Abstract
Study design
Retrospective case series.
Objective
To evaluate our treatment strategy for cervical dumbbell neurinoma.
Summary of background data
In treating cervical dumbbell neurinoma, possible difficulties include reoperation due to recurrent tumor, denervation due to nerve root resection, and postoperative spinal deformity due to extensive bony removal.
Methods
We reviewed 75 cases of cervical dumbbell neurinoma that were treated surgically between 1985 and 2006. Postoperative neurological deficits, effects of surgical margins on tumor recurrence, and surgical complications were investigated retrospectively.
Results
Sensory and motor deficits due to resection of specific nerve roots appeared temporarily in 33 and 23 % of all cases, and persisted in 8 and 8 % at final evaluation, respectively. Total, subtotal, and partial resection was performed in 57, 13, and 5 cases, respectively. The total resection rate was low in the tumors that had large extraforaminal components. Of the subtotally resected 13 cases, only two cases of high tumor-growth rate required re-operation or showed tumor growth. Among the five partially resected cases, re-operation was necessary in two cases 13 and 15 years later because of aggravated neurological symptoms due to tumor growth. Two patients who underwent C2 laminectomy developed kyphosis, and three patients who underwent facet joint resection and curettage of vertebral body lesions developed scoliosis.
Conclusion
Total resection should be attempted for cervical dumbbell tumors. In cases where total resection was potentially of high risk, however, subtotal resection (within the capsule) was found to be a practical choice yielding favorable long-term outcome when the tumor growth rate (MIB-1 index) was low.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical outcomes for spinal cord tumors, particularly intradural extramedullary tumors, have improved remarkably following advances in microscopic surgery and diagnostic imaging, as well as the introduction of new surgical devices such as the Cavitron ultrasonic surgical aspirator (CUSA) [1]. A variety of therapeutic strategies for cervical dumbbell neurinomas have been proposed using multiple classification systems, because this tumor is diverse in terms of the affected spinal levels, location, and size [2, 3]. Surgeons often face difficulties such as (1) reoperation when total resection is impossible at the first operation, (2) the development of denervation symptoms when the nerve roots were sacrificed, and (3) postoperative spinal deformity when a large amount of bony component was removed to extirpate the tumor [3–5]. We undertook a retrospective analysis of the long-term outcomes of surgery undertaken at our hospital for cervical dumbbell neurinoma in order to establish the optimal treatment strategy.
Patients and methods
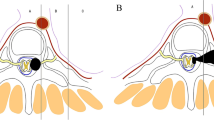
The study group involved 75 patients with a cervical dumbbell neurinoma (36 males and 39 females) who underwent surgery at our institute between 1985 and 2006. At surgery, the ages of the patients ranged from 21 to 81 years (mean 52.3 years, SD 15.5 years). The affected levels were C1 in 2 cases, C2 in 30 cases, C3 in 13 cases, C4 in 5 cases, C5 in 12 cases, C6 in 5 cases, C7 in 5 cases, and C8 in 3 cases. The tumor location in the axial plane, according to Toyama’s classification [2] (Fig. 1), was type I in 2 cases, IIa in 10 cases, IIb in 11 cases, IIIa in 29 cases, IIIb in 19 cases, IV in 1 case, V in 1 case, and VI in 3 cases. The surgical approaches were posterior in 67 cases, anterior in 1 case, and combined anterior + posterior in 7 cases. In the 67 cases in which a posterior approach was employed, hemilaminectomy, hemilaminectomy with open-door laminoplasty, and laminectomy were performed in 45, 17, and 5 cases (C2:2, C3:2, C5:1), respectively. Furthermore, unilateral partial facet joint resection, unilateral total resection of a single facet joint, and unilateral total resection of two facet joints were performed in 56, 8, and 3 cases, respectively. In all cases, the proximal affected nerve roots were resected and then dural plasty was performed with artificial dura mater. The surgical margins of the tumor resection were classified into en bloc total resection (en bloc tumorectomy with resection of the distal affected nerve root), gross total resection (tumorectomy using CUSA without resection of the distal affected nerve roots and no evidence of the residual tumor), subtotal resection (more than 90 % resection), and partial resection (less than 90 % resection), based on the findings of the axial images of postoperative Gd-enhanced MRI. We considered en bloc total resection and gross total resection to be total resection. The size of the residual tumor was quantified using OsiriX® imaging software (Pixmeo, Bernex, Switzerland). The postoperative follow-up periods ranged from 4.8 to 25.8 years (mean 12.4 years, SD 3.2 years). Neurological symptoms including the presence/absence of denervation symptoms due to the resection of the affected nerve root, the feasibility of total resection, the need for re-operation, and postoperative complications were evaluated depending on the affected spinal level and the type of tumor. The Japanese Orthopaedic Association (JOA) scoring system for cervical myelopathy was used to determine the pre- and postoperative neurological status. The recovery rate after treatment was calculated using the Hirabayashi method: (postoperative JOA score − preoperative score)/(17 − preoperative score) × 100 %. To evaluate the proliferation capacity of all the tumors, MIB-1 staining was performed and the MIB-1 index was calculated.
An imaging-based anatomic classification of dumbbell tumors, including nine types. Type I, intradural and extradural tumors, are located only in the spinal canal and constrict only the dura. Type II, epidural tumors with constriction at the foramen, include three subtypes (a, b, and c) defined according to the degree of extraforaminal spread. Type IIa tumors do not extend beyond the intervertebral foramen, while types IIb and IIc extend increasingly beyond the intervertebral foramen. Type III tumors, with both dural and foraminal constriction, include an intradural- and extradural-foraminal type (type IIIa) and an intradural- and extradural-paravertebral type (IIIb). Type IV tumors are extradural and intravertebral, invading only the vertebral body; type V lesions are extradural and extralaminal with invasion of the lamina; and type VI tumors show multidirectional erosion of the bone
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of our patients were followed during the course of this research. This study was approved by the Institutional Review Board of School of Medicine, Keio University. We obtained signed consent forms about this study from all patients.
Results
Functional recovery and neurological deficits after tumor resection
In all cases, neurological recovery from cervical myelopathy was observed immediately after the surgery. The preoperative JOA score of 11.4 improved to 15.2 postoperatively (recovery rate 67.8 %). Sensory deficits after the resection of the nerve roots affected by the tumor were seen in 25 cases (33 %), and the most frequent spinal segment affected was C2 (18 cases), followed by C7 (3 cases) and C8 (2 cases). The sensory deficits persisted in five of these C2 cases and one of the C8 cases (six cases in total, 8 %) until the last evaluation (Fig. 2a). Motor deficits after resection of the nerve roots affected by the tumor were seen in 17 cases (23 %), and the most frequent spinal segment affected was C5 (11 cases), followed by C8 (3 cases), C6 (2 cases), and C7 (1 case). In 11 of these 17 cases, muscle strength returned to normal within three months after surgery, whereas the motor weakness was still observed at the last evaluation in six cases (four C5, two C8) (Fig. 2b).
Postoperative neurological deficits (motor and sensory) according to the level of the tumor. a Sensory deficits after the resection of the nerve roots affected by the tumor were seen in 25 cases (33 %), and the most frequent spinal segment affected was C2, followed by C7 and C8. In five of the C2 cases and one C8 case the sensory deficits persisted until the last evaluation. b Motor deficits after resection of the nerve roots affected by the tumor were seen in 17 cases (23 %), and the most frequent spinal segment affected was C5, followed by C8, C6, and C7. In 11 of these 17 cases, muscle strength returned to normal within three months after surgery, whereas the motor weakness was still observed at the last evaluation in six cases (four C5, two C8)
Surgical margin and re-operation
The tumor was totally resected in 57 cases (76 %), subtotally (more than 90 % resection) in 13 cases, and partially (less than 90 % resection) in 5 cases, based on the findings of the axial images of postoperative Gd-enhanced MRI. Among the 57 cases of total resection, en bloc total resection was performed in 39 cases and gross total resection in 18 cases. Tumor recurrence was not seen in any of the cases of total resection. Re-operation was necessary due to aggravation of neurological symptoms from the growth of residual tumors four and five years later in two cases (type VI) of subtotal resection, and 13 and 15 years later in two cases of partial resection (one each of type IIb and IIIb) (Table 1). In the two type VI cases, no sign of malignancy was demonstrated histologically, but the MIB-1 index was higher (5 and 8 %) than for the other two cases (MIB-1 index <2 %). In the non re-operation cases, the MIB-1 index was below 1 % in 41 cases and below 2 % in 30 cases.
The percentage of patients in whom total resection could be performed (the total resection rate) was lower in types IIb, IIIb, and VI than the other types. In addition, the total resection rate was lower in cases where the tumor affected the C3, 5, and 6 segments than in cases where the tumor affected other spinal segments (Table 2). In other words, incomplete tumor resection was performed in the cases of (1) an upper cervical dumbbell tumor with a large extraforaminal portion, (2) vascular damage arising from adhesion to the vertebral artery, and (3) mid-cervical dumbbell tumor involving multiple nerve roots due to extraforaminal growth. It is worth noting that tumor growth has been absent to date in 11 of the 13 subtotally resected cases, and that no re-operation was needed in 2 of the 5 partially resected cases.
Complications
Soon after the first operation, one patient developed cerebrospinal fluid leakage, which was alleviated by lumbar drainage. Pseudomeningocele was noted in eight cases, which resolved spontaneously in 6–9 months in all cases. Postoperative cervical spine deformities occurred in five cases (progression in the local kyphosis or scoliosis was defined as a >20° increase in the C2–7 angle or Cobb angle). Kyphosis developed in two patients who underwent C2 laminectomy for a tumor developing in the upper cervical vertebrae (C2, 3). Scoliosis was noted postoperatively in three patients in whom unilateral resection of two facet joints was necessary to remove the tumor invading the vertebral body (type V in one case and type VI in two cases). However, bone union was achieved in all three cases, and no additional operation was needed. It is worth noting that no scoliotic deformity was seen in any of the eight cases involving unilateral resection of a single facet joint.
Discussion
When a cervical dumbbell tumor is so diffusely intermingled with the nerve rootlet that the nerves can no longer be separated from the tumor, it may be impossible to achieve radical removal of the tumor without sacrificing the nerve roots [6]. In cases where the tumor within the spinal canal is left unresected, it is likely that re-growing tumor will aggravate neurological symptoms, necessitating re-operation [7]. However, the incidence of denervation symptoms arising from the resection of the nerve roots varies greatly among different reports (0–23 %) and there is no consensus on this issue [3–9]. This may be explained by differences in the level of the affected nerve root and the operative procedure used in previous reports. To date, no detailed analysis of these issues has been performed and reported.
In the present study, a sensory deficit after resection of an affected nerve root was seen in 33 % of all cases, and it persisted until the last evaluation in 8 %. Regarding the level of the tumor-affected spinal segment, a sensory deficit often appeared after resection of the C2 and C8 nerve roots. Motor deficits after resection of an affected nerve root appeared in 23 % of all cases and also persisted up to the last evaluation in 8 %. Motor deficits appeared frequently after resection of the C5 and C8 nerve roots. Because the deltoid muscle and the intrinsic muscles, which are governed by the C5 and C8 nerve roots, respectively, appear to be poorly supplied by nerves from the adjacent levels, there is almost no motor function compensation after resection of the C5 and C8 nerve roots. Therefore, this anatomical characteristic caused more severe motor functional deficits following the resection of the C5 and C8 nerve roots than other nerve roots.
Given the risk of tumor recurrence, total resection should be attempted for all cervical dumbbell neurinomas. However, previous reports show total resection rates of 86–94 % for cervical dumbbell neurinomas, indicating that total resection is not possible in cases [1–3, 5, 6]. In our series, the total resection rate was 76 %, lower than those in previous reports. The low percentage in our series is attributable to the inclusion of 18 cases with an upper cervical tumor with a large extraforaminal portion, a tumor that adhered strongly to the vertebral artery, and a mid-cervical tumor involving multiple nerve roots. Of these 18 cases, four cases required re-operation because of tumor re-growth, including two subtotally resected cases (both type VI) and two partially resected cases (type IIb and IIIb). The two type VI cases required re-operation within five years after the first operation, and they showed a high tumor growth rate (MIB-1 index, 5 and 8 %), suggesting that total resection through an anterior and posterior approach should be applied to type VI cases whenever possible if the MIB-1 index is high. However, the length of time from the first operation to the re-operation was longer (13 and 15 years, respectively) in the other two cases (type IIb and IIIb), suggesting that total resection is not always necessary in elderly patients with a low MIB-1 index (below 2 %). After subtotal resection, tumor re-growth was not seen in any of the cases other than the two type VI cases. On the basis of these results, total resection of a cervical dumbbell tumor (except for types IIb, IIIb and VI) should initially be performed through a posterior approach with or without facetectomy. Even if total resection cannot be performed due to bleeding around the vertebral artery, no additional surgery is necessary as long as the postoperative tumor growth rate is low (MIB-1 index <2 %). If the postoperative tumor proliferation rate is high (MIB-1 index >5 %), additional resection through a second-stage anterior approach should be considered.
Several investigations [10, 11], including our study, have reported the development of postoperative cervical spine deformity. In the present study, kyphotic deformity developed in two out of 30 cases in which a C2 laminectomy was performed for a tumor affecting the upper cervical segments, which was consistent with the previous studies [12, 13]. Local scoliosis developed in three cases in which two-level facet joint resection was performed to remove the tumor invading the vertebral body (types V and VI). In these cases, bone union was achieved by anterior intervertebral fusion with an autologous bone graft. We therefore recommend the concomitant application of surgical fusion in such cases. Several reports have been published on the instability of the cervical spine following facet joint resection [6, 14]. However, no conclusion has been reached on the development of cervical spine deformities during long-term postoperative follow-up. In the present study, no cervical spine deformity was seen in the eight cases followed for long periods after the unilateral resection of a single facet joint, probably because these tumors were removed through two-level hemilaminectomy.
Conclusions
This study revealed a high frequency of denervation symptoms, including sensory deficits following resection of the C2, 7, and 8 nerve roots as well as motor deficits following resection of the C5 and 8 nerve roots. Total resection should be attempted for cervical dumbbell tumors. In cases where total resection carries too much risk considering the patient’s age, the tumor’s location, or the level of the tumor-affected spinal segment, subtotal resection is a practical choice that yields a favorable long-term outcome if the tumor growth rate is low.
References
Conti P, Pansini G, Mouchaty H, Capuano C, Conti R. Spinal neurinomas: retrospective analysis and long-term outcome of 179 consecutively operated cases and review of the literature. Surg Neurol. 2004;61:34–43. (discussion 4).
Asazuma T, Toyama Y, Maruiwa H, Fujimura Y, Hirabayashi K. Surgical strategy for cervical dumbbell tumors based on a three-dimensional classification. Spine (Phila Pa 1976). 2004;29:E10–4.
Jiang L, Lv Y, Liu XG, Ma QJ, Wei F, Dang GT, Liu ZJ. Results of surgical treatment of cervical dumbbell tumors: surgical approach and development of an anatomic classification system. Spine (Phila Pa 1976). 2009;34:1307–14.
Klekamp J, Samii M. Surgery of spinal nerve sheath tumors with special reference to neurofibromatosis. Neurosurgery. 1998;42:279–89. (discussion 89–90).
Lot G, George B. Cervical neuromas with extradural components: surgical management in a series of 57 patients. Neurosurgery. 1997;41:813–20. (discussion 20–2).
McCormick PC. Surgical management of dumbbell tumors of the cervical spine. Neurosurgery. 1996;38:294–300.
Celli P. Treatment of relevant nerve roots involved in nerve sheath tumors: removal or preservation? Neurosurgery. 2002;51:684–92. (discussion 92).
Kim P, Ebersold MJ, Onofrio BM, Quast LM. Surgery of spinal nerve schwannoma. Risk of neurological deficit after resection of involved root. J Neurosurg. 1989;71:810–4.
Schultheiss R, Gullotta G. Resection of relevant nerve roots in surgery of spinal neurinomas without persisting neurological deficit. Acta Neurochir (Wien). 1993;122:91–6.
Fassett DR, Clark R, Brockmeyer DL, Schmidt MH. Cervical spine deformity associated with resection of spinal cord tumors. Neurosurg Focus. 2006;20:E2.
Sciubba DM, Chaichana KL, Woodworth GF, McGirt MJ, Gokaslan ZL, Jallo GI. Factors associated with cervical instability requiring fusion after cervical laminectomy for intradural tumor resection. J Neurosurg Spine. 2008;8:413–9.
Asazuma T, Nakamura M, Matsumoto M, Chiba K, Toyama Y. Postoperative changes of spinal curvature and range of motion in adult patients with cervical spinal cord tumors: analysis of 51 cases and review of the literature. J Spinal Disord Tech. 2004;17:178–82.
Watanabe M, Sakai D, Yamamoto Y, Iwashina T, Sato M, Mochida J. Upper cervical spinal cord tumors: review of 13 cases. J Orthop Sci. 2009;14:175–81.
Zhao B, Xu J. Extensive posterolateral exposure and total removal of the giant extraforaminal dumbbell tumors of cervical spine: surgical technique in a series of 16 patients. Spine J. 2009;9:822–9.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Nakamura, M., Iwanami, A., Tsuji, O. et al. Long-term surgical outcomes of cervical dumbbell neurinomas. J Orthop Sci 18, 8–13 (2013). https://doi.org/10.1007/s00776-012-0300-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-012-0300-2