Abstract
Although spontaneous remission occurs in patients with idiopathic juvenile osteoporosis (IJO), permanent bone deformities may occur. The effects of long-term pamidronate treatment on clinical findings, bone mineral status, and fracture rate were evaluated. Nine patients (age 9.8 ± 1.1 years, 7 males) with IJO were randomized to intravenous pamidronate (0.8 ± 0.1 mg/kg per day for 3 days; cycles per year 2.0 ± 0.1; duration 7.3 ± 1.1 years; n = 5) or no treatment (n = 4). Fracture rate, phalangeal quantitative ultrasound, and lumbar bone mineral density (BMD) by dual energy X-ray absorptiometry at entry and during follow-up (range 6.3–9.4 years) were assessed. Bone pain improved in treated patients. Difficulty walking continued for 3–5 years in untreated patients, and vertebral collapses occurred in three of them. During follow-up, phalangeal amplitude-dependent speed of sound (AD-SoS), bone transmission time (BTT), and lumbar BMDarea and BMDvolume progressively increased in treated patients (P < 0.05–P < 0.0001). In untreated patients AD-SoS and BTT decreased during the first 2–4 years of follow-up (P < 0.05–P < 0.01); lumbar BMDarea increased after 6 years (P < 0.001) whereas BTT and lumbar BMDvolume increased after 7 years of follow-up (P < 0.05 and P < 0.001, respectively). At the end of follow-up, AD-SoS, BTT, lumbar BMDarea, and BMDvolume Z-scores were lower in untreated patients than in treated patients (−2.2 ± 0.3 and −0.5 ± 0.2; −1.9 ± 0.2 and −0.6 ± 0.2; −2.3 ± 0.3 and −0.7 ± 0.3; −2.4 ± 0.2 and −0.7 ± 0.3, P < 0.0001, respectively). Fracture rate was higher in untreated patients than in treated patients during the first 3 years of follow-up (P < 0.02). Our study showed that spontaneous recovery of bone mineral status is unsatisfactory in patients with IJO. Pamidronate treatment stimulated the onset of recovery phase reducing fracture rate and permanent disabilities without evidence of side-effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic juvenile osteoporosis (IJO), recognized by Dent and Friedman in 1965 [1] and subsequently well defined in its clinical features by Brenton and Dent in 1995 [2], is a rare primary form of osteoporosis of unknown etiology that develops in a previously healthy child. Diagnosis of IJO is based on the exclusion of known causes of osteoporosis in childhood, mainly the mild forms of osteogenesis imperfecta. Typical features of patients with IJO are fractures of the metaphyses and vertebral bodies after minimal trauma, pain in the back and extremities, and difficulty walking. With the exception of the most severe cases, patients with IJO have a gradual remission 1–5 years after the onset of puberty [1, 3, 4]. However, permanent disabilities, such as scoliosis, kyphosis, rib and spine deformities, and fractures may occur in young adulthood [3, 4], suggesting that remission cannot be complete and that some patients should be treated to improve bone health.
Treatment of patients with IJO is complicated by a clear lack of understanding of the cause of the disease. Moreover, the spontaneous recovery which may occur during skeletal growth is a confounding factor in examining the effects of treatments. Therapeutic trials with vitamin D or calcium supplements, calcitonin, and anabolic steroids failed to modify the natural course of IJO [5–7]. Conflicting data on the effect of calcitriol treatment in improving bone mineral density (BMD) and fracture rate were reported [6, 8, 9]. Some studies, the majority of them describing a single case, showed that bisphosphonate treatment improved symptoms and/or BMD [10–17], restored vertebral fractures [16], or reduced bone turnover [14]. However, to our knowledge, there are no studies assessing bone mass accrual and fracture rate in patients with IJO receiving bisphosphonate treatment compared with untreated patients.
The aim of the study was to examine the efficacy and safety of long-term pamidronate treatment on bone mineral status assessed by two different techniques at peripheral or axial skeleton and fracture rate in patients with IJO and to compare the results with untreated patients.
Materials and methods
Patients
Nine patients (7 males and 2 females) aged 8.1–11.4 years (9.8 ± 1.1 years, mean ± SD) affected by IJO were enrolled in a prospective study from the Pediatric Unit I of the University Hospital, Pisa. The diagnosis of IJO was based on the exclusion of all other known causes of osteoporosis in childhood, and according to the Dent and Brenton criteria [1, 2]. All patients showed progressive symptoms of back pain and difficulty walking, and two of them were confined to a wheelchair. Moreover, all patients suffered recurrent fractures at the metaphyses or diaphyses of long bones and/or at the vertebral bodies. In all patients, the typical extraskeletal manifestations of some forms of osteogenesis imperfecta (blue sclerae, dentinogenesis imperfecta, joint hyperlaxity, deafness, cardiac lesions) were absent. Family history for IJO and osteogenesis imperfecta was negative. All patients underwent collagen type I sequencing analysis; no mutation in one of the two genes encoding collagen type I alpha chains (COL1A1 and COL1A2) was observed. Karyotype was 46, XY in all boys and 46, XX in both girls.
Study design
At entry into the study the patients were randomized to receive intravenous pamidronate treatment (n = 5) or were untreated (n = 4). Anthropometric data in treated and untreated patients are summarized in Table 1; mean age, height, weight, and body mass index (BMI) did not differ between the two groups of patients. All patients were longitudinally examined for 7.6 ± 1.0 years (range 6.3–9.4 years).
Fracture rate and bone mineral status at phalanges of the hand by quantitative ultrasound (QUS) and BMD at lumbar spine by dual energy X-ray absorptiometry (DXA) were assessed in all patients at entry into the study and approximately every 12 months. The values of phalangeal QUS variables and lumbar BMD of patients were compared with appropriate sex and age reference values by using our own [18] and those reported by Boot et al. [19] which were obtained by the same DXA machinery and software we used, respectively. The values of phalangeal QUS variables and lumbar BMD, and fracture rate were compared between treated and untreated patients.
In all patients, clinical examination and biochemical measurements, including complete blood count, electrolytes, total alkaline phosphatase, hepatic and renal functional tests, and serum 25-hydroxyvitamin D (25-OH-D) concentrations were measured at entry and every 4–6 months throughout the study. Anthropometric data were assessed at entry and every 6 months during the study. Electrocardiographic examination was performed before and during each cycle of pamidronate infusion. Complete eye examination by an ophthalmologist and oral/dental examination by two odontologists were performed in all patients approximately every 6 months. Bisphosphonate-related osteonecrosis of the jaw (BRONJ) was defined according to the American Association of Oral and Maxillo-Facial Surgeons [20] and the American Society for Bone and Mineral Research [21] criteria.
Pamidronate treatment
In all treated patients, disodium pamidronate (Aredia, Novartis Pharma) was administered intravenously (0.5–1.0 mg/kg body weight per day) for three consecutive days for each cycle of infusion. Pamidronate diluted in 250 mL isotonic saline solution was infused over a 3-h period. In all treated patients, each intravenous pamidronate infusion was followed by intravenous 10 % calcium gluconate infusion (0.5 mg/kg body weight per day) diluted in 100 mL isotonic saline solution over a 1-h period. An additional intravenous 10 % calcium gluconate infusion was administered on the fourth day.
In all treated patients, serum calcium concentrations were measured each day before and after pamidronate infusion, as well as after 10 % calcium gluconate infusion. Serum calcium concentrations were also measured on the fourth day before and after 10 % calcium gluconate infusion. The protocol for pamidronate and 10 % calcium gluconate infusion, and the timing of serum calcium measurements are schematized in Fig. 1. All treated patients received a supplement of calcium salts as carbonate (25 mg/kg body weight per day as elemental calcium) for 2 weeks after each cycle of pamidronate.
All treated and untreated patients received a vitamin D supplement of 400 IU per day for the duration of the study.
Anthropometric measurements
Standing height and body weight were measured with a wall-mounted stadiometer and a mechanical balance, respectively. For each patient, both length and weight were the mean of three measurements. BMI was calculated using the formula weight (kg)/height (m)2. To allow a comparison between different ages and genders, height, weight, and BMI were expressed as Z-score according to the LMS method of Cole [22] and Cole and Green [23].
Phalangeal QUS measurements
The QUS device (DBM Sonic, IGEA, Carpi, Modena, Italy) is based on the transmission of ultrasound through the distal end of the proximal phalangeal diaphysis in the proximity of the condyles (region-of-interest, ROI) of the last four fingers of the hand. The ROI contains both cortical and trabecular bone, as well as a small medullary canal; the anatomic ROI is mostly cortical bone (approximately 60 %) [24]. The ROI does not have a growth plate, so that it is not a confounding factor in QUS measurements.
Amplitude-dependent speed of sound (AD-SoS, m/s) is a QUS variable reflecting the speed of sound through the proximal phalanx. It is calculated by measuring the width of the finger (including soft tissues) divided by the time of flight, defined as the time from emitted pulse to received signal considering the signal which reaches a predetermined minimum amplitude value (2 mV) for the first time; thus, the assessed ultrasound velocity is amplitude-dependent [25]. Bone transmission time (BTT, μs) is a QUS variable derived from the difference between the time when the first peak of the signal received attains its maximum and the time that would be measured if no bone but only soft tissue is present between the transducers. Therefore, BTT, unlike AD-SoS, is largely independent of ultrasound attenuation and soft tissue bias, and depends only on bone properties [26]. The final result is the average AD-SoS and BTT over four fingers (digit II–V). Further details of AD-SoS and BTT are reported elsewhere [18].
All the QUS measurements were performed by the same operator (GIB) on the nondominant hand. The coefficients of precision, in vivo, were 0.8 and 1.5 % for AD-SoS and BTT, respectively.
Lumbar BMD measurements
Lumbar BMDarea (bone mineral content corrected by the vertebral bone area scanned) was measured by posteroanterior DXA (Lunar-GE, DPX-L/PED, Madison, WI, USA) at L2–L4 level, a site which provides a measure of integral (cortical plus trabecular) bone. Lumbar BMDvolume was calculated as bone mineral content per bone volume estimated by the method of Kroger et al. [27] that assumes the lumbar vertebral body to have a cylindrical shape. The bone volume of each vertebral body was calculated as follows: volume = π × (diameter/2)2 × height, where diameter = width of vertebral body, and height = height of vertebral body. The validity of this model was assessed using in vivo volumetric data obtained from magnetic resonance imaging (MRI) of lumbar vertebrae [28]. Although the volume correction is not anatomical, lumbar BMDvolume values provide a better approximation of the true bone density than lumbar BMDarea [27, 29]. Width, height and bone area were provided by the DXA software program. The results were calculated as g/cm2 for lumbar BMDarea and as g/cm3 for lumbar BMDvolume.
The coefficient of precision, in vivo, was <1.0 % for both lumbar BMDarea and lumbar BMDvolume.
Assessment of fracture findings
The severity of injury was classified as slight or moderate according to Landin [30]. Slight trauma consisted of an injury caused by forces exerted by the injured individual (e.g., falling to the ground from standing on the same level, ball playing, running); moderate trauma consisted of an injury caused by forces connected to height above ground level (e.g.,, falling from between 0.5 and 3 m) or velocities (e.g., falling downstairs, from a bicycle or scooter, from swings or slides). In all patients, data on fractures were accurately reviewed and the sites of fractures were confirmed by examining the plain radiographs. Two or more fractures of the same bone caused by the same injury were recorded as one fracture.
In all patients fracture rate (number of fractures/patient-year) at entry and during follow-up was assessed.
Consent
Written informed consent to perform the study was obtained from a parent of each patient. The study was approved by the ethics committee for human investigation at our institution.
Statistical analysis
The results are expressed as mean ± SD. Nonparametric Wilcoxon’s (Mann–Whitney) rank-sum test was used to compare mean QUS variables (AD-SoS and BTT) and mean DXA variables (lumbar BMDarea and BMDvolume) data between patients and age and sex reference values, as well as to compare mean QUS and DXA variables results between treated and untreated patients at entry into the study and at each time point of measurement during follow-up, and to compare mean value of difference (Δ change Z-score) of QUS and DXA variables data between time point 0 and at the end of follow-up in treated versus untreated patients. Wilcoxon’s (Mann–Whitney) rank-sum test was also used to compare mean fracture rate, mean serum levels of biochemical parameters (calcium, phosphate, total alkaline phosphatase, and 25-OH-D concentrations) and mean values of the anthropometric data (height, weight, and BMI, Z-scores) between treated and untreated patients at entry into the study and at each time point of measurement during follow-up.
Two-ways analysis of variance (ANOVA) for repeated measurements with the time dependent parameter (years of follow-up) corrected by the Bonferroni method was used to compare the changes of QUS and DXA variables and fracture rate during follow-up with the values at entry into the study.
All statistical analyses were carried out using the SPSS (Statistical Package of Social Sciences, Chicago, IL, USA) for Windows software program version 16.0. A P value <0.05 was considered significant.
Results
Phalangeal QUS variables and lumbar BMD at entry
At entry, in all patients as a whole, mean AD-SoS and BTT Z-scores were reduced in comparison with their normal mean (−2.4 ± 0.2, P < 0.0001 and −2.7 ± 0.3, P < 0.001, respectively), as well as mean lumbar BMDarea and lumbar BMDvolume Z-scores (−3.8 ± 0.4, P < 0.0001, and −3.4 ± 0.5, P < 0.0001, respectively). There was no difference between treated and untreated patients for mean AD-SoS Z-score (−2.3 ± 0.1 and −2.4 ± 0.3, P = 0.41, respectively), BTT Z-score (−2.7 ± 0.3 and −2.7 ± 0.3, P = 0.96, respectively), lumbar BMDarea Z-score (−3.8 ± 0.5 and −3.9 ± 0.2, P = 0.82, respectively) and lumbar BMDvolume Z-score (−3.4 ± 0.5 and −3.4 ± 0.3, P = 0.90, respectively).
Pamidronate treatment duration, cycles, and doses
In treated patients, total duration of pamidronate treatment was 7.3 ± 1.1 years (range 6.3–9.4 years). The total number and the number of cycles per year of pamidronate were 14.4 ± 1.9 (range 13–18) and 2.0 ± 0.1 (range 1.9–2.1), respectively. The total and the mean dose (mg/body weight) of pamidronate were 1,570 ± 319 mg (range 1,366–2,135 mg) and 0.8 ± 0.1 mg (range 0.7–0.8 mg), respectively.
Clinical findings during follow-up
A rapid bone pain relief was observed in all treated patients; all of them were able to walk normally within a few weeks of starting pamidronate treatment, including the two patients who were confined to a wheelchair at entry. Sporadic pain at the hip occurred in one patient during the first year of pamidronate treatment. In all treated patients, zebra lines developed in the metaphyseal regions of growing bones, and increased vertebral height in previously fractured vertebrae occurred (Fig. 2).
Anteroposterior view of the distal part of femur and proximal part of tibia and fibula by plain standard radiograph (a) showing typical multiple zebra lines in one treated male patient (treated case 2, Table 1; age 14.2 years). Lateral view of the thoracic spine by plain standard radiograph in one treated male patient (treated case 1, Table 1; age 8.1 years) showing osteopenia of the vertebral bodies with mild deformity of T9 due to wedge pathological fracture at entry into the study (b) and showing improvement of osteopenia with ossification of the vertebral superior and inferior epiphyses and reshaping of the body of T9 after 4.7 years of pamidronate treatment (c)
Duration of follow-up was 8.0 ± 0.6 years (range 7.2–8.8 years) in untreated patients. Bone pain with difficulty walking continued for 3–5 years in all untreated patients. To reduce severe bone pain they received nonsteroideal anti-inflammatory drugs for some days or weeks with a partial remission of symptoms. During the first year of follow-up, one patient was confined to wheelchair for some months due to severe back and hip pain associated with severe difficulty walking. At the end of follow-up, two patients developed scoliosis and two showed lumbar spine deformities due to some vertebral collapses (Fig. 3).
Anteroposterior (a) and lateral (b) view of the last three thoracic and lumbar vertebrae by plain standard radiographs in one untreated male patient (untreated case 2, Table 1; age 16.7 years) showing severe biconcave pathological vertebral collapse of L1, mild biconcave deformity of L2 and L5, with near total fusion of the inferior endplate of L4 with the superior endplate of L5. Severe scoliosis with rotation on the frontal plane of some vertebral bodies was also evident. MRI of the last two thoracic, lumbar and sacral vertebrae in lateral view (c) in one untreated male patient (untreated case 1, Table 1; age 17.7 years) showing biconcave deformity due to pathological fracture of L3
At the end of follow-up, mean height Z-score decreased significantly in untreated patients (−0.4 ± 0.2, P < 0.05), whereas it did not change (0.4 ± 0.3, P = 0.15) in treated patients in comparison with the value at entry; however, mean height Z-score was higher (P < 0.01) in treated than in untreated patients at the end of the study. Weight and BMI Z-scores did not vary in both treated (P = 0.40 and P = 0.55, respectively) and untreated (P = 0.99 and P = 0.65, respectively) patients (data not shown).
Changes of phalangeal QUS variables and lumbar BMD during follow-up
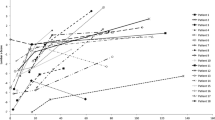
Figure 4 shows mean and individual values of phalangeal AD-SoS and BTT Z-scores, and lumbar BMDarea and BMDvolume Z-scores during follow-up. In treated patients, mean values of AD-SoS and BTT Z-scores, and mean values of lumbar BMDarea and BMDvolume Z-scores increased significantly. In untreated patients mean values of AD-SoS and BTT Z-scores decreased significantly during the first 2–4 years of follow-up; subsequently, mean AD-SoS Z-score did not vary in comparison with the value at entry, whereas mean BTT Z-score increased significantly after 7 years of follow-up. Mean values of lumbar BMDarea and BMDvolume Z-scores showed a significant increase after 6 and 7 years of follow-up, respectively. Furthermore, mean values of AD-SoS and BTT Z-scores and mean values of lumbar BMDarea Z-scores were lower in untreated patients than in treated patients at each time point of measurement during follow-up; whereas, mean BMDvolume Z-scores were lower in untreated patients compared with treated patients after the second year of follow-up.
Changes in mean values of phalangeal QUS variables and lumbar BMD, expressed as Z-score, in treated (broken thick black lines) and untreated (solid thick black lines) patients during follow-up. Solid and broken thin black lines represent the changes of the individual values in treated (filled symbols) and untreated (empty symbols) patients, respectively. 0 on the abscissa is the time at entry into the study. The letters represent the comparison of the mean value in treated or untreated patients at each time point of measurement versus the value at entry; P value is reported in the box. Panel a and b show phalangeal QUS variables AD-SoS and BTT Z-scores, respectively; panel c and panel d show lumbar BMDarea and lumbar BMDvolume Z-scores, respectively. Comparison of mean values between treated and untreated patients at entry and during each time point of measurement during follow-up are AD-SoS, P = 0.41 at time point 0; P < 0.001 at time point 1; P < 0.0001 at time points 2–7. BTT, P = 0.96 at time point 0; P < 0.01 at time points 1; P < 0.001 at time points 2, 4, 6, and 7; P < 0.0001 at time points 3 and 5. BMDarea, P = 0.82 at time point 0; P < 0.05 at time point 1; P < 0.01 at time points 2 and 4; P < 0.001 at time points 3, and 5–7. BMDvolume, P = 0.90 and P = 0.10 at time points 0 and 1, respectively; P < 0.01 at time point 2; P < 0.001 at time points 3 and 4; P < 0.0001 at time points 5–7
At the end of follow-up, mean values of phalangeal QUS variables and lumbar BMD in treated and untreated patients were AD-SoS, −0.5 ± 0.2 Z-score and −2.2 ± 0.3 Z-score, P < 0.0001, respectively; BTT, −0.6 ± 0.2 Z-score and −1.9 ± 0.2 Z-score, P < 0.0001, respectively; BMDarea, −0.7 ± 0.3 Z-score and −2.3 ± 0.3 Z-score, P < 0.0001, respectively; BMDvolume, −0.7 ± 0.3 Z-score and −2.4 ± 0.2 Z-score, P < 0.0001, respectively). Moreover, Δ changes of mean values of phalangeal QUS variables and lumbar BMD between time point 0 and at the end of follow-up were significantly higher in treated than in untreated patients (AD-SoS, 1.8 ± 0.3 Z-score and −0.2 ± 0.2 Z-score, P < 0.0001, respectively; BTT, 2.1 ± 0.4 Z-score and 0.8 ± 0.4 Z-score, P < 0.01, respectively; BMDarea, 3.1 ± 0.4 Z-score and 1.6 ± 0.5 Z-score, P < 0.001, respectively; BMDvolume, 2.7 ± 0.3 Z-score and 0.9 ± 0.2 Z-score, P < 0.0001, respectively).
Sites of fractures and fracture rate at entry and during follow-up
Number and sites of fractures in treated and untreated patients at entry and during follow-up are summarized in Table 2. At entry, a total of forty fractures occurred in all patients; the total number of fractures in treated patients was similar to that of untreated patients. During follow-up, the total number of fractures was twice as high in untreated patients compared to treated patients.
Both at entry and during follow-up, the majority of treated and untreated patients suffered fractures of the upper limb. During follow-up four fractures of lumbar spine occurred in three untreated male patients; whereas, no treated patient suffered vertebral fractures.
A slight trauma was the cause of fracture in all treated and untreated patients. None of the treated patients showed atypical femur fractures. In treated patients who sustained fractures pamidronate was administered no earlier than 1 month after the complete fracture repair as documented by plain radiographs.
Figure 5 shows the fracture rate in treated and untreated patients at entry and during follow-up. At entry, fracture rate did not differ (P = 0.50) between treated and untreated patients, but during the first 3 years of follow-up it was significantly higher in untreated than in treated patients. Fracture rate decreased significantly after 2 and 6 years of follow-up in treated and untreated patients compared with the value at entry, respectively.
Fracture rate (number of fractures per patient-year) in treated (black columns) and untreated (white columns) patients at entry (0) and during follow-up. The letters represent the comparison of the mean value in treated or untreated patients at each time point of measurement vs. the value at entry; P value is reported in the box. Comparison of mean values between treated and untreated patients at entry and during each time point of measurement during follow-up are P = 0.50 at time point 0; P < 0.02 at time points 1–3; P = 0.30 and P = 0.11 at time points 4 and 5, respectively. Bars represent mean ± SD
Changes of serum calcium concentrations during pamidronate treatment
On day 1 of the first cycle of pamidronate mean serum calcium concentrations decreased significantly after pamidronate infusion (before, 9.4 ± 0.4 mg/dL; post-pamidronate, 8.0 ± 0.2 mg/dL; P < 0.0001), but they increased significantly after 10 % calcium gluconate infusion (10.3 ± 0.5 mg/dL; P < 0.01 vs before and P < 0.0001 vs post-pamidronate). Similar changes of serum calcium concentrations were observed on day 2 and 3 (data not shown). On day 4, before and after 10 % calcium gluconate infusion serum calcium concentrations were 8.9 ± 0.5 mg/dL and 10.8 ± 0.6 mg/dL (P < 0.001), respectively. Similar changes of serum calcium concentrations were found during the subsequent cycles of pamidronate (data not shown). No treated patient had symptomatic hypocalcemia.
Biochemical parameters at entry and during follow-up
Mean serum levels of calcium, phosphate, total alkaline phosphatase, and 25-OH-D did not differ between treated and untreated patients at entry into the study (9.4 ± 0.2 and 9.4 ± 0.3 mg/dL, P = 0.99, respectively; 4.9 ± 0.4 and 4.8 ± 0.3 mg/dL, P = 0.69, respectively; 432.4 ± 42.3 and 407.5 ± 51.0 IU/L, P = 0.45, respectively; 23.4 ± 1.3 and 22.3 ± 1.2 ng/mL, P = 0.23, respectively) and during follow-up (9.3 ± 0.3 and 9.5 ± 0.4 mg/dL, P = 0.42, respectively; 4.8 ± 0.2 and 4.7 ± 0.2 mg/dL, P = 0.48, respectively; 451.4 ± 30.8 and 427.0 ± 36.5 IU/L, P = 0.16, respectively; 27.6 ± 2.3 and 26.3 ± 2.4 ng/mL, P = 0.44, respectively).
In all treated patients complete blood count, as well as hepatic and renal functions were normal throughout the entire follow-up period.
Adverse effects during pamidronate treatment
An acute-phase reaction including mild fever and malaise was observed in four of five patients during the first cycle of pamidronate. Mild fever occurred in two patients during the second cycle of pamidronate too. None of the patients had fever during the following cycles of pamidronate. One patient had myalgia during the first pamidronate cycle. Symptoms were self-limiting and resolved over hours to a few days; symptomatic treatment with paracetamol or other analgesics/antipyretics was effective in reducing the symptoms.
No patient showed prolonged corrected QT interval or arrhythmias after pamidronate infusion. Moreover, none of the patients had severe side-effects, such as uveitis, periscleritis, scleritis, skin reactions, or BRONJ.
Discussion
The mechanisms leading to the onset and the spontaneous resolution of IJO are unknown. It has been suggested that bone pain in patients with IJO likely reflects the accumulation of microfractures which are a consequence of the striking imbalance between muscle and bone tissue at onset and during the acute phase of disease. During the recovery phase, normalization of the muscle−bone relationship was associated with improvement of BMD and progressive disappearance of bone pain and fractures [31]. These results indicate that the rate of bone mass accrual occurring during prepuberty and early puberty could be a trigger mechanism in patients with IJO.
Some patients with IJO do not have a complete disease remission during the recovery phase that usually occurs with the progression of puberty [3, 4, 31]. Likely, some of them should be treated to improve the accumulation of bone mass and to reduce fracture rate and permanent disabilities. Although there is no a reliable treatment in patients with IJO, bisphosphonates would seem to be the most effective therapy for improving painful symptoms and bone mass accumulation [10–17].
Our treated patients showed complete recovery of painful symptoms, normalization of bone mineral status at phalanges of the hand and lumbar spine, and reduction of fracture rate without changes of linear growth. Conversely, untreated patients had a variable degree of bone pain and difficulty walking for 3–5 years associated with higher fracture rate during the first 3 years of follow-up and lower bone mineral status at both phalanges of the hand and lumbar spine during the entire follow-up period compared to treated patients. In addition, untreated patients showed a mild but significant mean height Z-score reduction, due at least in part, to the vertebral collapses which occurred in all the three males; indeed, mean height Z-score was lower in untreated than in treated patients at the end of follow-up. These data indicate that the spontaneous bone mass accrual occurring during the recovery from disease was impaired in our untreated patients. Similar data were reported in some patients with IJO by Płudowski et al. [31] who showed only a partial increase of BMD assessed at lumbar spine and total skeleton during the progression of puberty.
IJO could affect the attainment of peak bone mass at lumbar spine and phalanges of the hand, which are usually achieved, in both sexes, within the second [32] and third [33, 34] decade of life, respectively. Indeed, at age 29, the untreated patient we previously described [9] had reduced lumbar and femoral neck BMDarea (−2.9 T-score and −2.5 T-score, respectively) by DXA, and phalangeal AD-SoS and BTT (−2.2 T-score and −2.6 T-score, respectively) by QUS associated with recurrent back pain which required prolonged analgesic therapy (personal unpublished data).
Although spontaneous recovery might have influenced, at least in part, the outcome in our treated patients, pamidronate treatment was able to modify the natural course of IJO stimulating the onset of the recovery phase. This suggests that it may be justified in patients with IJO on the basis of potential benefit compared to risk, as also suggested by Shaw et al. [13] and Speiser et al. [35]. Conversely, none of the untreated patients showed complete disappearance of symptoms or complete recovery of bone mineral status during the progression of puberty; moreover, some lumbar spine deformities were found in late adolescence, as also found by Smith [3] and Płudowski [31]. Nevertheless, we cannot exclude that the reduced bone mineral status and the severe disabilities would not have occurred in our own untreated patients if they had received pamidronate treatment.
The optimum duration and dose of bisphosphonate therapy in patients with IJO are unknown. In a patient with severe IJO who showed a clinical, biochemical and radiological improvement during parenteral clodronate administration recurrent bone pain and one fracture occurred within a year of stopping the treatment; a rapid improvement was again evident when the treatment was reinstated [17]. This may indicate that bisphosphonate therapy should be continued until disease remission is achieved, as also suggested by Hoekman et al. [10] and Melchior et al. [17].
Histological studies have shown that reduced bone formation rather than increased bone resorption was a main cause of IJO [36, 37]. These data were confirmed by more recent histomorphometric studies that demonstrated a marked decrease in cancellous bone volume with reduced trabecular thickness and number, and impaired osteoblast team performance without evidence of increased bone resorption [38]. The process mainly affects bone surfaces that are in contact with the bone marrow cavity, including the internal cortex [39].
The main effect of bisphosphonate therapy is to inhibit osteoclast-mediated bone resorption by disrupting the activity and survival of osteoclasts; as a result, the number of highly mineralized bone modeling units increases leading to increased BMD [40]. However, bisphosphonates may also enhance viability of osteoblasts and osteocytes contributing to the reduction of osteoclasts formation and activity [41]. The positive effect of bisphosphonates on bone formation, even in the face of reduced overall bone remodeling, could explain part of the anti-fracture efficacy and bone mass recovery found in patients with IJO receiving this treatment. Indeed, our treated patients showed reshaping of vertebral bodies associated with normal metaphyseal growth of long bones with the occurrence of the typical zebra lines related to cyclical bisphosphonate therapy [42], likely reflecting horizontal trabeculae undergoing turnover [43]. This suggests that physeal growth is still occurring, with a relative increase in bone formation as can occur with uncoupling of osteoblastic and osteoclastic activity [42]. Therefore, the effects on bone mass accrual and bone modeling could reflect a positive influence of pamidronate treatment on endochondral ossification in patients with IJO.
No patient had severe side-effects associated with pamidronate treatment, including BRONJ and atypical femur fractures. These severe complications have not been reported with bisphosphonate therapy in any child or adolescent to date [44, 45]. None of our treated patients had symptomatic hypocalcemia during pamidronate infusion. However, severe hypocalcemia with tetany was observed in our own patient with IJO during the first cycle of pamidronate who did not receive 10 % calcium gluconate infusion (not enrolled in this study, unpublished data). Pamidronate treatment did not affect serum phosphate and total alkaline phosphatase levels. A vitamin D supplement of 400 IU per day provided adequate 25-OH-D levels (>20 ng/mL) according to the recent indications by the Institute of Medicine [46] in all treated and untreated patients, without any difference between them, for the entire duration of the study.
Our study has some limitations. The number of the examined patients is small but the rarity of IJO makes it difficult to recruit larger numbers. Another limitation is the lack of placebo control design. On the other hand, the strength of our study is its longitudinal design and the length of the follow-up throughout the pubertal years in both treated and untreated patients. In all patients the compliance with the study was good for entire duration of the follow-up period.
In conclusion, in untreated patients with IJO spontaneous recovery of bone mineral status may be unsatisfactory and it may be associated with increased fracture rate and permanent disabilities in late adolescence. In patients with IJO parenteral pamidronate treatment stimulates the onset of recovery phase improving bone mineral status, reducing fracture rate, and preventing skeletal deformities. These effects may contribute to improve the quality of life of patients with IJO who are receiving pamidronate treatment.
Although pamidronate treatment may be justified in patients with IJO by the fact that potential benefits on bone health would outweigh any potential risk, further studies are needed to better define criteria for treatment, treatment duration, and dosing regimen of pamidronate.
References
Dent CE, Friedman M (1965) Idiopathic juvenile osteoporosis. Q J Med 34:177–210
Brenton DP, Dent CE (1995) Idiopathic juvenile osteoporosis. In: Bicket JH, Stern J (eds) Inborn errors of calcium and bone metabolism. University Park Press, Baltimore, pp 223–238
Smith R (1995) Idiopathic juvenile osteoporosis: experience of twenty-one patients. Br J Rheumatol 34:68–77
Lorenc RS (2002) Idiopathic juvenile osteoporosis. Calcif Tissue Int 70:395–397
Teotia M, Teotia SPS, Singh RK (1979) Idiopathic juvenile osteoporosis. Am J Dis Child 133:894–900
Jackson EC, Strife F, Tsang RC, Marder HK (1988) Effect of calcitonin replacement therapy in idiopathic juvenile osteoporosis. Am J Dis Child 142:1237–1239
Krassas GE (2000) Idiopathic juvenile osteoporosis. Ann N Y Acad Sci 900:409–412
Marder HK, Tsang RC, Hug G, Crawford AC (1982) Calcitriol deficiency in idiopathic juvenile osteoporosis. Am J Dis Child 136:914–917
Saggese G, Bertelloni S, Baroncelli GI, Perri G, Calderazzi A (1991) Mineral metabolism and calcitriol therapy in idiopathic juvenile osteoporosis. Am J Dis Child 145:457–462
Hoekman K, Papapoulos SE, Peters ACB, Bijvoet OLM (1985) Characteristics and bisphosphonate treatment of a patient with juvenile osteoporosis. J Clin Endocrinol Metab 61:952–956
Tick D, Singer F, Rimoin D (1991) Pamidronate disodium in the treatment of idiopathic juvenile osteoporosis. Am J Hum Genet 49:S180 (abs)
Levis S, Gruber HE, Cohn D, Howard GA, Roos BA (1993) Juvenile osteoporosis treated with pamidronate. Calcif Tissue Int 52:S41 (abs)
Shaw NJ, Boivin CM, Crabtree NJ (2000) Intravenous pamidronate in juvenile osteoporosis. Arch Dis Child 83:143–145
Kaufman RP, Overton TH, Shiflett M, Jennings JC (2001) Osteoporosis in children and adolescent girls: case report of idiopathic juvenile osteoporosis and review of the literature. Obstet Gynecol Surv 56:492–504
Gandrup LM, Cheung JC, Daniels MW, Bachrach LK (2003) Low-doses intravenous pamidronate reduces fractures in childhood osteoporosis. J Pediatr Endocrinol Metab 16:887–892
Sumník Z, Land C, Rieger-Wettengl G, Körber F, Stabrey A, Schoenau E (2004) Effect of pamidronate treatment on vertebral deformity in children with primary osteoporosis. A pilot study using radiographic morphometry. Horm Res 61:137–142
Melchior R, Zabel B, Spranger J, Schumacher R (2005) Effective parenteral clodronate treatment of a child with severe juvenile idiopathic osteoporosis. Eur J Pediatr 164:22–27
Baroncelli GI, Federico G, Vignolo M, Valerio G, del Puente A, Maghnie M, Baserga M, Farello G, Saggese G, The Phalangeal Quantitative Ultrasound Group (2006) Cross-sectional reference data for phalangeal quantitative ultrasound from early childhood to young-adulthood according to gender, age, skeletal growth, and pubertal development. Bone 39:159–173
Boot AM, De Ridder MAJ, Pols HAP, Krenning EP, De Muinck Keizer-Schrama SMPF (1997) Bone mineral density in children and adolescents: relation to puberty, calcium intake, and physical activity. J Clin Endocrinol Metab 82:57–62
American Association of Oral and Maxillofacial Surgeons (2007) Position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg 65:369–376
Khosla S, Burr D, Cauley J, Dempster DW, Ebeling PR, Felsenberg D, Gagel RF, Gilsanz V, Guise T, Koka S, McCauley LK, McGowan J, McKee MD, Mohla S, Pendrys DG, Raisz LG, Ruggiero SL, Shafer DM, Shum L, Silverman SL, Van Poznak CH, Watts N, Woo SB, Shane E, American Society for Bone and Mineral Research (2007) Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 22:1479–1491
Cole TJ (1990) The LMS method for constructing normalized growth standards. Eur J Clin Nutr 44:45–60
Cole TJ, Green PJ (1992) Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med 11:1305–1319
Njeh CF, Richards A, Boivin CM, Hans D, Fuerst T, Genant HK (1999) Factors influencing the speed of sound through the proximal phalanges. J Clin Densitom 2:241–249
Cadossi R, Canè V (1996) Pathways of transmission of ultrasound energy through the distal metaphysis of the second phalanx of pigs: an in vitro study. Osteoporos Int 6:196–206
Barkmann R, Rohrschneider W, Vierling M, Troger J, De Terlizzi F, Cadossi R, Heller M, Glüer CC (2002) German pediatric reference data for quantitative transverse transmission ultrasound of finger phalanges. Osteoporos Int 13:55–61
Kroger H, Kotaniemi A, Vainio P, Alhava E (1992) Bone densitometry of the spine and femur in children by dual-energy X-ray absorptiometry. Bone Miner 17:75–85
Kroger H, Vainio P, Nieminen J, Kotaniemi A (1995) Comparison of different models for interpreting bone mineral density measurements using DXA and MRI technology. Bone 17:157–159
Baroncelli GI, Bertelloni S, Ceccarelli C, Saggese G (1998) Measurement of volumetric bone mineral density accurately determines degree of lumbar undermineralization in children with growth hormone deficiency. J Clin Endocrinol Metab 83:3150–3154
Landin LA (1983) Fracture patterns in children. Acta Orthop Scand (Suppl 202) 54:1–109
Płudowski P, Lebiedowski M, Olszaniecka M, Marowska J, Matusik H, Lorenc RS (2006) Idiopathic juvenile osteoporosis: an analysis of the muscle-bone relationship. Osteoporos Int 17:1681–1690
Rizzoli R, Bianchi ML, Garabédian M, McKay HA, Moreno LA (2010) Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Bone 46:294–305
Wuster C, Albanese C, De Aloysio D, Duboeuf F, Gambacciani M, Gonnelli S, Glüer CC, Hans D, Joly J, Reginster JY, De Terlizzi F, Cadossi R, The Phalangeal Osteosonogrammetry Study Group (2000) Phalangeal osteosonogrammetry study: age-related changes, diagnostic sensitivity, and discrimination power. J Bone Miner Res 15:1603–1614
Montagnani A, Gonnelli S, Cepollaro C, Mangeri M, Monaco R, Bruni D, Gennari C (2000) Quantitative ultrasound at the phalanges in healthy Italian men. Osteoporos Int 11:499–504
Speiser PW, Clarson CL, Eugster EA, Kemp SF, Radovick S, Rogol AD, Wilson TA, LWPES Pharmacy and Therapeutic Committee (2005) Bisphosphonate treatment of pediatric bone disease. Pediatr Endocrinol Rev 3:87–96
Smith R (1980) Idiopathic osteoporosis in the young. J Bone Joint Surg 62B:417–427
Evans RA, Dunstan CR, Hills E (1983) Bone metabolism in idiopathic juvenile osteoporosis: a case report. Calcif Tissue Int 35:5–8
Rauch F, Travers R, Norman ME, Taylor A, Parfitt AM, Glorieux FH (2000) Deficient bone formation in idiopathic juvenile osteoporosis: a histomorphometric study of cancellous iliac bone. J Bone Miner Res 15:957–963
Rauch F, Travers R, Norman ME, Taylor A, Parfitt AM, Glorieux FH (2002) The bone formation defect in idiopathic juvenile osteoporosis is surface-specific. Bone 31:85–89
Rogers MJ, Crockett JC, Coxon FP, Mönkkönen J (2011) Biochemical and molecular mechanisms of action of bisphosphonates. Bone 49:34–41
Bellido T, Plotkin LI (2011) Novel actions of bisphosphonates in bone: preservation of osteoblast and osteocyte viability. Bone 49:50–55
Al Muderis M, Azzopardi T, Cundy P (2007) Zebra lines of pamidronate therapy in children. J Bone Joint Surg Am 89:1511–1516
Rauch F, Travers R, Munns C, Glorieux FH (2004) Sclerotic metaphyseal lines in a child treated with pamidronate: histomorphometric analysis. J Bone Miner Res 19:1191–1193
Chahine C, Cheung MS, Head TW, Schwartz S, Glorieux FH, Rauch F (2008) Tooth extraction socket healing in pediatric patients treated with intravenous pamidronate. J Pediatr 153:719–720
Maines E, Monti E, Doro F, Morandi G, Cavarzere P, Antoniazzi F (2012) Children and adolescents treated with neridronate for osteogenesis imperfecta show no evidence of any osteonecrosis of the jaw. J Bone Miner Metab 30:434–438
Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G, Kovacs CS, Mayne ST, Rosen CJ, Shapses SA (2011) The 2011 report on dietary reference intakes for calcium and vitamin D from the institute of medicine: what clinicians need to know. J Clin Endocrinol Metab 96:53–58
Acknowledgments
The authors are very grateful to the parents of all the patients for their consent and help to perform the study.
Conflict of interest
All authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Baroncelli, G.I., Vierucci, F., Bertelloni, S. et al. Pamidronate treatment stimulates the onset of recovery phase reducing fracture rate and skeletal deformities in patients with idiopathic juvenile osteoporosis: comparison with untreated patients. J Bone Miner Metab 31, 533–543 (2013). https://doi.org/10.1007/s00774-013-0438-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-013-0438-9