Abstract
Objective
The objective of the study was to investigate the clinical outcome for electroplated telescopic removable dental prostheses (E-RDPs) with zirconia primary crowns.
Materials and methods
Sixty E-RDPs, with primary crowns manufactured from either cobalt–chromium alloy or zirconia, were fabricated for 56 participants. Electroplating was used to produce gold copings directly on the telescopic primary crowns. These copings were bonded intra-orally to the prosthesis framework. After 36 months, prosthesis survival and number of complications were assessed. Statistical analysis was performed by the use of Kaplan–Meier modeling and the log-rank test.
Results
Survival of the E-RDPs, 96.4% after 3 years, was identical in both groups. The need for aftercare was high but not significantly different: technical complications were observed for 37% and 42.9% of the prostheses for the zirconia and cobalt–chromium alloy primary crowns, respectively. Fracture of composite veneer was the most frequent complication (59.1%). The incidence of fractured abutment teeth, decementation, and endodontic problems was 7.9% in the zirconia group and 14% in the control group. The majority of abutment-level complications were treated restoratively. A significant difference was found for maximum probing depth at the abutment teeth: In the zirconia group, it decreased by 0.2 mm, whereas it increased by 0.8 mm in the control group (p = 0.04).
Conclusions
After 3 years of observation, survival of zirconia E-RDPs was favorable and comparable with that of established double-crown-retained prostheses. Further studies must clarify whether there are benefits of zirconia primary crowns for periodontal health.
Clinical relevance
Although these results encourage the use of zirconia primary crowns, more research is necessary to reduce the number of complications observed for secondary telescopic crowns, for example, failure of the veneer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
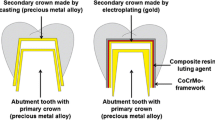
Double-crown attachments have proven successful for retention of removable dental prostheses (RDPs) [1–3]. They are characterized by inner, or primary, crowns, which are cemented to abutment teeth, and secondary crowns, which are integrated within removable prostheses [4]. Electroplating, or galvanoforming, can be used to manufacture the secondary crowns [5]. The electroplated copings are not affected by casting shrinkage and are bonded intra-orally to the denture framework to optimize “passive” fit, particularly with multiple attachment teeth or implants. Electroplating is an extensively automated process and does not require special technical skills [6]. Survival and incidence of complications are acceptable for electroplated telescopic removable dental prostheses (E-RDPs) [6].
Primary crowns for E-RDPs can be manufactured from zirconia by the use of CAD/CAM technology [7]. With zirconia primary crowns, healthy soft tissues and good denture retention have been observed [7, 8]. Zirconia primary crowns might, furthermore, improve function as a result of reduced retention force variability [9] and are of interest to patients who demand an attachment with tooth-like color when the denture is removed [10]. Retention forces for ceramic primary crowns are stable, even after extensive use [11]. Despite these advantages, clinical data for zirconia E-RDPs is sparse [12].
This prospective study was therefore designed to evaluate clinical outcome for zirconia E-RDPs. For comparison, E-RDPs with conventional, cast, cobalt–chromium primary crowns were fabricated, i.e., the groups differed with regard to the material of the primary crowns. More specifically, survival and the most frequent biological and technical complications were studied in a randomized clinical study.
Materials and methods
Trial design
This study was approved by the local ethics committee (file S-451/2005) and was conducted in accordance with the principles of the Declaration of Helsinki. Participants were randomly assigned to receive E-RDPs with either zirconia primary crowns (test group) or cast cobalt–chromium alloy primary crowns (control group). Before preparation of the abutment teeth, randomization was performed, i.e., the operating clinician opened an envelope containing computer-generated information about the respective study group.
Participants
Consecutive patients visiting the Department of Prosthodontics at Heidelberg University Hospital with a need for partial denture treatment were assessed for eligibility. The predefined inclusion criteria were minimum age 18 years, number of abutment teeth between 2 and 6, and ability to give written informed consent. Exclusion criteria were proved allergies to the dental materials to be used and patient’s wish for implant-supported restorations. Fifty-six patients were enrolled in this trial. Four participants (test group 3, control group 1) received prostheses in both maxilla and mandible, resulting in manufacture of a total of 60 E-RDPs (30 in each study group). As reported elsewhere [12], main baseline characteristics were balanced: in both groups, most participants were female (test group 27 participants, 10 male, 17 female; control group 29 participants, 6 male, 23 female). At the time the prostheses were integrated, the mean age was 61 years (SD 9.5 years; range 44–76 years). In both groups, more E-RDPs were inserted in the maxilla (test group 19 in maxilla, 11 in mandible; control group 20 in maxilla, 10 in mandible). The mean number of abutment teeth per denture was four (test group 114/30 = 3.8; control group 129/30 = 4.3). Most patients were Kennedy class I (test group 22; control group 21). Fewer cases were Kennedy class II (test group 6, control group 5) and class III (test group 2, control group 4). Follow-ups were scheduled 6, 12, 24, and 36 months after denture insertion.
Clinical procedure
Participants were treated either during student courses, under supervision by experienced resident dentists or by the resident dentists themselves. A routine procedure described by Weigl et al. was used for E-RDP manufacture [11]. The abutment teeth were prepared and conventional impressions were taken (Impregum; 3M Espe, Bad Seefeld, Germany). In the dental laboratory, type IV gypsum models were produced. These models were digitized to manufacture the zirconia primary crowns (Procera Forte; Nobel Biocare, Göteborg, Sweden). The datasets were transferred to Nobel Biocare for milling of a coping with the Procera system (Fig. 1). After a clinical try-in session, the copings were finished in the dental laboratory on the master cast.
The cobalt–chromium primary crowns (Remanium 2000+; Dentaurum, Ispringen, Germany) were made by the use of the lost-wax technique. Both primary crown types were manufactured with a 1° taper. The thickness of the zirconia primary crowns was set to a minimum of 0.7 mm; the cobalt–chromium crowns were 0.5 mm thick. In both groups, electroplated secondary crowns were produced (AGC Micro Plus; Wieland Dental, Pforzheim, Germany) and bonded intra-orally to the frameworks by the use of AGC Cem (Wieland Dental, Pforzheim, Germany) to guarantee passive fit. Before cementation of the primary crowns, the prepared teeth were thoroughly cleaned with H202. The cobalt–chromium primary crowns were preconditioned with sandblasting in the dental laboratory (alumina, 50 μm, 2 bar). The zirconia primary crowns were not sandblasted. Non-adhesive, conventional cementation with glass-ionomer cement (Ketac Cem, 3M Espe) was chosen. Standardized procedures were used for clinical and laboratory stages of denture manufacture. All participating clinical operators, dental laboratories, and investigators were repeatedly re-calibrated by the principal investigator (T.S.).
Study endpoints
The baseline examination was performed after primary crown cementation. Between these dates, there was a mean time of 17.2 days (SD 3.3) in the study group and of 17.2 (SD 2.9) in the control group. The period of RDP fabrication reached from January 2009 to June 2013. After the participants had completed the scheduled 36-months follow-up, trial data were analyzed to assess prosthesis survival, defined as the number of prostheses still in use without any need for replacement. During the follow-up examinations, technical and biological complications had been recorded by the use of standardized assessment sheets. Abutment-level complications (attachment tooth fractures, decementation, and endodontic problems) and prosthesis-level complications (denture base fractures, veneering failures, and need for relining) were recorded. It was decided to reline the prostheses when a denture base misfit was observed and confirmed with a silicone impression material. To assess periodontal health, a periodontal probe with a millimeter scale was used. Probing was performed on the mesial and distal aspect of all abutment teeth. The maximum probing depth was analyzed, computing mean values for the groups and comparing these means.
Statistical analysis was performed with SPSS Statistics 22 (IBM, Armonk, NY, USA). Kaplan–Meier modeling was used to analyze prosthesis survival. Two-sample t test and the log-rank test were used to detect possible inter-group differences. The level of significance was set at 0.05.
Results
Prosthesis survival
Fifty-four E-RDPs (Fig. 2) were re-assessed after 36 months, i.e., 90% (54/60). Six E-RDPs were not re-examined because of the following:
-
Four patients (two in each study group) did not attend their re-examination session, despite several attempts to arrange an appointment.
-
One zirconia E-RDP failed during manufacture, because of zirconia fracture, and the participant did not wish to continue participating in the study and withdrew consent. The failure occurred during a try-in session and not during clinical use.
-
One other prosthesis was replaced after 24 months (control group), because the patient was dissatisfied with the esthetics of the denture.
One E-RDP failure was observed in each group (54 participants were still under risk) and two participants did not attend re-examination. As a result, cumulative prosthesis survival was 96.4% (27/28) after 36 months in both test and control groups.
Abutment-level complications
Maximum probing depth at baseline was 3.7 mm (SD 1.4 mm) in the test group and 4.1 mm (SD 1.4 mm) in the control group (p = 0.2). After 36 months, probing depth decreased slightly in the test group (3.5 mm, SD 1.1 mm) whereas it increased in the control group (4.9 mm, SD 2.6 mm) (p = 0.01). In the test group, maximum probing depth decreased by 0.2 mm (SD 1.4 mm), whereas it increased by 0.8 (SD 2.1 mm) in the control group (p = 0.04). This difference was statistically significant.
Abutment-level complications, i.e., fractured abutment teeth, decementation, and endodontic problems, were evaluated relative to the total number of abutment teeth (test group 114; control group 129) and the number of prostheses. In each study groups, 27 E-RDPs were compared (because of one prosthesis failure and two absent patients in each group, see above). Relative to the total number of abutments, the incidence of complications was 7.9% (9/114) in the test group and 14% (18/129) in the control group. Six complications occurred in the test group (incidence 6/27 = 22.2%) and 11 in the control group (incidence 11/27 = 40.7%). The difference between abutment-level complication-free survival in the groups was not statistically significant (log-rank test, p = 0.192, Fig. 3). The distribution of the abutment complications is listed in Table 1.
Technical complications at abutment level in both study groups. The mean number of abutment teeth and their distribution were comparable at baseline. After 36 months, the difference between the study groups was not statistically significant. All abutment complications were included in this Kaplan–Meier analysis, irrespective of subsequent therapy (extraction or restoration)
In both groups, most complications were treated restoratively; extractions were usually unnecessary. In five cases (5/17 = 29.4%), abutments needed extraction, whereas in 12 cases, the complications were managed by the use of restorative procedures only. In all cases of abutment tooth extraction, the RDPs could be preserved, because support and retention were acceptable with the remaining abutment teeth.
Prosthesis-level complications
Denture base and framework fracture, veneer failure, need for relining, and failure of the electroplated structures were defined as technical complications at the prosthesis level. Again, 27 E-RDPs were compared in each group. One additional complication was observed for a patient who later did not attend the 36-month recall. This complication was nevertheless included in the analysis (resulting in 28 E-RDPs in the control group). Technical complications occurred in 10 cases in the test group (incidence of complications 10/27 = 37%) and in 12 cases in the control group (incidence of complications 12/28 = 42.9%). The difference between prosthesis-level complication-free survival in the groups was not statistically significant (log-rank test, p = 0.531, Fig. 4). Table 2 shows the most frequent technical complication with E-RDPs was failure of the secondary crown veneer (13/22 = 59.1%). In addition, for one zirconia E-RDP, fracture of two primary crowns was observed. This fracture occurred during trepanation of the abutment teeth in order to perform root canal treatment.
Discussion
In this randomized trial, we observed identical, favorable survival for E-RDPs with cobalt–chromium alloy and zirconia primary crowns after 3 years. Zirconia E-RDPs were as successful as established cobalt–chromium E-RDPs for treatment of patients with reduced dentition, although a need for intensive aftercare and treatment of complications was observed, stressing the need for further research and development in this field of prosthodontics.
In previous studies, zirconia E-RDP attachments were predominantly tested in vitro, with promising results. Beuer et al. compared zirconia and gold primary crowns [13]: for zirconia, retention force when a 0° taper was used exceeded that in the gold control group. For long abutment teeth and a 2° taper, zirconia was also described as a viable alternative to cast gold. Bayer et al. showed that retentive force changed less for zirconia primary crowns than for a gold control group; it was assumed this would be beneficial in clinical use [14]. This finding was supported by Turp et al., who observed more predictable and less excursive retention force for zirconia primary crowns [15].
Despite the multitude of in vitro investigations, as far as the authors are aware, clinical use of zirconia primary crowns has not previously been investigated in a randomized clinical trial. Our comparison is relevant because digital manufacture of removable appliances is currently attracting attention [16–18]. RDPs account for up to 29% of prosthetic restorations in Western society [19], with double crowns being a frequently used mode of attachment. Zirconia primary crowns are an important stage in the digitization of RDP production; their manufacture introduced digital procedures into fabrication of partial dentures. In this investigation, cobalt–chromium alloy was chosen for the control group. Combining primary crowns made of cobalt–chromium alloy with electroplated secondary crowns is a well-established therapy [20, 21]. As a result of lower cost and favorable mechanical properties, cobalt–chromium is of more interest than gold alloys in dental practice.
The main baseline characteristics of the study groups were balanced. In this context, it was particularly important that the number and distribution of abutment teeth were similar, to enable comparison. We have previously reported on oral health-related quality of life, which had not been significantly different between the groups at baseline [12], and similar to results from other cross-sectional studies [22]. This implies that the study groups were comparable with other populations. The university setting of this study must be emphasized, however, and selection and operator bias cannot, therefore, be excluded: the treatments were performed by several dentists with different operating experience. In particular, at the beginning of the investigation, several zirconia primary crowns fractured during fabrication. For one patient, several zirconia primary crowns failed during a clinical try-in session. Subsequently, the thickness of the zirconia primary crowns was set to a minimum of 0.7 mm, and not 0.5 mm as previously; this terminated fracture problems. This meant, however, that zirconia primary crowns were fabricated thicker than their cobalt–chromium counterparts. This must be kept in mind, because it might affect the esthetics and substance removal from the abutment teeth.
Probing depth at the abutment teeth developed significantly different in the two study groups. While maximum probing depth decreased by 0.2 mm in the zirconia group after 36 months, it increased by 0.8 in the control group. The evidence from the present study suggests that the use of zirconia primary crowns might be more beneficial for periodontal health than the use of cobalt–chromium primary crowns. Possible reasons might be the high biocompatibility [23] and low-microbiological colonization [24] of zirconia. Several limitations to this finding must be addressed: probing forces were not standardized with force gauges. This might have led to an inter-operator bias. Furthermore, only the maximum probing depth was assessed, which has been measured at only two sides of the abutment teeth. Therefore, this result must be interpreted with care. In future studies, it must be evaluated in more detail, using additional and more specific periodontal parameters. However, this interesting result has clinical relevance and might be the basis for further research in the biological effects of zirconia primary crowns.
With regard to prosthesis survival, favorable results were obtained for zirconia E-RDPs after mid-term periods of observation. In the literature, survival of E-RDPs with cast primary crowns have been reported to be 93.3% after 3 years [6]. This confirms the results obtained for the control group in our investigation and thus the validity of the study. Stober et al. reported survival of 100% after 3 years for conventional conical, double-crown-retained RPDs without electroplating and with cast primary crowns [6]. Wöstmann et al. reported survival of 95.1% after 5 years for cast telescopic crown-retained RDPs, without electroplating [2]. Schwindling et al. reported survival of 93.8% after 7 years for cast double-crown-retained prostheses [1]. Taken together, survival reported in this study seems to be in the range previously reported for electroplated and conventional RDPs.
Despite favorable survival, there was a need for intensive aftercare for all E-RDPs. Complications occurred for 37% of the zirconia E-RDPs prostheses, even though some of the complications (for example, the need for relining) might be interpreted more as regular aftercare than as a “complication.” In accordance with literature reports, composite veneer was a major weakness, accounting for 59.1% of the technical complications. Hahnel et al. reported veneer failure for 27.9% of retrospectively examined conventional conical crown-retained dentures [25]. In another retrospective analysis, Wöstmann et al. found 26.9% of telescopic crown-retained RDPs needed facing repairs [2]. The use of electroplating requires increased space in the region of the attachment tooth (for primary crown, electroplated coping, CoCr framework, and composite veneering). It can be speculated that in borderline cases, less attention was paid to the minimum thickness of the composite veneer, which might have increased the risk of veneer failure. With regard to abutment-level complications, there was a tendency towards increased complications in the control group (11 cases, compared with six in the study group), although the difference was not statistically significant. In several cases (Table 1), multiple combinations occurred, for example, endodontic problems and subsequent abutment fractures. It can be speculated that E-RDP abutment teeth which received root canal treatment after denture integration might have had a tendency to fracture. This is supported by Stober et al., who previously revealed the risk of failure for non-vital abutments to be significantly higher than that for vital teeth (hazard ratio 2.29) [26].
More research is necessary to reduce the high incidence of complications. Nevertheless, the complications were not associated with the use of zirconia primary crowns, but with veneer chipping, denture base fracture, or decementation. It has, however, been calculated that cost per failure for clasp-retained prostheses is more than twice as high as that for double-crown systems [27]. Zirconia has many advantages, for example, tooth-like color, the good mechanical properties, high biocompatibility [23], and low microbiological colonization [24]. It is plausible that this might have led to the decrease in probing depth in this trial, whereas mean probing depth increased in the control group. Zirconia is, therefore, an interesting and highly promising material for RDP treatment.
Conclusion
This randomized trial of zirconia E-RDPs found survival was favorable after 36 months of observation and identical with that for E-RDPs with cast cobalt–chromium primary crowns. No statistically significant difference between complications in the two study groups was found. It remains a challenge of future research to develop new combinations of material or treatment rationales to limit the need for repair of E-RDP.
References
Schwindling FS, Dittmann B, Rammelsberg P (2014) Double-crown-retained removable dental prostheses: a retrospective study of survival and complications. J Prosthet Dent 112:488–493. doi:10.1016/j.prosdent.2014.02.017
Wöstmann B, Balkenhol M, Weber A, Ferger P, Rehmann P (2007) Long-term analysis of telescopic crown retained removable partial dentures: survival and need for maintenance. J Dent 35:939–945. doi:10.1016/j.jdent.2007.09.010
Verma R, Joda T, Brägger U, Wittneben JG (2013) A systematic review of the clinical performance of tooth-retained and implant-retained double crown prostheses with a follow-up of >/= 3 years. J Prosthodont 22:2–12. doi:10.1111/j.1532-849X.2012.00905.x
Isaacson GO (1969) Telescope crown retainers for removable partial dentures. J Prosthet Dent 22:436–448
Diedrichs G, Rosenhain P (1991) Galvano-outer telescope by direct technique. Quintessenz 42:49–56
Stober T, Bermejo JL, Beck-Mussotter J, Seche AC, Lehmann F, Koob J, Rammelsberg P (2012) Clinical performance of conical and electroplated telescopic double crown-retained partial dentures: a randomized clinical study. Int J Prosthodont 25:209–216
Rinke S, Buergers R, Ziebolz D, Roediger M (2015) Clinical outcome of double crown-retained implant overdentures with zirconia primary crowns. J Adv Prosthodont 7:329–337. doi:10.4047/jap.2015.7.4.329
Zahn T, Zahn B, Janko S, Weigl P, Gerhardt-Szep S, Lauer HC (2016) Long-term behavior of double crown retained dentures with metal and metal-free secondary crowns and frameworks made of Vectris((c)) on all-ceramic primary crowns: a prospective, randomized clinical trial up to 14 years. Clin Oral Investig 20:1087–1100. doi:10.1007/s00784-015-1597-y
Bayer S, Kraus D, Keilig L, Gölz L, Stark H, Enkling N (2012) Changes in retention force with electroplated copings on conical crowns: a comparison of gold and zirconia primary crowns. Int J Oral Maxillofac Implants 27:577–585
Zafiropoulos GG, Rebbe J, Thielen U, Deli G, Beaumont C, Hoffmann O (2010) Zirconia removable telescopic dentures retained on teeth or implants for maxilla rehabilitation. Three-year observation of three cases. J Oral Implantol 36:455–465. doi:10.1563/AAID-JOI-D-09-00065
Weigl P, Lauer HC (2000) Advanced biomaterials used for a new telescopic retainer for removable dentures. J Biomed Mater Res 53:337–347
Schwindling FS, Deisenhofer UK, Seche AC, Lehmann F, Rammelsberg P, Stober T (2016) Randomized trial investigating zirconia electroplated telescopic retainers: quality of life outcomes. Clin Oral Investig. doi:10.1007/s00784-016-1869-1
Beuer F, Edelhoff D, Gernet W, Naumann M (2010) Parameters affecting retentive force of electroformed double-crown systems. Clin Oral Investig 14:129–135. doi:10.1007/s00784-009-0271-7
Bayer S, Zuziak W, Kraus D, Keilig L, Stark H, Enkling N (2011) Conical crowns with electroplated gold copings: retention force changes caused by wear and combined off-axial load. Clin Oral Implants Res 22:323–329. doi:10.1111/j.1600-0501.2010.02003.x
Turp I, Bozdag E, Sunbuloglu E, Kahruman C, Yusufoglu I, Bayraktar G (2014) Retention and surface changes of zirconia primary crowns with secondary crowns of different materials. Clin Oral Investig 18:2023-2035. doi:10.1007/s00784-013-1183-0
Schwindling FS, Stober T, Rustemeier R, Schmitter M, Rues S (2016) Retention behavior of double-crown attachments with zirconia primary and secondary crowns. Dent Mater 32:695–702. doi:10.1016/j.dental.2016.03.002
Kattadiyil MT, Jekki R, Goodacre CJ, Baba NZ (2015) Comparison of treatment outcomes in digital and conventional complete removable dental prosthesis fabrications in a predoctoral setting. J Prosthet Dent 114:818–825. doi:10.1016/j.prosdent.2015.08.001
Hagiwara Y, Nakajima K (2016) Use of ceria-stabilized zirconia/alumina nanocomposite for fabricating the frameworks of removable dental prostheses: a clinical report. J Prosthet Dent 116:166–171. doi:10.1016/j.prosdent.2016.01.020
Zitzmann NU, Hagmann E, Weiger R (2007) What is the prevalence of various types of prosthetic dental restorations in Europe? Clin Oral Implants Res 18(Suppl 3):20–33. doi:10.1111/j.1600-0501.2007.01435.x
Ozyemisci-Cebeci N, Yavuzyilmaz H (2013) Comparison of the effects of friction varnish and electroforming on the retention of telescopic crowns. J Prosthet Dent 109:392–396. doi:10.1016/S0022-3913(13)60325-X
Engels J, Schubert O, Güth JF, Hoffmann M, Jauernig C, Erdelt K, Stimmelmayr M, Beuer F (2013) Wear behavior of different double-crown systems. Clin Oral Investig 17:503–510. doi:10.1007/s00784-012-0746-9
Inukai M, Baba K, John MT, Igarashi Y (2008) Does removable partial denture quality affect individuals’ oral health? J Dent Res 87:736–739
Manicone PF, Rossi Iommetti P, Raffaelli L, Paolantonio M, Rossi G, Berardi D, Perfetti G (2007) Biological considerations on the use of zirconia for dental devices. Int J Immunopathol Pharmacol 20:9–12
Bremer F, Grade S, Kohorst P, Stiesch M (2011) In vivo biofilm formation on different dental ceramics. Quintessence Int 42:565–574
Hahnel S, Bürgers R, Rosentritt M, Handel G, Behr M (2012) Analysis of veneer failure of removable prosthodontics. Gerodontology 29:e1125–e1128. doi:10.1111/j.1741-2358.2010.00394.x
Stober T, Bermejo JL, Séché AC, Lehmann F, Rammelsberg P, Bömicke W (2015) Electroplated and cast double crown-retained removable dental prostheses: 6-year results from a randomized clinical trial. Clin Oral Investig 19:1129–1136. doi:10.1007/s00784-014-1335-x
Hofmann E, Behr M, Handel G (2002) Frequency and costs of technical failures of clasp- and double crown-retained removable partial dentures. Clin Oral Investig 6:104–108
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This study was financially supported by a grant from Nobel Biocare Services AG (grant no. 2005-362). Sebastian Schwindling was supported by the Physician Scientist-Programme of the Medical Faculty of the University of Heidelberg.
Ethical approval
All procedures performed were in accordance with the ethical standards of the local institutional review board (file S-451/2005) and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Informed consent was obtained from all the participants included in the study.
Rights and permissions
About this article
Cite this article
Schwindling, F.S., Lehmann, F., Terebesi, S. et al. Electroplated telescopic retainers with zirconia primary crowns: 3-year results from a randomized clinical trial. Clin Oral Invest 21, 2653–2660 (2017). https://doi.org/10.1007/s00784-017-2067-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-017-2067-5