Abstract
Summary
Thalassemia-associated osteoporosis constitutes a major complication in patients with thalassemia. This review presents the existing studies on the treatment of thalassemia-associated osteoporosis and discusses the management of this debilitating complication. A brief presentation of the disease characteristics and pathogenetic mechanisms is also provided.
The life expectancy of patients with thalassemia has increased markedly in recent years resulting in the aging of the population and the emergence of new comorbidities. The majority of patients with thalassemia have low bone mineral density and experience lifelong fracture rates as high as 71 %. The pathogenesis of thalassemia-associated osteoporosis (TAO) is multifactorial with anemia and iron overload playing crucial role in its development. Data concerning the prevention and treatment of TAO are extremely limited. We performed a literature research in Pubmed and Scopus to identify interventional studies evaluating the effects of various agents on TAO. Seventeen studies were retrieved. We present the results of these studies as well as a brief overview of TAO including presentation, pathogenesis, and management. Most of the studies identified are of poor quality, are not randomized controlled, and include small number of participants. There are no data concerning effects on fracture rates. Bisphosphonates are the most widely studied agents and among them zoledronic acid is the most well studied. Hormone replacement treatment (HRT) shows beneficial but small effects. Denosumab and strontium ranelate have each been evaluated in only a single study, while there are no data about the effects of anabolic agents. Given the increased life expectancy and the increase in fracture rates with age, more data about the management of TAO are warranted. Moreover, due to the need for lifelong management starting at young age, careful treatment plans which may include sequential treatment may often be required. However, currently, there are no relevant data available.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The thalassemias constitute a group of hereditary disorders in the synthesis of hemoglobin (Hb), resulting in various degrees of anemia. The spectrum of the disease ranges from mild anemia to intrauterine death. Milder forms, grouped under “thalassemia intermedia,” only occasionally require transfusion therapy, whereas, in more severe cases, grouped under “thalassemia major,” regular transfusion therapy is usually required to maintain acceptable Hb levels, as well as chelation therapy to prevent iron overload [1]. Iron overload is a cardinal manifestation of the disease and is associated with most of the complications in these patients [2]. According to WHO, worldwide and yearly, there are about 56,000 conceptions affected by thalassemia and at least 30,000 of them need regular transfusions to survive while 5500 die perinatally. Most children with thalassemia are born in low-income countries; however, worldwide transfusion is available only for a small fraction of those who need it (12 %). Alpha-thalassemia major is lethal perinatally, and beta-thalassemia major is lethal by the age of 3 in children unable to receive transfusion. In countries where screening and prevention programs are established, the number of births decreases, whereas the advances in treatment have led to increasing life expectancy resulting in a worldwide population of 100,000 patients with beta-thalassemia under transfusion [3].
Despite regular transfusion and chelation therapy, patients with thalassemia exhibit increased mortality rate as compared with the general population [4]. However, in the recent years, where access to proper treatment is available, their life expectancy seems to be increased [5], thus, age-related conditions become more prevalent and chronic co-morbidities require lifelong management plans. Thalassemia-associated osteoporosis (TAO) constitutes a very frequent co-morbidity, even in appropriately treated patients [6], with a lifetime fracture rate up to 71 % [7]. Most patients require lifelong management, which can be particularly challenging given the complex pathophysiology of their bone disease and the lack of large well-designed interventional studies.
We aimed to systematically review the available data regarding the use of various therapeutic options for the management of thalassemia-associated osteoporosis and to provide a brief overview of the complex pathophysiology of the disease and its principal characteristics.
Methods
We performed a literature search in Pubmed and Scopus on May 2016 using the words thalassemia AND osteoporosis AND bisphosphonates/denosumab/strontium ranelate/teriparatide/hormone replacement therapy/growth hormone/calcium and vitamin D. Search was limited to English literature and dated from 1990 onward. One hundred forty-nine articles were retrieved. From these, we sought to identify all the interventional studies and 17 studies were identified. Cross-sectional studies describing findings between treated and non-treated patients were excluded. The relevant flow chart is depicted in Fig. 1.
Fractures, bone mineral density, bone accrual, and bone turnover in thalassemia
Thalassemia had been associated with increased risk of fracture, especially before the advances in transfusion and chelation treatment, with fracture rates varying from 30 to 50 % in earlier cohorts [8–10]. In recent studies, fracture rates range from 12.1 to 38.8 % depending on study population and method of data collection [11–13]. In even more recent and more aged cohorts, however, the prevalence of history of fracture escalates to 55 % for adults with thalassemia major and to 71 % for adults with thalassemia intermedia, while fracture rates in children are no longer increased compared to the general population [7]. The new increase in fracture rates observed in more recent studies in the western world seems to be associated with the aging population in these cohorts which is the result of a combination of fewer new cases and increased life expectancy of the existing cases. However, in eastern countries, higher fracture rates are still observed in pediatric populations [14] mainly due to the inadequacy in blood transfusions and chelation schemes. This results in a discrepancy between the developing countries, where fractures are of concern even from childhood and where there is room for improvement by optimizing transfusion and chelation, and the western world, where fractures are becoming of increasing concern in aging thalassemia groups, irrespective of the advances in the disease management.
Extremity fractures are the most common [7], and the upper extremity seems to be the most common fracture site [11]. Vertebral fractures seem to be less common although their prevalence is usually underestimated in self-reported studies [15]. Unrecognized vertebral deformities are prevalent in 2.6–13 % [7, 15].
The severity of the thalassemia syndrome, which is reflected in the degree of anemia, and the resultant need for more regular transfusion schemes, as well as the increasing age, seem to be important factors affecting fracture risk [7, 11, 12, 15]. Moreover, as in the general population, there is good correlation between bone mineral density (BMD) and fractures, and thalassemia patients with fractures tend to have lower BMD T-scores and Z-scores [7, 12] and are more likely to be hypogonadal and on hormone replacement treatment (HRT) [7, 11, 12].
Some degree of BMD deficit (namely osteopenia or osteoporosis, defined by densitometric criteria) in at least one skeletal site is estimated to be found in up to 92.7 % of optimally transfused (with pre-transfusion Hb levels at 9–9.5 g/dl) and well chelated adult patients [6]. The spine is more severely affected than other skeletal sites and BMD Z-scores are usually lower at the lumbar spine (LS) than at the hip [7].
Bone accrual during adolescence is disrupted in patients with thalassemia. It is noteworthy that although low BMD (with Z-score value <−2) is prevalent in less than 10 % of patients aged 6–10 years, the percentage increases to 44 % for adolescents 11–19 years old and exceeds 60 % for adults >20 years old [7]. The inability to proceed normally through puberty, with delay in sexual maturation, is an important factor affecting BMD during adolescence in patients with thalassemia [16]. This has deleterious effects on peak bone mass and among patients aged 20–29 years old, 86 % of them display spine BMD Z-scores <−1, indicating suboptimal peak bone mass [7].
Apart from the suboptimal bone mass, there is also a continuous and gradual decline in bone mass at the femoral neck (FN) and total body, which is more prevalent among males than females [17]. On the contrary, BMD at the LS stays rather stable or may even increase, indicating that the hip is the best skeletal site to assess changes during follow-up.
Patients with beta-thalassemia display increased bone resorption, especially when hypogonadal [18]; however, increased bone turnover markers have also been described in patients with normal gonadal function [7, 19]. There is evidence that alterations in the receptor activator of nuclear factor kappa-B ligand (RANKL)/osteoprotegerin (OPG) system may have a role in the pathogenesis of increased bone resorption [20]. However, increased bone resorption has not been identified in most histomorphometric studies [21, 22], although there are limited data.
As far as bone formation is concerned, studies evaluating bone formation markers have conferred conflicting results [7, 18, 20]. However, histomorphometry studies suggest a possible impairment of bone formation. Iron overload has been associated with iron deposition on mineralization fronts, osteoid surfaces, and bone marrow spaces [21–23] and exhibits a negative correlation with trabecular bone volume and BMD [22]. A direct effect of iron on osteoblasts with intracellular iron deposits and mitochondrial damage has been observed [23], as well as a decrease in osteoblast recruitment [21]. However, bone formation rate has been described as either normal [22] or decreased [21], depending on study population (transfusion dependent vs non-dependent and adults vs children and adolescents). It has been suggested that there might be differences in bone turnover between thalassemia major and intermedia [24]. A non-randomized case control study including nine patients with paired bone biopsies reported that patients with thalassemia major have high bone turnover and respond favorably to BSPs in terms of BMD, while patients with thalassemia intermedia had evidence of low bone turnover and poor response to pamidronate. However, their findings must be interpreted with caution given that the number of biopsies was small (three patients with thalassemia intermedia), while following pamidronate there was increase in indices of both resorption and formation, a finding difficult to interpret [24].
Findings consistent with osteomalacia have also been described, although not invariably [21, 23, 25]. The inconsistency of findings is likely attributed to differences in the severity of anemia, adequacy of transfusion therapy, and level of iron overload.
It is possible that alterations in the Wnt/b catenin signaling might be implicated in the development of TAO. Sclerostin levels in patients with beta-thalassemia are increased and correlate positively with LS Z-score, while Dickkopf-1 levels are also increased and correlate negatively with LS BMD [26, 27]. These findings are in keeping with previous studies showing positive correlations between serum sclerostin levels and BMD in postmenopausal women [28] and negative associations between serum Dickkopf-1 levels and BMD [29]. Notably, in patients with sclerostin deficiency, the levels of Dickkopf-1 are increased and this is probably an adaptive mechanism to sclerostin deficiency even though it cannot compensate for the increased bone formation observed in these patients [30]. It would be extremely difficult to say which of the above findings in thalassemia are primary disorders affecting bone health and which ones constitute adaptive responses, and these data highlight the complexity of the Wnt/b catenin system and the limitations in linking its inhibitors’ circulating levels with their effects at the bone microenvironment.
Pathogenetic mechanisms
The pathogenesis of thalassemia-associated osteoporosis is multifactorial (Fig. 2). Anemia itself, along with iron overload and its associated complications, can all have detrimental effects on bone health. The ineffective erythropoiesis can cause a fivefold to sixfold increase in the number of erythroid precursors resulting in bone marrow expansion [31]. Regular transfusion therapy is able to suppress bone marrow expansion; the degree of suppression depends on transfusion regimen and target pre-transfusion Hb levels; however, even with hypertransfusion (which is generally avoided due to its effect in iron overload), erythroid activity is not completely normal [32]. Other factors associated with anemia and ineffective erythropoiesis including hypoxia, increased erythropoietin levels, and reduced hepcidin levels may exert negative affects in bone homeostasis primarily by disrupting bone formation [33–35] but also by increasing bone resorption [33, 36].
Iron overload is caused both by the transfusion iron burden and by a disruption in the hepcidin-ferropontin axis, leading to increased iron absorption by the gastrointestinal tract. It is one of the most important factors in the development of TAO and exerts both direct and indirect effects on bone metabolism. Iron directly disrupts bone formation [35, 37], has toxic effects on osteoblasts [23], and induces a decrease in the recruitment of cells of the osteoblastic lineage [21]. On the other hand, iron deposition results in several complications such as liver disease, cardiac dysfunction, and several endocrine disorders which are also implicated in the development of TAO. However, attempts to associate the iron burden with TAO have been rather unsuccessful. Ferritin is one of the most useful and handy tools to assess iron overload, albeit with several limitations, and researchers have failed to demonstrate a constant correlation between serum ferritin levels and LS or hip BMD [7, 17] or between ferritin levels and fractures [11].
The endocrine system is particularly vulnerable to the effects of iron deposition. Hypogonadism, hypothyroidism, hypoparathyroidism, overt diabetes mellitus (DM) or impaired glucose tolerance (IGT), and disruption of the growth hormone (GH)—insulin-like growth factor 1 (IGF-1) axis are all endocrine disorders that are prevalent even in appropriately treated patients with thalassemia [6]. Hypogonadism is the most common endocrine deficiency [6, 38], and hypogonadal thalassemia patients have lower BMD compared to those with normal gonadal function, even if they are on replacement therapy [6]. Hypogonadism is particularly important when present during the second decade of life leading to lack of spontaneous puberty and thus impairing bone accrual [16, 39].
Iron overload can also result in hypothyroidism primarily by direct effects on the thyroid gland [39]. Thyroid hormones are known to play an important role in the development and maintenance of the skeleton, and hypothyroidism is associated with significant growth retardation [40]. Data, however, about the association of hypothyroidism and fractures in thalassemia are contradictory [11, 12], probably because of differences in the adequacy and timing of thyroid hormone replacement on different populations.
Hypoparathyroidism affects approximately 13.5 % of adult patients with thalassemia; however, it does not appear to be associated with TAO [41]. On the contrary, the presence of hypoparathyroidism has been correlated with higher hip BMD in thalassemia patients [6]. However, hypoparathyroidism may play a part in the development of hypercalciuria and nephrolithiasis.
DM is associated with increased fracture risk and this can be observed even in the context of normal or increased BMD [42]. In patients with thalassemia, however, DM does not seem to be an independent risk factor for low BMD [6, 7] or for fractures [12].
Diminished peak GH secretion after growth hormone-releasing hormone (GHRH) infusion as well as low IGH-1 levels are quite common in patients with thalassemia and have been associated with diminished hip BMD values [43]. Low IGF-1 levels in thalassemia are not only due to the reduced GH secretion but might also be related to chronic liver disease, which is induced either by iron overload, viral hepatitis, or by a combination of both.
Chronic hepatitis C is highly prevalent among adult patients with thalassemia and contributes along with the increased hepatic iron concentration to the development of liver disease and cirrhosis [38]. This could also contribute to TAO by affecting IGF-1 levels or, in severe cases, by disrupting vitamin D metabolism.
Renal dysfunction expressed as renal hyperfiltration, hypercalciuria, albuminuria phosphaturia, and hyperuricosuria is common in patients with thalassemia [44] and is believed to be associated with iron overload. There are data suggesting that ferritin correlates well with renal dysfunction and that kidney damage can be at least partly reversible with improvement of iron chelation [45]. Anemia itself, or through hypoxia and oxidative stress, can also be associated with the kidney damage in thalassemia, while there are data that iron chelators can also play a role [45]. It is suggested that one third of patients exhibit some degree of hypercalciuria and that there is an association between regular transfusion and the degree and frequency of hypercalciuria [46]. Recently, Baldan et al. demonstrated that hypercalciuria in patients with thalassemia is associated with decreased levels in soluble Klotho [47]. Interestingly, lower levels of Klotho were also associated with higher prevalence of fragility fractures. Moreover, in thalassemia patients, there is an association between hypercalciuria and lower BMD, which is more pronounced for LS BMD [48]. Nephrolithiasis is prevalent in up to 18 % of patients with thalassemia and interestingly, its presence is associated with lower FN BMD and, in males, with higher fracture rates, even after adjusting for confounders [49].
Even though iron chelation constitutes an invaluable tool in the management of thalassemia, there are several data concerning the deleterious effects of desferrioxamine on the skeleton. In a retrospective study, up to 39 % of young children with thalassemia exhibited signs of desferrioxamine-induced bone dysplasia consisting of metaphyseal sclerosis in long bones, irregular sclerosis at the costochondral junctions, and platyspondyly [50]. Bone dysplasia is associated with increased doses of desferrioxamine and reduced ferritin levels [51] and can contribute to growth retardation and lower standing height [50, 51]. Current guidance about the use of desferrioxamine suggests a careful approach not to exceed recommended doses until linear growth has ceased and calls for particular attention when treatment is initiated at younger ages (< 3 years) [52].
As far as the newer chelation regiments are concerned, one longitudinal study found that in that particular cohort, bone loss was more severe during the period when most patients were switched from desferrioxamine to deferasirox [17]. A possible explanation could be its association with renal tubular dysfunction [53]. Interestingly, it has been demonstrated that patients on deferasirox are more prone to developing hypercalciuria in a dose-dependent manner [54]. The effect of this finding on skeletal health certainly needs to be investigated. However, in another longitudinal study, patients treated with deferasirox maintained stable hip BMD values during follow-up [55]. More data about the effects of newer chelation medications are definitely warranted, and careful monitoring of renal function in patients receiving deferasirox is recommended [52].
Patients with thalassemia display lower 25 hydroxy-vitamin D (25OHD) levels compared to healthy controls and up to 42.8 % of patients with thalassemia major display levels <20 ng/ml [56]. Severe deficiency (25OHD <10.4–11 ng/ml) is described in 10 to 12 % of patients [7, 56]. 25OHD levels are inversely correlated with ferritin levels and age [56], and Asian ethnicity is another risk factor for low vitamin D levels [57]. Patients with deficiency have significantly lower BMD [7]. The reasons for lower 25OHD are still unclear; however, it is postulated that defective skin synthesis associated with jaundice might be implicated. Moreover, reduced physical activity due to the anemia and consequently lower sun exposure might contribute, while, in patients with severe liver disease, reduced 25-hydroxylase activity may also play a part.
Micronutrient deficiency is considered common in patients with thalassemia and is related either to reduced intake or to increased requirements. Some of them, such as zinc, are thought to play an important role in the development of TAO [58].
Reduced physical activity as a consequence of chronic anemia is thought to contribute to the development of TAO. However, there are no data about the levels of physical activity in adequately managed patients with thalassemia. Physical activity is generally known to be associated with body composition, and in patients with thalassemia, very high levels of physical activity are correlated with higher lean mass and BMD [59]. Notably, there was no association between physical activity and BMD for patients with low or moderate physical activity.
Pain in patients with thalassemia
Pain is a common complaint of thalassemia patients [7, 60], although not necessarily an effect of reduced BMD and fractures. Thirty-seven percent of patients report having pain during the past 7 days, while 64 % report having pain over the past 4 weeks [61]. Pain seems to interfere with all measures of life activities [61, 62] and to influence the quality of life [62]. The most common site is the lower back although many patients report pain in various sites, such as legs, upper back, or head [60, 61]. When comparing patients who report pain to those who do not, patient groups do not differ in terms of Hb levels, iron overload, chelation regiment, history of fractures, bisphosphonates (BSPs) use, or BMD [7, 61]. However, in controlled trials with the use of BSPs for thalassemia-associated osteoporosis, these agents have been shown to be effective in reducing pain in patients with thalassemia [63–65]. An association of pain severity with low 25OHD levels has been reported [60], however, not consistently [7]. Increasing age is the most significant factor associated consistently both with pain prevalence and severity [7, 60, 61, 66]. Among patients who report having pain, those who require more frequent transfusion therapy report pain more often, however, rather unexpectedly, so do patients with higher pre-transfusion Hb levels. Even though pain is thought to be associated with bone marrow expansion, it is not yet entirely clear if the transfusion reduces pre-transfusion pain [66].
Challenges in assessing bone health in thalassemia
The best modality to assess bone health and to estimate fracture risk in patients with thalassemia has not been established yet. In general, dual energy X-ray absorptiometry (DXA) is considered the gold standard in assessing bone health, and there is good correlation between DXA derived T-scores and fracture risk in postmenopausal osteoporosis. Likewise, in patients with thalassemia, there is good correlation between DXA-derived Z-scores and fracture risk and for this reason, DXA is considered the method of choice to assess bone status in thalassemia. For every 1-SD decrease in spine or femur BMD Z-score, the mean fracture rate increases by 37 or 47 %, respectively [7].
Common calculation tools for fracture risk have not been validated in patients with thalassemia; however, taking into consideration clinical risk factors such as age (which is a well established risk factor for fractures in thalassemia as well), body mass index (BMI), smoking, and alcohol consumption when evaluating a patient seems logical even though this is not supported by published prospective data, and research on this field is definitely warranted.
Several attempts have been made to evaluate BMD using other methodologies, however, those are sporadic and some of them can also result in misleading findings. Specifically, QCT derived Z-scores are significantly higher than DXA derived Z-scores [67, 68] and very few patients are found to have osteoporosis when using QCT [68]. It is suggested that in patients with inadequate chelation, the accumulation of iron might account for falsely increased BMD values obtained by QCT; indeed, patients with high ferritin values exhibit very high BMD, even higher than normal controls, despite having several risk factors for osteoporosis [69]. Patients with thalassemia have been reported to have lower trabecular bone score (TBS) compared to a group of controls, even though patients with thalassemia were significantly younger [48]. TBS in these patients correlated negatively with age and positively with BMD but was similar in patients with and without a history of fragility fractures, limiting its utility in fracture prediction in this population. Data derived by the use of quantitative ultrasound sonography (QUS) to evaluate the skeletal status in thalassemia have been inconsistent. There is poor correlation between measurements derived by QUS and those derived by DXA, as well as that of the number of patients identified as having osteoporosis with the two methods largely differ [70, 71]. However, in patients with a history of fragility fracture, QUS has been shown to be equally effective to DXA in assessing bone demineralization [70]. QUS ability to predict fractures in thalassemia needs to be evaluated. Evaluation of bone density in young patients with thalassemia using peripheral quantitative computed tomography (pQCT) resulted in low volumetric BMD (vBMD) Z-scores, which is in line with DXA-derived measurements. Moreover, using pQCT, the researchers were able to highlight that the low BMD obtained by two-dimensional DXA measurements is not only accounted for by low bone size [72]. However, the utility of pQCT in the prediction of fracture risk or in the monitoring of treatment in thalassemia needs further research.
Bone turnover markers in thalassemia display a good negative correlation with BMD; however, it has not been demonstrated that they can independently predict fracture risk irrespective of BMD [7]. Even though bone turnover markers might be useful in monitoring response to treatment, more data are needed before they can become implemented in decision making for pharmacological intervention.
The management of thalassemia-associated osteoporosis
Regular transfusion therapy and keeping adequate Hb levels are the mainstays of treatment in transfusion dependent thalassemias. However, even though some studies have suggested an association between higher Hb levels and BMD at the LS and total body [6, 17], other studies have failed to demonstrate an association between mean pre-transfusion Hb levels and BMD [39]. Current guidance suggests maintaining a pre-transfusion Hb level above 9–10.5 g/dl in most patients with thalassemia [52]. This is associated with 1–4 times normal levels of erythroid activity [32]. It is suggested that in certain cases, higher pre-transfusion Hb levels may be attempted if deemed appropriate [52]; however, this should always be balanced against the increase in iron accumulation and subsequent need for higher chelation treatment doses.
As 25OHD levels are frequently low in patients with thalassemia, screening and supplementation are recommended [73]; however, there are not enough data to indicate the optimal target levels for 25OHD. Vogiatzi et al. have demonstrated that the inverse relationship between 25OHD and BMD reaches a plateau at levels >15 ng/ml [7]. Parathyroid hormone (PTH) levels have no value in determining target 25OHD levels as, at least in patients with thalassemia major, patients with levels <20 ng/ml have similar PTH levels to those with levels 20–30 ng/ml and to patients with levels >30 ng/ml [56]. This probably reflects the state of overt or subclinical hypoparathyroidism which is often encountered in these patients.
There are no available data about the effects of calcium and vitamin D on thalassemia-associated osteoporosis; however, their use is very common among patients with thalassemia. Recently there has been an exhaustive debate about the effects of calcium and vitamin D supplements on fracture risk and some concerns have been raised, associating calcium supplementation with increased cardiovascular risk [74]. A small positive effect of supplements on hip and spine BMD has been demonstrated [75], and several meta-analyses have shown from no to small positive effects on fracture risk [75–78], depending on study population, with more pronounced positive effects in institutionalized patients [78]. Several studies have failed to demonstrate an association between the use of calcium supplements and cardiovascular risk [79, 80] and although the debate still remains, currently there is no strong evidence to advise against the use of supplements.
Apart from vitamin D, patients with thalassemia suffer several micronutrients deficiency, including zinc. In a single double-blind, placebo-controlled study, zinc supplementation was shown to increase whole body BMD and bone mineral content (BMC) compared to placebo, while patients allocated to zinc supplementation preserved their spine and hip Z-scores in contrast to the placebo group which experienced a decline in Z-scores [81]. Even though sample size was small and dropout rates were high, a high percentage of study participants had low plasma zinc concentrations and it is possible that zinc supplementation might be beneficial particularly to patients with deficiency. Further studies are warranted to establish which patients would benefit from such interventions, the optimal dose of supplementation, the side effects, and the appropriate monitoring (such as cooper levels).
Even though the current status of physical activity in patients with thalassemia is largely unknown, and there are no data about the effects of exercise interventions on BMD or fracture risk in such cohorts, encouraging adequate physical activity to promote bone health and to reduce the risk of falls seems logical and is generally recommended [73].
GH deficiency and reduced IGF-1 levels can be quite common in thalassemia and are probably implicated in the development of TAO. There are several studies demonstrating the positive effects of recombinant GH on growth velocity in children with thalassemia [82, 83], while there is only one non-controlled study on five pre-pubertal GH-deficient children, which also provided data on the effects of 12 months recombinant GH administration on BMD [84]. No significant changes were observed on that study. There are no studies evaluating its effect on BMD or fractures in adult GH thalassemia patients. However, recombinant GH administration in non-thalassemia adults with GH deficiency has led to the reduction of fractures [85], and thus it seems logical that selected adult patients with thalassemia and GH deficiency might benefit from replacement therapy. Further investigation on the field is indicated.
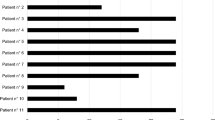
The number of studies addressing the treatment of TAO is limited, while there are no randomized controlled trials with data on fractures. The studies evaluating the effects of various agents in TAO are summarized in Table 1. Most of them are of poor quality and include small numbers of participants.
BSPs represent the most widely studied agents in TAO. They reduce the osteoclastic activity leading to reductions in bone turnover and their use seems logical in thalassemia, where bone turnover has been found to be increased. Zoledronic acid is the most widely studied, has been evaluated in various schemes, and has provided good results in terms of BMD improvement. It should be noted, however, that none of the evaluated schemes is similar to the dose of 5 mg annually which is recommended for postmenopausal women and adult men with osteoporosis or for glucocorticoid induced osteoporosis, and that the schemes used in these studies are far more frequent. In a 2-year randomized, double-blind, placebo-controlled study by Gilfillan et al., zoledronic acid (4 mg) every 3 months produced significant increases in LS (10.2 %), FN (5.2 %), total hip (6 %), and total body (4.6 %) BMD, compared to placebo, which were evident by the first year of the study, while BMD either exhibited small increments or remained stable during the second year [86]. Similarly, in a non-randomized, controlled study, Otrock et al. with the administration of the same therapeutic scheme for 1 year demonstrated a significant increase in LS, total hip, and FN BMD from baseline values [64]. On the other hand, Voskaridou et al. have demonstrated that zoledronic acid (4 mg) administered every 3 months for 1 year was effective in increasing both LS (15.2 %) and FN (11.3 %) BMD; however, this had no significant effect on BMD or markers of bone resorption, compared to placebo, when administered every 6 months [65]. Lower doses were also used by Perifanis et al. who demonstrated an increase in LS BMD from baseline with the administration of 1 mg of zoledronic acid every 3 months; however, the study was not controlled and no other skeletal sites were evaluated [87].
Bone turnover markers decreased following the administration of zoledronic acid compared to baseline values in most studies; however, findings were not consistent among the four studies. Notably, in two studies where pain was evaluated using specific questionnaires, the administration of zoledronic acid had significant beneficial effects on pain scores [64, 65].
Pamidronate administration was evaluated in a controlled study for 3 years [24]. Pamidronate was associated with significant increases in LS and total hip BMD Z-scores from baseline, while the control group experienced no significant changes. Pamidronate also resulted in significant increase in LS and FN BMD Z-score from baseline in another 3-year study, while observation alone or the combination of calcium and alphacalcidol failed to produce similar results [88]. However, there were significant differences at the FN BMD Z-score among groups at baseline. Similar findings were observed in another 2-year non-controlled study [89]. On the contrary, in a non-controlled trial, with two different doses of pamidronate for 12 months, the drug produced significant increases in LS but not FN and forearm BMD, irrespective of dose [90]. Perhaps the shorter duration of the latter study compared to all the others with pamidronate did not allow for any significant changes at the hip and the forearm. In another small non-controlled study, the administration of pamidronate in young children with thalassemia for 12 months resulted in significant increase in FN BMD at 12 months. The same cohort on follow-up at 24 months had significant increases both at LS and FN BMD [91]. However, the findings of this study should be interpreted with caution as it was non-controlled, and in growing children, an increase in BMD is expected over time due to the effect of normal bone accrual. In studies with pamidronate where bone turnover markers were evaluated, pamidronate administration resulted in a decrease in bone turnover as expected.
Forni et al. evaluated the effects of IV neridronate administration for 1 year in a randomized controlled study [63]. There was a significant increase in LS, FN, and total hip BMD in patients receiving neridronate compared to controls, and many of the changes were already prevalent by the sixth month of treatment, while bone turnover was suppressed as expected. Moreover, the administration of neridronate was associated with a significant reduction in pain scores, which resulted in a decrease in the use of analgesic drugs already prevalent by the third month of the study. This reduction in the use of analgesics is possibly related to the reduction in aminotransferases which was observed in patients receiving neridronate.
Data concerning the effects of clodronate are less encouraging. Penissi et al. demonstrated that even though clodronate failed to increase LS and FN BMD, it resulted in a relative preservation of BMD compared to a group of patients on simple observation which experienced a significant decline in BMD [92]. This effect was accompanied by a reduction in bone resorption markers without affecting bone formation. On the other hand, in a study by Morabito, clodronate had no significant effect on LS and FN BMD compared to baseline or placebo [93].
Oral BSPs have only been sporadically studied in thalassemia. The daily administration of alendronate for 2 years resulted in significant increases in LS (2.8 %) and FN (5.6 %) BMD compared to placebo [93]. Similarly, in another, non-controlled study, oral alendronate administration leads to significant increases at both LS and FN BMD compared to baseline values [94]. The positive effect was restricted only to patients achieving good compliance. However, in another non-controlled study, the administration of alendronate for 24 months did not produce significant changes in LS and FN BMD [89].
Hypogonadism is an important factor in the pathogenesis of TAO, and timely and regular administration of HRT is very important, as hypogonadal patients that adhere to HRT have higher BMD values compared to hypogonadal patients with poor compliance [95]. However, it is usually inadequate in preventing or treating TBD in hypogonadal thalassemia patients [6]. In a study by Anapliotou et al. in hypogonadal thalassemia patients, a continuous scheme of HRT resulted in significant increase in LS BMD at 16 and 32 months of follow-up, whereas, administration of an on/off scheme did not result in a significant increase in 16 months. Those patients exhibited larger increments in LS BMD from month 16 to 32 when they crossed over to the continuous scheme [96].
Denosumab is a monoclonal antibody against RANKL and a potent inhibitor of bone resorption. RANKL levels have been found to be increased in patients with thalassemia [20] and a potent inhibitor of bone resorption. Denosumab has been studied in a single non-controlled trial in adult regularly transfused thalassemic patients [97]. Administration of denosumab for 12 months resulted in significant increases in BMD both at the LS (9.2 %) and at the FN (6 %), accompanied with significant reductions in bone resorption.
Strontium ranelate is thought to have a dual action, both increasing bone formation and decreasing bone resorption, even though its anabolic properties have been questioned [98]. The effects of strontium ranelate in TAO have been studied in only one randomized controlled study which included exclusively postmenopausal women with thalassemia major. Daily administration of strontium ranelate for 2 years resulted in significant increases in LS BMD compared to baseline values, while at the FN, only a trend was observed which did not reach statistical significance [99]. It should be noted, however, that part of the increase might be attributed to the artifact effect of strontium ranelate [100]. Notably, in this study, strontium ranelate resulted in uncoupling of bone turnover, with increased formation and decreased resorption markers, while it also produced a decrease in pain scores.
Calcitonin is no longer approved for the treatment of osteoporosis. However, in a small study of children and young adolescents, calcitonin has been shown to decrease pain and improve some bone parameters. Distal femur cortical bone thickness, as measured by computerized axial tomography, increased significantly in the intervention group and pain was reported to decrease; however, this was not evaluated in a formal manner [101].
The use of an anabolic agent for the treatment of TAO seems attractive as patients with thalassemia often have significantly decreased BMD, and there are several data supporting impaired bone formation in these patients [21, 23]. However, there are no data about the effects of anabolic agents on TAO, except for sporadic case reports with the use of teriparatide [102, 103]. More data are definitely warranted.
Specific considerations-limitations
The route of administration of HRT could be important in the management of TAO. In healthy postmenopausal women, the long-term administration of oral and transdermal HRT resulted in similar increases in BMD [104]. In conditions where amenorrhea is accompanied by low levels of IGF-1, as in patients with anorexia nervosa where generally the administration of HRT is largely inefficient, administration of transdermal estradiol can have beneficial effects on BMD due to absence of suppression of IGF-1 which is observed when using the oral route [105]. There are no data concerning the differential effects of HRT in BMD or fractures in patients with thalassemia according to the route of administration. However, it should also be noted that transdermal HRT has minimal, if any, effects on deep vein thrombosis or pulmonary thromboembolism [106], which might be particularly important in thalassemia, and especially thalassemia intermedia and in patients with splenectomy, where a hypercoagulable state has been documented [107].
Similarly, in those patients with thalassemia where a hypercoagulable state is suspected, concerns raised about the effect of strontium ranelate on venous thromboembolism [108] should be taken into account during decision making for treatment. Moreover, as highlighted by the European Medicines Agency (EMA), strontium ranelate should be avoided in patients at risk of cardiovascular disease, i.e., in patients with a history of ischemic heart disease, peripheral artery disease, cerebrovascular disease, and in those with uncontrolled hypertension [108].
It should be noted that particular caution should be taken when treating patients with thalassemia with potent antiresorptive agents for the development of severe hypocalcemia related to the underlying subclinical hypoparathyroidism.
The use of high dose calcium supplements has been associated with an increased risk of nephrolithiasis [76] [109], whereas dietary calcium intake has been associated with less risk presumably due to its effect in decreasing the absorption of oxalates [109]. As previously mentioned, patients with thalassemia are at high risk for hypercalciuria and nephrolithiasis, so particular caution should be exercised to encourage calcium intake from dietary sources and reserve the use of supplements for patients unable to meet the recommended daily calcium intake from diet and for those for whom the supplements are an adjunct to bone specific treatment.
The optimal timing for initiating bone-specific therapy for TAO remains to be clarified. In general, for young adults with osteoporosis, the presence of low energy fractures represents an absolute indication for treatment [110]. A significant decline in BMD over time (above the least significant change) might also constitute an indication for treatment in certain cases; however, there is no clear guidance and this should be carefully considered on a case by case basis. In light of the need for lifelong management of TAO, a careful treatment plan including the timing of initiation of bone specific treatment, the selection of the therapeutic agent (taking into account any co-morbidities), the duration of administration, and the treatment target should be considered.
There are no data about the effects of prolonged treatment with BSPs in TAO, and only two studies provided results for 36 months of treatment. However, there are certain limitations to the duration of use of BSPs as they have been associated with adverse events such as osteonecrosis of the jaw and atypical fractures [111]. Moreover, it should be noted that even though most studies concerning the use of zoledronic acid in TAO have been carried out with frequent 4 mg doses, this scheme is not an established scheme for osteoporosis and therefore, currently, the recommended treatment in TAO, in keeping with postmenopausal osteoporosis, would be the use of 5 mg yearly. There is an increasing number of reports of patients with thalassemia on BSPs who presented with atypical femoral fractures [112–114]. Notably, one report involves a patient who had been on alendronate only for 6 months [114], and another patient had been treated with zoledronic acid for 3 years but was off treatment for 1 year prior to the fracture [112]. Certainly, a causal relationship between the use of BSPs and the atypical fractures could not be established; however, these cases raise questions as to the optimal duration of treatment in TAO.
Likewise, there are only limited data about BMD changes after discontinuing treatment. In a follow-up study by Voskaridou et al., patients who had received zoledronic acid every 3 months for 12 months continued to increase their LS BMD over the 2-year drug-free follow-up [115]. Interestingly, while hip BMD had not reached statistical significance at 12 months of treatment, BMD continued to increase posttreatment and reached statistical significance compared to baseline values at 2 years of drug-free follow-up. The same was observed in the treatment group who received zoledronic acid every 6 months and had not increased BMD significantly at the 12 months of the study; the group displayed significant increases at all skeletal sites at 36 months compared to baseline. The authors concluded that the results of the administration of zoledronic acid may be delayed in patients receiving more infrequent therapeutic schemes. Zoledronic acid is characterized by strong binding to the skeleton, and it can circulate even long after its discontinuation and this might explain its prolonged effects 2 years after the completion of the study. However, this observation might as well be a chance finding and must be formally tested given the absence of control (placebo) group and the small sample size. Of note, in the follow-up of the Horizon study, there were no differences in clinical fractures between patients who continued treatment with zoledronic acid for 6 years and those who discontinued treatment at 3 years and were then followed-up, supporting a prolonged affect of the medication [116]. However, patients who continued treatment for 6 years displayed a further decrease in morphometric vertebral fractures, suggesting that selected patients might benefit from more prolonged treatment.
Due to the concerns and subsequent limitations with the prolonged use of BSPs [111], as well as the limitation in the duration of treatment for anabolic agents, a need for sequential treatment for patients with osteoporosis has arisen, especially when lifelong treatment is indicated. There are a few data in the literature about the effects of sequential treatment in postmenopausal osteoporosis. It has been demonstrated that patients who switch from antiresorptive therapy with BSPs to teriparatide may experience a delayed response in bone turnover markers and a reduction in hip BMD by the sixth month of treatment, which is however transient [117]. Nevertheless, a full 2-year course of teriparatide is likely required to obtain maximum positive effects at the hip in such patients. On the other hand, a decline in BMD follows the withdrawal of teriparatide which is prevented when patients switch to an antiresorptive agent after the completion of the teriparatide course [118]. In the DATA Switch study, the administration of denosumab after a course of teriparatide resulted in further increases in BMD at all measured sites, whereas the administration of teriparatide after denosumab resulted in transient bone loss [119]. There are no data on the effects of sequential treatments in thalassemia; teriparatide has not been yet formally evaluated, and it is uncertain that the above data can be extrapolated to TAO due to its unique pathogenesis and thus, designing a long-term treatment plan can be really challenging.
Pediatric patients represent a particular challenge. Even though TAO can be prevalent even at younger ages, fracture risk increases with age, and, in contemporary western world cohorts, children and adolescents do not seem to be at particularly increased risk for fractures [7, 12], and it is postulated that this might also be related to the reduced physical activity and reduced participation in sports in thalassemia patients. Adequate transfusion and chelation treatment are probably behind the reduction in fracture rates in children in these western world cohorts, and thus, optimizing thalassemia treatment should be the mainstay for the prevention of TAO in this population, especially in the absence of low energy fractures. Subclinical vertebral fractures, which are under-recognized in self-report studies, could be of concern at this age. However, as vertebral growth disturbances, defined as a uniform decrease in the height of several vertebrae, can be quite prevalent, particularly in beta-thalassemia major patients [7], particular caution should be taken no to misdiagnose bone dysplasia as multiple vertebral fractures. As these disturbances are associated with younger age at initiation of chelation treatment [7] and desferrioxamine-induced bone dysplasia is associated with higher doses and reduced ferritin levels [51], timely recognition and intervention with adjustment of chelation during growth are recommended. The management of TAO in pediatric thalassemia patients in the presence of multiple low energy fractures can be particularly challenging. In general, in pediatric patients, osteoporosis is defined by the presence of both a clinically significant fracture history and low BMD and not by densitometric criteria alone. In specific, clinically significant fracture history corresponds to either two or more long bone fractures by age 10 years, or three or more long bone fractures at any age up to 19 years or a vertebral compression fracture in the absence of high-energy trauma, and low BMD corresponds to a Z-score ≤ −2 [120]. There is no consensus as to when to initiate bone-specific treatment in children, and the only agents that have been studied to some extent are BSPs. BSPs have been predominantly studied in children with osteogenesis imperfecta and with glucocorticoid-induced osteoporosis, and it has been demonstrated that apart from increasing BMD, they can also increase the size of vertebral bodies and produce a reshaping of already existing vertebral compression fractures [121]. Recombinant GH might be considered in GH-deficient children to improve both height and bone accrual; however, more data are definitely warranted. There are only limited and not convincing data about the effects of bone-specific treatment in pediatric thalassemia patients, even though some adolescents seem to have been included along with adults in the studies summarized in Table 1 and one study included only pediatric patients.
On the other hand, elderly patients might represent another particular challenge. Many of these patients were born before the advances in transfusion and chelation schemes and are thus more likely to have attained poor peak bone mass. Moreover, through the years, they have probably experienced progressive bone loss as it has been demonstrated [17]. This combination is probably behind the significant increase of fracture risk with age. Complications are also more prevalent in older cohorts [2] and should be taken into account when selecting bone-specific treatment. Finally, another issue that slowly emerges is that many of these older patients have been exposed to bisphosphonates for many years and have still low BMD, which would make a “drug holiday” inappropriate and raise questions as to the safety of more prolonged treatment or necessity for sequential treatment schemes. Studies addressing TAO in this elderly population are strongly warranted.
Orthopedic management of fragility fractures in older thalassemia patients carries several difficulties [122]. In this particular population, the surgical treatment is difficult due to the poor quality of the broken bone that limits the reduction, the hardware fixation, and the physiologic process of bone healing. Other important problems are the postoperative management of older patients with concomitant chronic diseases that are more prone to develop local and general complications with several difficulties to conduct a good rehabilitation program. However, the results of orthopedic treatment has improved in the last years thanks to a better knowledge of pathogenesis of secondary osteoporosis due to thalassemia and fracture repair pattern, hardware quality improvement, a more accurate surgical technique, and rehabilitation protocols focused on this special group of patients. The rate of complication though is still higher than in younger population, but dropping continuously.
Most fractures in patients with thalassemia seem to heal normally within the expected time frame. In a study including 61 thalassemia patients with fractures, Finsterbush et al. demonstrated that fracture healing rates were well within normal limits and all patients but two had no permanent deformities after healing [9]. Some patients displayed deformities which were however temporary and quickly resolved due to the increased remodeling observed after fracture. All fractures were managed conservatively with no use of fixation materials. On the contrary, in another study, Dines et al. reported delayed healing and deformities in 25 thalassemia patients with fractures [10]. However, this study was published several decades ago, and the findings of impaired healing in this study might be related to the fact that the study was completed before the introduction of more frequent transfusion schemes and before the introduction of intensive chelation therapy. It is possible that similar defects might still be encountered in parts of the world where transfusion and chelation treatment schemes are still inadequate. In subsequent cohorts, there are only reports of occasional cases with delayed healing; however, they have been attributed to a concurrent severe vitamin C deficiency and are probably not the result of the disease per se [123].
Existing guidance
Several organizations have attempted to provide guidance regarding the diagnosis, follow-up, and treatment of TAO. The Thalassemia International Federation in 2014 issued a guidance on the management of transfusion dependant thalassemia [52]. The authors suggested annual check of BMD with DXA starting at adolescence, encouragement of physical activity, adequate calcium intake, vitamin D supplementation, smoking cessation, early diagnosis and treatment of diabetes mellitus, adequate blood transfusion and iron chelation, HRT in hypogonadal patients, and BSPs with treatment duration up to 2 years. The International Network on Growth Disorders and Endocrine Complications in Thalassemia (I-CET) issued a guideline on TAO in 2013 [73]. They suggested that BMD measurements should begin at age 10–12 and repeated every 2 years thereafter and that the bone markers carboxy-terminal telopeptide (CTX) and procollagen type 1 amino-terminal propeptide (P1NP) might be useful in the diagnosis of TAO and monitoring of treatment. An extensive guidance on the management of endocrine complications that have an impact on TAO as well as dietary recommendations were provided. The authors also suggested abstinence from smoking and alcohol and encouragement of physical activity, while for patients with established osteoporosis, they suggested that bone-specific treatment apart from HRT should be considered. However, it was acknowledged that there is no consensus on the best agent, dose, and duration of treatment.
Conclusion
Concerning adults with TAO, proposed indications for specific treatment are low BMD and low trauma fractures, with BSPs being the most studied agents, especially zoledronic acid. In the absence of fragility fractures, progressive significant BMD loss or even very low BMD values might be considered as an indication for specific treatment. These indications must be balanced against the need for lifelong treatment, the possible adverse effects of long-term BSPs administration on the skeleton, and the inability in most cases to normalize bone mass with current treatments. Based on data from postmenopausal women with osteoporosis, an initial 3-year course of zoledronic acid (or 5-year oral BSPs) might be the most prudent approach. During follow–up, the absence of skeletal events and stability of BMD, even at low values, is probably reassuring. On the contrary, progressive significant decrease of BMD and especially low trauma fractures is an absolute indication for reinstituting treatment. Anabolic therapy with teriparatide must be formally tested in interventional studies. Moreover, given that teriparatide could be administered only once in a lifetime, careful evaluation of current bone status and planning of long-term treatment is of paramount importance for successful management.
References
Weatherall DJ (1997) The thalassaemias. BMJ 314(7095):1675–1678
Borgna-Pignatti C, Cappellini MD, De Stefano P, Del Vecchio GC, Forni GL, Gamberini MR, Ghilardi R, Origa R, Piga A, Romeo MA, Zhao H, Cnaan A (2005) Survival and complications in thalassemia. Ann N Y Acad Sci 1054:40–47
Modell B, Darlison M (2008) Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ 86(6):480–487
Fung EB, Harmatz P, Milet M, Ballas SK, De Castro L, Hagar W, Owen W, Olivieri N, Smith-Whitley K, Darbari D, Wang W, Vichinsky E (2007) Multi-Center Study of Iron Overload Research Group. Morbidity and mortality in chronically transfused subjects with thalassemia and sickle cell disease: a report from the multi-center study of iron overload. Am J Hematol 82(4):255–265
Voskaridou E, Ladis V, Kattamis A, Hassapopoulou E, Economou M, Kourakli A, Maragkos K, Kontogianni K, Lafioniatis S, Vrettou E, Koutsouka F, Papadakis A, Mihos A, Eftihiadis E, Farmaki K, Papageorgiou O, Tapaki G, Maili P, Theohari M, Drosou M, Kartasis Z, Aggelaki M, Basileiadi A, Adamopoulos I, Lafiatis I, Galanopoulos A, Xanthopoulidis G, Dimitriadou E, Mprimi A, Stamatopoulou M, Haile ED, Tsironi M, Anastasiadis A, Kalmanti M, Papadopoulou M, Panori E, Dimoxenou P, Tsirka A, Georgakopoulos D, Drandrakis P, Dionisopoulou D, Ntalamaga A, Davros I, Karagiorga M, Group GHS (2012) A national registry of haemoglobinopathies in Greece: deducted demographics, trends in mortality and affected births. Ann Hematol 91(9):1451–1458
Baldini M, Forti S, Marcon A, Ulivieri FM, Orsatti A, Tampieri B, Airaghi L, Zanaboni L, Cappellini MD (2010) Endocrine and bone disease in appropriately treated adult patients with beta-thalassemia major. Ann Hematol 89(12):1207–1213
Vogiatzi MG, Macklin EA, Fung EB, Cheung AM, Vichinsky E, Olivieri N, Kirby M, Kwiatkowski JL, Cunningham M, Holm IA, Lane J, Schneider R, Fleisher M, Grady RW, Peterson CC, Giardina PJ, Network TCR (2009) Bone disease in thalassemia: a frequent and still unresolved problem. J Bone Miner Res 24(3):543–557
Exarchou E, Politou C, Vretou E, Pasparakis D, Madessis G, Caramerou A (1984) Fractures and epiphyseal deformities in beta-thalassemia. Clin Orthop Relat Res 189:229–233
Finsterbush A, Farber I, Mogle P, Goldfarb A (1985) Fracture patterns in thalassemia. Clin Orthop Relat Res 192:132–136
Dines DM, Canale VC, Arnold WD (1976) Fractures in thalassemia. J Bone Joint Surg Am 58(5):662–666
Fung EB, Harmatz PR, Milet M, Coates TD, Thompson AA, Ranalli M, Mignaca R, Scher C, Giardina P, Robertson S, Neumayr L, Vichinsky EP, Multi-Center Iron Overload Study Group (2008) Fracture prevalence and relationship to endocrinopathy in iron overloaded patients with sickle cell disease and thalassemia. Bone 43(1):162–168
Vogiatzi MG, Macklin EA, Fung EB, Vichinsky E, Olivieri N, Kwiatkowski J, Cohen A, Neufeld E, Giardina PJ (2006) Prevalence of fractures among the thalassemia syndromes in North America. Bone 38(4):571–575
Ruggiero L, De Sanctis V (1998) Multicentre study on prevalence of fractures in transfusion-dependent thalassaemic patients. J Pediatr Endocrinol Metab 11(Suppl 3):773–778
Sutipornpalangkul W, Janechetsadatham Y, Siritanaratkul N, Harnroongroj T (2010) Prevalence of fractures among Thais with thalassaemia syndromes. Singap Med J 51(10):817–821
Engkakul P, Mahachoklertwattana P, Jaovisidha S, Chuansumrit A, Poomthavorn P, Chitrapazt N, Chuncharunee S (2013) Unrecognized vertebral fractures in adolescents and young adults with thalassemia syndromes. J Pediatr Hematol Oncol 35(3):212–217
Bielinski BK, Darbyshire PJ, Mathers L, Crabtree NJ, Kirk JM, Stirling HF, Shaw NJ (2003) Impact of disordered puberty on bone density in beta-thalassaemia major. Br J Haematol 120(2):353–358
Wong P, Fuller PJ, Gillespie MT, Kartsogiannis V, Kerr PG, Doery JC, Paul E, Bowden DK, Strauss BJ, Milat F (2014) Thalassemia bone disease: a 19-year longitudinal analysis. J Bone Miner Res 29(11):2468–2473
Voskaridou E, Kyrtsonis MC, Terpos E, Skordili M, Theodoropoulos I, Bergele A, Diamanti E, Kalovidouris A, Loutradi A, Loukopoulos D (2001) Bone resorption is increased in young adults with thalassaemia major. Br J Haematol 112(1):36–41
Angelopoulos NG, Goula A, Katounda E, Rombopoulos G, Kaltzidou V, Kaltsas D, Konstandelou E, Tolis G (2007) Markers of bone metabolism in eugonadal female patients with beta-thalassemia major. Pediatr Hematol Oncol 24(7):481–491
Morabito N, Gaudio A, Lasco A, Atteritano M, Pizzoleo MA, Cincotta M, La Rosa M, Guarino R, Meo A, Frisina N (2004) Osteoprotegerin and RANKL in the pathogenesis of thalassemia-induced osteoporosis: new pieces of the puzzle. J Bone Miner Res 19(5):722–727
Mahachoklertwattana P, Sirikulchayanonta V, Chuansumrit A, Karnsombat P, Choubtum L, Sriphrapradang A, Domrongkitchaiporn S, Sirisriro R, Rajatanavin R (2003) Bone histomorphometry in children and adolescents with beta-thalassemia disease: iron-associated focal osteomalacia. J Clin Endocrinol Metab 88(8):3966–3972
Domrongkitchaiporn S, Sirikulchayanonta V, Angchaisuksiri P, Stitchantrakul W, Kanokkantapong C, Rajatanavin R (2003) Abnormalities in bone mineral density and bone histology in thalassemia. J Bone Miner Res 18(9):1682–1688
Bordat C, Constans A, Bouet O, Blanc I, Trubert CL, Girot R, Cournot G (1993) Iron distribution in thalassemic bone by energy-loss spectroscopy and electron spectroscopic imaging. Calcif Tissue Int 53(1):29–37
Chatterjee R, Shah FT, Davis BA, Byers M, Sooranna D, Bajoria R, Pringle J, Porter JB (2012) Prospective study of histomorphometry, biochemical bone markers and bone densitometric response to pamidronate in β-thalassaemia presenting with osteopenia-osteoporosis syndrome. Br J Haematol 159(4):462–471
Rioja L, Girot R, Garabédian M, Cournot-Witmer G (1990) Bone disease in children with homozygous beta-thalassemia. Bone Miner 8(1):69–86
Voskaridou E, Christoulas D, Plata E, Bratengeier C, Anastasilakis AD, Komninaka V, Kaliontzi D, Gkotzamanidou M, Polyzos SA, Dimopoulou M, Terpos E (2012) High circulating sclerostin is present in patients with thalassemia-associated osteoporosis and correlates with bone mineral density. Horm Metab Res 44(12):909–913
Voskaridou E, Christoulas D, Xirakia C, Varvagiannis K, Boutsikas G, Bilalis A, Kastritis E, Papatheodorou A, Terpos E (2009) Serum Dickkopf-1 is increased and correlates with reduced bone mineral density in patients with thalassemia-induced osteoporosis. Reduction post-zoledronic acid administration. Haematologica 94(5):725–758
Polyzos SA, Anastasilakis AD, Bratengeier C, Woloszczuk W, Papatheodorou A, Terpos E (2012) Serum sclerostin levels positively correlate with lumbar spinal bone mineral density in postmenopausal women—the six-month effect of risedronate and teriparatide. Osteoporos Int 23(3):1171–1176. doi:10.1007/s00198-010-1525-6
Memon AR, Butler JS, O’Riordan MV, Guerin E, Dimitrov BD, Harty JA (2013) Comparison of serum Dkk1 (Dickkopf-1) and bone mineral density in patients on bisphosphonate treatment vs no treatment. J Clin Densitom 16(1):118–124. doi:10.1016/j.jocd.2012.07.003
van Lierop AH, Moester MJ, Hamdy NA, Papapoulos SE (2014) Serum Dickkopf 1 levels in sclerostin deficiency. J Clin Endocrinol Metab 99(2):E252–E256
Centis F, Tabellini L, Lucarelli G, Buffi O, Tonucci P, Persini B, Annibali M, Emiliani R, Iliescu A, Rapa S, Rossi R, Ma L, Angelucci E, Schrier SL (2000) The importance of erythroid expansion in determining the extent of apoptosis in erythroid precursors in patients with beta-thalassemia major. Blood 96(10):3624–3629
Cazzola M, De Stefano P, Ponchio L, et al. (1995) Relationship between transfusion regimen and suppression of erythropoiesis in beta-thalassaemia major. Br J Haematol 89(3):473–478
Arnett TR (2010) Acidosis, hypoxia and bone. Arch Biochem Biophys 503(1):103–109
Lu H, Lian L, Shi D, Zhao H, Dai Y (2015) Hepcidin promotes osteogenic differentiation through the bone morphogenetic protein 2/small mothers against decapentaplegic and mitogen-activated protein kinase/P38 signaling pathways in mesenchymal stem cells. Mol Med Rep 11(1):143–150
Shen GS, Yang Q, Jian JL, Zhao GY, Liu LL, Wang X, Zhang W, Huang X, Xu YJ (2014) Hepcidin1 knockout mice display defects in bone microarchitecture and changes of bone formation markers. Calcif Tissue Int 94(6):632–639
Hiram-Bab S, Liron T, Deshet-Unger N, et al. (2015) Erythropoietin directly stimulates osteoclast precursors and induces bone loss. FASEB J 29(5):1890–1900
Yang Q, Jian J, Abramson SB, Huang X (2011) Inhibitory effects of iron on bone morphogenetic protein 2-induced osteoblastogenesis. J Bone Miner Res 26(6):1188–1196
Cunningham MJ, Macklin EA, Neufeld EJ, Cohen AR (2004) Thalassemia Clinical Research Network. Complications of beta-thalassemia major in North America. Blood 104(1):34–39
Jensen CE, Tuck SM, Agnew JE, Koneru S, Morris RW, Yardumian A, Prescott E, Hoffbrand AV, Wonke B (1998) High prevalence of low bone mass in thalassaemia major. Br J Haematol 103(4):911–915
Waung JA, Bassett JH, Williams GR (2012) Thyroid hormone metabolism in skeletal development and adult bone maintenance. Trends Endocrinol Metab 23(4):155–162
Angelopoulos NG, Goula A, Rombopoulos G, Kaltzidou V, Katounda E, Kaltsas D, Tolis G (2006) Hypoparathyroidism in transfusion-dependent patients with beta-thalassemia. J Bone Miner Metab 24(2):138–145
Dede AD, Tournis S, Dontas I, Trovas G (2014) Type 2 diabetes mellitus and fracture risk. Metabolism 63(12):1480–1490
Scacchi M, Danesi L, Cattaneo A, Valassi E, Pecori Giraldi F, Argento C, D’Angelo E, Mirra N, Carnelli V, Zanaboni L, Tampieri B, Cappellini MD, Cavagnini F (2008) Bone demineralization in adult thalassaemic patients: contribution of GH and IGF-I at different skeletal sites. Clin Endocrinol 69(2):202–207
Sadeghi-Bojd S, Hashemi M, Karimi M (2008) Renal tubular function in patients with beta-thalassaemia major in Zahedan, southeast Iran. Singap Med J 49(5):410–412
Ponticelli C, Musallam KM, Cianciulli P, Cappellini MD (2010) Renal complications in transfusion-dependent beta thalassaemia. Blood Rev 24(6):239–244
Quinn CT, Johnson VL, Kim HY, Trachtenberg F, Vogiatzi MG, Kwiatkowski JL, Neufeld EJ, Fung E, Oliveri N, Kirby M, Giardina PJ, Thalassemia Clinical Research Network (2011) Renal dysfunction in patients with thalassaemia. Br J Haematol 153(1):111–117
Baldan A, Giusti A, Bosi C, Malaventura C, Musso M, Forni GL, Volpato S, Zuliani G, Borgna-Pignatti C (2015) Klotho, a new marker for osteoporosis and muscle strength in β-thalassemia major. Blood Cells Mol Dis 55(4):396–401
Baldini M, Ulivieri FM, Forti S, Serafino S, Seghezzi S, Marcon A, Giarda F, Messina C, Cassinerio E, Aubry-Rozier B, Hans D, Cappellini MD (2014) Spine bone texture assessed by trabecular bone score (TBS) to evaluate bone health in thalassemia major. Calcif Tissue Int 95(6):540–546
Wong P, Fuller PJ, Gillespie MT, Kartsogiannis V, Strauss BJ, Bowden D, Milat F (2013) Thalassemia bone disease: the association between nephrolithiasis, bone mineral density and fractures. Osteoporos Int 24(7):1965–1971
Chan YL, Pang LM, Chik KW, Cheng JC, Li CK (2002) Patterns of bone diseases in transfusion-dependent homozygous thalassaemia major: predominance of osteoporosis and desferrioxamine-induced bone dysplasia. Pediatr Radiol 32(7):492–497
Olivieri NF, Koren G, Harris J, Khattak S, Freedman MH, Templeton DM, Bailey JD, Reilly BJ (1992) Growth failure and bony changes induced by deferoxamine. Am J Pediatr Hematol Oncol 14(1):48–56
Cappellini MD, Cohen A, Porter J, Taher A, Viprakasit V. (2014) Guidelines for the management of transfusion dependent thalassaemia (TDT). 3rd edition. Thalassaemia International Federation; ISBN-13: 978-9963-717-06-4
Naderi M, Sadeghi-Bojd S, Valeshabad AK, Jahantigh A, Alizadeh S, Dorgalaleh A, Tabibian S, Bamedi T (2013) A prospective study of tubular dysfunction in pediatric patients with beta thalassemia major receiving deferasirox. Pediatr Hematol Oncol 30(8):748–754
Wong P, Polkinghorne K, Kerr PG, Doery JC, Gillespie MT, Larmour I, Fuller PJ, Bowden DK, Milat F (2016) Deferasirox at therapeutic doses is associated with dose-dependent hypercalciuria. Bone 85:55–58
Casale M, Citarella S, Filosa A, De Michele E, Palmieri F, Ragozzino A, Amendola G, Pugliese U, Tartaglione I, Della Rocca F, Cinque P, Nobili B, Perrotta S (2014) Endocrine function and bone disease during long-term chelation therapy with deferasirox in patients with β-thalassemia major. Am J Hematol 89(12):1102–1106
Napoli N, Carmina E, Bucchieri S, Sferrazza C, Rini GB, Di Fede G (2006) Low serum levels of 25-hydroxy vitamin D in adults affected by thalassemia major or intermedia. Bone 38(6):888–892
Fung EB, Aguilar C, Micaily I, Haines D, Lal A (2011) Treatment of vitamin D deficiency in transfusion-dependent thalassemia. Am J Hematol 86(10):871–873
Fung EB (2010) Nutritional deficiencies in patients with thalassemia. Ann N Y Acad Sci 1202:188–196
Fung EB, Xu Y, Kwiatkowski JL, Vogiatzi MG, Neufeld E, Olivieri N, Vichinsky EP, Giardina PJ, Thalassemia Clinical Research Network (2010) Relationship between chronic transfusion therapy and body composition in subjects with thalassemia. J Pediatr 157(4):641–647
Trachtenberg F, Foote D, Martin M, Carson S, Coates T, Beams O, Vega O, Merelles-Pulcini M, Giardina PJ, Kleinert DA, Kwiatkowski J, Thompson AA, Neufeld EJ, Schilling L, Thayalasuthan V, Pakbaz Z, Yamashita R, Thalassemia Clinical Research Network (2010) Pain as an emergent issue in thalassemia. Am J Hematol 85(5):367–370
Haines D, Martin M, Carson S, Oliveros O, Green S, Coates T, Eile J, Schilling L, Dinu B, Mendoza T, Gerstenberger E, Trachtenberg F, Vichinsky E, Thalassemia Clinical Research Network (2013) Pain in thalassaemia: the effects of age on pain frequency and severity. Br J Haematol 160(5):680–687
Oliveros O, Trachtenberg F, Haines D, Gerstenberger E, Martin M, Carson S, Green S, Calamaras D, Hess P, Yamashita R, Vichinsky E, Thalassemia Clinical Research Network (2013) Pain over time and its effects on life in thalassemia. Am J Hematol 88(11):939–943
Forni GL, Perrotta S, Giusti A, Quarta G, Pitrolo L, Cappellini MD, D’Ascola DG, Borgna Pignatti C, Rigano P, Filosa A, Iolascon G, Nobili B, Baldini M, Rosa A, Pinto V, Palummeri E (2012) Neridronate improves bone mineral density and reduces back pain in β-thalassaemia patients with osteoporosis: results from a phase 2, randomized, parallel-arm, open-label study. Br J Haematol 158(2):274–282
Otrock ZK, Azar ST, Shamseddeen WA, Habr D, Inati A, Koussa S, Mahfouz RA, Taher AT (2006) Intravenous zoledronic acid treatment in thalassemia-induced osteoporosis: results of a phase II clinical trial. Ann Hematol 85(9):605–609
Voskaridou E, Anagnostopoulos A, Konstantopoulos K, Stoupa E, Spyropoulou E, Kiamouris C, Terpos E (2006) Zoledronic acid for the treatment of osteoporosis in patients with beta-thalassemia: results from a single-center, randomized, placebo-controlled trial. Haematologica 91(9):1193–1202
Green ST, Martin MB, Haines D, Carson S, Coates T, Oliveros O, Gerstenberger E, Trachtenberg F, Kwiatkowski JL, Network TCR (2014) Variance of pain prevalence and associated severity during the transfusion cycle of adult thalassaemia patients. Br J Haematol 166(5):797–800
Angelopoulos NG, Katounda E, Rombopoulos G, Goula A, Kaltzidou V, Kaltsas D, Ioannis P, Tolis G (2006) Evaluation of bone mineral density of the lumbar spine in patients with beta-thalassemia major with dual-energy X-ray absorptiometry and quantitative computed tomography: a comparison study. J Pediatr Hematol Oncol 28(2):73–78
Mylona M, Leotsinides M, Alexandrides T, Zoumbos N, Dimopoulos PA (2005) Comparison of DXA, QCT and trabecular structure in beta-thalassaemia. Eur J Haematol 74(5):430–437
Bansal D, Venkateshwaran S, Khandelwal N, Marwaha RK (2011) Quantitative computed tomography is unreliable for measurement of bone mineral density in inadequately chelated adolescent patients with β-thalassemia major: a case-control study. Pediatr Blood Cancer 56(3):409–412
Argentiero A, Neglia C, Peluso A, di Rosa S, Ferrarese A, Di Tanna G, Caiaffa V, Benvenuto M, Cozma A, Chitano G, Agnello N, Paladini D, Baldi N, Distante A, Piscitelli P (2013) The ability of lumbar spine DXA and phalanx QUS to detect previous fractures in young thalassemic patients with hypogonadism, hypothyroidism, diabetes, and hepatitis-B: a 2-year subgroup analysis from the Taranto Area of Apulia Region. J Pediatr Hematol Oncol 35(6):e260–e264
Christoforidis A, Perifanis V, Papadopoulou E, Dimitriadou M, Kazantzidou E, Vlachaki E, Tsatra I (2009) Poor correlations between measurements of bone quality by quantitative ultrasound sonography and dual energy X-ray absorptiometry in patients with beta-thalassaemia major. Eur J Haematol 82(1):15–21
Fung EB, Vichinsky EP, Kwiatkowski JL, Huang J, Bachrach LK, Sawyer AJ, Zemel BS (2011) Characterization of low bone mass in young patients with thalassemia by DXA, pQCT and markers of bone turnover. Bone 48(6):1305–1312
de Sanctis V, Soliman AT, Elsedfy H, Yassin M, Canatan D, Kilinc Y, Sobti P, Skordis N, Karimi M, Raiola G, Galati MC, Bedair E, Fiscina B, El Kholy M, I-CET (International Network on Growth Disorders and Endocrine Complications in Thalassemia) (2013) Osteoporosis in thalassemia major: an update and the I-CET 2013 recommendations for surveillance and treatment. Pediatr Endocrinol Rev 11(2):167–180
Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR (2011) Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ 342:d2040
Tang BM, Eslick GD, Nowson C, Smith C, Bensoussan A (2007) Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet 370(9588):657–666
Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, Bassford T, Beresford SA, Black HR, Blanchette P, Bonds DE, Brunner RL, Brzyski RG, Caan B, Cauley JA, Chlebowski RT, Cummings SR, Granek I, Hays J, Heiss G, Hendrix SL, Howard BV, Hsia J, Hubbell FA, Johnson KC, Judd H, Kotchen JM, Kuller LH, Langer RD, Lasser NL, Limacher MC, Ludlam S, Manson JE, Margolis KL, McGowan J, Ockene JK, O’Sullivan MJ, Phillips L, Prentice RL, Sarto GE, Stefanick ML, Van Horn L, Wactawski-Wende J, Whitlock E, Anderson GL, Assaf AR, Barad D, Women’s Health Initiative Investigators (2006) Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med 354(7):669–683
Chung M, Lee J, Terasawa T, Lau J, Trikalinos TA (2011) Vitamin D with or without calcium supplementation for prevention of cancer and fractures: an updated meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med 155(12):827–838
Avenell A, Gillespie WJ, Gillespie LD, O’Connell D (2009) Vitamin D and vitamin D analogues for preventing fractures associated with involutional and post-menopausal osteoporosis. Cochrane Database Syst Rev 15(2):CD000227
Lewis JR, Calver J, Zhu K, Flicker L, Prince RL (2011) Calcium supplementation and the risks of atherosclerotic vascular disease in older women: results of a 5-year RCT and a 4.5-year follow-up. J Bone Miner Res 26(1):35–41
Paik JM, Curhan GC, Sun Q, Rexrode KM, Manson JE, Rimm EB, Taylor EN (2014) Calcium supplement intake and risk of cardiovascular disease in women. Osteoporos Int 25(8):2047–2056
Fung EB, Kwiatkowski JL, Huang JN, Gildengorin G, King JC, Vichinsky EP (2013) Zinc supplementation improves bone density in patients with thalassemia: a double-blind, randomized, placebo-controlled trial. Am J Clin Nutr 98(4):960–971
Wu KH, Tsai FJ, Peng CT (2003) Growth hormone (GH) deficiency in patients with beta-thalassemia major and the efficacy of recombinant GH treatment. Ann Hematol 82(10):637–640
Arcasoy A, Ocal G, Kemahli S, Berberoğlu M, Yildirmak Y, Canatan D, Akçurin S, Akar N, Uysal Z, Adiyaman P, Cetinkaya E (1999) Recombinant human growth hormone treatment in children with thalassemia major. Pediatr Int 41(6):655–661
Sartorio A, Conte G, Conti A, Masala A, Alagna S, Rovasio P, Faglia G (2000) Effects of 12 months rec-GH therapy on bone and collagen turnover and bone mineral density in GH deficient children with thalassaemia major. J Endocrinol Investig 23(6):356–361
Mo D, Fleseriu M, Qi R, Jia N, Child CJ, Bouillon R, Hardin DS (2015) Fracture risk in adult patients treated with growth hormone replacement therapy for growth hormone deficiency: a prospective observational cohort study. Lancet Diabetes Endocrinol 3(5):331–338
Gilfillan CP, Strauss BJ, Rodda CP, Bowden DK, Kean AM, Obaid M, Crawford BA (2006) A randomized, double-blind, placebo-controlled trial of intravenous zoledronic acid in the treatment of thalassemia-associated osteopenia. Calcif Tissue Int 79(3):138–144
Perifanis V, Vyzantiadis T, Tziomalos K, Vakalopoulou S, Garipidou V, Athanassiou-Metaxa M, Harsoulis F (2007) Effect of zoledronic acid on markers of bone turnover and mineral density in osteoporotic patients with beta-thalassaemia. Ann Hematol 86(1):23–30
Leung TF, Chu Y, Lee V, Cheng FW, Leung WK, Shing MM, Li CK (2009) Long-term effects of pamidronate in thalassemic patients with severe bone mineral density deficits. Hemoglobin 33(5):361–369
Skordis N, Ioannou YS, Kyriakou A, Savva SC, Efstathiou E, Savvides I, Christou S (2008) Effect of bisphosphonate treatment on bone mineral density in patients with thalassaemia major. Pediatr Endocrinol Rev Suppl 1:144–148
Voskaridou E, Terpos E, Spina G, Palermos J, Rahemtulla A, Loutradi A, Loukopoulos D (2003) Pamidronate is an effective treatment for osteoporosis in patients with beta-thalassaemia. Br J Haematol 123(4):730–737
Patıroğlu T, Torun YA, Kula M, Karakükçü M (2008) Treatment of thalassemia-induced osteoporosis with intermittent pamidronate infusions: two-year follow up. Turk J Hematol 25(2):79–82
Pennisi P, Pizzarelli G, Spina M, Riccobene S, Fiore CE (2003) Quantitative ultrasound of bone and clodronate effects in thalassemia-induced osteoporosis. J Bone Miner Metab 21(6):402–408
Morabito N, Lasco A, Gaudio A, Crisafulli A, Di Pietro C, Meo A, Frisina N (2002) Bisphosphonates in the treatment of thalassemia-induced osteoporosis. Osteoporos Int 13(8):644–649
Shirani F, Iashkari M, Ahmadi AS, Arabi M, Asefi N (2012) Evaluation of alendronate efficacy on bone mineral density in thalassemic patients. Int J Hematol Oncol Stem Cell Res 6(4):20–24
Lasco A, Morabito N, Gaudio A, Buemi M, Wasniewska M, Frisina N (2001) Effects of hormonal replacement therapy on bone metabolism in young adults with beta-thalassemia major. Osteoporos Int 12(7):570–575
Anapliotou ML, Kastanias IT, Psara P, Evangelou EA, Liparaki M, Dimitriou P (1995) The contribution of hypogonadism to the development of osteoporosis in thalassaemia major: new therapeutic approaches. Clin Endocrinol 42(3):279–287
Yassin MA, Soliman AT, De Sanctis V, Abdelrahman MO, Aziz Bedair EM, AbdelGawad M (2014) Effects of the anti-receptor activator of nuclear factor kappa B ligand denusomab on beta thalassemia major-induced osteoporosis. Indian J Endocrinol Metab 18(4):546–551. doi:10.4103/2230-8210.137516
Chavassieux P, Meunier PJ, Roux JP, Portero-Muzy N, Pierre M, Chapurlat R (2014) Bone histomorphometry of transiliac paired bone biopsies after 6 or 12 months of treatment with oral strontium ranelate in 387 osteoporotic women: randomized comparison to alendronate. J Bone Miner Res 29(3):618–628
Morabito N, Catalano A, Gaudio A, Morini E, Bruno LM, Basile G, Tsiantouli E, Bellone F, Agostino RM, Piraino B, La Rosa MA, Salpietro C, Lasco A. Effects of strontium ranelate on bone mass and bone turnover in women with thalassemia major-related osteoporosis. J Bone Miner Metab. 2015 24. Epub
Blake GM, Lewiecki EM, Kendler DL, Fogelman I (2007) A review of strontium ranelate and its effect on DXA scans. J Clin Densitom 10(2):113–119
Canatan D, Akar N, Arcasoy A (1995) Effects of calcitonin therapy on osteoporosis in patients with thalassemia. Acta Haematol 93(1):20–24
Tournis S, Dede AD, Savvidis C, Triantafyllopoulos IK, Kattamis A, Papaioannou N (2015) Effects of teriparatide retreatment in a patient with β-thalassemia major. Transfusion 55(12):2905–2910
Trotta A, Corrado A, Cantatore FP (2010) Anabolic therapy of induced osteoporosis in beta-thalassaemia major: case report and literature review. Reumatismo 62(2):119–126
Hillard TC, Whitcroft SJ, Marsh MS, Ellerington MC, Lees B, Whitehead MI, Stevenson JC (1994) Long-term effects of transdermal and oral hormone replacement therapy on postmenopausal bone loss. Osteoporos Int 4(6):341–348
Misra M, Katzman D, Miller KK, Mendes N, Snelgrove D, Russell M, Goldstein MA, Ebrahimi S, Clauss L, Weigel T, Mickley D, Schoenfeld DA, Herzog DB, Klibanski A (2011) Physiologic estrogen replacement increases bone density in adolescent girls with anorexia nervosa. J Bone Miner Res 26(10):2430–2438
L’hermite M, Simoncini T, Fuller S, Genazzani AR (2008) Could transdermal estradiol + progesterone be a safer postmenopausal HRT? A review. Maturitas 60(3–4):185–201
Cappellini MD, Poggiali E, Taher AT, Musallam KM (2012) Hypercoagulability in β-thalassemia: a status quo. Expert Rev Hematol 5(5):505–511
Recommendation to restrict the use of Protelos/Osseor (Strontium ranelate), EMA/258269/2013. Accessed at http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2013/04/news_detail_001774.jsp&mid=WC0b01ac058001d126
Curhan GC, Willett WC, Speizer FE, Spiegelman D, Stampfer MJ (1997) Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann Intern Med 126(7):497–504
Ferrari S, Bianchi ML, Eisman JA, Foldes AJ, Adami S, Wahl DA, Stepan JJ, de Vernejoul MC, Kaufman JM, IOF Committee of Scientific Advisors Working Group on Osteoporosis Pathophysiology (2012) Osteoporosis in young adults: pathophysiology, diagnosis, and management. Osteoporos Int 23(12):2735–2748
Lewiecki EM (2011) Safety of long-term bisphosphonate therapy for the management of osteoporosis. Drugs 71(6):791–814
Lampropoulou-Adamidou K, Tournis S, Triantafyllopoulos IK (2016) Atypical femoral fracture in a beta-thalassemia major patient with previous bisphosphonate use: case report and a review of the literature. J Musculoskelet Neuronal Interact 16(1):75–78
Giusti A, Barone A, Balocco M, Pinto V, Pilotto A, Forni GL. (2015) Atypical fractures of the femur and bisphosphonate therapy in patients with beta thalassemia-associated osteoporosis: report of three cases [abstract #19]. In 10th Cooley’s Anemia Symposium, New York Academy of Sciences, New York
Leung F, Lau TW, To M, Luk KD, Kung AW. (2009) Atypical femoral diaphyseal and subtrochanteric fractures and their association with bisphosphonates. BMJ Case Rep. 2009. pii: bcr10.2008.1073.
Voskaridou E, Christoulas D, Konstantinidou M, Tsiftsakis E, Alexakos P, Terpos E (2008) Continuous improvement of bone mineral density two years post zoledronic acid discontinuation in patients with thalassemia-induced osteoporosis: long-term follow-up of a randomized, placebo-controlled trial. Haematologica 93(10):1588–1590
Black DM, Reid IR, Boonen S, Bucci-Rechtweg C, Cauley JA, Cosman F, Cummings SR, Hue TF, Lippuner K, Lakatos P, Leung PC, Man Z, Martinez RL, Tan M, Ruzycky ME, Su G, Eastell R (2012) The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res 27(2):243–254
Eriksen EF, Keaveny TM, Gallagher ER, Krege JH (2014) Literature review: the effects of teriparatide therapy at the hip in patients with osteoporosis. Bone 67:246–256
Eastell R, Nickelsen T, Marin F, Barker C, Hadji P, Farrerons J, Audran M, Boonen S, Brixen K, Gomes JM, Obermayer-Pietsch B, Avramidis A, Sigurdsson G, Glüer CC (2009) Sequential treatment of severe postmenopausal osteoporosis after teriparatide: final results of the randomized, controlled European Study of Forsteo (EUROFORS). J Bone Miner Res 24(4):726–736
Leder BZ, Tsai JN, Uihlein AV, Wallace PM, Lee H, Neer RM, Burnett-Bowie SA (2015) Denosumab and teriparatide transitions in postmenopausal osteoporosis (the DATA-Switch study): extension of a randomised controlled trial. Lancet 386(9999):1147–1155
Bishop N, Arundel P, Clark E, Dimitri P, Farr J, Jones G, Makitie O, Munns CF, Shaw N, International Society of Clinical Densitometry (2013) Fracture prediction and the definition of osteoporosis in children and adolescents: the ISCD 2013 Pediatric Official Positions. J Clin Densitom 17(2):275–280
Eghbali-Fatourechi G (2014) Bisphosphonate therapy in pediatric patients. J Diabetes Metab Disord 13(1):109
Pietri M, Lucarini S (2007) The orthopaedic treatment of fragility fractures. Clinical Cases in Mineral and Bone Metabolism 4(2):108–116
Michelson J, Cohen A (1988) Incidence and treatment of fractures in thalassemia. J Orthop Trauma 2(1):29–32
Acknowledgments
The authors would like to thank Irene Delikoura for her kind contribution in providing library services.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Dede, A.D., Trovas, G., Chronopoulos, E. et al. Thalassemia-associated osteoporosis: a systematic review on treatment and brief overview of the disease. Osteoporos Int 27, 3409–3425 (2016). https://doi.org/10.1007/s00198-016-3719-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3719-z