Abstract
Introduction
This multicenter, retrospective study aimed to clarify the changes in postoperative care provided by orthopaedic surgeons after hip fractures and clarify the incidence of secondary fractures requiring surgery.
Materials and methods
Subjects were patients with hip fracture treated surgically in seven hospitals during the 10-year period from January 2008 to December 2017. Data on patient demographics, comorbidities, preoperative and postoperative osteoporosis treatments, and secondary fractures were collected from the medical records.
Results
In total, 4764 new hip fractures in 982 men and 3782 women (mean age: 81.3 ± 10.0 years) were identified. Approximately 10% of patients had a history of osteoporosis drug treatment and 35% of patients received postoperative drug treatment. The proportion of patients receiving postoperative drug therapy increased by approximately 10% between 2009 and 2010, 10% between 2010 and 2011, and 10% between 2011 and 2013. Although the rate of secondary fractures during the entire period and within 3 years decreased from 2011, the rate of secondary fracture within 1 year remained at around 2% every year.
Conclusions
The approval of new osteoporosis drugs and the establishment of osteoporosis liaison services have had a positive effect on the use of postoperative drug therapy in the orthopedic field. Our finding that the rate of secondary fracture within 1 year of the initial fracture remained around 2% every year, despite improvements in postoperative drug therapy, suggests that both rehabilitation for preventing falls and early postoperative drug therapy are essential to prevent secondary fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are associated with increased morbidity, functional decline, and death in older adults, as well as increased use of health care services in most industrialized countries [1, 2]. It is estimated that the number of hip fractures worldwide will rise from 1.7 million in 1990 to 6.3 million in 2050 [3]. In particular, given that three-quarters of the world’s population lives in Asia, it is projected that Asian countries will contribute more to the pool of hip fractures in the coming years. By 2050, more than 50% of all osteoporotic fractures will occur in Asia [4, 5]. According to a nationwide survey of hip fractures in Japan, the total number of patients who experienced a hip fracture in 2012 was 175,700 (men, 37,600; women, 138,100), which represents an increase from 2007 (total, 148,100; men, 31,300; women, 116,800) [6, 7]. The annual costs of medical and nursing care associated with osteoporotic fractures have been estimated to be JPY 797.4 to 989.5 billion (US$7.974 to 9.895 billion; US$1 = JPY100) in Japan [8] and are expected to rise in parallel with the increase in the incidence of osteoporotic fractures.
Patients with hip fractures have a 2.5-fold increased risk of secondary fractures compared to age-matched persons without previous fractures [9]. More specifically, patients who have sustained one hip fracture have a higher risk of a contralateral hip fracture compared to the general populations [10], and second hip fractures often occur within 1 year of initial fractures [11, 12]. Treatment with anti-osteoporosis drugs is essential for patients after their initial fracture, as a first fracture is the highest risk factor for a second fracture [13, 14]. Nevertheless, data suggest that few patients with hip fracture actually received pharmacologic therapy for osteoporosis [15,16,17,18]. Therefore, poor persistence with osteoporosis treatments is a global public health problem.
Recently, various anti-osteoporosis drugs have been developed and are available on the market. In Japan, teriparatide (TPD), recombinant human parathyroid hormone (1–34), and denosumab (DSMAB), a fully human monoclonal antibody that binds the cytokine receptor activator of NFκB ligand (RANKL), were approved in 2010 and 2013, respectively. Additionally, based on the fracture liaison services (FLS) [19, 20], a coordinator-based secondary fracture prevention service developed in the United Kingdom; the osteoporosis liaison service (OLS) was established in Japan in 2012 as a comprehensive care system for osteoporosis. On the contrary, in Japan, hip fractures are usually treated by orthopedic surgical procedures and followed with postoperative therapy by the same orthopedic surgeon, not a physician specializing in osteoporosis treatment. Therefore, it is of great importance to assess how postoperative care after hip fracture that is provided by an orthopedic surgeon has changed now that various anti-osteoporosis drugs have been approved and the OLS has been established.
The objectives of this multicenter retrospective study were to investigate the rate of postoperative care change after hip fracture and the incidence of secondary fractures requiring surgery. The hypothesis of this study is that development of anti-osteoporosis drugs and dissemination of knowledge about treatment for osteoporosis among surgeons has improved the treatment rate for bone fragility and the prevention of secondary fractures.
Materials and methods
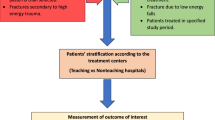
This study was designed as a retrospective, registry-based, uncontrolled, follow-up study. This study was approved by the local ethics committee at the Hokkaido University Hospital (017-0448) and by each participating hospital. A total of 4803 hip fracture patients treated with surgery at seven hospitals that function as base hospitals in regional cities in Hokkaido prefecture in Japan during the 10-year period from January 2008 to December 2017 were included. Data were collected from medical records. Thirty-nine patients who were younger than 50 years were excluded. Finally, 4764 patients (male, 982; female, 3782) were included in this current study. Three of the seven hospitals carried out OLS.
Data on patient demographics including age, sex, and body mass index (BMI), comorbidities including diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), malignant tumor, and rheumatoid arthritis, and glucocorticoid use, preoperative medical history for osteoporosis drugs including bisphosphonate (BP), selective estrogen receptor modulator (SERM), TPD and DSMAB, and calcium (Ca) or active vitamin D3 preparation at surgery were collected from their medical records. Data on postoperative osteoporosis treatment, osteoporosis inspection (dual-energy X-ray absorptiometry), outpatient visits after discharge, the occurrence of a secondary fracture (contralateral hip fracture, distal radial fracture and proximal humerus fracture) requiring surgery, and follow-up period after the initial surgery were also collected from medical records.
Chi-squared or independent t tests were used to compare differences in subject demographics. The incidence of secondary fracture was estimated by the Kaplan–Meier method, and differences were investigated by the log-rank test among the patients who could be followed. All statistical analyses were performed using SPSS Statistics version 23.0 (IBM Corporation, Armonk, NY) with a significance level set at 0.05.
Results
Patient demographics and osteoporosis care during the whole period
In this study, the number of the hip fractures treated with the surgery in this study gradually increased during the entire period (Fig. 1). Table 1 shows a summary of patient demographics. Male patients with hip fracture were significantly younger than the female patients (P < 0.001). A significantly higher proportion of male patients experienced COPD and malignant tumors compared to female patients (P < 0.001). In contrast, a significantly higher proportion of female patients experienced rheumatoid arthritis (RA) compared to male patients (P = 0.024). Preoperatively, 8.4% of patients underwent osteoporosis drug therapy and 6.3% took active vitamin D3 or Ca preparations. Postoperatively, 13.0% of patients underwent osteoporosis inspection, 34.2% underwent osteoporosis drug therapy, and 12.6% took active vitamin D3 or Ca preparations. A significantly lower proportion of male patients underwent preoperative and postoperative inspection and therapy compared to female patients (P < 0.001). Postoperatively, 35.7% of patients attended outpatient visits after discharge, 4.1% sustained a secondary fracture, and 2.0% had a secondary fracture within 1 year of the initial fracture. The mean follow-up period was 25.8 months. There were no significant differences in these parameters between male and female patients.
Patients who underwent preoperative drug therapy were older than those who did not (P < 0.001) (Table 2). Significantly more patients who underwent preoperative osteoporosis drug therapy experienced RA and used glucocorticoid steroids (GCs) compared to those who did not (P < 0.001). The proportion of patients who underwent postoperative osteoporosis inspection, took active vitamin D3 or Ca preparations, and attended outpatient visits after discharge was higher in patients who received preoperative drug therapy compared to those who did not (P < 0.001). Although 1278 patients of 4360 patients (29.3%) who did not receive preoperative therapy started drug therapy postoperatively, 51 patients of 404 patients (12.2%) who received preoperative therapy did not continue drug therapy. No differences in the incidence of secondary fracture and secondary fracture within 1 year and 3 years, or the duration between the initial and secondary fractures were found in patients who underwent preoperative drug therapy and those who did not.
Changes in postoperative osteoporosis care over time (2008–2017)
The proportion of patients who received postoperative osteoporosis drug therapy increased by approximately 10% from 2010 (when TPD was approved), 2011 and 2013 (when DSMAB was approved) compared with their proportion in the preceding (Fig. 2). The proportion of patients who received preoperative osteoporosis drug therapy was around 5%. The majority of the postoperative drug therapy involved BP (over 80%) (Fig. 3). The proportion of TPD and DSMAB administration increased slowly after approval. On the contrary, the proportion of postoperative osteoporosis inspection and outpatient visits after discharge increased gradually from 2014 (Fig. 2). The proportion of patients who took Ca or active vitamin D3 was 5–10% until 2012, increased gradually and reached around 20% in 2017. One hospital started OLS from 2012 and the other two hospitals stared it from 2015. There were totally 1295 patients who received OLS. The hospitals operating OLS exhibited higher proportion of postoperative therapy compared to those without OLS (Fig. 4).
Longitudinal trends in postoperative osteoporosis care during the whole period. Black circle, proportion of patients who received preoperative drug therapy; white circle, proportion of patients who received postoperative drug therapy; square, proportion of patients who received postoperative inspection; triangle, proportion of patients who attended outpatient appointments after discharge. TPD teriparatide, OLS osteoporosis liaison service
Longitudinal trends in postoperative osteoporosis drug therapy during the whole period. Black circle, proportion of patients who received postoperative bisphosphonate (BP) therapy; white circle, proportion of patients who received postoperative selective estrogen receptor modulator (SERM) therapy; square, proportion of patients who received postoperative teriparatide (TPD) therapy; triangle, proportion of patients who received postoperative denosumab (DSMAB) therapy
Efficacy of postoperative osteoporosis drug therapy
Patients who received postoperative drug therapy were significantly more likely to have received preoperative drug therapy and take Ca or active vitamin D3 preparations compared to those who did not receive postoperative drug therapy (Table 3). Of the 1631 patients who received postoperative osteoporosis drug therapy, 509 patients (31.2%) underwent postoperative inspection, and 728 patients (44.6%) attended outpatient appointments after discharge. These proportions were significantly higher compared to patients who did not receive postoperative drug therapy. On the contrary, no significant differences in the occurrence of secondary fractures, occurrence of secondary fractures within 1 year of the initial fracture, or duration between initial and secondary fractures were noted in patients who had received postoperative drug therapy and those who had not.
The 120-month cumulative incidence of secondary fracture was estimated to be 23.9% in patients with postoperative therapy and 32.5% in those without postoperative therapy, with a difference between the two groups, albeit not statistically significant (P = 0.057, log-rank test) (Fig. 5). Although the prevalence of secondary fractures during the whole period and within 3 years of initial surgery decreased from 2011, the prevalence of secondary fractures occurring within 1 year was around 2% every year (Fig. 6). No significant differences in the occurrence of secondary fractures, occurrence of secondary fractures within 1 year of the initial fracture, or duration between initial and secondary fractures were found in patients who had received postoperative Ca or active vitamin D3 preparations and those who had not.
Longitudinal trends in secondary fractures during the whole period. White circle, proportion of patients who sustained a secondary fracture; white square proportion of patients who had a secondary fracture within 3 years of the initial hip fracture; black circle, proportion of patients who suffered a secondary fracture within 1 year of the initial hip fracture. Fx fracture
Discussion
This multicenter retrospective study addressed the changes in approaches to postoperative osteoporosis treatment. The finding of this current study that the total number of hip fractures increased over 10 years is consistent with the overall trend of increase due to the aging population in Japan [21]. Although the majority of the postoperative drug therapy involved bisphosphonate over the whole period, the proportion of patients undergoing postoperative drug therapy and inspection and the number of patients attending outpatient visits after discharge increased gradually. Considering that the proportion of the secondary fracture within 3 years clearly decreased from 2011, when the proportion of the postoperative drug therapy got increased, the improvement of the postoperative therapy could be considered to have a positive effect for preventing the secondary fracture.
The increase in the proportion of drug therapy demonstrated in this study is consistent with the recent Japanese report [22], suggesting that orthopedic surgeons are promoting awareness of osteoporosis interventions after the first fragility fractures much better. In North America, several studies have recommended that the orthopedic surgeon directly treating the fracture should perform a BMD examination and forward the results to the primary care physician following the course of osteoporosis treatment [23,24,25]. Additionally, Miki et al. showed improved rates of early osteoporosis drug treatment following hip fractures when osteoporosis education was initiated by the treating orthopedic surgeon while the patient is still in the hospital and the treatment is initiated in an orthopedic osteoporosis clinic [25]. The main limitation of this multicenter retrospective therapy was that the time of starting OLS and insurance medical treatment system, such as on diagnosis procedure combination system, varies with each hospital. The finding of this study that almost all postoperative therapy in the entire period was BP and TPD and DSMAB might not contribute directly to the increase in postoperative therapy as expected might be affected by the medical care system in Japan. However, considering that the rates of postoperative osteoporosis drug therapy increased by approximately 10% in 2010, 2011, and 2013 and the differences in the proportions of postoperative therapy between hospitals with and without OLS, the approval of new osteoporosis drugs and the establishment of OLS programs could have a further positive effect on the administration of postoperative drug therapy in patients with the hip fracture. The finding of this study that the proportion of the postoperative osteoporosis inspection has risen since 2014 could also be considered to be the effect of OLS.
Our finding that postoperative drug therapy showed a trend to reduce the secondary fracture is consistent with the previous prospective cohort studies about the efficacy of bisphosphonate for preventing a secondary hip fracture [26, 27]. Because less than half of the patients who received postoperative drug therapy attended outpatient visits after discharge in this study, the discrepancy of efficacy for preventing the secondary fracture between this study and these previous prospective cohort studies might be explained by the differences in follow-up rate, as well as the study design. More specifically, the proportion of patients undergoing postoperative drug therapy was higher than the proportion of patients who attended outpatient appointments after discharge between 2011 and 2013, suggesting that the continuation of postoperative drug therapy might be more difficult in Japan compared to in the immediate postoperative period. Because the prescription of anti-osteoporosis therapy medications in rehabilitation hospitals is limited in Japan, modification of the care system as well as osteoporosis education for orthopedic surgeons might be necessary for the prevention of secondary fractures.
Our finding that half of patients with a secondary fracture experienced that fracture within 1 year of the initial hip fracture is consistent with the previous reports about the incidence of secondary hip fracture [28,29,30]. The reason for the transient marked increase in risk is not known, but immobilization and impaired coordination are potential factors [31, 32]. In contrast, our finding that the rate of secondary fracture within 1 year after the initial fracture remained around 2% every year, regardless of improvements in postoperative drug therapy, is contrary to the conclusion of the recent large cohort studies that reported immediate treatment after initial fracture can prevent a higher number of new fractures compared to when treatment is delayed [33, 34]. The discrepancy between this current study and other reports might be explained by a limitation of this study that we did not include all secondary fractures, but only those treated surgically. Considering Lyles’s report that there was no difference in new hip fracture occurrence within 1 year of the surgery [26], rehabilitation for preventing fall in addition to early postoperative drug therapy after surgery is essential for secondary fracture prevention.
Several other limitations need to be considered when interpreting the results of this study. First, in this study, patients who received BP therapy were not divided according to alendronate, risedronate, minodronate, ibandronate, and zoledronate therapy. Given the possibility of differences in adherence and absorptivity of each drug, future studies should address the efficacy and adherence of each individual drug. Second, because all data were collected retrospectively from medical records, adherence to therapy could not be investigated.
Third, other secondary fragility fractures such as distal radius, proximal humerus, and lumbar vertebrae fractures that do not require surgery were not investigated. Therefore, future prospective studies that focused on specific therapies might be necessary. Fourth, this study did not include dementia as a comorbidity. Dementia has reported to be a strong risk factor for hip fracture. In addition, the presence of dementia is expected to disturb the follow-up, nutritional instruction, and treatment compliance in osteoporotic patients. Fifth, although the participating hospitals were main hospitals in their cities, patients who received therapy from other hospitals in the same area may have been included.
Conclusions
Over the study period, the proportion of patients receiving postoperative drug therapy and inspection, and attending outpatient visits after discharge increased gradually in the north side of Japan. The approval of new osteoporosis drugs and establishment of OLS programs could have a further positive effect on postoperative drug therapy in the orthopedic field. Our finding that the proportion of secondary fractures within 1 year of the initial fracture remained around 2% every year, despite improvements in postoperative osteoporosis drug therapy, suggests that rehabilitation for preventing falls as well as early postoperative drug therapy after surgery, are essential for secondary fracture prevention.
References
Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA (1990) Hip fracture incidence among the old and very old: a population-based study of 745,435 cases. Am J Public Health 80:871–873
Boonen S, Autier P, Barette M, Vanderschueren D, Lips P, Haentjens P (2004) Functional outcome and quality of life following hip fracture in elderly women: a prospective controlled study. Osteoporos Int 15:87–94. https://doi.org/10.1007/s00198-003-1515-z
Sambrook P, Cooper C (2006) Osteoporosis. Lancet 367:2010–2018. https://doi.org/10.1016/S0140-6736(06)68891-0
Dhanwal DK, Dennison EM, Harvey NC, Cooper C (2011) Epidemiology of hip fracture: Worldwide geographic variation. Indian J Orthop 45:15–22. https://doi.org/10.4103/0019-5413.73656
Bhandari M, Swiontkowski M (2017) Management of acute hip fracture. N Engl J Med 377:2053–2062. https://doi.org/10.1056/NEJMcp1611090
Orimo H, Yaegashi Y, Onoda T, Fukushima Y, Hosoi T, Sakata K (2009) Hip fracture incidence in Japan: estimates of new patients in 2007 and 20-year trends. Arch Osteoporos 4:71–77. https://doi.org/10.1007/s11657-009-0031-y
Orimo H, Yaegashi Y, Hosoi T, Fukushima Y, Onoda T, Hashimoto T, Sakata K (2016) Hip fracture incidence in Japan: Estimates of new patients in 2012 and 25-year trends. Osteoporos Int 27:1777–1784. https://doi.org/10.1007/s00198-015-3464-8
Harada A, Matsui Y, Takemura M, Ito Z, Wakao N, Ota T (2005) Cost-utility analysis of osteoporosis. Nihon Ronen Igakkai Zasshi 42:596–608
Colon-Emeric C, Kuchibhatla M, Pieper C, Hawkes W, Fredman L, Magaziner J, Zimmerman S, Lyles KW (2003) The contribution of hip fracture to risk of subsequent fractures: data from two longitudinal studies. Osteoporos Int 14:879–883. https://doi.org/10.1007/s00198-003-1460-x
Hagino H, Sawaguchi T, Endo N, Ito Y, Nakano T, Watanabe Y (2012) The risk of a second hip fracture in patients after their first hip fracture. Calcif Tissue Int 90:14–21. https://doi.org/10.1007/s00223-011-9545-6
Yamanashi A, Yamazaki K, Kanamori M, Mochizuki K, Okamoto S, Koide Y, Kin K, Nagano A (2005) Assessment of risk factors for second hip fractures in Japanese elderly. Osteoporos Int 16:1239–1246. https://doi.org/10.1007/s00198-005-1835-2
Nymark T, Lauritsen JM, Ovesen O, Rock ND, Jeune B (2006) Short time-frame from first to second hip fracture in the Funen County Hip Fracture Study. Osteoporos Int 17:1353–1357. https://doi.org/10.1007/s00198-006-0125-y
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332:767–773. https://doi.org/10.1056/NEJM199503233321202
Gehlbach S, Saag KG, Adachi JD, Hooven FH, Flahive J et al (2012) Previous fractures at multiple sites increase the risk for subsequent fractures: the Global Longitudinal Study of Osteoporosis in Women. J Bone Miner Res 27:645–653. https://doi.org/10.1002/jbmr.1476
Solomon DH, Finkelstein JS, Katz JN, Mogun H, Avorn J (2003) Underuse of osteoporosis medications in elderly patients with fractures. Am J Med 115:398–400
Gardner MJ, Brophy RH, Demetrakopoulos D, Koob J, Hong R, Rana A, Lin JT, Lane JM (2005) Interventions to improve osteoporosis treatment following hip fracture. A prospective, randomized trial. J Bone Jt Surg Am 87:3–7. https://doi.org/10.2106/JBJS.D.02289
Colon-Emeric CS, Lyles KW, House P, Levine DA, Schenck AP, Allison J, Gorospe J, Fermazin M, Oliver K, Curtis JR, Weissman N, Xie A, Saag KG (2007) Randomized trial to improve fracture prevention in nursing home residents. Am J Med 120:886–892. https://doi.org/10.1016/j.amjmed.2007.04.020
Tsukutani Y, Hagino H, Ito Y, Nagashima H (2015) Epidemiology of fragility fractures in Sakaiminato, Japan: incidence, secular trends, and prognosis. Osteoporos Int 26:2249–2255. https://doi.org/10.1007/s00198-015-3124-z
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14:1028–1034. https://doi.org/10.1007/s00198-003-1507-z
Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE Jr, McLellan A, Mitchell PJ, Silverman S, Singleton R, Siris E, Prevention ATFoSF (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27:2039–2046. https://doi.org/10.1002/jbmr.1698
Hagino H, Endo N, Harada A, Iwamoto J, Mashiba T, Mori S, Ohtori S, Sakai A, Takada J, Yamamoto T (2017) Survey of hip fractures in Japan: recent trends in prevalence and treatment. J Orthop Sci 22:909–914. https://doi.org/10.1016/j.jos.2017.06.003
Iba K, Dohke T, Takada J, Sasaki K, Sonoda T, Hanaka M, Miyano S, Yamashita T (2018) Improvement in the rate of inadequate pharmaceutical treatment by orthopaedic surgeons for the prevention of a second fracture over the last 10 years. J Orthop Sci 23:127–131. https://doi.org/10.1016/j.jos.2017.09.008
Bogoch ER, Elliot-Gibson V, Beaton DE, Jamal SA, Josse RG, Murray TM (2006) Effective initiation of osteoporosis diagnosis and treatment for patients with a fragility fracture in an orthopaedic environment. J Bone Jt Surg Am 88:25–34. https://doi.org/10.2106/JBJS.E.00198
Rozental TD, Makhni EC, Day CS, Bouxsein ML (2008) Improving evaluation and treatment for osteoporosis following distal radial fractures. A prospective randomized intervention. J Bone Jt Surg Am 90:953–961. https://doi.org/10.2106/JBJS.G.01121
Miki RA, Oetgen ME, Kirk J, Insogna KL, Lindskog DM (2008) Orthopaedic management improves the rate of early osteoporosis treatment after hip fracture. A randomized clinical trial. J Bone Jt Surg Am 90:2346–2353. https://doi.org/10.2106/JBJS.G.01246
Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF et al (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357:1799–1809. https://doi.org/10.1056/NEJMoa074941
Osaki M, Tatsuki K, Hashikawa T, Norimatsu T, Chiba K, Motokawa S, Furuichi I, Doiguchi Y, Aoyagi K, Shindo H (2012) Beneficial effect of risedronate for preventing recurrent hip fracture in the elderly Japanese women. Osteoporos Int 23:695–703. https://doi.org/10.1007/s00198-011-1556-7
Dretakis KE, Dretakis EK, Papakitsou EF, Psarakis S, Steriopoulos K (1998) Possible predisposing factors for the second hip fracture. Calcif Tissue Int 62:366–369
Wiktorowicz ME, Goeree R, Papaioannou A, Adachi JD, Papadimitropoulos E (2001) Economic implications of hip fracture: health service use, institutional care and cost in Canada. Osteoporos Int 12:271–278. https://doi.org/10.1007/s001980170116
Chapurlat RD, Bauer DC, Nevitt M, Stone K, Cummings SR (2003) Incidence and risk factors for a second hip fracture in elderly women. The study of osteoporotic fractures. Osteoporos Int 14:130–136. https://doi.org/10.1007/s00198-002-1327-6
Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, Wong JB (2004) Effect of Vitamin D on falls: a meta-analysis. JAMA 291:1999–2006. https://doi.org/10.1001/jama.291.16.1999
van Helden S, Wyers CE, Dagnelie PC, van Dongen MC, Willems G, Brink PR, Geusens PP (2007) Risk of falling in patients with a recent fracture. BMC Musculoskelet Disord 8:55. https://doi.org/10.1186/1471-2474-8-55
Johansson H, Siggeirsdottir K, Harvey NC, Oden A, Gudnason V, McCloskey E, Sigurdsson G, Kanis JA (2017) Imminent risk of fracture after fracture. Osteoporos Int 28:775–780. https://doi.org/10.1007/s00198-016-3868-0
Kanis JA, Johansson H, Oden A, Harvey NC, Gudnason V, Sanders KM, Sigurdsson G, Siggeirsdottir K, Fitzpatrick LA, Borgstrom F, McCloskey EV (2018) Characteristics of recurrent fractures. Osteoporos Int 29:1747–1757. https://doi.org/10.1007/s00198-018-4502-0
Acknowledgements
This project was supported in part by a Grant-in-Aid for Young Scientists (B) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan 17K16670 (T. Shimizu).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shun Shimodan, Dai Sato, Kaname Takahashi, Ryosuke Hishimura, Masahiro Ota, Hirokazu Shimizu, Yuichi Hasegawa, Toshiya Chubachi, Takeru Tsujimoto, Yukinori Tsukuda, Tsuyoshi Asano, Daisuke Takahashi, Masahiko Takahata, Norimasa Iwasaki, Tomohiro Shimizu declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shun Shimodan and Dai Sato are first authors.
About this article
Cite this article
Shimodan, S., Sato, D., Takahashi, K. et al. Ten years change in post-fracture care for hip fracture patients. J Bone Miner Metab 38, 222–229 (2020). https://doi.org/10.1007/s00774-019-01047-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-019-01047-3