
Materials and methods
Fifty-four participants requiring RDP with at least two, up to a maximum of six, abutment teeth provided with double crowns were included in the study. All participants gave informed consent. The university’s review board approved the study (ethical approval no. 074/2003). Patients’ ages ranged from 38 to 80 years (mean age 64, SD = 9); 34 (63.3 %) of the patients were male. The participants were randomly assigned to two study groups (C-RDP and EP-RDP). Six participants received RDP in both jaws, which resulted in a total of 60 RDP (n = 30 RDP in each group). Two dental laboratories fabricated the prostheses (n = 30 prostheses and n = 15 for both C-RDP and EP-RDP in each laboratory) by dental technicians with more than 5 years of experience in both of the fabrication techniques used in the study. Two hundred and seventeen abutment teeth were provided with double crowns (135 anterior teeth (incisors and canines), 58 premolars, and 24 molars).
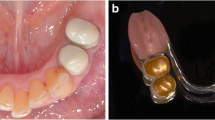
Manufacturing of the two different double crown systems has already been explained in detail in a previous paper [28]. Therefore, only the most important aspects of the study design should be outlined. In the C-RDP group, the primary and secondary crowns were made of precious metal alloy (Bio Portadur; Wieland, Pforzheim, Germany); they were conventionally cast by the use of the lost wax technique and had a conical design with 6° milling. In the EP-RDP group, the primary crowns were also fabricated by casting with precious metal alloy (Bio Portadur; Wieland, Pforzheim, Germany), but in contrast, the secondary crowns were made by electroplating with 0° milling (99.9 % gold, Goldbath 6607 AGC; Wieland, Pforzheim, Germany). With a composite resin-luting agent (AGC Cem; Wieland, Pforzheim, Germany), the electroplated secondary crowns were luted to a CoCrMo framework (Remanium GM 800; Dentaurum, Ispringen, Germany). In both groups, the buccal and/or occlusal surfaces of the secondary crowns were faced with veneering composites (Sinfony; 3M ESPE, Signum; Heraeus Kulzer, Hanau, Germany) by the use of the Rocatec universal bonding system (3M ESPE, Seefeld, Germany). In both groups, the primary crowns were luted to the abutment teeth by the use of a glass ionomer-luting cement (Ketac Cem Aplicap; 3M ESPE). Figure 1 illustrates the two different double crown systems by a schematic diagram.
Five calibrated dentists performed clinical evaluations by the use of a written case record file according to the following criteria: (1) failure (=renewal) or survival of RDP, (2) failure (=extraction) or survival of abutment teeth, (3) loss or fracture of facing with a need for repair, (4) loss of cementation of primary crown, or (5) need for post-prosthetic endodontic treatment. Baseline measurement was 1 week after incorporation of the RDP; this was followed by re-evaluation after 6, 12, 24, 36, 48, 60, and 72 months (6 years).
Statistical analysis
T, U, and chi-squared tests were used to assess the significance of differences between the characteristics of patients in the EP-RDP and C-RDP groups. Survival differences were investigated by the use of log-rank tests and Cox proportional regression models; secondary data were assessed by logistic regression. Calculations were performed by the use of SAS version 9.2.
Results
Table 1 shows some characteristics of patients and RDP in the two study groups. The EP-RDP and C-RDP groups were similar regarding age, restored arch, and number, vitality, and mobility of abutment teeth. The percentage of male patients was 77 % in the EP-RDP and 50 % in the C-RDP group (p = 0.03). The position of abutment teeth, i.e., the proportion of anterior teeth, premolars, and molars, and the mean values of maximal probing depth differed significantly between the two study groups (p < 0.001, Table 1).
At 6-year recall (72 months ± 4 weeks), 32 of 54 participants and 34 of 60 RDP were re-evaluated. Eleven participants (with 14 RDP) were lost to follow-up, three participants (with four RDP) had died, and eight RDP of eight participants failed.
Over the whole 72-month period, eight RDP failed, so the overall cumulative survival was 87 %. In the EP-RDP group, 7 of 30 RDP (23 %) failed and had to be replaced. In one case, technical defects (loss of retention and loss of facings) were the reason for replacement. The other EP-RDP had to be replaced because of loss of the abutment teeth, mostly because of caries and/or periodontal problems. Only one failure (3 %) occurred in the C-RDP group because caries resulted in tooth loss. The resulting cumulative survival was 77 % for EP-RDP and 97 % for C-RDP; this difference was not statistically significant (p = 0.06, HR = 7.27, 95 % CI 0.89 to 59).
With regard to abutment teeth, median survival of extracted teeth was 39 months. In the EP-RDP group, 16 of 105 abutment teeth (15 %) were lost. The reasons were caries (n = 8), periodontal disease (n = 3), tooth fracture (n = 1), and trauma (n = 4). Ten of 112 teeth (9 %) had to be extracted in the C-RDP group because of caries (n = 7), periodontal disease (n = 1), and endodontic disease (n = 2). The resulting cumulative survival of abutment teeth after 72 months was 85 % in the EP-RDP group and 91 % in the C-RDP group. This difference was not statistically significant (p = 0.16, HR = 1.77, 95 % CI 0.80 to 3.89). The risk of failure was higher for nonvital abutments than for vital teeth (p = 0.04, HR = 2.29, 95 % CI 1.05 to 4.98). Age or gender of patient and the number, arch, position, and mobility of abutment teeth had no effect on survival (Table 2, with probability values from multiple Cox regression, and Figs. 2 and 3 with probability values from log-rank tests).
Sixty-three (29 %) losses or fractures of facings needed repair. The number of veneer failures was almost the same in the EP-RDP (n = 33) and C-RDP (n = 30) groups (p = 0.45, OR = 1.25, 95 % CI 0.70 to 2.25). The number of abutment teeth in the RDP significantly increased the risk of veneer failure (p < 0.001, OR = 1.63, 95 % CI 1.24 to 2.13, Table 3).
In both groups, 10 decementations of primary crowns occurred (overall incidence 9 %). Loss of cementation was not different between the study groups (p = 0.88, OR = 1.07, 95 % CI 0.43 to 2.69, Table 4). All primary crowns that were lost could be luted again. Other investigated patient and abutment tooth characteristics had no effect on decementation.
Eighteen abutment teeth (11 %) needed post-prosthetic endodontic treatment: 10 in the EP-RDP group and 8 in the C-RDP group. The root canal filling of one nonvital abutment tooth had to be revised. The study group had no effect on the incidence of post-prosthetic endodontic treatment (p = 0.53, OR = 1.37, 95 % CI 0.52 to 3.61, Table 5).
Discussion
Overall, the 6-year cumulative survival of RDP (87 %) in the present study is in good agreement with literature data. One recently published review found that survival of tooth-supported double crown-retained prostheses was between 67 and 99 % after 6 to 10 years of observation [16]. Regarding the two study groups, cumulative survival was 77 % for EP-RDP and 97 % for C-RDP. Although the difference between the two groups did not reach the 5 % level of statistical significance, these preliminary findings may reflect better clinical performance of C-RDP. It was not, unfortunately, possible to calculate the size of the treatment groups during study planning because no clinical data were available for electroplated double crowns. Power analysis was therefore performed subsequently. Assuming that cumulative survival in the two groups investigated (77 and 97 %) also applies to other studies, 43 independent prostheses should be followed up per group for at least 6 years to validate these findings with 80 % statistical power (type I error probability 5 %, uncorrected chi-squared statistic).
It is important to mention here that the present survival rates must be interpreted with caution because only one RDP failure was directly correlated with the double crowns. All other failures were caused by loss of abutment teeth because of caries, periodontitis, fracture, and trauma, biological failures which possibly were not related to abutment type. Furthermore, it should be remembered that replacement of RDP after abutment tooth loss is always a joint—dentist and patient—decision on a case-by-case basis, according to the number and condition of the residual dentition.
Estimates of cumulative survival of abutment teeth in this study are also very similar to those in previous reports [15, 16]. In the two reviews already cited, survival of teeth supporting double crown-retained RDP ranged from 61 to 95 % after 4 to 10 years of observation [15] and from 83 to 97 % after an observation period of 3 to 6 years [16]. Nearly all of the factors used to interpret the survival of RDP apply to the abutment teeth also. Previous long-term studies [4, 8, 9, 14] and the results of this study showed that abutment tooth loss was not correlated with the type of abutment; the most common reasons for tooth loss were biological complications, for example periodontal disease, caries, and tooth fracture. The lower cumulative survival of abutment teeth in the EP-RDP group (85 %) than in the C-RDP group (91 %)—without reaching statistical significance—may be correlated with the larger number of males in the EP-RDP group. At least two previous studies have reported lower survival of teeth with double crowns in male patients [10, 14], although in our study, gender did not affect survival.
In agreement with previous reports [10, 12, 14, 29, 30], the significant effect of tooth vitality on survival of abutment teeth for double crown-retained RDP was, again, confirmed in our investigation. For example, probability of survival of 94 % for vital abutment teeth and 80 % for nonvital abutment teeth supporting removable partial dental prostheses, after a mean observation period of 6 years, has previously been reported [12]. It has, furthermore, been shown that failure risk is larger for posterior than for anterior teeth supporting double crown-retained RDP [12]. We have already reported the results for this group of patients after observation for 3 years. In this previous report, we found the risk of failure to be higher for premolars and molars than for anterior teeth [28]; this difference was not replicated after 6 years of follow-up, however.
In this study, 29 % of the double crowns needed at least one repair of the facing; the type of double crown had no effect on failure of facings. This finding is within the ranges reported in the literature [2, 3, 5, 11], which show that facings are among the main weaknesses of double crown-retained RDP.
Another frequent technical complication described in the literature is decementation of the primary crowns of double crown-retained RDP [3, 8, 11, 13, 16]. Previous clinical investigations have reported decementations between 11 and 26 % [1, 3, 11, 13, 14]. All in all, in the present study, loss of cementation during 6 years of observation was rare and somewhat lower than in the literature; no significant difference between C-RDP and EP-RDP was observed. This result may be caused by the tooth preparation technique and the consequent use of glass ionomer cement for luting the primary crowns. Another factor affecting loss of cementation may be the retention forces between the primary and secondary crowns. In clinical use, retentive forces of manually fabricated, cast double crowns are somewhat unpredictable [20, 21]; increased retention may result in a higher rate of decementation of primary crowns. With electroplated double crowns, on the other hand, ease of handling without unpredictable increase or decrease in retentive forces could be expected [20, 21]. Clinical experiences obtained from the present study confirm the aforementioned statements.
In this study, 11 % of the vital abutment teeth needed post-prosthetic endodontic treatment during the observation period of 6 years; the type of double crown had no effect. This finding is in good agreement with literature data reporting a risk of post-prosthetic endodontic treatment of 6 % after 5 years [6], 5–6 % after 4 years [8], and 82–87 % after 10 years [13]. Endodontic treatment of abutment teeth may become necessary if tooth preparation causes pulp damages. According to Murray et al., the remaining dentin thickness of 0.5 mm or greater is necessary to avoid pulp injury [31]. Removal of enamel and dentin during tooth preparation should, therefore, be as low as possible. Both double crown systems used in the present study need comparable space, and removal of enamel and dentin is nearly equal. Considering the risk of pulp damage caused by tooth preparation, the use of clasp-retained RDP could be a reasonable alternative to double crown-retained RDP. Natural appearance and similarity to natural teeth are, however, important reasons for choosing or refusing prosthodontic treatment [32]; for this reason, double crowns with facings are advantageous for patients asking for RDP.
The strengths of this study are the prospective, randomized design with two rather homogenous study groups; the fact that only two dental laboratories, with experienced and highly skilled dental technicians, were involved in prosthesis fabrication; and that all clinical evaluations were performed by calibrated dentists only. The weaknesses are the relatively small number of participants and events, which limited the statistical power, and dropout of 26 % (participants) and 30 % (prostheses) after 6 years, although these were taken into account in the statistical analysis. Furthermore, it should be noted that it is nearly impossible to devise a truly comparative clinical study for these two double crown systems because many other factors (tooth position, tooth conditions, length of prostheses saddles) are highly variable.
It should be taken into account that the treatments were performed by several dentists with different operating experiences. Therefore, bias of the results cannot be excluded, and the results should be interpreted with caution, bearing in mind that nonsignificant results do not imply the absence of an effect. Multicenter studies which involve more participants and longer follow-up periods may be reasonable in future investigations. Patients from dental offices should be included to avoid selection bias. Longer follow-up observation of the patients will show if the clinical performance of C-RDP and EP-RDP remains similar over time.
Conclusions
Survival of teeth supporting double crown-retained RDP is affected by their vitality. Clinical performance is acceptable for both RDP supported by electroplated or cast double crowns; RDP retained by electroplated double crowns tend to result in lower survival rates. Longer follow-up periods and larger numbers of patients are needed to identify possible differences between different double crown systems.
References
Bergman B, Ericson A, Molin M (1996) Long-term clinical results after treatment with conical crown-retained dentures. Int J Prosthodont 9:533–538
Igarashi Y, Goto T (1997) Ten-year follow-up study of conical crown-retained dentures. Int J Prosthodont 10:149–155
Behr M, Hofmann E, Rosentritt M, Lang R, Handel G (2000) Technical failure rates of double crown-retained removable partial dentures. Clin Oral Investig 4:87–90
Eisenburger M, Gray G, Tschernitschek H (2000) Long-term results of telescopic crown retained dentures—a retrospective study. Eur J Prosthodont Restor Dent 8:87–91
Wagner B, Kern M (2000) Clinical evaluation of removable partial dentures 10 years after insertion: success rates, hygienic problems, and technical failures. Clin Oral Investig 4:74–80
Wenz HJ, Hertrampf K, Lehmann KM (2001) Clinical longevity of removable partial dentures retained by telescopic crowns: outcome of the double crown with clearance fit. Int J Prosthodont 14:207–213
Saito M, Notani K, Miura Y, Kawasaki T (2002) Complications and failures in removable partial dentures: a clinical evaluation. J Oral Rehabil 29:627–633
Widbom T, Lofquist L, Widbom C, Soderfeldt B, Kronstrom M (2004) Tooth-supported telescopic crown-retained dentures: an up to 9-year retrospective clinical follow-up study. Int J Prosthodont 17:29–34
Piwowarczyk A, Köhler KC, Bender R, Büchler A, Lauer HC, Ottl P (2007) Prognosis for abutment teeth of removable dentures: a retrospective study. J Prosthodont 16:377–382
Rehmann P, Weber A, Wöstmann B, Ferger P (2007) Clinical evaluation of teeth fitted with telescope crowns for retaining a partial denture. Dtsch Zahnärztl Z 62:99–103
Wöstmann B, Balkenhol M, Weber A, Ferger P, Rehmann P (2007) Long-term analysis of telescopic crown retained removable partial dentures: survival and need for maintenance. J Dent 35:939–945
Dittmann B, Rammelsberg P (2008) Survival of abutment teeth used for telescopic abutment retainers in removable partial dentures. Int J Prosthodont 21:319–321
Behr M, Kolbeck C, Lang R, Hahnel S, Dirschl L, Handel G (2009) Clinical performance of cements as luting agents for telescopic double crown-retained removable partial and complete overdentures. Int J Prosthodont 22:479–487
Szentpétery V, Lautenschläger C, Setz JM (2010) Longevity of frictional telescopic crowns in the severely reduced dentition: 3-year results of a longitudinal prospective clinical study. Quintessence Int 41:749–758
Koller B, Att W, Strub JR (2011) Survival rates of teeth, implants, and double crown-retained removable dental prostheses: a systematic literature review. Int J Prosthodont 24:109–117
Verma R, Joda T, Brägger U, Wittneben JG (2013) A systematic review of the clinical performance of tooth-retained and implant-retained double crown prostheses with a follow-up of ≥3 years. J Prosthodont 22:2–12
Breitman JB, Nakamura S, Freedman AL, Yalisove IL (2012) Telescopic retainers: an old or new solution? A second chance to have normal dental function. J Prosthodont 21:79–83
Diedrichs G, Rosenhain P (1991) Galvanoteleskope in der direkten Technik. Quintessenz 42:49–56 (in German)
Wirz J, Jäger K (1998) Galvanoteleskope – präzise, einfach und klinisch bewährt. Quintessenz 49:283–292 (in German)
Weigl P, Hahn L, Lauer HC (2000) Advanced biomaterials used for a new telescopic retainer for removable dentures: ceramic vs. electroplated gold copings: part I. In vitro tribology effects. J Biomed Mater Res (Appl Biomater) 53:320–336
Weigl P, Lauer HC (2000) Advanced biomaterials used for a new telescopic retainer for removable dentures: ceramic vs. electroplated gold copings: part II. Clinical effects. J Biomed Mater Res (Appl Biomater) 53:337–347
Rößler J, Göbel R, Welker D (2005) Der haftmechanismus von galvano-doppelkronen. ZWR 10:437–442 (in German)
Beuer F, Edelhoff D, Gernet W, Naumann M (2010) Parameters affecting retentive force of electroformed double-crown systems. Clin Oral Investig 14:129–135
Bayer S, Kraus D, Keilig L, Gölz L, Stark H, Enkling N (2012) Wear of double crown systems: electroplated vs. casted female part. J Appl Oral Sci 20:384–391
Gurbulak AG, Kilic K, Eroğlu Z, Gercekcioglu E, Kesim B (2013) Evaluation of the retention force of double conical crowns used in combination with a galvanoforming and casting fabrication technique. J Prosthodont 22:63–68
Engels J, Schubert O, Güth JF, Hoffmann M, Jauernig C, Erdelt K, Stimmelmayr M, Beuer F (2013) Wear behavior of different double-crown systems. Clin Oral Investig 17:503–510
Grossmann AC, Hassel AJ, Schilling O, Lehmann F, Koob A, Rammelsberg P (2007) Treatment with double crown-retained removable partial dentures and oral health-related quality of life in middle- and high-aged patients. Int J Prosthodont 20:576–578
Stober T, Bermejo JL, Beck-Mussoter J, Seche AC, Lehmann F, Koob J, Rammelsberg P (2012) Clinical performance of conical and electroplated telescopic double crown-retained partial dentures: a randomized clinical study. Int J Prosthodont 25:209–216
Molin M, Bergman B, Ericson A (1993) A clinical evaluation of conical crown retained dentures. J Prosthet Dent 70:251–256
Wegner PK, Freitag S, Kern M (2006) Survival rate of endodontically treated teeth with posts after prosthetic restoration. J Endod 32:928–931
Murray PE, Smith AJ, Windsor LJ, Mjör IA (2003) Remaining dentine thickness and human pulp responses. Int Endod J 36:33–43
Leles CR, Martins RR, Silva ET, Nunes MF (2009) Discriminant analysis of patients’ reasons for choosing or refusing treatments for partial edentulism. J Oral Rehabil 36:909–915
Acknowledgments
We thank all the patients in the study, especially for their high attendance during the recalls. We thank Wieland Pforzheim, Germany, for financial support of this study. The resources were used to compensate the patients for their additional effort attending recalls. The authors have no financially beneficial arrangements with Wieland. We also thank Ian Davies, copy editor, for the English language revision.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ethical standards
The study was reviewed and approved by the university’s review board (ethical approval no. 074/2003) and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants gave their informed consent prior to their inclusion in the study.
Rights and permissions
About this article
Cite this article
Stober, T., Bermejo, J.L., Séché, AC. et al. Electroplated and cast double crown-retained removable dental prostheses: 6-year results from a randomized clinical trial. Clin Oral Invest 19, 1129–1136 (2015). https://doi.org/10.1007/s00784-014-1335-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-014-1335-x