Abstract
Subjects affected by thalassemia major (TM) often have reduced bone mass and increased fracture risk. Strontium ranelate (SrR) is an effective treatment for postmenopausal and male osteoporosis. To date, no data exist on the use of SrR in the treatment of TM-related osteoporosis. Our aim was to evaluate the effects of SrR on bone mineral density (BMD), bone turnover markers and inhibitors of Wnt signaling (sclerostin and DKK-1). Twenty-four TM osteoporotic women were randomized to receive daily SrR 2 g or placebo in addition to calcium carbonate (1,000 mg) and vitamin D (800 IU). BMD at the lumbar spine and femoral neck, bone turnover markers (C-terminal telopeptide of procollagen type I [CTX], bone-specific alkaline phosphatase [BSAP]) and insulin-like growth factor-1 (IGF-1), sclerostin and DKK-1 were assessed at baseline and after 24 months. Back pain was measured by visual analog scale (VAS) every 6 months. After 24 months, TM women treated with SrR had increased their spine BMD values in comparison to baseline (p < 0.05). Moreover, they also exhibited a reduction of CTX and sclerostin levels (but not DKK-1) and exhibited an increase of BSAP and IGF-1 (p < 0.05); however, no significant changes were observed in the placebo group. In the SrR group, a reduction of back pain was observed after 18 months in comparison to baseline (p < 0.05) and after 24 months in comparison to placebo (p < 0.05). Our study reports for the first time the effects of SrR in the treatment of TM-related osteoporosis. SrR treatment improved BMD and normalized bone turnover markers, as well as lowering sclerostin serum levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Considerable morbidity in older subjects with thalassemia major (TM) results from bone disease due to osteoporosis which is often accompanied by disabling pain and fractures [1, 2].
The pathogenesis of osteoporosis in TM is complex and multifactorial. Bone marrow expansion due to ineffective erythropoiesis, endocrine dysfunction, as well as complications related to treatment all have detrimental effects on bone tissue [3–6].
Prevention of bone disease includes lifestyle adjustments (increased calcium intake and physical activity and refraining from smoking), adequate monitoring of iron-chelation, hormonal replacement therapy, and vitamin D supplementation. However, despite improved treatment for this hematologic disorder and its complications, TM patients exhibit unbalanced bone turnover, with increased bone resorption and decreased bone formation resulting in diminished bone mineral density (BMD) [7–10]. The RANK/RANK-L/OPG system has been recognized as a major regulator of osteoclast proliferation and activation, and its role has also been described in the pathogenesis of TM-induced osteoporosis [4]. Enhanced osteoclastic activity provides the rationale use of bisphosphonates (BPs), which are potent inhibitors of osteoclastic function, in the medical management of TM-induced osteoporosis [8–10].
In addition to increased bone resorption, reduced osteoblastic activity is believed to be a major determinant of bone loss in TM. The poor bone formation is proven by histomorphometric studies and is mainly caused by iron poisoning in osteoblasts and the reduced function of growth hormone and insulin-like growth factor-1 (IGF-1) axis [1, 5, 10].
The Wnt/β-catenin canonical pathway has been suggested to play a key role in bone remodeling, leading to increased proliferation and differentiation of osteoblast precursor cells, reducing apoptosis of mature osteoblasts and promoting the ability of differentiated osteoblasts to inhibit osteoclast differentiation [11, 12]. This pathway is modulated by a number of factors that include Dickkopf-1 (DKK-1) and sclerostin, which compete with Wnt/β-catenin for binding to LRP5/6, disrupting (Dkk-1) or antagonizing (sclerostin) LRP5/6-mediated Wnt signaling. Recently, sclerostin and DKK-1 were found to be increased in TM patients, highlighting a possible role of the Wnt pathway in the pathogenesis of TM-induced osteoporosis [13, 14].
Strontium ranelate (SrR) is a current treatment option for postmenopausal and male osteoporosis [15–17]. It has been proposed that SrR acts by simultaneously promoting bone formation and inhibiting bone resorption. This uncoupling of the bone remodeling process contributes to a net gain in BMD, an increase of bone strength and finally a fracture risk reduction [18–25].
SrR has been proven to influence various regulators of bone metabolism, i.e., IGF-1, RANKL/OPG, and Wnt signaling, that are involved in the pathophysiology of TM-induced osteoporosis [26, 27].
To our knowledge, no data are available about SrR treatment in patients with TM-induced osteoporosis. Therefore, the main aim of our study was to investigate the effects of SrR on BMD, bone remodeling markers and IGF-1, sclerostin and DKK-1 levels. Furthermore, we also considered back pain assessment, drug safety and tolerability in this population.
Materials and methods
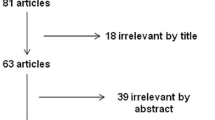
We studied a total of twenty-four TM women affected by osteoporosis, defined in accordance with WHO criteria [28]. Recruitment of these subjects was carried out at the Department of Clinical and Experimental Medicine of University Hospital of Messina between May 2008 and October 2009. Exclusion criteria were age <18 years, pregnancy, use of glucocorticoid, oral contraceptives or other bone active agents (e.g., BPs, selective estrogen receptor modulators, parathyroid hormone [PTH] or recombinant human PTH) in the past 6 months, chronic renal or liver failure, and celiac disease. All the patients had been maintained on a regular transfusion program and received oral deferiprone (75/mg/kg/day) as iron chelation treatment. Each patient gave written informed consent to participate in the study, which was conducted in accordance with the Declaration of Helsinki. Recruited subjects were randomized into two groups to receive either placebo or SrR 2 g/day for 24 months, administered at bedtime 2 h after dinner. All TM subjects also received a daily supplementation of calcium carbonate (1,000 mg) and cholecalciferol (800 IU) over the study period.
At baseline and at the end of the study, BMD and bone turnover markers were measured in all patients. BMD was assessed by dual-energy X-ray absorptiometry (DXA) densitometry (Hologic 4500 QDR) at the lumbar spine (L1–L4) in AP projection and at the femoral neck. The DXA densitometer was calibrated on a daily basis according to the manufacturer’s instruction and its coefficient of variation (CV) was 0.5 % with the standard phantom.
Serum levels of C-telopeptide of type 1 collagen (CTX) and bone-specific alkaline phosphatase (BSAP) were measured to evaluate bone resorption and bone formation, respectively. PTH, 25(OH)D, IGF-1, sclerostin and DKK-1 serum levels were also detected. Sclerostin and DKK-1were determined by enzyme immunoassay (Biomedica Medizinprodukte GmbH & Co KG, Vienna Austria) with intra-assay and inter-assay CV <7 % for both analytes. CTX was assessed using the Elecys 2010 Immunoassay System (Roche, Basel, Switzerland) with intra-assay CVs of 1.6–3 % and inter-assay CVs of 1.3–4.3 %. BSAP was measured by immunoenzymatic assay with the Access Immunoassay System (Beckman Coulter) with intra-assay and inter-assay CVs of 2.3–3.7 % and 4.9–9.8 %, respectively. Concentrations of IGF-1 were determined by RIA (DIAsource ImmunoAssays, Nivelles, Belgium) with within-assay and between-assay CVs of 1.7–9.1 % and 4.1–9.0 %, respectively.
At baseline and then every 6 months, TM subjects were asked to assign a score to back pain using a visual analog scale (VAS) (cm 0 = no pain, cm 10 = unbearable pain). Moreover, standard clinical and biochemical evaluations were carried out at baseline and then every 6 months to rule out any possible and detectable side-effects due to treatment.
A group of twenty healthy women matched for age and anthropometric data, recruited from our hospital staff, were considered as controls. Statistical analyses were performed using MedCalc (version 10.2.0.0; MedCalc Software, Mariakerke, Belgium). All values were expressed as mean ± SD. The normal distribution of values was verified with the Kolmogorov–Smirnov test. Differences were evaluated using the Student’s t test for paired and unpaired observations as appropriate. Pearson’s correlation was used to analyze the degree of association between two variables. Values of p < 0.05 were considered to indicate statistical significance.
Results
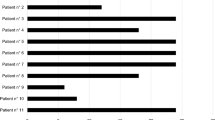
The clinical characteristics of the recruited TM women and healthy controls are shown in Table 1. Different from eugonadic controls, all TM subjects were postmenopausal women for at least 12 months, with a mean menopausal age of 35.2 ± 2.1 years. None of our recruited women were suffering from diabetes, hypothyroidism, hypoparathyroidism, or any cardiovascular diseases. In comparison to controls, TM women showed lower BMD values at the lumbar spine and femoral neck and higher CTX and lower BSAP levels; higher sclerostin and DKK-1 values and lower IGF-1 and PTH levels were also observed (p < 0.05). At baseline, no significant differences were detected between the main clinical characteristics of TM women receiving SrR or placebo. All TM subjects received previous treatment for osteoporosis (placebo group—3 alendronate, 3 risedronate, 3 neridronate, 3 clodronate; SrR group—3 alendronate, 2 risedronate, 4 neridronate, 3 clodronate). TM subjects received no more than 3 years of BP treatment over the past 5 years. With the exception of clodronate that was interrupted at least 6 months prior to the beginning of the study, the other BPs (alendronate, risedronate, neridronate) were stopped >12 months before enrolment.
At baseline, in the whole TM population, a positive association was observed between lumbar spine BMD and sclerostin (Fig. 1); lumbar spine BMD was also positively associated with IGF-1 levels and negatively associated with ferritin and DKK-1 levels (Fig. 1) (p < 0.05). Femoral neck BMD was not significantly related to the studied variables, and bone turnover markers were not significantly related to sclerostin and DKK-1.
After 24 months, the lumbar spine BMD did not change significantly in the TM women receiving placebo (Fig. 2), whereas lumbar spine BMD increased significantly in the SrR group (Fig. 2). No significant BMD change was observed at the femoral neck in both groups, although improvement of values was seen only in the SrR group (Fig. 2). In the SrR group only, bone turnover markers significantly changed, with a reduction of CTX and an increase of BSAP levels in comparison with baseline values; sclerostin levels were also reduced in the SrR group (Table 2). No modification of PTH, 25(OH)D or DKK-1 was observed in both groups after exposure to SrR or placebo (Table 2).
In the SrR group, we observed a negative correlation between changes in sclerostin and BSAP levels (r = −0.64, p = 0.023), and between BSAP changes and BMD gain at the femoral neck (r = 0.53, p = 0.08).
Back pain score was not significantly different at baseline in the placebo group in comparison to the SrR group (3.8 ± 0.9 vs 4.1 ± 0.8, respectively). After 18 months, in comparison to baseline values, a significant pain reduction was detected only in the SrR group (2.9 ± 0.7), and at the end of the study, back pain was significantly different between the groups (3.2 ± 0.7 vs 2.5 ± 0.7 in the placebo and SrR groups, respectively) (Fig. 3). No significant change in routine laboratory data, including liver and renal function tests were reported over the observation period (data not shown). No relevant side-effects were recorded apart from comparable incidences of self-limited gastrointestinal disorders (nausea, diarrhea, dyspepsia) within the first 6 months which occurred in two subjects in both groups. In particular, no subjects developed heart or circulatory problems, such as uncontrolled high blood pressure or angina or venous thromboembolism, and no clinical fractures were recorded over the observation period. No subjects discontinued the study.
Discussion
As the longevity of patients with TM increases, osteoporosis is becoming a prominent problem [1, 9]. Because osteoporosis is a progressive disease, prevention, early diagnosis and treatment of the established disease are crucial to avoid fractures and preserve quality of life [29]. The maintenance of bone mass involves the balanced effects of bone-resorbing osteoclasts and bone-forming osteoblasts. Our study reports for the first time the effects of SrR in the treatment of TM-induced osteoporosis. Different from BPs which are antiresorptive agents, SrR has been suggested to exert anabolic effects on bone by osteoblast modulation [18, 21, 22] and, at the same time, an antiresorptive action by osteoclast inhibition [19–22]. It is thought that SrR increases preosteoblast proliferation, osteoblast differentiation, collagen type I synthesis, and bone matrix mineralization, probably through a calcium-sensing receptor-dependent mechanism. Moreover, inhibition of osteoclast differentiation and activity as a consequence of an increase in OPG and a decrease in RANKL levels was reported [22]. The concept of the dual action of SrR was recently discussed [23]. The greater breaking strength of bone treated with SrR may also be caused by the incorporation of strontium into hydroxyapatite crystals, so that the mechanism of action is largely linked to a physical effect [24].
In accordance with data from previous studies [30, 31], SrR administration in our study significantly increased the bone formation marker BSAP and reduced CTX. SrR normalized the rate of bone turnover, and caused a rise of BMD values at the lumbar spine and the femoral neck sites. Improvement of BMD in TM subjects receiving SrR was in line with findings from SOTI (Spinal Osteoporosis Therapeutic Intervention) and TROPOS (Treatment of Peripheral Osteoporosis) trials in a population of osteoporotic postmenopausal women [15, 16]. The increased BMD observed, however, is in part due to the higher atomic number of strontium compared to calcium which leads to greater attenuation of X-rays and an overestimation of BMD as measured by DXA [32].
As previously reported by Voskaridou et al., subjects with TM-induced osteoporosis showed higher values of soluble DKK-1 and sclerostin (which are well-characterized receptor inhibitors of the Wnt pathway in bone) when compared with healthy controls [13, 14]. In TM subjects, L1-L4 BMD was positively related to sclerostin, and this could be explained, at least in part, to the higher osteocyte number or osteocyte viability. Moreover, BMD was also inversely related to ferritin levels which could account for direct or indirect bone damage by iron overload. In fact, in vitro studies suggest that iron could reduce the expression of genes involved in bone matrix formation or reported to be involved in osteoblast differentiation [33].
In vitro, SrR was proven to promote canonical Wnt signaling in osteoblasts. This effect occurs at least in part via activation of an Akt-dependent signaling mechanism. SrR also suppresses sclerostin expression, an effect that would be expected to increase canonical Wnt signaling [26]. Taken together these results highlight a possible molecular mechanism for the enhanced bone formation rate seen in vivo with SrR. In accordance with these findings, SrR was able to reduce sclerostin serum levels, and possibly modulate osteoblast activity via Wnt signaling modulation in our TM patients. Women treated with SrR significantly improved their BMD at the lumbar spine, although the BMD gain at the femoral neck was not significant. This could be explained by the fact that prior BP exposure may blunt BMD response to SrR [34]. All our patients were previously treated with BPs for up to three years, although a wash-out period of at least 6 months was observed before entering the study. Our findings are consistent with the observations of Middleton et al. [34]. In fact, women exposed to SrR did not show a significant change in BMD at the femoral neck in comparison to baseline, but an overall increase in BMD was detected. Although TM subjects were supplemented with cholecalciferol, their 25(OH)D levels were not significantly improved by the treatment. This finding might have contributed to a reduced BMD gain of SrR at the femoral neck, in accordance with our previous observation in women with postmenopausal osteoporosis exposed to SrR [35].
Although not designed to look at cardiovascular end-points, our study showed that, in a selected population eligible for management with SrR according to the recommendations of the European Medicines Agency [36] and under regular medical control, SrR treatment was well tolerated and not complicated by any type of cardiovascular problems.
Treatment with SrR was associated with improvement of back pain, which is a symptom often reported by TM subjects. A significant reduction of back pain was observed after 18 months of treatment in TM subjects treated with SrR, but not in the placebo group. SrR was previously reported to prevent quality of life impairment in postmenopausal women with established vertebral osteoporosis [37]. Back pain reduction observed in our study, in addition to improvement of BMD and possibly a reduction of fracture risk, could be effective in the preservation of quality of life. Moreover, it could encourage adherence to treatment in TM women with osteoporosis.
We must recognize that our study has several limitations. The design excluded TM men who may also be at risk of developing osteoporosis and related fractures, the sample size was small, the use of BMD to measure SrR effects on bone, and the observation period was not long enough to account for fractures. At the same time, this is the first report on the effects of SrR in osteoporotic TM women, and a possible new mechanism of action of SrR, involving modulation of sclerostin levels, has been hypothesized. Our findings suggest that SrR may be an effective treatment for TM-related osteoporosis, but further studies aimed at fractures are required.
In conclusion, our study reported the effects of SrR in the treatment of TM-related osteoporosis for the first time. SrR treatment was well tolerated and caused an increase of BMD and normalization of bone turnover markers, as well as reducing sclerostin serum levels. A significant reduction of back pain was also detected.
References
Wong P, Fuller PJ, Gillespie MT, Kartsogiannis V, Kerr PG, Doery JC, Paul E, Bowden DK, Strauss BJ, Milat F (2014) Thalassemia bone disease: a 19 year longitudinal analysis. J Bone Miner Res 29:2468–2473
Ruggiero L, De Sanctis V (1998) Multicentre study on prevalence of fractures in transfusion-dependent thalassaemic patients. J Pediatr Endocrinol Metab 11:773–778
Lasco A, Morabito N, Gaudio A, Crisafulli A, Meo A, Denuzzo G, Frisina N (2002) Osteoporosis and beta-thalassemia major: role of the IGF-I/IGFBP-III axis. J Endocrinol Invest 25:338–344
Morabito N, Gaudio A, Lasco A, Atteritano M, Pizzoleo MA, Cincotta M, La Rosa M, Guarino R, Meo A, Frisina N (2004) Osteoprotegerin and RANKL in the pathogenesis of thalassemia-induced osteoporosis: new pieces of the puzzle. J Bone Miner Res 19:722–727
Mahachoklertwattana P, Sirikulchayanonta V, Chuansumrit A, Karnsombat P, Choubtum L, Sriphrapradang A, Domrongkitchaiporn S, Sirisriro R, Rajatanavin R (2003) Bone histomorphometry in children and adolescents with beta-thalassemia disease: iron-associated focal osteomalacia. J Clin Endocrinol Metab 88:3966–3972
Morabito N, Russo GT, Gaudio A, Lasco A, Catalano A, Morini E, Franchina F, Maisano D, La Rosa M, Plota M, Crifò A, Meo A, Frisina N (2007) The “lively” cytokines network in beta-Thalassemia Major-related osteoporosis. Bone 40:1588–1594
Lasco A, Morabito N, Gaudio A, Buemi M, Wasniewska M, Frisina N (2001) Effects of hormonal replacement therapy on bone metabolism in young adults with β-thalassemia major. Osteoporos Int 12:570–575
Morabito N, Lasco A, Gaudio A, Crisafulli A, Di Pietro C, Meo A, Frisina N (2002) Bisphosphonates in the treatment of thalassemia-induced osteoporosis. Osteoporos Int 13:644–649
Giusti A (2014) Bisphosphonates in the management of thalassemia-associated osteoporosis: a systematic review of randomised controlled trials. J Bone Miner Metab 32:606–615
Voskaridou E, Terpos E (2008) Pathogenesis and management of osteoporosis in thalassemia. Pediatr Endocrinol Rev 6:86–93
Rossini M, Gatti D, Adami S (2013) Involvement of WNT/b-catenin signaling in the treatment of osteoporosis. Calcif Tissue Int 93:121–132
Catalano A, Morabito N, Basile G, Brancatelli S, Cucinotta D, Lasco A (2013) Zoledronic acid acutely increases sclerostin serum levels in women with postmenopausal osteoporosis. J Clin Endocrinol Metab 98:1911–1915
Voskaridou E, Christoulas D, Xirakia C, Varvagiannis K, Boutsikas G, Bilalis A, Kastritis E, Papatheodorou A, Terpos E (2009) Serum Dickkopf-1 is increased and correlates with reduced bone mineral density in patients with thalassemia-induced osteoporosis. Reduction post-zoledronic acid administration. Haematologica 94:725–728
Voskaridou E, Christoulas D, Plata E, Bratengeier C, Anastasilakis AD, Komninaka V, Kaliontzi D, Gkotzamanidou M, Polyzos SA, Dimopoulou M, Terpos E (2012) High circulating sclerostin is present in patients with thalassemia-associated osteoporosis and correlates with bone mineral density. Horm Metab Res 44:909–913
Meunier PJ, Roux C, Seeman E, Ortolani S, Badurski J, Spector T, Cannata J, Balogh A, Lemmel EM, Pors-Nielsen S, Rizzoli R, Genant HK, Reginster JY (2004) The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med 350:459–46825
Reginster JY, Seeman E, De Vernejoul MC, Adami S, Compston J, Phenekos C, Devogelaer JP, Curiel MD, Sawicki A, Goemaere S, Sorensen OH, Felsenberg D, Meunier PJ (2005) Strontium ranelate reduces the risk of nonvertebral fractures in postmenopausal women with osteoporosis: treatment of peripheral osteoporosis (TROPOS) study. J Clin Endocrinol Metab 90:2816–2822
Kaufman JM, Audran M, Bianchi G, Braga V, Diaz-Curiel M, Francis RM, Goemaere S, Josse R, Palacios S, Ringe JD, Felsenberg D, Boonen S (2013) Efficacy and safety of strontium ranelate in the treatment of osteoporosis in men. J Clin Endocrinol Metab 98:592–601
Canalis E, Hott M, Deloffre P, Tsouderos Y, Marie PJ (1996) The divalent strontium salt S12911 enhances bone cell replication and bone formation in vitro. Bone 18:517–523
Marie PJ, Hott M, Modrowski D, De Pollak C, Guillemain J, Deloffre P, Tsouderos Y (1993) An uncoupling agent containing strontium prevents bone loss by depressing bone resorption and maintaining bone formation in estrogen-deficient rats. J Bone Miner Res 8:607–615
Marie PJ, Ammann P, Boivin G, Rey C (2001) Mechanisms of action and therapeutic potential of strontium in bone. Calcif Tissue Int 69:121–129
Bonnelye E, Chabadel A, Saltel F, Jurdic P (2008) Dual effect of strontium ranelate: stimulation of osteoblast differentiation and inhibition of osteoclast formation and resorption in vitro. Bone 42:129–138
Marie PJ, Felsenberg D, Brandi ML (2011) How strontium ranelate, via opposite effects on bone resorption and formation, prevents osteoporosis. Osteoporos Int 22:1659–1667
Stepan JJ (2013) Strontium ranelate: in search for the mechanism of action. J Bone Miner Metab 31:606–612
Ammann P, Badoud I, Barraud S, Dayer R, Rizzoli R (2007) Strontium ranelate treatment improves trabecular and cortical intrinsic bone tissue quality, a determinant of bone strength. J Bone Miner Res 22:1419–1425
Reginster JY, Kaufman JM, Goemaere S, Devogelaer JP, Benhamou CL, Felsenberg D, Diaz-Curiel M, Brandi ML, Badurski J, Wark J, Balogh A, Bruyère O, Roux C (2012) Maintenance of antifracture efficacy over 10 years with strontium ranelate in postmenopausal osteoporosis. Osteoporos Int 23:1115–1122
Rybchyn MS, Slater M, Conigrave AD, Mason RS (2011) An Akt-dependent increase in canonical Wnt signaling and a decrease in sclerostin protein levels are involved in strontium ranelate-induced osteogenic effects in human osteoblasts. J Biol Chem 286:23771–23779
Gulhan I, Bilgili S, Gunaydin R, Gulhan S, Posaci C (2008) The effect of strontium ranelate on serum insulin like growth factor-1 and leptin levels in osteoporotic post-menopausal women: a prospective study. Arch Gynecol Obstet 278:437–441
Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser (1994) 843:1–129
Catalano A, Morabito N, Basile G, Fusco S, Castagna G, Reitano F, Albanese RC, Lasco A (2013) Fracture risk assessment in postmenopausal women referred to an Italian center for osteoporosis: a single day experience in Messina. Clin Cases Miner Bone Metab 10:191–194
Reginster JY, Deroisy R, Dougados M, Jupsin I, Colette J, Roux C (2002) Prevention of early postmenopausal bone loss by strontium ranelate: the randomised, 2 year, double masked, dose-ranging, placebo-controlled PREVOS study. Osteoporos Int 13:925–931
Meunier PJ, Slosman DO, Delmas PD, Sebert JL, Brandi ML, Albanese C, Lorenc R, Pors-Neilsen S, de Vernejoul MC, Roces A, Reginster JY (2002) Strontium ranelate: dose-dependent effects in established postmenopausal vertebral osteoporosis–a 2 year randomised placebo controlled trial. J Clin Endocrinol Metab 87:2060–2066
Bruyere O, Roux C, Detilleux J, Slosman DO, Spector TD, Fardellone P, Brixen K, Devogelaer JP, Diaz-Curiel M, Albanese C, Kaufman JM, Pors-Nielsen S, Reginster JY (2007) Relation between bone mineral density changes and fracture risk reduction in patients treated with strontium ranelate. J Clin Endocrinol Metab 92:3076–3081
Doyard M, Fatih N, Monnier A, Island ML, Aubry M, Leroyer P, Bouvet R, Chalès G, Mosser J, Loréal O, Guggenbuhl P (2012) Iron excess limits HHIPL-2 gene expression and decreases osteoblastic activity in human MG-63 cells. Osteoporos Int 23:2435–2445
Middleton ET, Steel SA, Aye M, Doherty SM (2012) The effect of prior bisphosphonate therapy on the subsequent therapeutic effects of strontium ranelate over 2 years. Osteoporos Int 23:295–303
Catalano A, Morabito N, Di Stefano A, Morini M, Basile G, Faraci B, Loddo S, Ientile R, Lasco A (2015) Vitamin D and bone mineral density changes in postmenopausal women treated with strontium ranelate. JENI. doi:10.1007/s40618-015-0299-2
European medicines agency. Press release: European medicines agency recommends that protelos/osseor remain available but with further restrictions (2014) http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2014/02/news_detail_002031. jsp&mid = WC0b01ac58001d126
Marquis P, Roux C, de la Loge C, Diaz-Curiel M, Cormier C, Isaia G, Badurski J, Wark J, Meunier PJ (2008) Strontium ranelate prevents quality of life impairment in post-menopausal women with established vertebral osteoporosis. Osteoporos Int 19:503–510
Acknowledgments
We would like to thank Dr. Corrado Andrè for DXA assessment of subjects involved in this research study.
Conflict of Interest
Nunziata Morabito, Antonino Catalano, Agostino Gaudio, Elisabetta Morini, Lucia Maria Bruno, Giorgio Basile, Eleni Tsiantouli, Federica Bellone, Rita Maria Agostino, Basilia Piraino, Maria Angela La Rosa, Carmelo Salpietro and Antonino Lasco declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Morabito, N., Catalano, A., Gaudio, A. et al. Effects of strontium ranelate on bone mass and bone turnover in women with thalassemia major-related osteoporosis. J Bone Miner Metab 34, 540–546 (2016). https://doi.org/10.1007/s00774-015-0689-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-015-0689-8