Abstract
Objectives
This prospective randomized clinical trial aimed to evaluate the long-term behavior of metal-free double crown retained dentures with secondary crowns and dental frameworks made of the fiber-reinforced composite Vectris© on all-ceramic primary crowns (IPS Empress 2©) over a period of up to 14 years and to subsequently evaluate patient satisfaction. For the control group, electroplated gold copings and metal frameworks were used.
Materials and methods
A total of 29 patients were treated with a total of 37 prostheses on 165 primary crowns. Of these 37 prostheses, 27 were allotted to the control group and 10 to the test group. The mean observation time was 91 ± 57 months; patient satisfaction surveys were conducted over 77 ± 59 months.
Results
Success rates in both groups were compared using Kaplan–Meier survival curves and log-rank test. Up to about 3 years, both types of prostheses exhibited similar success rates. Afterwards, a massive decrease in the Vectris© curve could be noted, whereas the metal curve dropped only slightly. This difference was also statistically significant (p = 0.032361). There was a comparable susceptibility to damages in both groups: 88.9 % (control) and 90 % (test), respectively, of the prostheses had to be repaired within the period of investigation (p = 0,121). Damages of the Vectris© secondary crowns could be detected significantly more often compared to the electroformed gold copings (p < 0.00005). Patient satisfaction with the restorations was comparably high in both groups.
Conclusion
Metal-free secondary crowns and denture frameworks made with the glass fiber-reinforced composite material Vectris© showed a lower survival rate than the electroplated gold copings and metal frameworks. Primary crowns made of IPS Empress 2© had insufficient stability. Exclusively high-strength zirconia ceramics should be recommended for this indication.
Clinical relevance
Both clinical and statistical data indicated the superiority of the restorations made with electroplated secondary crowns and metal framework. Therefore, the use of Vectris© cannot be recommended for the fabrication of double crown retained removable dentures as permanent restorations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
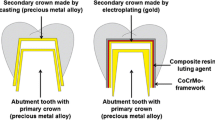
For decades, double crown retained removable dentures have been an approved method for clinical treatment of reduced residual dentition, combining the advantages of fixed with those of removable partial dentures [1–6]. Apart from enabling optimal hygiene, double crown retained removable dentures achieve a favorable axial load and suitable fitting of the abutment teeth. However, integrating dental implants into such a prosthetic reconstruction often leads to problems concerning the fitting precision of wide-span dental frameworks as material-related dimensional inaccuracies are unavoidable during impression and casting. Because of the rigid anchoring of osseointegrated implants, those changes cannot be compensated. Therefore, intraoral luting of the framework components may be useful to compensate the inaccuracy [7, 8]. For this purpose, the electroplated gold copings are joined intraorally with the tertiary structure. The long-term and reliable adhesion of this bonding has been shown in numerous clinical and in vitro studies [7, 9–13] (Fig. 1).
A major trend in dental therapy is the substitution of conventional substances, especially metallic, by metal-free, mostly ceramic, materials. In addition to the development and improvement of high-performance ceramics, this trend is due to the patients’ needs for optimal aesthetics as well as their concern about the biocompatibility of metallic alloys [14–16]. Regarding double crown retained dentures, usually primary and secondary crown and the framework of the prosthesis are made out of metallic materials. For the manufacturing of primary crowns, ceramic materials offer alternatives. Extensive clinical experience supports the suitability for this indication [7, 17–19].
The substitution of the secondary crown is more challenging. The precision and fit achieved during the production process of the electroformed crowns so far cannot be attained with metal-free materials. Ceramic materials show deficiencies in tensile strength as well as increased brittleness. Composite materials [20] or fiber-reinforced composites like Vectris© (Fa. Ivoclar Vivadent, Liechtenstein) seem to be more appropriate to serve this purpose.
The framework constitutes a further metallic component in dentures. An alternative material must exhibit sufficient stiffness and torsional stability with low weight and small dimensions. For this purpose, fiber composites may also be suitable [21]. Originally, these materials were considered appropriate for single crowns and three-unit bridges. Clinical trials regarding the material properties and clinical application showed positive or moderate results [21–25]. Mainly, two problems were reported when using this material for fixed removable dentures: fracture of facing and framework fracture [22, 26, 27]. The risk for fracture is correlated with the thinness of the material; increasing thickness leads to a better load-bearing capacity [28]. When Vectris© is used as a framework in a removable partial denture, its diameter can reach higher values compared with the framework of a fixed partial denture. Furthermore, problems with the facing will not occur. Taking into account these considerations, Vectris© might be a suitable material to replace the metal in a double crown retained removable denture.
The aim of this prospective clinical trial was to investigate the long-term clinical behavior of all-ceramic primary crowns made out of glass ceramic (IPS Empress 2©), combined either with electroplated gold copings and a metallic framework or with metal-free secondary crowns and a framework made of glass fiber composite (Vectris©). Furthermore, patient satisfaction with these restorations was evaluated.
The null hypothesis was that the long-term performance of the metal-free removable dentures made out of Vectris© is comparable to the results for dentures with electroplated secondary crowns and a metallic framework.
Materials and methods
In the present prospective clinical trial, 29 patients (12 female, 17 male) were supplied with intraorally assembled conical crown retained dentures between June 1999 and December 2001 at the department of Prosthodontics, University Dental Clinic (Carolinum) at J.W. Goethe University, Frankfurt am Main. A positive vote of the Ethics Committee to conduct the trial had been granted in 1999. Each patient received an oral and written explanation of the trial protocol, and an informed consent form was obtained.
All patients had to fulfill the following inclusion criteria: indication for the fabrication/use of double crown retained denture, minimum age 18, maximum 75 years, good oral hygiene, and a healthy/treated periodontal situation. The respective abutments had to be clinically and radiologically free of pathological findings. Pregnant and lactating women were excluded from the trial.
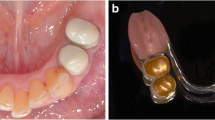
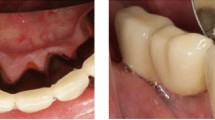
No difference was made regarding the use of teeth or implants as abutments for the primary crowns. A randomized distribution of the patients into two groups was carried out using a computer-generated randomization list (simple, unrestricted randomization) [29–31].This procedure allows complete randomness of the assignment of a subject to a particular group. While the test group received metal-free dentures with secondary crowns and a framework made of Vectris©, the control group received electroplated gold copings and a metal framework (Figs. 2, 3 and 4). Originally, this investigation was designed with a projected duration of 5 years. As no relevant clinical data about Vectris© used for this indication was available, a sample size estimation could not be conducted. In order to further check the long-term performance of the materials used, it was decided to continue the trial. Follow-up examinations were conducted until May 2014.
A total of 37 prostheses, 27 with metal and 10 with Vectris© framework, on 165 ceramic primary crowns were fabricated. The production and the incorporation of the prostheses were performed by different experienced clinicians, who followed the treatment protocol by Weigl [8]. At the beginning of the treatment, after the integration of the prosthesis and during the follow-up visits, clinical findings were collected, and patient satisfaction with the respective dentures was evaluated.
Clinical follow-up examinations were done by two practitioners familiar with the trial protocol. The examiners had not been involved in patient treatment within the trial. To avoid person-specific bias or measurement errors, a standardized calibration was conducted at the beginning.
Initially and every 6 months, the primary crowns, the secondary structures, and the prostheses were comprehensively examined to detect damages like chipping, hairline cracks, wear, loss of facings, abutment loosening, fractures (framework, primary crowns), loss of retention, or necessity of relining. Patient satisfaction was evaluated using a questionnaire. The patient satisfaction review comprised aspects as to general satisfaction, denture retention, wearing comfort, chewing ability, and aesthetics using Likert scales with questions scored by a 5-point scale (strongly agree = 5 point, agree = 4 point, neutral = 3 point, disagree = 2 point, strongly disagree = 1 point) and dichotomous questions (yes/no). In addition, a photographic documentation of the situation was carried out at the beginning of treatment, after the incorporation, and every 12 months thereafter.
Repair and maintenance measures, such as facing repairs or reattachment of crowns, were carried out as soon as damages were identified or the patient complained about them and were recorded in the trial documents. The procedure was similar with aftercare treatments like hygiene instructions or denture adjustments. More extensive damages were also documented photographically, especially if they occurred at the primary or secondary crowns.
A prosthesis was classified as failure if it could not be further used, for example, due to massive damage of one of its parts, loss of the supporting teeth, or retention. In these cases, new dentures were made, and the patient was afterwards excluded.
Furthermore, all changes and damages of the primary crowns were recorded and analyzed in detail. In particular, it was examined whether parameters such as type, number, vitality, and topography of the abutments and the type of opposing dentition (fixed, removable partial or complete denture) played a role in the frequency of events concerning the primary crown.
The analysis was performed using the STATISTICA software package (StatSoft, Inc. STATISTICA for Windows [Computer Program Manual, Version 7.1]. Self Publishing: Tulsa, OK, USA, 2005). For the determined continuous quantitative data, the mean value was calculated; for the discrete qualitative ordinal data, the median was determined. Depending on the nature and specificity of the data to be examined, Mann–Whitney U-test or Fisher’s exact test was used. Survival analyses were performed using Kaplan–Meier method and log-rank test, which is suitable for comparison of survival times and also applicable to censored data. A p value less than 0.05 was considered to be statistically significant.
Results
A total of 37 prostheses, 27 with metal and 10 with Vectris© framework on 165 ceramic primary crowns were fabricated. The patients had a mean age of 60 ± 8.4 years at the beginning of the trial. Each prosthesis was based on an average of 4.5 ± 1.6 primary crowns, with a minimum of 1 and a maximum of 7. The clinical follow-up of patients lasted on average about 91 ± 57 months (minimum 16, maximum 173 months); surveys on patient satisfaction were conducted 77 ± 59 months (min. 15, max. 173 months). In 17 cases (control group 15, test group 2), the examined dentures were located in the upper jaw and in 20 cases (control group 12, test group 8) in the lower jaw. The comparison of the two trial groups showed no significant differences related to parameters such as patient age, sex, number of incorporated primary crowns, abutment distribution, or supply situation of the opposing arch at the time of treatment initiation. Three patients (control group—two, test group—one) were deceased during the follow-up phase. In these cases, follow-up sessions were terminated, and patients were censored. Four further patients (control group—three, test group—one) did not complete all follow-ups of the initial 5-year period and were also censored. During the second phase of the trial (from 60 up to 173 month), further nine patients (control group—seven, test group—two) had to be considered dropouts as they stopped coming to the follow-up sessions for reasons unexplained. These patients were likewise censored. Failure of restoration was determined in a total of 11 cases (29.7 %) (control group—six, test group—five) as further use of the prostheses was no longer possible. Failure was due to the following reasons: abutment loss in three cases, lack of retention in six cases, and framework fracture of the prosthesis in two cases (Figs. 5 and 6). The graphical representation of the prosthetic success of both groups showed that, up to a period of less than 3 years, both types of prosthesis exhibited similar success rates. After this period, however, a massive decrease in the Vectris© curve could be noted, whereas the metal curve dropped only slightly. This difference was statistically significant (log-rank test, p = 0.032361) (Fig. 7). Overall, a great need for repairs of all incorporated prostheses was found: 88.9 % (control) and 90 % (test), respectively, of the prostheses had to be repaired (Mann–Whitney U-test, p = 0,121). Facing repairs and relines were the most common corrective measures (respectively 37.8 % of all repairs). With increasing duration (from approximately 18 months), prosthesis with metal secondary crowns showed benefits in terms of the need for repairs (Fig. 8), but this difference was not statistically significant (log-rank test, p = 0.256379). The long-term clinical behavior of the secondary structures was of particular interest. Damage in this area could be detected in a total of 14 secondary crowns (8.5 %), four in the control group and ten in the test group. Therefore, the risk for damage of secondary structures was significantly higher in the Vectris© group (Fisher's exact test, p < 0.00005). The damages in the electroplated secondary crowns concerned deformations of the gold template. However, only one of the four secondary crowns in question had to be renewed. In the Vectris© templates, signs of wear were detected in five cases, chipping or fracture of the material occurred four times, and one hairline crack was found. Only six of the damaged structures had to be renewed (Figs. 9 and 10). With regard to the two types of dentures, significant differences could be observed as well. In five out of ten Vectris© prostheses, damages could be found at the secondary structure, whereas in the control group, only three patients exhibited detectable damage (Fisher's exact test, p = 0.021; Fig. 11).
Overall, 165 abutments were reviewed in the trial, 128 in the control group, and 37 in the study group. More comprehensive information is shown in Table 1.
A total of 77 (46.7 %) were natural teeth, and 88 (53.3 %) were dental implants. Among the natural teeth, 14 (18.2 %) had already received an endodontic treatment. A total of 86 abutments (52.1 %) were located in the upper jaw, while 79 (47.9 %) were situated in the lower jaw. A total of 72 teeth or implants, representing 43.6 %, were in terminal position. The most common abutment region was the canine region in the maxilla or mandible with a total of 58 teeth or implants (35.2 %). In 19 abutments (control group—13, test group—6), damages of the primary crown occurred. This included, for example, transverse fractures, cracks, or chipping of the ceramic (Figs. 12 and 13). A total of 12 primary crowns (control group—11, test group—1) had to be replaced. Between the two groups, there was no significant difference in the incidence of damage or renewal. A total of 11 abutments (control group—nine, test group—two) were completely lost (Figs. 14 and 15).
The risk of tooth loss was not significantly higher than the risk of implant loss (Fisher's exact test, p = 0.35556). A total of 18 primary crowns (control group—14, test group—4) had to be reattached during use, corresponding to 10.9 % of all primary crowns. Of these crowns, 11 (control group—ten, test group—one) were located on teeth, and seven (control group—four, test group—three) on implants. No significant difference was found regarding the risk of detaching for natural abutments or implants (Fisher's exact test, p = 0.2184). Overall, however, a significantly higher rate of complications for natural teeth compared with implants was identified (Fisher's exact test, p = 0.01879). This was caused by the higher number of tooth fractures (11 of 77 abutments, 14.29 %; control group—ten, test group—one) and the low number of implant abutment fractures (1 of 88 implants, 1.14 %; control group—one, test group—zero). Statistically significant differences between the terminal and non-terminal abutments were not detectable (Fisher's exact test, all p > 0.05). However, the number of incidents in connection with terminal abutments was slightly higher than for non-terminal. The complication rate for root canal-treated teeth was higher than in non-endodontically treated abutments. Of 63 vital abutments, five (7.94 %) fractured, as did six of the 14 non-vital teeth (42.86 %) (Fisher's exact test, p = 0.00348). A separate analysis of these parameters by groups yielded no further results beyond the presented findings. Furthermore, it was examined whether a correlation could be detected between the number of abutments per prosthesis (n ≤ 4 abutments and n > 4 abutments) and patient satisfaction, adhesive force, wearing comfort, aesthetic evaluation of the denture, and chewing ability within a group and between both groups. However, no statistically significant differences (p > 0.05) were identified.
Before fabrication of the new dentures, 65 % of patients surveyed were dissatisfied with their current dental prosthesis. Specifically, chewing and wearing comfort as well as adhesion force was classified as insufficient. Patients’ evaluation of the old dentures is presented in Figs. 16 and 17. The new prosthesis received substantially better evaluations. At all points during the follow-up period, general satisfaction, adhesive force, wearing comfort, appearance, and ability to chew were rated highly positive and significantly better than the old denture (general satisfaction, p = 0.000076; retention, p = 0.0000002; wearing comfort, p = 0.0000002; appearance, p = 0.0018; chewing ability, p = 0.000003; Fisher's exact test). No significant differences were detected between the two groups (Fisher's exact test, all p > 0.05). The results of the patient satisfaction survey (collected after 5 years of use) are shown in Figs. 18, 19, 20, and 21.
At the time of the final examination (t = after at least 13 years of wear), all manufactured prostheses were evaluated as satisfactory in both groups. All patients stated that they would choose the denture again. Also, wearing comfort (control group, 4.33 ± 0.7; test group, 3.5 ± 0.7), appearance (control group, 4 ± 0.5; test group, 3.5 ± 0.7), and chewing ability (control group, 4.44 ± 0.53; test group, 3.5 ± 0.7) were favorably rated.
Discussion
Longevity as well as low repair susceptibility and a suitable strain on the integrated abutment teeth are essential criteria for the assessment of a dental prosthesis. In this clinical trial, a total of 11 prostheses (29.7 %) (control group—six, test group—five) were classified as failures after a mean observation period of more than 7.5 years, three due to abutment losses and eight caused by material-related deficiencies, such as retention loss and framework fracture. An analysis of the relevant literature shows failure rates for double crown retained dental prostheses between 0 and 39.6 % after several years of use [2, 4–6, 32–37]. However, the different follow-up periods have to be considered in the interpretation of these results. Overall, the detected failure rate of observed prostheses corresponds to published data. Improved prosthetic success could possibly be achieved by more rigorous abutment selection before fabricating the denture since more than a third of the observed failure was caused by the need for extraction of abutment teeth. When comparing the two groups regarding frequency of failure, clear results emerge. The survival analysis indicates an advantage for the control group after more than 3 years, which further increases after about 4 years, when it reaches statistical significance (p = 0.032361). Consequently, Vectris© prostheses cannot be recommended as a therapeutic agent since even in a period of less than 5 years, prostheses with electroplated secondary crowns show better results. Therefore, the null hypothesis has to be rejected.
Regarding the susceptibility to damage, this trial led to notable results. After less than 2 years, 60 % of the prostheses from the test group and nearly 50 % from the control group had already been repaired. A total of 88.9 % (control) and 90 % (test), respectively, of the prostheses had to be mended within the period of investigation. Often, damages could already be detected at the ceramic copings. Since damages such as chipping and hairline cracks do not occur in metal copings, this represents a serious disadvantage of the material used. Because of the high failure rate of ceramic primary crowns made of IPS Empress 2©, this glass ceramic cannot be recommended for the production of primary crowns. Stability is not sufficient for the present indication. The considerably higher durability of zirconia ceramics [38, 39] promises an improved success rate for all-ceramic conical crowns manufactured out of this material. Current in vitro and clinical studies with primary crowns made out of yttrium-stabilized zirconia ceramics show positive results [40–44], but long-term studies of large populations are necessary to confirm suitable clinical properties. Longer follow-up periods of larger collectives are published for double crown retained prostheses with metal copings. Incidence of repair is specified with values between 32.5 and 92.8 % [2–6, 36, 45–47]. These data confirm our results. An important aspect to examine was the damage frequency of the secondary crowns. Overall, in five out of ten Vectris© prostheses, damages could be found at the secondary structure, in all cases chipping, cracks, and/or wear of Vectris© material. In the control group, only three patients exhibited detectable damage. This difference was highly significant and supports the critical impression concerning the metal-free prostheses the examiners gained during the trial (Fisher's exact test, p = 0.021). Based on the total number of abutments, an even stronger result was achieved: 10 out of 37 Vectris© secondary crowns showed damage, while those changes were found in only 4 of 128 electroplated secondary structures (Fisher's exact test, p < 0.00005). In particular, the retention of the Vectris© dentures decreased significantly after a short time, which might be explained by a high wear of this material and/or the frequent damages of the secondary structures.
The number of patients who were subjectively satisfied with the new dentures was very high at any time of investigation and did not differ between the two groups (Fisher's exact test, p > 0.2). This overall positive assessment is particularly remarkable in light of the great need for repairs of the prostheses and the detected failure rate with need for renewing. The recognizable deficiencies–—especially for the Vectris© prostheses—apparently had no effect on the assessment of the patients who were at the beginning and end of the trial equally satisfied with their dentures. This is consistent with the clinical experience that the patients’ tolerance of defects can be very different and the subjective evaluation of the patient with regard to satisfaction, masticatory function, aesthetics, or stability may differ markedly from the review of an investigator. This phenomenon has been demonstrated in numerous studies as well, in which the patients’ assessment did not correlate with clinical success [36, 48–52]. The studies demonstrate the importance of subjective assessment in relation to the overall clinical success of a restoration. Related publications on patient satisfaction show that the supply of the reduced residual dentition using conical crown retained dentures is a therapeutic agent which leads to high patient satisfaction and acceptance [34–36, 53–56]. This finding is consistent with the results of the present trial, although detailed analysis and comparison are difficult because questionnaires are mostly used in a non-standardized form. With tools like OHIP, it is possible to assess the oral health-related quality of life in a standardized way [57–59]. OHIP offers a reliable and valid instrument for detailed measurement of the social impact of oral disorders. Therefore, the use of these validated questionnaires would be desirable in order to facilitate comparability with other studies.
The distribution of the patients into the groups was carried out using a simple, unrestricted randomization as this procedure allows complete randomness of the assignment to a particular group. No other method, irrespective of its complexity, surpasses the unpredictability and bias prevention of simple randomization [60]. This unpredictability, however, can also be a disadvantage. With small sample sizes, simple randomization (one-to-one allocation ratio) can yield disparate sample sizes in the groups [61, 62]. This effect could also be observed in our trial as the small total number of participants distributed using the described randomization procedure led to different group sizes. Originally, it was planned to include a larger number of patients to avoid the risk of recruiting an unequal number of participants among the groups, but recruitment was terminated after a period of 2.5 years. A further prolongation of the recruitment period might have resulted in problems regarding the homogeneity of the groups, the comparability within the groups, and the patients’ motivation. The equal distribution of implants and teeth to both groups was not regarded as necessary as recent publications show comparable results for both kinds of abutments supporting double crown retained dentures [63–65].
As a review of the literature shows, there are no publications available that present the long-term behavior of Vectris© used as material for the framework and the secondary crowns of removable partial dentures. Thus, the results published here are unique. Only some case reports exist, in which either no completely metal-free solutions are presented [66] or a removable long-term temporary solution made of glass fiber-reinforced composites is described [67, 68]. More extensive clinical data can therefore only be found for the long-term clinical behavior of glass fiber-reinforced composites as a framework for fixed partial dentures. For this indication, only moderate long-term results are presented. Thus, the survival rate of such constructions constitutes between 45 and 75 %, depending on the length of the follow-up period [69–72]. Framework fractures and chipping of veneering are mentioned as typical problems. Similar problems with this material in terms of strength and durability under stress conditions could also be confirmed in the present trial. As a result of these findings, electroplated secondary structures can clearly be preferred regarding clinical performance. The reliable integrity of the matrices is explained by the precise shaping process and the ductility of this material [8]. The matrices made of the fiberglass composite Vectris© show in return a reduced quality of fit and high brittleness, which might explain the poor clinical results with this material. Based on the experience gained in this trial, Vectris© may not be recommended for this indication because the expectations regarding the performance could not be confirmed in clinical use.
With regard to the basic idea of introducing metal-free double crown retained dental prostheses, further follow-up studies are required, e.g., with zirconia as a framework material. However, these may encounter similar problems regarding the substitution of the secondary structure. Up to now, only singular case reports or in vitro studies have been published on metal-free, removable dentures on double crowns respectively on full-ceramic bar-retained dentures, which is why data are scarce, and the field requires further detailed and long-term studies [73–75]. In the case reports available, friction of prostheses was achieved using acrylic or nylon materials. PEEK appears to hold even more potential as an alternative to frameworks made out of metal alloys. This material has been extensively used in other areas of medicine, such as in orthopedics, and exhibits ideal mechanic characteristics, good temperature resistance, and appropriate chemical characteristics. Although the usage of PEEK for fixed or removable dentures has only been studied in a limited number of case reports and a few in vitro studies [76–79], published results on PEEK so far show appropriate characteristics for the clinical situations investigated. They should, however, be validated in clinical long-term studies.
Conclusion
As a result of this prospective, randomized-controlled clinical trial, the use of metal-free prosthesis with secondary crowns and framework made of Vectris© cannot be recommended. However, the electroformed secondary copings showed enhanced clinical results. The high and precise fit, which is achieved by the intraoral luting, ensures an ideal mounting of the dental prosthesis and damage because the movement of the prosthesis is reduced to a minimum. With regard to failure, retention of the prostheses, and stability of the framework, the control group showed a significantly better clinical long-term behavior than the glass fiber composite prostheses. Furthermore, the present trial confirms that the use of ceramic copings with double crown restorations is, in principle, worthy and meets the required parameters, such as adhesion stability, biocompatibility, and aesthetics. However, the lithium disilicate glass ceramic IPS Empress 2© has an inadequate stability. Therefore, the use of high-strength zirconia ceramics is recommended. With this material, a much lower risk of damage can be expected. Although the reexamined metalliferous and metal-free prostheses exhibited a high need for repairs, the results of the patient survey showed a remarkably high degree of patient satisfaction with the new dentures. This can probably be explained by the generally high level of clinical performance of conical crown retained prostheses. Thus, the realization of a clinically reliable metal-free conical crown retained prosthesis still requires considerable further research and development. In particular, the substitution of electroplated secondary matrices represents a major challenge. Futures studies will need to prove the long-term suitability of modern materials such as PEEK for this indication.
References
Beschnidt SM, Chitmongkolsuk S, Prull R (2001) Telescopic crown-retained removable partial dentures: review and case report. Compend Contin Educ Dent 22:927–928, 929–32, 934 passim; quiz 942
Köhler KC (2002) Clinical follow-up about long-term outcome of double-crown-retained removable dentures. Dissertation, University of Frankfurt
Piwowarczyk A, Köhler KC, Bender R, Büchler A, Lauer HC, Ottl P (2007) Prognosis for abutment teeth of removable dentures: a retrospective study. J Prosthodont 16:377–382
4 Schwindling FS, Dittmann B, Rammelsberg P (2014) Double-crown-retained removable dental prostheses: a retrospective study of survival and complications. J Prosthet Dent. May 12. doi:10.1016/j.prosdent.2014.02.017
Stober T, Bermejo JL, Beck-Mussoter J, Seche AC, Lehmann F, Koob J, Rammelsberg P (2012) Clinical performance of conical and electroplated telescopic double crown-retained partial dentures: a randomized clinical study. Int J Prosthodont 25(3):209–216
Wöstmann B, Balkenhol M, Weber A, Ferger P, Rehmann P (2007) Long-term analysis of telescopic crown retained removable partial dentures: survival and need for maintenance. J Dent 35:939–945
Bär C, Reich S (2008) Telescopically retained removable partial dentures on CAD/CAM generated all-ceramic primary telescopes. Int J Comput Dent 11(2):115–130
Weigl P, Kleutges D (1998) An innovative and simple therapy concept for removable suprastructures with a new retainer application. In: Weber H, Mönkemeyer UR (eds) Therapy concepts for implant dentistry. Quintessenz, Karlsruhe, pp 117–158
Baig MR, Gunaseelan R (2012) Intraoral framework pick-up technique to improve fit of a metal-resin implant prosthesis. Indian J Dent Res 23(3):435–436. doi:10.4103/0970-9290.102257
Di Felice R, Rappelli G, Camaioni E, Cattani M, Meyer JM, Belser UC (2007) Cementable implant crowns composed of cast superstructure frameworks luted to electroformed primary copings: an in vitro retention study. Clin Oral Implants Res 18(1):108–113
Greven B, Luepke M, von Dorsche SH (2007) Telescoping implant prostheses with intraoral luted galvano mesostructures to improve passive fit. J Prosthet Dent 98(3):239–244
Janko S (2002) Prospective clinical study of intraorally luted double-crown-retained dentures. Dissertation, University of Frankfurt
Longoni S, Sartori M, Maroni I, Baldoni M (2010) Intraoral luting: modified prosthetic design to achieve passivity, precision of fit, and esthetics for a cement-retained, implant-supported metal-resin-fixed complete denture. J Prosthodont 19(2):166–170. doi:10.1111/j.1532-849X.2009.00526.x
Dietschi D, Magne P, Holz J (1994) Recent trends in esthetic restorations for posterior teeth. Quintessence Int 25(10):659–677
Höland W, Rheinberger V, Apel E, Ritzberger C, Rothbrust F, Kappert H, Krumeich F, Nesper R (2009) Future perspectives of biomaterials for dental restoration. J Eur Ceram Soc 29(7):1291–1297
Walia S, Thomas PM, Sandhu H, Santos GC (2009) Restoring esthetics with metal-free ceramics: a case report. J Can Dent Assoc 75(5):353–355
Weigl P (1999) All-ceramic primary crowns in the telescope system. In: Heidemann D (ed) Deutscher Zahnärztekalender. Hanser, München – Wien, pp 51–76
Weigl P, Hahn L, Lauer HC (2000) Advanced biomaterials used for a new telescopic retainer for removable dentures. J Biomed Mater Res 53:320–336
Weigl P, Lauer HC (2000) Advanced biomaterials used for a new telescopic retainer for removable dentures. J Biomed Mater Res 53:337–347
Dabrowa T, Dobrowolska A, Wieleba W (2013) The role of friction in the mechanism of retaining the partial removable dentures with double crown system. Acta Bioeng Biomech 15(4):43–48
Körber K, Körber S, Ludwig K (1996) Experimental studies about the stiffening effect of fibre-reinforced bridge frameworks made of Vectris after facing with the ceromer Targis. Quintessenz Zahntech 22:1343–1354
Bohlsen F, Kern M (2003) Clinical outcome of glass-fiber-reinforced crowns and fixed partial dentures: a three-year retrospective study. Quintessence Int 34(7):493–496
Göhring TN, Möhrmann WH, Lutz F (1999) Clinical and scanning electron microscopic evaluation of fiber-reinforced inlay fixed partial dentures: preliminary after one year. J Prosthet Dent 82:662–668
Langner J (1997) Fiber-reinforced composite Targis and Vectris for crowns and bridges. Quintessenz Zahntech 23:631–646
Loose M, Rosentritt M, Leibrock A, Behr M, Handel G (1998) In-vitro study of fracture strength and marginal adaptation of fiber-reinforced composite versus all-ceramic fixed partial dentures. Eur J Prosthodont Restor Dent 6:55–62
Behr M, Rosentritt M, Leibrock A, Schneider-Feyrer S, Handel G (1999) In-vitro study of fracture strength and marginal adaptation of fibre-reinforced adhesive fixed partial inlay dentures. J Dent 27(2):163–168
Behr M, Rosentritt M, Handel G (2003) Fiber-reinforced composite crowns and FPDs: a clinical report. Int J Prosthodont 16(3):239–243
Perea L, Matinlinna JP, Tolvanen M, Lassila LV, Vallittu PKJ (2014) Fiber-reinforced composite fixed dental prostheses with various pontics. Adhes Dent 16(2):161–168. doi:10.3290/j.jad.a30755
Schulz KF, Grimes DA (2002) Generation of allocation sequences in randomised trials: chance, not choice. Lancet 359(9305):515–519
Altman DG, Bland JM (1999) Statistics notes. Treatment allocation in controlled trials: why randomise? BMJ 318(7192):1209
Suresh K (2011) An overview of randomization techniques: an unbiased assessment of outcome in clinical research. J Hum Reprod Sci 4(1):8–11. doi:10.4103/0974-1208.82352
Bergman B, Ericson A, Molin M (1996) Long-term clinical results after treatment with conical crown-retained dentures. Int J Prosthodont 9:533–538
Heners M, Walther W (1988) Abutment distribution and rigid support—a clinical long-term study. Dtsch Zahnärztl Z 43:1122–1126
Hulten J, Tillström B, Nilner K (1993) Long-term clinical evaluation of conical crown retained dentures. Swed Dent J 17:225–234
Trimpou G (2006) Long-term clinical trial of implant retained double crown based overdentures by using prefabricated primary and secondary components of the Ankylos-implant system. Dissertation, University of Frankfurt
Wagner B, Kern M (2000) Clinical evaluation of removable partial dentures 10 years after insertion: success rates, hygienic problems, and technical failures. Clin Oral Investig 4:74–80
Widbom T, Löfquist L, Widbom C, Söderfeldt B, Kronström M (2004) Tooth-supported telescopic crown-retained dentures: an up to 9-year retrospective clinical follow-up study. Int J Prosthodont 17:29–34
Manicone PF, Rossi Iommetti P, Raffaelli L (2007) An overview of zirconia ceramics: basic properties and clinical applications. J Dent 35:819–826
Yilmaz H, Aydin C, Gul BE (2007) Flexural strength and fracture toughness of dental core ceramics. J Prosthet Dent 98:120–128
Bayer S, Kraus D, Keilig L, Gölz L, Stark H, Enkling N (2012) Changes in retention force with electroplated copings on conical crowns: a comparison of gold and zirconia primary crowns. Int J Oral Maxillofac Implants 27(3):577–585
Bayer S, Zuziak W, Kraus D, Keilig L, Stark H, Enkling N (2011) Conical crowns with electroplated gold copings: retention force changes caused by wear and combined off-axial load. Clin Oral Implants Res 22(3):323–329. doi:10.1111/j.1600-0501.2010.02003.x
Rösch R, Mericske-Stern R (2008) Zirconia and removable partial dentures. Schweiz Monatsschr Zahnmed 118:959–966
Turp I, Bozdağ E, Sünbüloğlu E, Kahruman C, Yusufoğlu I, Bayraktar G (2014) Retention and surface changes of zirconia primary crowns with secondary crowns of different materials. Clin Oral Investig Jan 31
Zafiropoulos GG, Rebbe J, Thielen U, Deli G, Beaumont C, Hoffmann O (2010) Zirconia removable telescopic dentures retained on teeth or implants for maxilla rehabilitation. Three-year observation of three cases. J Oral Implantol 36(6):455–465. doi:10.1563/AAID-JOI-D-09-00065
Behr M, Hofmann E, Rosentritt M, Lang R, Handel G (2000) Technical failure rates of double crown-retained removable partial dentures. Clin Oral Investig 4:87–90
Hofmann E, Behr M, Handel G (2002) Frequency and costs of technical failures of clasp- and double crown-retained removable partial dentures. Clin Oral Investig 6:104–108
Igarashi Y, Goto T (1997) Ten-year follow-up study of conical crown-retained dentures. Int J Prosthodont 10:149–155
Awad MA, Feine JS (1998) Measuring patient satisfaction with mandibular prostheses. Community Dent Oral Epidemiol 26:400–405
Awad MA, Locker D, Korner-Bitensky N, Feine JS (2000) Measuring the effect of intra-oral implant rehabilitation on health-related quality of life in a randomized controlled clinical trial. J Dent Res 79:1659–1663
Berg E (1984) The influence of some anamnestic, demographic, and clinical variables on patient acceptance of new complete dentures. Acta Odontol Scand 42:119–127
Bergman B, Carlsson GE (1972) Review of 54 complete denture wearers. Patients’ opinions 1 year after treatment. Acta Odontol Scand 30:399–414
Ettinger RL, Jakobsen JR (1997) A comparison of patient satisfaction and dentist evaluation of overdenture therapy. Community Dent Oral Epidemiol 25:223–227
Ericson A, Nilsson B, Bergman B (1991) Clinical results in patients treated with conical crown supported restorations. Quintessenz 8:1237–1252
Gernet W, Adam P, Reither W (1983) Follow-up studies of partial prostheses using K. H. Körber's conical crowns. Dtsch Zahnärztl Z 38:998–1001
Grossmann AC, Hassel AJ, Schilling O, Lehmann F, Koob A, Rammelsberg P (2007) Treatment with double crown-retained removable partial dentures and oral health-related quality of life in middle- and high-aged patients. Int J Prosthodont 20:576–578
John MT, Slade GD, Szentpétery A, Setz JM (2004) Oral health-related quality of life in patients treated with fixed, removable, and complete dentures 1 month and 6 to 12 months after treatment. Int J Prosthodont 17:503–511
Heydecke G (2002) Patient satisfaction as outcome measure in clinical studies of oral health. Schweiz Monatsschr Zahnmed 112:330–336
Slade GD (1997) Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol 25(4):284–290
Slade GD, Spencer AJ (1994) Development and evaluation of the oral health impact profile. Community Dent Health 11(1):3–11
Lachin JM, Matts JP, Wei LJ (1988) Randomization in clinical trials: conclusions and recommendations. Control Clin Trials 9:365–374
Altman DG, Doré CJ (1990) Randomisation and baseline comparisons in clinical trials. Lancet 335(8682):149–153
Schulz KF (1998) Randomized controlled trials. Clin Obstet Gynecol 41:245–256
Bernhart G, Koob A, Schmitter M, Gabbert O, Stober T, Rammelsberg P (2012) Clinical success of implant-supported and tooth-implant-supported double crown-retained dentures. Clin Oral Investig 16(4):1031–1037. doi:10.1007/s00784-011-0592-1
Krennmair G, Krainhöfner M, Waldenberger O, Piehslinger E (2007) Dental implants as strategic supplementary abutments for implant-tooth-supported telescopic crown-retained maxillary dentures: a retrospective follow-up study for up to 9 years. Int J Prosthodont 20(6):617–622
Nickenig HJ, Spiekermann H, Wichmann M, Andreas SK, Eitner S (2008) Survival and complication rates of combined tooth-implant-supported fixed and removable partial dentures. Int J Prosthodont 21(2):131–137
Duncan JP, Freilich MA, Latvis CJ (2000) Fiber-reinforced composite framework for implant-supported overdentures. HJ Prosthet Dent 84:200–204
Akin H, Turgut M, Coskun ME (2007) Restoration of an anterior edentulous space with a unique glass fiber-reinforced composite removable partial denture: a case report. J Esthet Restor Dent 19(4):193–197, discussion 198
Mete JJ, Dange SP, Khalikar AN, Vaidya SP (2011) Rehabilitation of anterior edentulous space by glass fiber reinforced composite removable partial denture during preadolescent period: a case report. J Indian Prosthodont Soc 11(3):195–198. doi:10.1007/s13191-011-0092-7
Izgi AD, Eskimez S, Kale E, Değer Y (2011) Directly fabricated inlay-retained glass- and polyethylene fiber-reinforced composite fixed dental prostheses in posterior single missing teeth: a short-term clinical observation. J Adhes Dent 13:383–391
Vallittu PK (2004) Survival rates of resin-bonded, glass fiber-reinforced composite fixed partial dentures with a mean follow-up of 42 months: a pilot study. J Prosthet Dent 91:241–246
Van Heumen CC, Kreulen CM, Creugers NH (2009) Clinical studies of fiber-reinforced resin-bonded fixed partial dentures: a systematic review. Eur J Oral Sci 117:1–6
Van Heumen CC, van Dijken JW, Tanner J, Pikaar R, Lassila LV, Creugers NH, Vallittu PK, Kreulen CM (2009) Five-year survival of 3-unit fiber-reinforced composite fixed partial dentures in the anterior area. Dent Mater 25:820–827
Bühler NM, Teubner E, Marinello CP (2011) Zirconia in removable prosthodontics. A case report. Schweiz Monatsschr Zahnmed 121(7–8):659–678
Groesser J, Sachs C, Heiß P, Stadelmann M, Erdelt K, Beuer F (2014) Retention forces of 14-unit zirconia telescopic prostheses with six double crowns made from zirconia—an in vitro study. Clin Oral Investig 18(4):1173–1179. doi:10.1007/s00784-013-1093-1
Karl M, Bauernschmidt B (2010) Erste Erfahrungen mit teleskopierendem Zahnersatz aus 100% Zirkoniumdioxid. Quintessenz Zahntech 36:86–94
Schmidlin PR, Stawarczyk B, Wieland M, Attin T, Hämmerle CH, Fischer J (2010) Effect of different surface pre-treatments and luting materials on shear bond strength to PEEK. Dent Mater 26(6):553–559. doi:10.1016/j.dental.2010.02.003
Siewert B, Parra M (2013) Eine neue Werkstoffklasse in der Zahnmedizin. PEEK als Gerüstmaterial bei 12-gliedrigen implantatgetragenen Brücken. Z Zahnärztl Implantol 29:148–159. doi:10.3238/ZZI.2013.0148−0159
Siewert B, Rieger H (2013) PEEK – Ein “neues” Gerüstmaterial für die metallfreie prothetische Therapie. Quintessenz Zahntech 39(10):2–11
Stawarczyk B, Beuer F, Wimmer T, Jahn D, Sener B, Roos M, Schmidlin PR (2013) Polyetheretherketone—a suitable material for fixed dental prostheses? J Biomed Mater Res B Appl Biomater 101(7):1209–1216. doi:10.1002/jbm.b.32932
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zahn, T., Zahn, B., Janko, S. et al. Long-term behavior of double crown retained dentures with metal and metal-free secondary crowns and frameworks made of Vectris© on all-ceramic primary crowns: a prospective, randomized clinical trial up to 14 years. Clin Oral Invest 20, 1087–1100 (2016). https://doi.org/10.1007/s00784-015-1597-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1597-y