Abstract
Introduction
Traditional surgical strategies for dumbbell neuroblastoma entail, among others, high risk of spinal deformity. Less invasive procedures might reduce these sequelae, however, there is small evidence comparing different strategies. Indications of minimally invasive surgery in neuroblastoma are still developing. Our aim is to identify and analyze different surgical approaches described in the recent literature and to suggest a minimally invasive option.
Methods
A systematic review of the literature was conducted in PubMed (Jan 2000–Dec 2021) to identify reports describing surgical resection of dumbbell neuroblastoma in children, according to the PRISMA guidelines. Only full-text articles were included.
Results
7 articles met the inclusion criteria which, added to the present case, represent a total of 43 patients. All were retrospective studies, most of them small series. Tumor location was mostly thoracic. Most of combined approaches were performed in two stages. Spinal deformity after surgery was reported in 3 patients. Minimally invasive approach was described in only one paper, with no reported cases of its use in a single-stage combined surgery. We also report, to our knowledge, the first single-stage posterior neurosurgical approach combined with thoracoscopy for resection of a dumbbell neuroblastoma in an infant.
Conclusion
Surgical resection of dumbbell neuroblastomas is challenging. There is no consensus on best surgical approach. Dumbbell tumors should not be considered a contraindication for minimally invasive surgery. A single stage and minimally invasive strategy is proposed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroblastoma represents 8–10% of all pediatric cancers, with a mean age at diagnosis of 20 months. This malignant neoplasm originates from neural crest cells and arises from the sympathetic nervous system. Dumbbell neuroblastoma occurs when a tumor arising from the sympathetic chain extends through the intervertebral foramina causing spinal cord compression, and the tumor has intra- and extraspinal component. It accounts for 5–15% of all cases of neuroblastoma [1]. Patients may present with symptoms of motor and sensitive deficit, sphincter dysfunction, or pain [2, 3]. The overall survival is reported as > 90% in the recent publications, as corresponds to paravertebral location [4], which usually entails favorable biology and low or intermediate risk group patients. However, the rate of severe neurological sequelae at short- and long-term remains very high [1, 5].
Over time, different treatment modalities have been used (surgery, radiotherapy, and chemotherapy), but there is still no consensus regarding the best approach for these patients. There is significant controversy regarding the surgical indication in these cases, but there is little evidence regarding the techniques used. If surgery is needed, the most common approach to date is a midline posterior incision first, for laminectomy or laminoplasty, followed by a posterolateral thoracotomy (and/or laparotomy) as separate procedures, or more seldom, in one single stage [1].
Almost 50% of patients with spinal compression by neuroblastoma develop scoliosis [5]. Spinal deformity is a possible long-term effect of laminoplasty and radiotherapy, but thoracotomy has also been described as an isolated risk factor for scoliosis [6]. To reduce these sequelae, thoracoscopy seems an interesting option [7, 8], adding the classical benefits of minimal invasive approach (less pain, shorter hospital stay, or reduced bleeding) [9].
In this review, we analyze the most recent literature regarding surgical techniques for pediatric dumbbell neuroblastoma and we describe, to our knowledge, the first single-stage resection of a dumbbell neuroblastoma in an infant through a combined approach (neurosurgical and thoracoscopic).
Methods
A systematic literature research was performed to identify different surgical techniques descried in the literature for resection of dumbbell neuroblastoma in children.
We also describe, to our knowledge, the first minimally invasive single-stage surgical approach for a thoracic dumbbell neuroblastoma. A literature search of similar approaches (including adults and children) for other tumors invading the spinal canal, was also performed.
Data sources and search strategy
A systematic literature review was conducted on PubMed from 2000 to 2021 using the terms “neuroblastoma surgery” AND “intraspinal involvement OR dumbbell”, in accordance with the PRISMA reporting checklist [10]. The last search was performed in February 2021.
Eligibility criteria
Inclusion criteria consisted of all papers published in English or Spanish language containing pediatric patients (0–18 years-old) affected of neuroblastoma with intraspinal involvement and that provided description of the surgical technique. Full-text articles were assessed for eligibility. Among the selected papers, we analyzed only those patients up to 18 years with diagnosis of neuroblastoma.
Data collection
From the selected articles, we collected the data regarding study characteristics, neurological symptoms at diagnosis, surgical approaches, spinal deformity and neurological sequelae after surgery. Any disagreement was discussed and resolved between the different authors.
Results
Regarding dumbbell neuroblastoma, a total of 69 potentially relevant articles were identified. After reading the abstract, 53 were excluded. Of the 16 articles selected for full-text reading 7 met the inclusion criteria. The search strategy used is detailed in Fig. 1.
The series of Sandberg et al. [11] was initially considered for inclusion in the review. This study reports 42 procedures in 30 patients: 21 single stage and 9 multiple procedures. Although it is a large interesting series, it was finally excluded because the approach undertaken in each patient is not explained in detail.
All papers were case reports (3) or retrospective reviews (4). Although some of the papers included adult patients and tumors with different histology, we analyzed only those up to 18 years with diagnosis of neuroblastoma, accounting for 43 cases of interest (including the present case), ranging from 2 months to 18 years of age: Hussein (n = 5), Pio (n = 32), Yiin (n = 1), Yang (n = 1), Yahya (n = 1), Kattepura (n = 1), Yilmaz (n = 1), and the present case (n = 1). Table 1 summarizes the most relevant information. Tumor location was most frequently thoracic (22/43; 51.2%). A limiting factor in this review is that most articles do not provide information on tumor biology, staging, or treatment protocol.
When analyzing surgical techniques, 9 patients (20.9%) did not require a neurosurgical procedure, 2 (4.7%) only underwent neurosurgical resection and in 10 cases (23.3%) both intra and extraspinal component were removed through one single approach, in some cases requiring widening of the intervertebral foramina. From those undergoing combined approaches (neurosurgical and transcavitary), making 51.16% of the patients, this was performed as a single stage in 5 (22.7%) of them, two stages in 14 (63.6%) and three or more in 3 (13.6%). Neurosurgical procedures where commonly the first to be performed (63.6%). Interestingly, from those patients who only had extraspinal canal surgery, only 2 (22.2%) were operated with a minimally invasive approach. In total, a minimally invasive approach was described in only one paper (3 thoracoscopies) [1], 2 did not even require neurosurgery and the last one underwent separately thoracoscopy after the previous neurosurgical resection.
The survival rate at the last follow-up was 88.4%. 5 patients died; 3 due to metastatic progression and 2 secondarily to chemotherapy toxicity.
Case presentation
An 11-month-old boy, with an unremarkable past medical history, was referred to our center after ultrasonographic discovery of a right paravertebral mass. The reason for consultation was a lump on his back noticed by his parents.
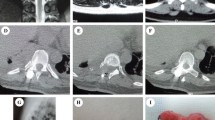
Physical examination demonstrated a hard, nonmobile and painless mass in the right paraspinal region. Neurological examination showed no impairment. An MRI revealed a 65 × 63 × 45 mm solid mass in the right paravertebral region with intraspinal extension from D7 to D10 (Fig. 2A). The tumor displaced anteriorly the inferior vena cava and contacted the descending thoracic aorta. The right paravertebral muscles were invaded. The image suggested a neuroblastoma occupying ¾ of the spinal canal, with abnormal signal of the spinal cord. Owing to the presence of this image-defined risk factor (IDRF) the tumor was then classified as L2, according to the International Neuroblastoma Risk Group Staging System (INRGSS).
A MRI at diagnosis showing a solid paravertebral mass (red arrows) extending over D8/D9 and D9/D10, producing compression of the spinal cord (yellow arrow). B MRI performed after chemotherapy shows reduction in tumor size with persistant intraspinal component, affecting more than 1/3 of the canal. C Postsurgical MRI
Laboratory examination showed elevated levels of lactate dehydrogenase (761 UI/L), alkaline phosphatase (838 UI/L), and neuron specific enolase (58.5 ng/mL). Urine catecholamine testing was normal.
An ultrasound guided needle biopsy was performed. The histopathology confirmed a differentiating neuroblastoma with low mitosis-karyorrhexis index. Genetic analysis showed no MYCN amplification and the presence of several numeric chromosomal aberrations, but also several segmental chromosomal aberrations (SCA) were present: + 1p11.1qter, + 8p23.2pter, and + 18q22.1qter. There was not loss of heterozygosity.
The bone marrow was not infiltrated and the 123I-MIBG scan revealed no metastatic lesions.
The patient was treated as per group 3 of the LINES protocol of the International Society of Pediatric Oncology Europe Neuroblastoma (SIOPEN), starting treatment based on the Carboplatin and Etoposide.
An MRI performed after four chemotherapy cycles demonstrated a marked reduction in the volume of the paravertebral tumor (60%) as well as of the intraspinal component, but the latter was still significative, affecting 1/3 of the spinal canal at D8/D9 and D9/D10 (Fig. 2B). The MDT decided to administer one more cycle of chemotherapy based on Vincristine, Cyclophosphamide and Adriamycin. However, the patient developed significant hematological toxicity and febrile neutropenia and the tumor response at this point was not improving further. Therefore, surgical resection of the lesion was decided by the multidisciplinary team.
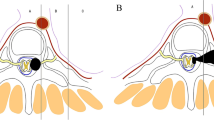
The surgical technique consisted in a combined single-staged approach. First, the Pediatric Neurosurgical team, through a posterior approach, performed D8-D9 right laminectomies and D10 hemilaminectomy and removed completely the intraspinal component of the tumor. Therefore, laminoplasty was carried out using absorbable plates of Poly-d, l-Lactic Acid (Resorb x®, KLS Martin, Germany) to provide stability (Fig. 3A). The second part of the surgery was performed by the Pediatric Surgical Oncology team. The child was positioned in the left lateral decubitus position with left bronchial selective intubation. A 3-port 5 mm thoracoscopy was performed. Adhesions secondary to chemotherapy were removed using bipolar diathermy. The parietal pleura was incised and the extraspinal intrathoracic part of the tumor was completely resected and extracted though an enlarged trocar incision inside an EndoBag. A 10Fr chest tube was placed (Fig. 3B). The patient had an excellent postoperative course with no complications, and was discharged home on the 4th postoperative day. Complete resection was confirmed on MRI (Fig. 2C).
After 12 months of follow-up, there are no signs of relapse on MRI and the patient is completely asymptomatic with no signs of neurological impairment, spinal deformity or other complications.
Discussion
Patients affected of dumbbell neuroblastoma are usually younger at diagnosis and they have more favorable histology, less MYCN amplification and less metastatic disease [2, 4]. For that reason, this group of patients have generally better outcomes in terms of survival [1, 3]. However, the risk of neurological sequelae is high (17–69% of neurological motor deficit, 9–50% of bladder and 4–29% of bowel disfunction and up to 80% of spinal deformity) [3]. This fact highlights the importance of an early diagnosis and treatment with the aim of avoiding permanent neurological impairment.
Dumbbell tumors have intraspinal and extraspinal components connected through the intervertebral foramina, making surgical resection challenging. Different operative techniques have been previously described for resection of dumbbell tumors, either by single posterior approach, thoracotomy, or a combination of both [7, 8, 12, 13]. Most of these treatments associate significant complications. Purely posterior thoracotomy usually includes extensive bone resection with laminectomy, facetectomy, and/or costotransversectomy which frequently entails postoperative pain, disability, and spinal instability [7, 14]. Even though a combined approach requires two incisions, changing the patient’s position and availability of two surgical teams, laminectomy followed by thoracotomy or thoracoscopy allows a less aggressive neurosurgical resection, reducing the risk of damaging nervous structures, and spinal instability [15,16,17,18]. Moreover, laminoplasty with instrumented fixation provides greater stability to the spine and appears to reduce the risk of deformity [19].
In this review, 3 cases of spinal deformity are reported: one hyperlordosis after lumbotomy, one scoliosis after 2 stage neurosurgery and laparotomy and one kyphosis after thoracotomy followed by neurosurgery [1].
Regarding neurological sequelae, Pio et al. reported 16 patients suffering neurological impairment after surgery, most of them (13) presenting symptoms prior to the intervention [1]. Kattepura et al. described mild weakness dorsiflexion of the left foot in a patient who required multilevel laminectomy (L5-S2), after 1 year of follow-up [20].
Although the indication for resecting the extraspinal part of the tumor is well defined, controversy remains on which patients could benefit from neurosurgical removal of the intraspinal component and when is the best moment to perform it. It seems beneficial in patients with rapid progression of neurological symptoms despite initial medical treatment and also in those in whom intraspinal component remains as an IDRF after chemotherapy [1, 5]. In the largest series to date [1], published by the group of Sarnacki, it was found that there is a high risk of local relapse and medullary compression if tumor remnant after chemotherapy occupied more than 1/3 of the spinal canal, as was our case. This, together with the biology of the tumor (with the presence of several SCA), prompted us to attempt a complete resection. In any case, MDT discussion of each patient and treatment in experienced reference centers (through national referral pathways or through European Reference Network PaedCan) is highly recommended.
In this review we found that in most cases of combined approach the intraspinal component was the first to be removed. This is consistent with current trends to avoid injuring the spinal cord. Pio et al. describe a case of paraplegia after primary resection of the extraspinal component due to diffusion of edema in the spinal canal, requiring emergent neurosurgery [1].
Thoracoscopy has demonstrated equivalent surgical results and overall survival outcomes than thoracotomy for resection of thoracic neuroblastomas. Moreover, studies have shown that minimally invasive surgery results in less postoperative pain, decreased length of hospital stay and less blood loss than open surgery [9, 13, 21]. Even though MIS is becoming very popular for NB resection, in our review we only found three cases in which thoracoscopy was performed. Furthermore, two of them did not require neurosurgery, so only the extracanal component was excised. The remaining case received a thoracoscopy as a third step after a transcavitary and a neurosurgical approach. Therefore, we found no reports of minimally invasive surgery for a single stage combined approach.
Although this combined approach (single-stage neurosurgical resection of the intracanal component associated to minimally invasive surgery of the extraspinal intrathoracic component) has been described before for other types of intraspinal lesions (mostly adult benign tumors) [15,16,17,18, 22] (Table 2), to our knowledge, this is the first pediatric case of thoracic dumbbell neuroblastoma treated with such strategy.
In our patient, complete resection of the tumor was possible. Nevertheless, considering the favorable biology of most of these tumors and the risk of neurosurgical damage, a subtotal resection in selected cases is advisable and provides similar survival rates [1].
So far, our patient has not developed any neurological sequelae or chest wall deformity. Nonetheless, long-term follow-up of both neoplastic disease and possible complications from surgery is important since these can appear several years later [5].
Conclusions
There is insufficient evidence to recommend one surgical approach over another. In our patient, single-stage neurosurgical and thoracoscopic resection with laminoplasty for treatment of a dumbbell pediatric thoracic tumor was feasible and showed the benefits of minimally invasive surgery. This strategy might reduce long-term sequelae, such as scoliosis or thoracic deformities. Prospective multicentric studies are needed to confirm which is the best and less aggressive surgical strategy.
Abbreviations
- IDRF:
-
Image-defined risk factor
- INRGSS:
-
International Neuroblastoma Risk Group Staging System
- SCA:
-
Segmental chromosomal aberrations
- SIOPEN:
-
International Society of Paediatric Oncology Europe Neuroblastoma Group
References
Pio L, Blanc T, de Saint DT, Irtan S, Valteau-Couanet D, Michon J, et al. Multidisciplinary surgical strategy for dumbbell neuroblastoma: a single-center experience of 32 cases. Pediatr Blood Cancer. 2019. https://doi.org/10.1002/pbc.27670.
De Bernardi B, Quaglietta L, Haupt R, Castellano A, Tirtei E, Luksch R, et al. Neuroblastoma with symptomatic epidural compression in the infant: the AIEOP experience: neuroblastoma and symptomatic epidural compression. Pediatr Blood Cancer. 2014;61(8):1369–75.
Kraal K, Blom T, van Noesel M, Kremer L, Caron H, Tytgat G, et al. Treatment and outcome of neuroblastoma with intraspinal extension: a systematic review. Pediatr Blood Cancer. 2017;64(8):e26451.
Brisse HJ, Blanc T, Schleiermacher G, Mosseri V, Philippe-Chomette P, Janoueix-Lerosey I, et al. Radiogenomics of neuroblastomas: relationships between imaging phenotypes, tumor genomic profile and survival. PLoS ONE. 2017;12(9):e0185190 (Baudis M, editor).
Angelini P, Plantaz D, De Bernardi B, Passagia J-G, Rubie H, Pastore G. Late sequelae of symptomatic epidural compression in children with localized neuroblastoma. Pediatr Blood Cancer. 2011;57(3):473–80.
Westfelt JN, Nordwall A. Thoracotomy and scoliosis. Spine (Phila Pa 1976). 1991;16(9):1124–5. https://doi.org/10.1097/00007632-199109000-00019.
McGirt MJ, Garcés-Ambrossi GL, Parker SL, Sciubba DM, Bydon A, Wolinksy J-P, et al. Short-term progressive spinal deformity following laminoplasty versus laminectomy for resection of intradural spinal tumors. Neurosurgery. 2010;66(5):1005–12.
Li C, Ye Y, Gu Y, Dong J. Minimally invasive resection of extradural dumbbell tumors of thoracic spine: surgical techniques and literature review. Eur Spine J. 2016;25(12):4108–15.
Malek MM, Mollen KP, Kane TD, Shah SR, Irwin C. Thoracic neuroblastoma: a retrospective review of our institutional experience with comparison of the thoracoscopic and open approaches to resection. J Pediatr Surg. 2010;45(8):1622–6.
Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, Stewart G, et al. Preferred reporting items for a systematic review and meta-analysis of individual participant data: the PRISMA-IPD statement. JAMA. 2015;313(16):1657.
Sandberg DI, Bilsky MH, Kushner BH, Souweidane MM, Kramer K, Laquaglia MP, et al. Treatment of spinal involvement in neuroblastoma patients. Pediatr Neurosurg. 2003;39(6):291–8.
Chen S, Wang Y, Su G, Chen B, Lin D. Primary intraspinal dumbbell-shaped mesenchymal chondrosarcoma with massive calcifications: a case report and review of the literature. World J Surg Onc. 2016;14(1):203.
Barrenechea IJ, Fukumoto R, Lesser JB, Ewing DR, Connery CP, Perin NI. Endoscopic resection of thoracic paravertebral and dumbbell tumors. Neurosurgery. 2006;59(6):1195–202.
Cabrera JP, Torche E, Luna F, Alarcón E, Spencer ML, López E, et al. Upper thoracic dumbbell-shaped tumor resected in one stage posterior approach: case report. AME Case Rep. 2019;3:25–25.
Okada D, Koizumi K, Haraguchi S, Hirata T, Hirai K, Mikami I, et al. A case of dumbbell tumor of the superior mediastinum removed by combined thoracoscopic surgery. J Nippon Med Sch. 2002;69(1):58–61.
Gámez García P, de Pablo GA, Salas Antón C, Santolaya Cohen R, Madrigal Royo L, Varela de Ugarte A. Angiolipoma mediastínico en reloj de arena. Arch Bronconeumol. 2002;38(11):545–6.
Vallières E, Findlay JM, Fraser RE. Combined microneurosurgical and thoracoscopic removal of neurogenic dumbbell tumors. Ann Thorac Surg. 1995;59(2):469–72.
Pojskić M (2018) Spinal Dumbbell Epidural Hemangioma: Two Stage/Same Sitting/Same Position Posterior Microsurgical and Transthoracic Endoscopic Resection – Case Report and Review of the Literature. ACC [Internet]. Available from: https://hrcak.srce.hr/index.php?show=clanak&id_clanak_jezik=318004. Accessed 2021 Jun 13
Wang H, Huo Y, Li L, Liu X, Yang D, Ding W, et al. (2020) Clinical Efficacy of Laminectomy with Instrumented Fixation in Treating Thoracolumbar Intradural Extramedullary Schwannomas: A Comparative Study. Med Sci Monit [Internet]. Available from: https://www.medscimonit.com/abstract/index/idArt/921719. Accessed 2021 Jun 13
Kattepura S, Alexander B, Kini U, Das K. Sporadic synchronous ganglioneuromas in a child—case report and review. J Pediatr Surg. 2010;45(4):822–5.
Ezekian B, Englum BR, Gulack BC, Rialon KL, Kim J, Talbot LJ, et al. Comparing oncologic outcomes after minimally invasive and open surgery for pediatric neuroblastoma and Wilms tumor. Pediatr Blood Cancer. 2018;65(1):e26755.
Ohya J, Miyoshi K, Kitagawa T, Sato Y, Maehara T, Mikami Y. Combined video-assisted thoracic surgery and posterior spinal surgery for the treatment of dumbbell tumor of the first thoracic nerve root. Asian Spine J. 2015;9(4):595.
Yahya FS, Al-Shami HA. Posterior mediastinal neuroblastoma masked as flaccid paraparesis in a 3 year child. Neurosci J. 2019;24(4):320–3.
Hussein HA. Paravertebral neurogenic tumors with intraspinal extension: preoperative evaluation and surgical approach. J Egypt Natl Cancer Inst. 2009;21:11.
Yiin J-J, Chang C-S, Jan Y-J, Wang Y-C. Treatment of neuroblastoma with intraspinal extensions. J Clin Neurosci. 2003;10(5):579–83.
Yang M, Wang X, Li J, Xiong G, Lu C, Lü G. Surgical treatment of large abdominally involved primary dumbbell tumor in the lumbar region. J Spinal Disord Tech. 2014;27(7):E268–75.
Yilmaz B, Toktas ZO, Akakin A, Demir MK, Yapicier O, Konya D. Lumbar spinal immature ganglioneuroma with conus medullaris invasion: case report. Pediatr Neurosurg. 2015;50(6):330–5.
Li Y, Wang B, Li L, Lü G. Posterior surgery versus combined laminectomy and thoracoscopic surgery for treatment of dumbbell-type thoracic cord tumor: a long-term follow-up. Clin Neurol Neurosurg. 2018;166:31–5.
Citow JS, Macdonald RL, Ferguson MK. Combined laminectomy and thoracoscopic resection of a dumbbell neurofibroma: technical case report. Neurosurgery. 1999;45(5):1263–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval is not required in this case since this is a systematic review of the literature and a retrospective case report. Regarding the clinical practice, all treatments were carried out according to most recent official guidelines.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martos, M., Cano, P., Molino, J.A. et al. Minimally invasive surgery for pediatric dumbbell neuroblastoma: systematic literature review and report of a single-stage neurosurgical and thoracoscopic approach. Clin Transl Oncol 24, 950–957 (2022). https://doi.org/10.1007/s12094-021-02724-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-021-02724-4