Abstract
A prospective observational study to test the effects of risedronate 17.5 mg/week treatment on quality of life (QOL) of 1,363 Japanese female patients with osteoporosis showed QOL improvement after 12 weeks of administration. Comorbid factors such as ischemic heart disease, hip osteoarthritis, and higher values of FRAX blunted the effects of QOL of the treatment. Few studies have investigated the effect of osteoporosis treatment on QOL in relationship to comorbid factors other than osteoporosis and fracture. Efficacy was determined by changes over time in EQ-5D at baseline, at 12 and 24 weeks, and at the final assessment. Factors affecting changes in EQ-5D were evaluated with a multivariate analysis. Safety was determined by assessing the incident rate of adverse events. The improvement of EQ-5D compared to baseline was observed as significant after 12 weeks of treatment (p < 0.001). The greatest improvement was observed in the dimension of “pain/discomfort” by the multivariate analysis (p < 0.001). Factors affecting QOL improvement were FRAX value without BMD, age, glucocorticoid use, ischemic heart disease, hip osteoarthritis, and pain. The incidence rate of drug-related adverse events was 4.72 % (95 % confidence interval 3.63–6.02 %). Risedronate at 17.5 mg/week improved the QOL in patients with osteoporosis among Japanese women, and comorbidity factors decreased the effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a skeletal disease with an increased risk of fractures [1]. Commonly associated diseases relating to lifestyle have been shown to increase the risk of fractures, consequently affecting the quality of life (QOL) of patients with osteoporosis. These diseases include ischemic heart disease [2], hypertension [2, 3], heart failure [2–4], diabetes [5–7], arteriosclerosis [2, 8, 9], and dyslipidemia [9–11]. Joint diseases including rheumatoid arthritis [12–14] and hip and knee osteoarthritis are also shown to reduce QOL [15–19]. However, the effect of comorbid factors in patients with osteoporosis has not been well investigated in relationship to the efficacy of improvement in QOL by treatment of osteoporosis. In this prospective observational study, we investigated the effects of risedronate (Actonel tablet) 17.5 mg/week on QOL improvement and safety in patients with osteoporosis. We also analyzed the effects of comorbid factors on QOL using EQ-5D [20, 21].
Materials and methods
Study design and subjects
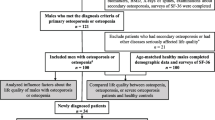
The present study was conducted in 307 medical institutions in Japan. The registration period was from November 2008 through June 2009: 1,363 women with osteoporosis who had not previously been treated with risedronate (17.5 mg/week) were registered prospectively by the central registration method, and the study period was set to continue until June 2010. Eligible subjects were those given diagnosis of osteoporosis using the criteria of the Japanese Primary Osteoporosis Diagnosis (2000 revised version) who had a QOL evaluation at baseline using the Japanese version of the EQ-5D at baseline. The study period was 24 weeks from the start of risedronate weekly administration with evaluations performed at 12 and 24 weeks. The data at 12 or 24 weeks were used for the final assessment depending on the follow-up period of the patients. Items for assessment included age, gender, height, weight, and prevalent comorbid factors. The primary efficacy endpoint was the utility value of the EQ-5D. Adverse events (AEs) were also examined by type and degree of severity.
The present study was conducted in compliance with ministerial ordinances concerning investigation after manufacturing and sales of Japanese medicines and study performance criteria GPSP (Good Post-marketing Study Practice).
EQ-5D
The EQ-5D consists of five dimensions (5D) and a visual assessment scale (VAS) [20, 21]. The five dimensions are “mobility,” “self-care,” “usual activities,” “pain/discomfort,” and “anxiety/depression”; each dimension was evaluated by three levels of grading. Subsequently, the scores obtained from the subjects were converted to utility values (EQ-5D[utility]) (−0.111 to 1.000) using the HRQOL score conversion table. For the VAS assessment, subjects evaluated their health status ranging from “best imaginable health state” (100) to “worst imaginable health state” (0). Background factors influencing changes in EQ-5D[utility] at the final assessment were investigated. When one or more levels of the grading increased from baseline in each dimension, the value of 1 was assigned for “Improved,” and when one or more level decreased or did not change, the value of 0 was assigned for “Not improved.”
FRAX (fracture risk assessment tool)
At registration, the values of major osteoporotic fracture risk and hip fracture risk without bone mineral density (FRAX without BMD) were calculated by entering risk factors into the Japanese version of the Fracture Risk Assessment Tool (FRAX®) (Web Version 3.1). The entered risk factors were age, gender, height, weight, previous fracture, parent had fractured hip, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, and alcohol intake (3 or more units/day). When required items were entered as “Unknown” [except for age, gender, and body mass index (BMI)], they were described as “None.”
Statistical analysis
To identify differences in the value of EQ-5D[utility] between two time points, a paired t test was used (Fig. 1). In addition, a two-sample t test was also performed to compare two level factors. An analysis of variance (ANOVA) was done to compare three or more level factors. For efficacy analyses, differences in the values of EQ-5D[utility] between baseline and the final assessment were used for the five dimensions as criterion variables, using multivariate analyses (Table 2). To investigate the comorbid factors influencing EQ-5D[utility] changes, multiple variable analyses were also performed (Table 3). For safety analyses, the incidence rates of AEs were calculated by preferred term (PT) (Table 4). All statistical analyses were performed SAS (ver. 8.2 or later). A two-sided 95 % confidence interval (95 % CI) was used for estimation of interval. A value of p < 0.05 was considered statistically significant.
Results
Subjects
During the registration period, 1,363 subjects were enrolled. Questionnaires were collected from 1,356 subjects, and for 1,069 subjects whose EQ-5, BMD, or bone metabolism markers were evaluated at baseline the efficacy analysis was performed. The safety analysis included 1,292 subjects; the 223 subjects who were not evaluated for reason of missing data at the final assessment were excluded from the safety analysis.
The discontinuation rate was 9.45 % (101 of 1,069 subjects). No significant differences were detected in EQ-5D[utility] values between subjects who discontinued or completed the study at the baseline, 12 weeks, 24 weeks, or at the final assessment (p = 0.644, 0.911, 0.388, and 0.340, respectively; two-sample t test). The reasons for discontinuation were “not visit again (70 cases),” “adverse events (14 cases),” “refusal to the treatment (7 cases),” “invalid (4 cases),” and others (9 cases) (duplicate tabulation).
Baseline characteristics of the subject
The baseline characteristics of the 1,069 subjects included in the efficacy analysis are shown in Table 1. The mean age (±SD) was 73.5 ± 8.9 years. The mean duration of osteoporosis after the period of diagnosis was 1.94 ± 3.98 years. The mean values of EQ-5D[utility] and EQ-5D[VAS] were 0.7064 ± 0.1991 and 63.70 ± 19.25. The mean FRAX without BMD and FRAX Hip without BMD were 19.05 ± 10.71 and 7.78 ± 7.35, respectively.
Efficacy assessment
The mean values of the EQ-5D[utility] were 0.7064 ± 0.1991 (baseline), 0.7797 ± 0.1855 (12 weeks), 0.8039 ± 0.1921 (24 weeks), and 0.8006 ± 0.1885 (final) (Fig. 1). The differences from baseline were significant (p < 0.001) starting at 12 weeks. The mean values and the changes in EQ-5D[VAS] were also increased. The estimated values of each explanatory variable by multivariate analysis at the final assessment were 0.195 (p < 0.001) for pain/discomfort, 0.134 (p < 0.001) for mobility, 0.078 (p < 0.001) for anxiety/depression, 0.064 (p < 0.001) for usual activities, and 0.051 (p < 0.001) for self-care (Table 2).
Pain showed a significant increase at the final assessment with an estimated value of 0.123 (p = 0.028) (Table 3). Factors that contributed to reduce the EQ-5D[utility] values during the treatment were age (estimated value −0.003, p < 0.001), glucocorticoid use (estimated value −0.056, p = 0.041), ischemic heart disease (estimated value −0.059, p = 0.045), and hip osteoarthritis (estimated value −0.130, p = 0.013). Factors that did not affect the EQ-5D[utility] were BMI, previous fracture, parent fractured hip, current smoking, rheumatoid arthritis, secondary osteoporosis, alcohol intake (3 or more units/day), arrhythmia, heart failure, hypertension, arteriosclerosis, diabetes, dyslipidemia, cervical spondylosis, lumbar spondylosis, knee osteoarthritis, spinal canal stenosis, and concomitant use of NSAIDs.
In a multivariate analysis model where the fracture risk factor is replaced with FRAX without BMD as an explanatory variable, factors that decreased EQ-5D[utility] were the FRAX without BMD value (estimated value −0.002, p < 0.001) and hip osteoarthritis (estimated value −0.125, p = 0.017). The changes in EQ-5D[utility] significantly correlated with FRAX values without BMD at baseline (coefficients of correlation −0.29), but the changes in EQ-5D[VAS] did not correlate with the FRAX without BMD baseline values.
Adverse events
In the safety analysis (1,292 subjects), AEs were observed in 112 cases. The incidence rate was 8.672 % with a 95 % CI of 7.19–10.34 %. Drug-related AEs were observed in 61 cases (4.72 %, 95 % CI 3.63–6.02 %). The major drug-related AEs were “abdominal discomfort” (14 cases, 1.08 %), “upper abdominal pain” (9 cases, 0.70 %), “dyspepsia” (7 cases, 0.54 %), “gastritis” (4 cases, 0.31 %), “diarrhea” (3 cases, 0.23 %), and “dizziness,” “gastric ulcer,” “nausea,” “reflux esophagitis,” and “malaise” (2 cases each, 0.15 %) (Table 4). The most frequent drug-related AEs were gastrointestinal disorders (50 cases, 3.56 %). Serious drug-related AEs included “osteomyelitis” and “cholelithiasis,” in 1 case each (0.08 %).
Discussion
The results of the present study demonstrated significant improvement in the QOL values of EQ-5D in patients with osteoporosis after 12 weeks of risedronate treatment. The highest improvement in the criteria of EQ-5D[utility] was found in the “pain/discomfort” category. We also found that the factors attenuating the effect of risedronate on QOL were age, ischemic heart disease, hip osteoarthritis, and glucocorticoid use. The FRAX values without BMD affected the efficacy of the treatment on the QOL.
Improvement of pain with the treatment of once daily administration of risedronate (2.5 mg) has also been observed in patients with osteoporosis by many investigators [22–26]. A decrease in the parameters evaluating pain by VAS has been observed in 2–4 weeks after the start of the treatment with daily dosing [22, 23]. Similarly, improvement in the parameters evaluating pain by SF-36 or Japanese Osteoporosis Quality of Life Questionnaire (JOQOL) has been observed in 4–12 months after the start of the treatment with daily dosing [24–26]. In this study, we observed a significant reduction of the value in the category of pain/discomfort in the EQ-5D after the first 12 weeks of weekly risedronate administration. Thus, the reduction of pain seemed to be consistent in both daily and weekly treatments of risedronate. This study confirmed the effect of pain with 17.5 mg risedronate treatment.
There are reports that risedronate shows a higher rate of improvement in the SF-36 bodily pain than etidronate and a lower rate of improvement than elcatonin [24, 26]. In this study, the increase in the total EQ-5D[utility] is associated with a decrease in pain/discomfort. Therefore, it is anticipated that the improvement of QOL by risedronate may be mainly the result of the effect of alleviation of pain. Multivariate analysis in this study did not find an effect of concomitant use of NSAIDs on either the total EQ-5D[utility] or the specific category of pain/discomfort. Thus, the effects of risedronate and NSAIDs on the alleviation of pain may be different in patients with osteoporosis.
Many factors including age, gender (being female), low BMI [27], low BMD [28, 29], previous fracture [30, 31], current smoking [32], alcohol intake [33], glucocorticoid use [34, 35], parent fractured hip [36], and rheumatoid arthritis [37, 38] have been reported to increase the fracture risk in patients with osteoporosis. Factors of age, previous fracture, and rheumatoid arthritis are also shown to affect QOL independently from consequent fracture. In this study, we found that age and glucocorticoid use affect the improvement of QOL in the early period of risedronate treatment, but previous fracture and rheumatoid arthritis did not reduce the effect on QOL. Thus, the relationships of fracture risk factors and QOL seem to be variable depending on the population of the subjects in the study. We found that FRAX values without BMD have a negative relationship with the changes in EQ-5D[utility] values. The efficacy of QOL improvement by risedronate treatment may be related to FRAX-integrated major risk factors in individuals.
Changes in QOL by risedronate treatment seem to depend on the comorbidities of lifestyle-related diseases in patients with osteoporosis. In this study we found that comorbidity of ischemic heart disease and medication with glucocorticoid use blunted the changes in EQ-5D[utility] values by risedronate treatment. It has been reported that lifestyle-related diseases, such as diabetes, ischemic heart disease; hypertension, heart failure, arrhythmia, arteriosclerosis, and dyslipidemia, are associated with an increased risk of hip fracture [2–4, 8, 9]. This association is independent from decreasing BMD. In our study these comorbid diseases seemed to reduce the increase in EQ-5D[utility] values during osteoporosis treatment. We are not certain of the reason for the oppression of these comorbid diseases on the efficacy of QOL. The limited activities resulting from these lifestyle-related diseases could obscure the efficacy on QOL in the osteoporosis treatment by risedronate.
Among comorbidities of skeletal disorders other than osteoporosis, hip osteoarthritis was the confounding factor to affect the improvement of QOL by risedronate treatment. Other association of skeletal disorders such as degenerative spondylosis, spinal canal stenosis, and knee osteoarthritis did not have any influence on the response of the treatment by EQ-5D[utility] assessments. The reduction in QOL has been well confirmed in patients with osteoarthritis because of pain, limited range of motion of the affected joints, and associated muscle weakness [15, 19]. Blunting the response of QOL to treatment in patients with hip osteoarthritis seems to relate to the limited activities caused by joint dysfunction. No association with knee osteoarthritis as a factor to reduce the efficacy of risedronate on QOL may be the result of the wide degree of QOL effects by the disease.
The rates of drug-related AEs observed in this study (4.72 %) seem to be lower than the values (2.5 mg for 32.2 %, 17.5 mg for 24.9 %) reported in the regulatory approval of the study using weekly 17.5 mg risedronate dosing in Japan [39]. The difference in the rate of drug-related AEs is probably the result of the presence or absence of source document verification (SDV) by monitors. Additionally, it may also occur because the presence of abnormal clinical and laboratory findings has been entrusted to the investigator’s judgment. The most frequent drug-related AEs in this study were gastrointestinal disorders (3.56 %), which are generally known to be a drug-related AE of bisphosphonate use [40]. The mechanism of onset is considered to be dependent on the frequency of contact with the gastrointestinal mucosa [41]. The results in this study were similar to the safety profile in previous literature reports including studies using daily risedronate at 2.5 mg and 5 mg dosing [24, 39, 42–44].
Limitations of this study include that administration of risedronate 4 months later significantly increases the BMD of the lumbar spine (L1–L4) and the femur (neck and total), and there is a report suggesting the possibility of reducing fracture risk [45]. Because the BMD data at final assessment were insufficient, the influence of BMD on QOL could not be sufficiently examined in this study.
In conclusion, we observed an improvement of QOL of patients with osteoporosis by risedronate 17.5 mg weekly dosing in daily practice. The improvements were blunted in patients with comorbidities. It is necessary to consider comorbidities before assessing the QOL effect in the treatment of osteoporosis.
References
(2000) Osteoporosis prevention, diagnosis, and therapy. NIH Consensus Statement 17:1–45
Sennerby U, Melhus H, Gedeborg R, Byberg L, Garmo H, Ahlbom A, Pedersen NL, Michaëlsson K (2009) Cardiovascular diseases and risk of hip fracture. JAMA 302:1666–1673
Vestergaard P, Rejnmark L, Mosekilde L (2009) Hypertension is a risk factor for fractures. Calcif Tissue Int 84:103–111
Carbone L, Buzková P, Fink HA, Lee JS, Chen Z, Ahmed A, Parashar S, Robbins JR (2010) Hip fractures and heart failure: findings from the Cardiovascular Health Study. Eur Heart J 31:77–84
Viégas M, Costa C, Lopes A, Griz L, Medeiro MA, Bandeira F (2011) Prevalence of osteoporosis and vertebral fractures in postmenopausal women with type 2 diabetes mellitus and their relationship with duration of the disease and chronic complications. J Diabetes Complications 25:216–221
Melton LJ 3rd, Leibson CL, Achenbach SJ, Therneau TM, Khosla S (2008) Fracture risk in type 2 diabetes: update of a population-based study. J Bone Miner Res 23:1334–1342
Janghorbani M, Van Dam RM, Willett WC, Hu FB (2007) Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 166:495–505
Samelson EJ, Cupples LA, Broe KE, Hannan MT, O’Donnell CJ, Kiel DP (2007) Vascular calcification in middle-age and long term risk of hip fracture: the Framingham Study. J Bone Miner Res 22:1449–1454
Bagger YZ, Rasmussen HB, Alexandersen P, Werge T, Christiansen C, Tankó LB, PERF study group (2007) Links between cardiovascular disease and osteoporosis in postmenopausal women: serum lipids or atherosclerosis per se? Osteoporos Int 18:505–512
Holmberg AH, Johnell O, Nilsson PM, Nilsson J, Berglund G, Akesson K (2006) Risk factors for fragility fracture in middle age. A prospective population-based study of 33,000 men and women. Osteoporos Int 17:1065–1077
Yamaguchi T, Sugimoto T, Yano S, Yamauchi M, Sowa H, Chen Q, Chihara K (2002) Plasma lipids and osteoporosis in postmenopausal women. Endocr J 49:211–217
Miyakoshi N, Itoi E, Kobayashi M, Kodama H (2003) Impact of postural deformities and spinal mobility on quality of life in postmenopausal osteoporosis. Osteoporos Int 14:1007–1012
Anonymous (2006) Guidelines for prevention and treatment of osteoporosis. Life Science Publishing, Tokyo, pp 61–63
Bazzichi L, Maser J, Piccinni A, Rucci P, Del Debbio A, Vivarelli L, Catena M, Bounani S, Merlini G, Bombardieri S, DellOsso L (2005) Quality of life in rheumatoid arthritis: impact of disability and lifetime depressive spectrum symptomatology. Clin Exp Rheumatol 23:783–788
Hopman-Rock M, Kraaimaat FW, Bijlsma JW (1997) Quality of life in elderly subjects with pain in the hip or knee. Qual Life Res 6:67–76
van der Waal JM, Terwee CB, van der Windt DA, Bouter LM, Dekker J (2005) Health-related and overall quality of life of patients with chronic hip and knee complaints in general practice. Qual Life Res 14:795–803
Moskowitz RW (2009) The burden of osteoarthritis: clinical and quality-of-life issues. Am J Manag Care 15:S223–S229
Altman RD (2010) Early management of osteoarthritis. Am J Manag Care 16(suppl):S41–S47
Muraki S, Akune T, Oka H, En-Yo Y, Yoshida M, Saika A, Suzuki T, Yoshida H, Ishibashi H, Tokimura F, Yamamoto S, Nakamura K, Kawaguchi H, Yoshimura N (2010) Impact of knee and low back pain on health-related quality of life in Japanese women: the Research on Osteoarthritis Against Disability (ROAD). Med Rheumatol 20:444–451
Brooks R with the EuroQol Group (1996) EuroQol: the current state of play. Health Policy 37:53–72
Ikegami N, Fukuhara S, Shimozuma K, Ikeda S (2001) QOL evaluation handbook for clinical practice. Igakushoin, Tokyo, pp 14–18
Saika A, Matsunaka H (2005) Studies of the effect of risedronate on removal of lower back pain in patients with osteoporosis and the effect on improvement of QOL. Osteoporos Jpn 13:485–490
Ohtori S, Akazawa T, Murata Y, Kinoshita T, Yamashita M, Nakagawa K, Inoue G, Nakamura J, Orita S, Ochiai N, Kishida S, Takaso M, Eguchi Y, Yamauchi K, Suzuki M, Aoki Y, Takahashi K (2010) Risedronate decreases bone resorption and improves low back pain in postmenopausal osteoporosis patients without vertebral fractures. J Clin Neurosci 17:209–213
Kushida K, Fukunaga M, Kishimoto H, Shiraki M, Itabashi A, Inoue T, Kaneda K, Morii H, Nawata H, Yamamoto K, Ohashi Y, Orimo H (2004) A comparison of incidences of vertebral fracture in Japanese patients with involutional osteoporosis treated with risedronate and etidronate: a randomized, double-masked trial. J Bone Miner Metab 22:469–478
Ohbayashi H (2009) Examination of beneficial effects of risedronate in improving quality of life during long-term treatment of primary osteoporosis. Nippon Rinsho 67:2009
Fujita T, Ohue M, Nakajima M, Fujii Y, Miyauchi A, Takagi Y (2011) Comparison of the effects of elcatonin and risedronate on back and knee pain by electroalgometry using fall of skin impedance and quality of life assessment using SF-36. J Bone Miner Metab 29:588–597
De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ 3rd, Meunier PJ, Pols HA, Reeve J, Silman A, Tenenhouse A (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330–1338
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fracture. BMJ 312:1254–1259
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ 3rd, O’Neill T, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA III, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garmero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone (NY) 35:375–382
Kanis JA, Johnell O, Oden A, Johansson H, De Laet C, Eisman JA, Fujiwara S, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Smoking and fracture risk: a meta-analysis. Osteoporos Int 16:155–162
Kanis JA, Johansson H, Johnell O, Oden A, De Laet C, Eisman JA, Pols H, Tenenhouse A (2005) Alcohol intake as a risk factor for fracture. Osteoporos Int 16:737–742
van Staa TP, Leufkens HG, Cooper C (2002) The epidemiology of corticosteroid-induce osteoporosis: a meta-analysis. Osteoporos Int 13:777–787
Kanis JA, Johansson H, Oden A, Johnell O, de Laet C, Melton LJ III, Tenenhouse A, Reeve J, Silman AJ, Pols HA, Eisman JA, McCloskey EV, Mellstrom D (2004) A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res 19:893–899
Kanis JA, Johansson H, Oden A, Johnell O, De Laet C, Eisman JA, McCloskey EV, Mellstrom D, Melton LJ 3rd, Pols HA, Reeve J, Silman AJ, Tenenhouse A (2004) A family history of fracture and fracture risk: a meta-analysis. Bone (NY) 35:1029–1037
Hooyman J, Melton LR, Nelson A, O’Fallon W, Riggs B (1984) Fractures after rheumatoid arthritis. A population-based study. Arthritis Rheum 27:1353–1361
van Staa TP, Geusens P, Bijlsma JW, Leufkens HG, Cooper C (2006) Clinical assessment of the long-term risk of fracture in patients with rheumatoid arthritis. Arthritis Rheum 54:3104–3112
Kishimoto H, Fukunaga M, Kushida K, Shiraki M, Itabashi A, Nawata H, Nakamura T, Ohta H, Takaoka K, Ohashi Y; Risedronate Phase III Research Group (2006) Efficacy and tolerability of once-weekly administration of 17.5 mg risedronate in Japanese patients with involutional osteoporosis: a comparison with 2.5 mg once-daily dosage regimen. J Bone Miner Metab 24:405–413, 439
Peter CP, Kindt MV, Majka JA (1998) Comparative study of potential for bisphosphonates to damage gastric mucosa of rats. Dig Dis Sci 43:1009–1015
Bone HG, Adami S, Rizzoli R, Favus M, Ross PD, Santra A, Praharada S, Daifotis A, Orloff J, Yates J (2000) Weekly administration of alendronate: rationale and plan for clinical assessment. Clin Ther 22:15–28
Shiraki M, Fukunaga M, Kushida K, Kishimoto H, Taketani Y, Minaguchi H, Inoue T, Morita R, Morii H, Yamamoto K, Ohashi Y, Orimo H (2003) A double-blind dose-ranging study of risedronate in Japanese patients with osteoporosis (a study by the Risedronate Late Phase II Research Group). Osteoporos Int 14:225–234
Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH 3rd, Brown J, Eriksen EF, Hoseyni MS, Axelrod DW, Miller PD (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. JAMA 282:1344–1352
Reginster J, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML, Lund B, Ethgen D, Pack S, Roumagnac I, Eastell R (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int 11:83–91
Takakuwa M, Iwamoto J, Konishi M, Qi Zhou Itabashi K (2011) Risedronate improves proximal femur bone density and geometry in patients with osteoporosis or osteopenia and clinical risk factors of fractures: a practice-based observational study. J Bone Miner Metab 29:88–95
Acknowledgments
The authors are very grateful to the physicians at the 307 nationwide institutions for providing valuable data and cooperation. This study was supported by the Eisai Co., Ltd., Tokyo, Japan and the Ajinomoto Pharmaceutical Co., Ltd., Tokyo, Japan.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Nakamura, T., Osawa, M., Itoh, M. et al. The effect of risedronate (17.5 mg/week) treatment on quality of life in Japanese women with osteoporosis: a prospective observational study. J Bone Miner Metab 30, 715–721 (2012). https://doi.org/10.1007/s00774-012-0372-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-012-0372-2