Abstract
Purpose
Dumbbell-shaped thoracic tumors represent a distinct type of tumor and involve in both the spinal canal and the posterior thoracic cavity. Successful treatment for the tumors depends on gross total resection (GTR) via an open laminectomy and facetectomy or transthoracic transpleural approach. In this case series, we report our experiments with minimally invasive method for the removal of extradural dumbbell thoracic tumor and present related literature review.
Methods
We retrospectively reviewed two patients with dumbbell-shaped thoracic tumors who underwent minimally invasive resection and unilateral transforaminal thoracic intervertebral fusion (TTIF) through unilateral paraspinal muscle approachwith a spotlight expandable tubular retractor. Clinical data, tumor characteristics, and outcomes were analyzed.
Results
Two patients underwent successful minimally invasive treatment of their spinal neoplasms. There were no procedure-related complications. The efficacy in terms of neurological recovery, pain improvement and operative variables (length of incision, operative duration, blood loss, and hospital stay) was better when compared with prior published studies. Postoperative CT image demonstrated complete resection of dumbbell tumor in the patients. The solid fusion was obtained after 3 months follow-up and there was no failure of internal fixation.
Conclusion
If the medial border of intracanal component of extradural dumbbell tumor is near the midline of canal and the pedicles of adjacent vertebrae to tumor are intact, minimally invasive resection of tumor through unilateral paraspinal muscle approach combined with unilateral TTIF is good choice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal dumbbell-shaped tumor is characterized by growing inside and outside of the spinal canal by a connection through the foramen, and approximately 90 % is nerve sheath tumor (NST) arising from the spinal nerve sheath, in which neurofibroma and shwannomas make up the vast majority with ganglioneuromas and malignant NST being far less common [1, 2]. The NSTs are most often seen in the cervical or lumbar region, followed by the thoracic region [3]. Typically, they are found on the dorsal sensory roots. More than half of all these lesions are extramedullary intradural, about 25 % are completely extradural, some (15 %) are both intra- and extradural, and very rarely they are seen intramedullary (<1 %) [4]. Although majority (>90 %) of spinal NSTs are benign neurogenic tumors, these tumors can compress nerve root and spinal cord, resulting in severe neurological symptoms, including pain, or neurological deficits [4].
The conventional gross total resection (GTR) for the lesions of spinal dumbbell tumor include posterior, combined posterior and anterior, posterolateral, transthoracic transpleural approaches [5, 6]. However, these operations have significant morbidity related to the surgical approach, potential blood loss, or extensive dissection. Especially, the risk of postoperative complications deriving from injury of paraspinal tissue is also of concern. A safe operative approach to these tumors is essential. The thoracolumbar paraspinal sacrospinalis muscle-splitting approach can provide a good exposure for the foramen and unilateral lamina. Recent studies have suggested that minimally invasive removal of these tumors using expandable tubular retractors though the paraspinal muscle could get a satisfying result [6].
The dumbbell tumor of thoracic, especially for upper thoracic tumor, has certain characteristic features not shared by its counterparts in the other regions of the vertebral column, which presents an increased difficult of surgery [7]. In current literature, the treatment of dumbbell thoracic tumor has not been methodically addressed nor given more attention due to their rarity. We reported two cases of minimally invasive removal of dumbbell thoracic tumors and unilateral transforaminal thoracic intervertebral fusion (TTIF) through unilateral paraspinal muscle approach with an expandable tubular retractor. The feasibility, safety and efficacy of this method are discussed. This report raised an important issue regarding the treatment of dumbbell thoracic tumors with a minimally invasive approach.
Material and method
Case report
Case 1
A 46-year-old woman presented with a 2-year history of chest pain, stufly, zonesthesia and even dyspnea. These symptoms were refractory to medical therapy. Neurological examination showed that there was no sensory loss and weak muscle strength found in double lower limbs. On MRI, an expansive, well-circumscribed, encapsulated dumbbell-shaped extradural lesion (35 × 25 × 15 mm) was found at the right T9–T10 level (Fig. 1a–c), which presented hyper-signal in T2W and hypo-signal in T1W. The globoid mass was seen with contiguous intracanal, foraminal, and extraspinal components. There was no infiltrative or invasive lesion seen.
Pre-operative a coronal and b axial MRI, c axial CT show a thoracic dumbbell-shaped tumor of T9/10 in Case 1. d–f CT scan and g lateral X-ray picture after minimally invasive removal of dumbbell thoracic tumor and unilateral TTIF present that the dumbbell tumor is completely removed and the screws and cage are all properly positioned. h Photography shows minimally invasive result 6 months after surgery. i The picture is the gross observation of completely removed tumor (ganglioneuromas)
Case 2
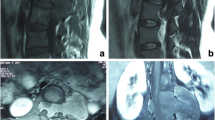
The patient was a man of 18 years old with chest pain, zonesthesia and walking instability for 6 weeks, and dysuria for 2 days. Double lower limbs had weak muscle strength and there was sensory loss below the level of xiphoid. The MRI showed an expansive extradural dumbbell-shaped tumor (45 × 35 × 35 mm) at the right T5–T6 level (Fig. 2a–c), which demonstrated high signal intensity in T2W and isointensity in T1W. Neurological elements were compressed by the intracanal component of dumbbell tumor.
Pre-operative a coronal and b axial MRI, c axial CT show a thoracic dumbbell-shaped tumor of T5/6 in Case 2. d–f CT scan and g lateral X-ray picture after minimally invasive removal of dumbbell thoracic tumor and unilateral TTIF present good position of pedicle screws and cage and complete removal of the dumbbell tumor. h Photography shows minimally invasive result 6 months after surgery. i The picture is the gross observation of completely removed tumor (schwannomas)
Inclusion criteria were that the medial border of intracanal component of extradural dumbbell tumor was near the midline of canal on MRI and the pedicles of adjacent vertebrae to tumor were intact on CT.
Operative technique
The patients with thoracic dumbbell-shaped tumor were electively operated by the senior author (YT.G) using a minimally invasive approach with an expandable tubular retractor. Patient consent and clinical information were obtained under the guidelines of the institutional review board.
Anesthesia and positioning
After sedation and endotracheal intubation, the patient was moved into the prone position on a radio-lucent operating table. Arterial line was placed for blood pressure monitoring. The posterior thoracolumbar area was subsequently sterilized and draped after the skin was dried.
Surgical procedure
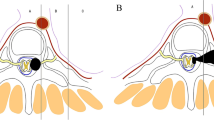
The precise location of the tumors was confirmed with a K-wire under anteroposterior intraoperative fluoroscopy. At this level, an about 30-mm-long paramedian skin incision was carried out 2 cm lateral off the midline. This paramedian longitudinal incision satisfied the adequate angle to directly access the ipsilateral thoracic extraforaminal space. Then, the thoracic fascia was incised parallel to the skin incision. The paraspinal sacrospinalis muscle-splitting approach was performed to expose the unilateral lamina, superior articular facet and transverse process of two involved vertebra [8, 9]. The entry site to the pedicle was located at the junction between the lateral border of the superior articular facet and the superior 1/3 line of the transverse process. Once the pedicle has been identified, either a pedicle probe or a hand-held curet was used to enter the pedicle. Preoperative anteroposterior and lateral roentgenograms and CT scans through the pedicles of the vertebral body to be instrumented were studied to determine the correct angle of entry in both the coronal and sagittal planes. The pedicle integrity was verified in all four quadrants to be sure that a solid tube of bone exists and that violation into the spinal canal or inferiorly into the neuroforamen has not occurred. Two pedicle screws of appropriate length were then introduced into the vertebral body via the pedicle to engage at least 75 % of the vertebral body anterior-posterior width. Posteoanterior and lateral fluoroscopic picture were taken to confirm their position (Fig. 3a, b).
Procedure of minimally invasive removal of dumbbell thoracic tumor and unilateral TTIF intraoperative a posteoanterior and b lateral fluoroscopic pictures show insertion of pedicle screws into the involved vertebrae under direct vision through unilateral paraspinal muscle approach. c Photography and d schematic diagram present the removal of dumbbell-shaped tumor through an expandable tubular retractor. e Fluoroscopic picture documents that the cage is implanted into the intervertebral space through the expandable tubular retractor
The series of dilators through the access were used to introduce an expandable tubular retractor into target area, which was fixed with a table mounted flexible arm. The involved hemilamina and unilateral facet joint were removed to expose intracanal and intraforaminal component of dumbbell tumor. And then, the lateral paraspinal muscle and intercostal muscle were subperiosteally elevated to expose the costotransverse joint and rib. The transverse process and rib were removed to dissect extraspinal component of tumor off the thoracic pleura. GTR of dumbbell tumor was performed, and attention was paid to protect the neurological elements and reserve the nerve root involved as much as possible (Fig. 3c, d). The pleura should be repaired if pleura breakage occurs. Then, the cage filled with autograft bone was transforaminally inserted into intervertebral space after the disc and endplate cartilage were removed (Fig. 3e). The rod of appropriate size was contoured and fixed over two pedicle screws after removing the retractor. The fascia was closed with absorbable sutures, and the paramedian skin incision was intradermally closed with 4–0 Vicryl sutures after the drainage tube had been positioned. The thin tube for closed thoracic drainage should be inserted if there was obvious pneumothorax or hydrothorax on the X-ray immediately after surgery in operation room.
Clinical follow-up
Two patients were observed for clinical assessment immediately, 1 week, 1, 3, 6 and 12 months after surgery. The pain intensity in the previously symptomatic region was graded with visual analog scale pain scores (VAS). A neurologic examination was performed before and after treatment in two patients. The severity of the neurologic deficit was assessed by using the ASIA impairment scale [10]: a (complete impairment), no motor or sensory function is preserved in segments S4 through S5; B (incomplete impairment), sensory but not motor function is preserved below the neurologic level and includes segments S4 through S5; C (incomplete impairment), motor function is preserved below the neurologic level and more than half of key muscles below the neurologic level have a muscle grade of less than 3; D (incomplete impairment), motor function is preserved below the neurologic level and at least one-half of key muscles below the neurologic level have a muscle grade of 3 or more; and E (normal impairment), motor and sensory function are normal.
The postoperative X-ray and CT scan were taken 1 week, 1, 3, 6 and 12 months after surgery.
Result
GTR of the dumbbell thoracic tumor was performed without sacrificing any nerve root. The completely extradural location of the tumor, as previewed on the preoperative diagnostic images, was corroborated with the intraoperative findings. There were no procedure-related complications. The postoperative CT image and X-ray showed that the dumbbell tumor was completely removed and the screws and cage were all properly positioned in two cases (Figs. 1d–g, 2d–g). The solid fusion was obtained after 3 months follow-up and there was no failure of internal fixation.
Case 1
The length of incision was 30 mm (Fig. 1h). The operative duration was 150 min and the estimated total blood loss was 200 ml without transfusion. In the immediate postoperative period the patient had complete resolution of some symptoms such as chest stufly, zonesthesia and dyspnea. She was discharged home, neurologically intact, on the third postoperative day. The patient returned to regular activities within 4 weeks. The VAS score dropped from 7 preoperatively to 2 immediately after surgery and to 0 at 1-year follow-up. The patient presented with normal neurological function (ASIA scale E) preoperatively and postoperatively. Histopathological analysis of the resected lesion demonstrated a benign ganglioneuromas in the patient (Fig. 1i).
Case 2
The incision length was 32 mm (Fig. 2h) and the duration of operation was 170 min. There was blood loss of 250 ml without transfusion. Although the pleura breakage occurred during the procedure, there was no obvious pneumothorax or hydrothorax on the X-ray immediately after surgery and closed thoracic drainage was not performed. The stay at hospital was 6 day. The VAS score was 6 before surgery, 1 immediately after surgery and 0 at 1-year follow-up. Improvement of paraplegia was observed from ASIA scale D before operation to E at 3-month follow-up. Histopathological evaluation showed schwannomas for the resected tumor (Fig. 2i).
Discussion
Dumbbell-shaped thoracic tumor represent a distinct type of tumor and can grow to involve the posterior thoracic cavity, which has certain characteristic features not shared by its counterparts in the other regions of the vertebral column [6, 11]. Due to the specific anatomic relationship with surrounding tissue, the extraspinal component of dumbbell tumor in thoracic spine is larger than that in cervical and lumbosacral region. Standard resection of dumbbell thoracic tumor typically entails a posterior midline approach with a relatively long incision and muscle dissection from the underlying lamina, spinous process, facet joint, and transverse process [6, 11]. A laminectomy and radical facetectomy are usually performed to access the intracanal and foraminal component of the tumor [12, 13]. However, the procedure usually results in spinal instability and deformity. Fusion surgery has thus been required for dumbbell tumor removal associated with radical facetectomy. In addition, complete removal often necessitates sacrifice of a nerve root and causes permanent deficits. Serious delayed morbidity includes dysesthesia, arachnoiditis, and cystic myelopathy [14].
In addition, for most thoracic tumors wholly confined to the chest wall, a video-assisted thoracoscopic surgery (VATS) via the thoracic cavity is advocated to carry out [15]. However, if a portion of the tumor extends into the spinal canal, the situation becomes quite different. Although the transthoracic approach has sometimes been employed for these dumbbell-shaped tumors, resection of the intraspinal component of tumor is difficult without laminectomy. Ghostines et al. demonstrated a thoracoscopic surgery was safety and effectiveness in treating the thoracic dumbbell nerve sheath tumors. Ohya et al. performed successfully a combined VATS and posterior spinal surgery for the treatment of thoracic dumbbell tumors [15]. Tanaka et al. treated successfully a woman with dumbbell-shaped thoracic neurinoma by combining hemilaminectomy and thoracoscopic surgery [16]. However, conventional open approach for treatment of extradural tumors results in iatrogenic complications, such as positively pain, spinal deformity, instability, and neurological deterioration. In addition, the thoracoscopic surgery usually results in pulmonary complication, intercostal neuralgias, and shoulder girdle dysfunction.
In recent years, minimally invasive surgery has been successfully used on the resection of spinal tumors, and the results, when compared with standard open approaches, demonstrated reduced soft tissue destruction (muscle atrophy and denervation), blood loss, and length of hospitalization [17–20]. Tredway et al. published their study including a series of six patents with intradural tumors and demonstrated that minimally invasive approaches are safe and effective with comparable resection and complication rates when compared to historical control. However, the data about the suitability of this approach for extradural or intradural–extradural tumors was rare so far [19]. A study published in 2011 by Haji et al. highlighted the minimally invasive technique with expandable tubular was carried out for the treatment of extradural, intradural–extramedullary, and intramedullary spinal tumors [17]. In their case series, GTR was achieved in all patents (five in the lumbar spine and one thoracic) and the comparable results such as blood loss, operative time, hospitalization days, and narcotic usage were acceptable in comparison to prior reported data with standard open techniques. Nzokou et al. reported their experiment involving a series of consecutive patients who underwent minimally invasive resection with nonexpandable tubular retractors [18]. In their study, GTR was achieved except one thoracic tumor, in which the tumor capsule was adherent to the diaphragm. In addition, less tissue destruction and quicker functional recovery were obtained with minimally invasive approach in comparison to open or mini-open technique. However, the spinal instrumentation has not been performed in the minimally invasive surgery, which might result in spinal instability and long-term spinal deformity.
The minimally invasive technique with the tubular retractor has not yet successfully been used in dumbbell thoracic tumor. In the present study, minimally invasive resection of tumor and unilateral TTIF were firstly performed to treat dumbbell thoracic tumor. The optimal surgical approach for tumor resection mainly depends on some factors including location, extension, size and the relation with neural compartments. In our cases, if the medial border of intracanal component of extradural dumbbell tumor was near the midline of canal on MRI and the pedicles of adjacent vertebrae to tumor were intact on CT, minimally invasive removal of hemilamina, unitlateral facet, transverse process, rib, tumor, and unilateral TTIF through unilateral paraspinal muscle approach with a spotlight expandable tubular retractor thus were recommended. The minimally invasive surgery can protect the attachment of paraspinal muscle to bone, supraspinous and interspinous ligaments, contralateral paraspinal muscle, lamina and facets. It can minimize incision length, decrease operative duration, reduce blood loss, and shorten hospital stay. In addition, it is very convenient to implant the pedicle screws through the paraspinal approach and unilateral TTIF can save the costs of patients. The minimally invasive surgery avoids transthoracic surgery and related complications.
The feasibility, safety and efficacy after operation is also a concern. The feasibility and relative safety of minimally invasive surgery were confirmed by the fact that postoperative radiographs and scanographic images showed that the screws and cage were all properly positioned in the present series of patients. None of the patients were found to have any postoperative neurological complications. Like all surgical interventions, pedicle screw stabilization is not devoid of risks, since it can cause nerve injuries. The pedicle must be carefully probed in all four quadrants to be sure that a solid tube of bone exists and that violation into the spinal canal or inferiorly into the neuroforamen has not occurred before the pedicle screws were implanted into the vertebrae with minimally invasive technique under direct vision in our study. These measures were taken to avoid the occurrence of neurological deficits and guarantee the safety of operation. The efficacy in two patients in terms of neurological recovery, pain improvement and operative variables (length of incision, operative duration, blood loss, and hospital stay) was better when compared with prior published studies. The postoperative CT image showed that the dumbbell tumor was completely removed in our two cases. In addition, the solid fusion was obtained after 3 months follow-up and there was no failure of internal fixation. These results indicated that the TTIF provided an adequate mechanical support, which was similar with the efficacy of unilateral TLIF [21].
Some scholars advocate that except for the cervico-thoracic and the thoraco-lumbal levels, the thoracic spine stability provided by rib cage usually compensates the resection of a facet joint. Stillerman et al. reported that the transfacettal approach was performed to treat the thoracic disc herniations without any additional fixation although the biomechanical quality of the disc should not be intact any more. They emphasized sparing the lateral aspect of the facet joint to avoid destabilization of the thoracic spine [22]. However, Bransford et al. suggested that the addition of an instrumented arthrodesis created a controlled environment for healing, facilitated mobilization, and allowed for maintenance of a physiological thoracic alignment with reasonable procedural safety. In addition, coexisting deformity can be corrected with the addition of a posterior segmental instrumentation [23]. In our study, the involved hemilamina and unilateral facet joint were completely removed to resect intracanal and intraforaminal component of dumbbell tumor, which destroyed the biomechanical stability of spine less or more. Additional unilateral TTIF could minimize the risk of secondary instability, deformity and continued spinal cord irritation after the resection of dumbbell tumor, and help to prevent postoperative axial back pain resulting from the potential increase in motion following the complete removal of facet joint, especially in the lower thoracic spine where the main motion segment was located. Meanwhile, the patients were allowed to mobilize as early as possible after thoracic dumbbell tumor resection and unilateral TTIF. It was worth mentioning that the unilateral TTIF was performed through the same incision with the tumor resection, which only devoted the limited additional trauma to the procedure.
We also realize the limitation of this report that the size of cases is too small and there is no control group. Further study should be performed to collect more cases and compare this technique with open posterior surgery, transthoracic operation or VATS.
Conclusion
If the medial border of intracanal component of extradural dumbbell tumor is near the midline of canal and the pedicles of adjacent vertebrae to tumor are intact, minimally invasive resection of tumor through unilateral paraspinal muscle approach combined with unilateral TTIF is good choice.
References
Celli P, Trillo G, Ferrante L (2005) Extrathecal intraradicular nerve sheath tumor. J Neurosurg Spine 3:1–11
Jinnai T, Hoshimaru M, Koyama T (2005) Clinical characteristics of spinal nerve sheath tumors: analysis of 149 cases. Neurosurgery 56:510–515. doi:10.1227/01.neu.0000153752.59565.bb
Van Goethem JW, van den Hauwe L, Ozsarlak O, De Schepper AM, Parizel PM (2004) Spinal tumors. Eur J Radiol 50:159–176. doi:10.1016/j.ejrad.2003.10.021
Hioki A, Miyamoto K, Hirose Y, Kito Y, Fushimi K, Shimizu K (2012) Cervical symmetric dumbbell ganglinoeuromas causing severe paresis. Asian Spine J 8:74–78
Gu BS, Park JH, Roh SW, Jeon SR, Jang JW, Hyun SJ, Rhim SC (2014) Surgical strategies for removal of intra- and extraforaminal dumbbell-shaped schwannomas in the subaxial cervical spine. Eur Spine J. doi:10.1007/s00586-014-3458-9
Tomii M, Itoh Y, Numazawa S, Watanabe K (2013) Surgical consideration of cervical dumbbell tumors. Acta Neurochir (Wien) 155:1907–1910. doi:10.1007/s00701-013-1787-9
Ito K, Aoyama T, Kuroiwa M, Horiuchi T, Hongo K (2014) Surgical strategy and results of treatment for dumbbell-shaped spinal neurinoma with a posterior approach. Br J Neurosurg 28:324–329. doi:10.3109/02688697.2013.835372
Gu YT, Zhu DH, Liu HF, Zhang F, McGuire R (2015) Minimally invasive pedicle screw fixation combined with percutaneous vertebroplasty for preventing secondary fracture after vertebroplasty. J Orthop Surg Res 10:31. doi:10.1186/s13018-015-0172-1
Gu Y, Zhang F, Jiang X, Jia L, McGuire R (2013) Minimally invasive pedicle screw fixation combined with percutaneous vertebroplasty in the surgical treatment of thoracolumbar osteoporosis fracture. J Neurosurg Spine 18:634–640. doi:10.3171/2013.3.SPINE12827
Association ASI (2003) Reference manual of the international standards for neurological classification of spinal cord injury. American Spinal Injury Association, Chicago
Varga PP, Szoverfi Z, Lazary A (2014) Surgical treatment of primary malignant tumors of the sacrum. Neurol Res 36:577–587. doi:10.1179/1743132814Y.0000000366
Gu R, Liu JB, Xia P, Li C, Liu GY, Wang JC (2014) Evaluation of hemilaminectomy use in microsurgical resection of intradural extramedullary tumors. Oncol Lett. doi:10.3892/ol.2014.1949
Turel MK, D’Souza WP, Rajshekhar V (2015) Hemilaminectomy approach for intradural extramedullary spinal tumors: an analysis of 164 patients. Neurosurg Focus 39:E9. doi:10.3171/2015.5.FOCUS15170
Masahiro K, Yutaka I, Daisuke S, Nahoko M, Masatsugu K, Hajime H (2005) Treatment of thoracolumbar fractures with vertebroplasty in combination with posterior instrumentation. Neurosurg Q 15:181–185
Ohya J, Miyoshi K, Kitagawa T, Sato Y, Maehara T, Mikami Y (2015) Combined video-assisted thoracic surgery and posterior spinal surgery for the treatment of dumbbell tumor of the first thoracic nerve root. Asian Spine J 9:595–599
Tanaka T, Kato N, Aoki K, Nakamura A, Watanabe M, Tochigi S, Marushima H, Akiba T, Hasegawa Y, Abe T (2012) Combined unilateral hemilaminectomy and thoracoscopic resection of the dumbbell-shaped thoracic neurinoma: a case report. Case Rep Neurol Med 2012:517563. doi:10.1155/2012/517563
Haji F, Cenic A, Crevier L, Murty N, Reddy K (2011) Minimally invasive approach for the resection of spinal neoplasm. Spine 36:1018–1026
Nzokou A, Weil AG, Shedid D (2013) Minimally invasive removal of thoracic and lumbar spinal tumors using a nonexpandable tubular retractor. J Neurosurg Spine 19:708–715. doi:10.3171/2013.9.SPINE121061
Tredway T, Santiago P, Hrubes M, Song J, Christie S, Fessler R (2006) Minimally invasive resection of intradural–extramedullary spinal neoplasms. Neurosurgery 58:52–58. doi:10.1016/j.joca.2014.02.004
Goncalves VM, Santiago B, Ferreira VC, Cunha ESM (2014) Minimally invasive resection of an extradural far lateral lumbar schwannoma with zygapophyseal joint sparing: surgical nuances and literature review. Case Rep Med 2014:739862. doi:10.1155/2014/739862
Hao D, Wang W, Duan K, Ma M, Jiang Y, Liu T, He B (2014) Two-year follow-up evaluation of surgical treatment for thoracolumbar fracture-dislocation. Spine 39:E1284–E1290. doi:10.1097/BRS.0000000000000529
Stillerman CB, Chen TC, Day JD, Couldwell WT, Weiss MH (1995) The transfacet pedicle-sparing approach for thoracic disc removal: cadaveric morphometric analysis and preliminary clinical experience. J Neurosurg 1995:971–976
Bransford R, Zhang F, Bellabarba C, Konodi M, Chapman JR (2010) Early experience treating thoracic disc herniations using a modified transfacet pedicle-sparing decompression and fusion. J Neurosurg Spine 2010:221–231. doi:10.3171/2009.9.SPINE09476
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
C. Li and Y. Ye contributed equally to this work.
Rights and permissions
About this article
Cite this article
Li, C., Ye, Y., Gu, Y. et al. Minimally invasive resection of extradural dumbbell tumors of thoracic spine: surgical techniques and literature review. Eur Spine J 25, 4108–4115 (2016). https://doi.org/10.1007/s00586-016-4677-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4677-z