Abstract
We investigated changes in quality of life (QOL), including pain, in Japanese women aged ≥ 55 years who were diagnosed as having osteoporosis at 265 centers across Japan and treated continuously with once-weekly bisphosphonates for 24 months. In 2650 evaluable patients, a significant improvement in QOL was observed from 3 months after enrollment onward and maintained throughout the 2-year observation period. A significant improvement in scores was observed for all domains of the Euro QOL 5 Dimension (EQ-5D), and the “pain”, “health perception”, and “posture, figure” domains of the Japanese Osteoporosis QOL Questionnaire (JOQOL). Factors identified as significantly contributing to QOL change were “fractures within the year before enrollment”, “presence of spondylosis deformans”, “presence of osteoarthritis”, “use of activated vitamin D3”, and “age” based on the JOQOL, and “presence of spondylosis deformans”, “use of activated vitamin D3”, and “age” based on the EQ-5D. The results suggested that the patients’ perception of treatment effects, such as improvement in pain, contributes to treatment continuation. Osteoporosis patients should be informed that continuous treatment with once-weekly bisphosphonates can lead to a significant improvement in QOL regardless of concomitant locomotor diseases, to encourage them to remain on treatment. In conclusion, continuous bisphosphonate treatment improved the QOL even in patients with locomotor diseases, and the concomitant use of activated vitamin D3 may also facilitate further improvement in QOL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the rapidly aging population, the number of patients with osteoporosis is increasing yearly in Japan. On the basis of the prevalence of osteoporosis (among persons aged ≥ 40 years), as determined according to the bone mineral density (BMD) of the lumbar vertebrae and femoral neck in large-scale cohort studies [1, 2], there are estimated 12.8 million osteoporotic patients (3 million men and 9.8 million women) [3], making the prevention and treatment of osteoporosis an important issue.
The guidelines proposed by the Japan Osteoporosis Society, Japanese Society for Bone and Mineral Research, and others state that the treatment of osteoporosis should aim to “maintain and improve the quality of life (QOL) by reducing fracture risk” [3]. The Japanese Osteoporosis QOL Questionnaire (JOQOL) was established for properly assessing the QOL of Japanese osteoporotic patients, taking into account the Japanese lifestyle [4]. The Euro QOL 5 Dimension (EQ-5D) is a non-disease-specific QOL questionnaire also used for calculating utility scores in health economic analyses. Only a few clinical studies have used these QOL assessment tools to evaluate responses to pharmacological treatments in Japanese osteoporotic patients. Particularly, no large-scale observational study has been conducted to evaluate the long-term QOL of osteoporotic patients receiving treatment in a real-world setting. This study aimed to investigate changes in QOL, including pain, in Japanese middle-aged to elderly women diagnosed as having osteoporosis and treated with once-weekly bisphosphonates at medical institutions across Japan in a 2-year, large-scale, prospective, multicenter, observational study.
Materials and methods
Study overview
A multicenter observational study was conducted in 265 participating centers across Japan between November 1, 2009, and April 30, 2011.
The study was reviewed and approved by the institutional review board (IRB) at AMC Nishi-Umeda Clinic and IRB/ethics committees at other study sites, and conducted in compliance with the ethical principles of the Declaration of Helsinki (1964, revised in 2008) and Ethical Guidelines for Medical Research in Humans. All patients were well informed of the study content and provided written consent for participation before enrollment. This study was registered at the University Hospital Medical Information Network-Clinical Trials Registry (study ID: UMIN000003481).
Inclusion and exclusion criteria
Study subjects had to meet all of the following criteria to be included in the study: (1) Japanese women aged ≥ 55 years, (2) patients diagnosed as having osteoporosis, (3) patients who started osteoporosis treatment (weekly bisphosphonate) in the last 30 days, and (4) patients who can adequately complete the patient questionnaire. The following patients were excluded: (1) patients who had received any bisphosphonate treatment within the last 6 months before the initiation of weekly bisphosphonate, (2) patients receiving bisphosphonate concomitantly with teriparatide, and (3) patients already participating in other osteoporosis-related clinical trials at the time of enrollment.
Study assessments
During a 2-year observation period starting from enrollment, assessments were performed at baseline and 3, 6, 12, and 24 months after enrollment. Data were collected from patients’ medical records and questionnaires completed by patients.
Data collected from medical records included baseline characteristics, such as age, body height/weight, date of diagnosis, comorbidities, antiosteoporotics used, history of fractures, and ability to walk. The previous fractures within the year before enrollment included all fractures, such as hip, spine, and distal radius fractures. For postbaseline assessments, the records were examined for new fractures, antiosteoporotics used, concomitant treatments, and treatment compliance. Incidental clinical vertebral fractures were defined on the basis of radiographic findings, and other incidental clinical fractures were also assessed. Among the comorbidities, diagnosis of spondylosis deformans was based on radiographic examination, with findings such as osteophyte formation, disc space narrowing, or spondylolisthesis. Osteoarthritis involved all joints; however, the knee joints were the most affected, and the diagnosis was determined according to the medical history as well as the interview of patients. Ability to walk was evaluated based on physical examination and the interview of patients.
A questionnaire survey was conducted with the JOQOL and EQ-5D for QOL evaluation at each assessment point. The JOQOL total score was converted to a scale ranging from 0 to 100. Pain was assessed according to the McGill Pain Questionnaire (MPQ) and visual analogue scale (VAS) from 0 to 100 mm (0: no pain, 100: greatest pain imaginable) for the first 6 months after enrollment, and then compared with the results of pain assessment with the JOQOL and EQ-5D.
Discontinuation of study participation
Patients were discontinued from study participation if they (1) were lost to follow-up, (2) withdrew consent, (3) discontinued treatment with once-weekly bisphosphonates, or (4) dropped from the study by the investigators.
Statistical analysis
All patients who completed the 2-year observation period and returned all questionnaires completed at each assessment point were included in the analysis. For the assessment of QOL and pain, data from all assessment points were subjected to multigroup comparison with repeated-measures analysis of variance, and significant differences (p < 0.05) were further examined with Dunnet’s test for changes from baseline to each assessment point. The incidence of fractures was analyzed in the entire population and according to history of fractures within the year before enrollment, using the Chi-square test. For the identification of factors contributing to QOL changes, multiple regression analysis was performed including changes in QOL scores (JOQOL and EQ-5D) from baseline to 24 months and the baseline patient characteristics as explanatory variables, which included the presence or absence of fracture history within the year before enrollment, spondylosis deformans, diabetes, hypertension, heart failure, osteoarthritis, rheumatoid arthritis, use of non-steroidal anti-inflammatory drugs, use of activated vitamin D3, and age and body mass index (BMI), with the presence and absence of each variable entered as “2: yes” and “1: no”, respectively. All statistical analyses were performed with SAS software version 9.3 (SAS Inc., Cary, NC, USA). Unless otherwise specified, all continuous variables were described as mean ± standard deviation, with a two-tailed significance level of 5% (p < 0.05).
Results
Patients
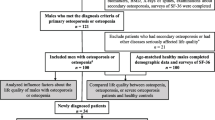
Evaluable population
A total of 6003 female patients with osteoporosis were enrolled from November 1, 2009, to April 30, 2011. After excluding 356 patients who did not return the questionnaire by the time of enrollment and 33 patients who did not meet the inclusion criteria, the study was initiated with 5614 patients. Because an increasing number of patients were withdrawn owing to loss to follow-up or other reasons as the study progressed, the number of patients with returned questionnaires decreased over time (4428 at 3 months, 3897 at 6 months, 3365 at 12 months, and 2741 at 24 months), leaving 2650 patients who returned all questionnaires during the 2-year period and were included in the evaluable population.
Baseline patient characteristics
The evaluable female osteoporotic patients (N = 2650) had a mean age of 73.8 ± 8.3 years (55–100 years), mean body weight 49.4 ± 8.3 kg (25–85 kg), mean height 149.0 ± 6.6 cm (114–174 cm), and mean BMI 22.2 ± 3.5 kg/m2, with 22.7% of them requiring help with walking (including 17.2% able to walk outdoors with partial assistance, 1.2% able to walk independently only indoors, 1.8% only able to walk indoors while holding on to something, and 2.6% unable to walk). Comorbidities were reported in 79.6% of patients, including 66.9% with internal medicine–related diseases (e.g., hypertension in 49.3%, diabetes in 9.1%), 6.0% with neurological diseases (e.g., stroke in 3.5%, Parkinson’s disease in 0.7%), and 36.3% with locomotor diseases (e.g., osteoarthritis in 29.7%, rheumatoid arthritis in 3.5%). Other osteoporosis-related prescription drugs concomitantly used with bisphosphonates included raloxifene hydrochloride in 70 (2.6%) patients, activated vitamin D3 in 770 (29.1%) patients, and vitamin K2 in 41 (1.5%) patients.
Efficacy evaluation
Fracture rate
The incidence of fractures within the year before enrollment was evaluated in 2557 patients with relevant data available in the questionnaires. Fractures within the year before enrollment were reported in 422 (16.5%) patients, whereas the incidence significantly decreased as treatment progressed to 132 (5.2%) and 101 (3.9%) patients at 1 and 2 years after enrollment, respectively (p = 0.042). We then evaluated the incidence of fractures after enrollment according to history of fractures within the year before enrollment. Of 422 patients with pre-enrollment history of fractures, 38 (9.0%) and 26 (6.2%) had fractures at first and second years after enrollment, respectively. In the remaining 2135 patients without pre-enrollment fracture history, fractures occurred in 94 (4.4%) and 75 (3.5%) at the first and second years after enrollment, respectively. Thus, patients with pre-enrollment fracture history had significantly higher incidence of fractures at the first (p < 0.001) and the second (p = 0.001) years after enrollment. In both groups, the fracture rate at the second year after enrollment was lower than that at the first year after enrollment, although there was no significant difference.
QOL assessment
JOQOL assessment
A significant improvement in the JOQOL total score was observed from 3 months after enrollment onward and maintained until 24 months after enrollment (Fig. 1). Among the JOQOL domains, a significant improvement was also observed in “pain”, “health perception”, and “posture, figure” from 3 months onward and maintained until 24 months. Whereas the improvement in the total score achieved at 6 months was maintained constantly until the end of the 2-year observation period, the scores for the “pain”, and “health perception” domains showed a tendency to increase continuously throughout the observation period.
Time-dependent changes in Japanese Osteoporosis Quality of Life Questionnaire (JOQOL) score induced by bisphosphonate treatment in Japanese osteoporotic women (N = 2650). Mean JOQOL score at baseline (white bar), month (M) 3 (black bar), M6 (dark gray bar), M12 (gray bar), and M24 (light gray bar). Error bars show standard deviation. #p < 0.0001: derived with repeated-measures analysis of variance among JOQOL scores at baseline, M3, M6, M12, and M24. *p < 0.0001: derived with Dunnet’s test among JOQOL scores at baseline and M3 or M6 or M12 or M24
EQ-5D assessment
A significant increase in the EQ-5D score was also observed from 3 months after enrollment onward and maintained until 24 months after enrollment (Fig. 2). In the EQ-5D domains, the scores for all domains were significantly improved between 3 and 24 months after enrollment (p < 0.0001, Dunnet’s test).
Time-dependent changes in Euro Quality of Life 5 Dimension (EQ-5D) score induced by bisphosphonate treatment in Japanese osteoporotic women (N = 2598). Mean score of EQ-5D at baseline, month (M) 3, M6, M12, and M24. Error bars show standard deviation. Repeated-measures analysis of variance among EQ-5D scores at baseline, M3, M6, M12, and M24 derived p < 0.0001. *p < 0.0001: derived with Dunnet’s test among EQ-5D scores at baseline and M3 or M6 or M12 or M24
Changes in QOL with or without factors contributing to QOL change
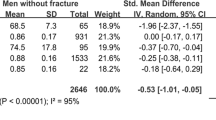
Analysis of factors contributing to QOL change
The following factors were identified as being significantly correlated to change in QOL in multiple regression analysis (p < 0.05), and thus defined as factors contributing to QOL change: “fractures within the year before enrollment”, “presence of spondylosis deformans”, “presence of osteoarthritis”, “use of activated vitamin D3”, and “age” based on the JOQOL, and “presence of spondylosis deformans”, “use of activated vitamin D3”, and “age” based on the EQ-5D (Table 1).
Analysis of improvement in QOL in relation to factors contributing to QOL change
The above results suggested that all factors identified as contributing to QOL change, except for “use of activated vitamin D3”, were associated with decreased QOL. We then evaluated the effects of those factors on changes in QOL scores.
The analysis of QOL based on the JOQOL total score (Fig. 3) showed decreased baseline QOL in patients with contributing factors “advanced age” (≥ 75 years) and “locomotor diseases” (fractures within the year before enrollment, spondylosis deformans, or osteoarthritis). In all patient groups except for those with advanced age, QOL was significantly improved by continuous treatment. At the end of the 2-year observation period, the difference in QOL scores between patients with and without contributing factors was smaller than that at baseline. Although no significant improvement in QOL was observed in patients with advanced age, their QOL scores did not decline and were maintained at levels similar to baseline, despite being older by 2 years at the end of the observation period.
Analysis on the effects of age, prevalent fracture influence, and musculoskeletal disorders on the total score of the Japanese Osteoporosis Quality of Life Questionnaire (JOQOL). a Mean total score of JOQOL at baseline, month (M) 3, M6, M12, and M24 according to age (≥ 75 years: circle, < 75 years: square). b Mean total score of JOQOL at baseline, M3, M6, M12, and M24 according to fracture (+, circle; −, square). c Mean total score of JOQOL at baseline, M3, M6, M12, and M24 according to spondylosis deformans (+, circle; −, square). d Mean total score of JOQOL at baseline, M3, M6, M12, and M24 according to osteoarthritis (+, circle; −, square). Error bars show standard deviation. Repeated-measures analysis of variance among JOQOL scores at baseline, M3, M6, M12, and M24 derived p < 0.0001. *p < 0.0001: derived with Dunnet’s test among JOQOL scores at baseline and M3 or M6 or M12 or M24
The EQ-5D-based analysis (Fig. 4) also showed decreased QOL at baseline in patients with advanced age (≥ 75 years) or osteoarthritis; however, in those with osteoarthritis, a significant improvement in QOL was observed as treatment progressed, and the difference between those with and without this factor at the end of the observation period was smaller than that at baseline. In patients with advanced age, QOL was maintained by continuous treatment.
Analysis on the effects of age and osteoarthritis on Euro Quality of Life 5 Dimension (EQ-5D) score. a Mean score of EQ-5D at baseline, month (M) 3, M6, M12, and M24 according to age (≥ 75 years: circle, < 75 years: square). b Mean score of EQ-5D at baseline, M3, M6, M12, and M24 according to osteoarthritis (+, circle; −, square). Error bars show standard deviation. Repeated-measures analysis of variance among EQ-5D scores at baseline, M3, M6, M12, and M24 derived p < 0.0001. *p < 0.0001: derived with Dunnet’s test among EQ-5D scores at baseline and M3 or M6 or M12 or M24
Pain assessment
In pain assessment with VAS, a significant reduction in pain was observed at 3 (37.2 ± 24.6) and 6 (34.2 ± 23.9) months after enrollment, as compared to baseline (40.4 ± 26.6; p = 0.0000, Dunnet’s test). The MPQ total score was also significantly decreased, indicating a significant reduction in pain, at 3 (7.52 ± 10.22) and 6 (6.61 ± 8.93) months after enrollment, as compared to baseline (8.83 ± 12.43; p = 0.0000, Dunnet’s test). Both scores were decreased insignificantly at 3 months and significantly at 6 months after enrollment (p = 0.0000, Dunnet’s test). The significant improvement in pain achieved by 6 months based on the VAS and MPQ was consistent with the improvement in the scores for the pain-related domains of the JOQOL and EQ-5D.
Discussion
There are an increasing number of osteoporotic patients who need interventions to prevent fractures with the rapid aging of the population in Japan, although the estimated percentage of patients who receive such interventions remains low. Even in those with fragility fracture, only 19–37% receive such interventions [5, 6]. The treatment continuation rate is also low. In a study on long-term administration of bisphosphonates, the 1-year compliance rate was reported to be about 40% [7]. Despite the urgent need for measures to prevent fractures among the elderly, the low rate of receiving or continuing treatment for osteoporosis is considered a major issue. We, therefore, considered it meaningful to follow the long-term outcome of treatment for osteoporotic patients with different backgrounds who were treated at primary care centers, and thereby provide data that can help reduce dropouts from treatment. In Japan, different medical institutions use different methods and sites of BMD measurement. In addition to BMD, which can be determined clinically, QOL is also considered an important parameter for evaluating response to treatment for osteoporosis [3]. However, as osteoporotic patients are less likely to perceive treatment effects owing to lack of subjective symptoms, they tend to discontinue treatment on their own will. Therefore, to obtain data that can help to promote treatment continuation, it is necessary to evaluate treatment response based on patient-reported changes in QOL. We, therefore, conducted a multicenter prospective observational study using QOL measurement tools that include pain assessment, in patients receiving treatment for osteoporosis in Japan.
The study was initiated with 5614 Japanese middle-aged to elderly women with osteoporosis treated with once-weekly bisphosphonates. After the 2-year observation period, 2741 (48.4%) patients remained on treatment, giving a low treatment continuation rate comparable to that reported in the previous studies. The fracture rate significantly decreased over time, being 5.2 and 3.9% at first and second years after enrollment, respectively, as compared to that within the year before enrollment (16.5%). Decreasing fracture rate was observed regardless of history of fractures within the year before enrollment, suggesting the efficacy of once-weekly treatment with bisphosphonates for preventing fractures even in patients at a high risk for fractures.
The analysis of changes in QOL in patients treated continuously with once-weekly bisphosphonates showed significant improvements in the JOQOL total score and EQ-5D score from 3 months after enrollment onward and maintained until 24 months after enrollment. In the analysis by domain, all domains of the EQ-5D were significantly improved, whereas only “pain”, “health perception”, and “posture, figure” were significantly improved among the eight domains of the JOQOL. In a previous study of 1-year treatment with once-weekly bisphosphonates, the score for the “pain” domain of a disease-specific QOL questionnaire was significantly improved in patients who remained on treatment as compared with those who discontinued treatment [7], suggesting that the patients’ perception of treatment effects, such as improvement in pain, contributes to treatment continuation. The treatment of osteoporosis lasts for a long time. Although increased risks of medication-related osteonecrosis of the jaw or atypical femoral fractures caused by long-term bisphosphonate treatment have been observed, their incidences are very low, and the benefits of continuing therapy probably far outweigh the risk of harm in patients with a high fracture risk [8]. To improve the treatment continuation rate, it is important to confirm treatment-related improvement in QOL from baseline through periodic QOL assessments and consult with patients based on these data.
We selected factors for explanatory variables that are commonly observed in the elderly and possibly affect the fracture risk or QOL. Fracture history, diabetes, rheumatoid arthritis, use of active vitamin D3, age, and BMI are independent risk factors for fragility fractures [9, 10]. Spondylosis deformans and osteoarthritis comprise locomotive syndrome, which could deteriorate the QOL. Hypertension and heart failure are also common in the elderly and possibly affect the QOL, and the use of non-steroidal anti-inflammatory drugs is closely related to bodily pain and QOL. As a result, the present study identified “age”, “fractures within the year before enrollment”, “presence of spondylosis deformans”, “presence of osteoarthritis”, and “use of activated vitamin D3” as factors contributing to QOL change, consistent with a previous study that also identified “age” and “presence of osteoarthritis” as contributing factors to QOL changes in Japanese female osteoporotic patients treated with risedronate for 12 weeks [11]. The present study also identified “use of activated vitamin D3” as contributing to improved QOL. In fact, it has been reported that 23.7% of elderly Japanese osteoporotic women with a high fracture risk had vitamin D deficiency (serum 25(OH)D < 20 ng/mL), and these vitamin D–deficient patients had decreased QOL [12] and showed reduced response to bisphosphonate treatment [13]. Elderly persons are known to be at a risk of developing vitamin D deficiency owing to their reduced capacity to synthesize vitamin D in the skin, reduced exposure to sunlight, and reduced dietary intake of the vitamin [14]. Although 25(OH)D level was not measured in this study, it is speculated that activated vitamin D3 improved the QOL and/or enhanced the clinical effect of bisphosphonate [10, 12]. Use of activated vitamin D3 is, therefore, preferred for elderly persons who do not show the anticipated response to bisphosphonate treatment.
Patients with locomotor diseases (history of fractures within the year before enrollment, spondylosis deformans, or osteoarthritis), a factor identified as contributing to QOL changes, had baseline QOL scores substantially lower than those in patients without locomotor diseases. Nevertheless, with continuous treatment with once-weekly bisphosphonates, these patients showed significantly improved QOL, with the difference in QOL scores between those with and without locomotor diseases at 24 months after enrollment being smaller than that at baseline. Thus, osteoporosis patients should also be fully informed that continuous treatment with once-weekly bisphosphonates can lead to a significant improvement in QOL regardless of other concomitant locomotor diseases, to encourage them to remain on treatment.
Elderly patients (age ≥ 75 years) showed no significant improvement in QOL with continuous treatment with once-weekly bisphosphonates. Age-related steep decline in EQ-5D score has been reported in persons aged ≥ 70 years [15]. In the present study, continuous treatment with once-weekly bisphosphonates might have prevented the decrease in QOL that could have been caused by the 2-year aging over the course of the study. Similarly, no significant improvement was observed in the scores for the “self-care”, “housework”, “transfer”, “leisure and social activities”, and “falls and mental factors” domains of the JOQOL. Given that the scores for these domains are known to decrease with increasing age, the result indicates that QOL was maintained at the baseline level by the continuous treatment with once-weekly bisphosphonates.
The limitations of this study include a low questionnaire recovery rate: only 47.2% of the enrolled patients returned all questionnaires during the 2-year period. This is because the present study was based on real-world data collection. Second, owing to different procedures for BMD measurement used in different medical institutions in Japan, we were unable to collect BMD data measured based on a standardized criterion in this observational study; thus, we were unable to investigate the association between improvement in QOL and change in BMD. Third, incidental vertebral fractures were defined based on radiographic findings and the diagnosis was determined based on clinical judgment, which might lead to some bias. However, in this study, the participating doctors at each hospital are mainly (79%) specialists in the bone and joint fields, and the large number of patients attenuates the possible bias with the diagnosis and definition. Nevertheless, one of the strengths of this study is that it enrolled about 6000 patients from multiple centers across Japan, and collected and analyzed primary data derived from daily clinical practice. With an increasing importance of data derived from clinical practice, extensive studies are being conducted outside Japan using secondary data from databases and electrical medical records. As these secondary data–based studies do not provide patient outcome data, such as patients’ QOL reflecting response to treatment, the results of the present analysis are of great significance.
In conclusion, a significant improvement in QOL was observed from 3 months of treatment with once-weekly bisphosphonates onward and maintained throughout the 2-year observation period in Japanese middle-aged to elderly female patients with osteoporosis. Despite concerns over reduced improvement in QOL in elderly patients and patients with locomotor diseases, our data suggest that continuous bisphosphonate treatment will lead to improved QOL even in those patient populations. The concomitant use of activated vitamin D3 may also facilitate further improvement in QOL.
References
Yoshimura N, Muraki N, Oka H, Kawaguchi H, Nakamura K, Akune T (2010) Cohort profile: research on Osteoarthritis/Osteoporosis Against Disability study. Int J Epidemiol 39:988–995
Yoshimura N, Muraki S, Oka H, Mabuchi A, En-Yo Y, Yoshida M, Saika A, Yoshida H, Suzuki T, Yamamoto S, Ishibashi H, Kawaguchi H, Nakamura K, Akune T (2009) Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: the research on osteoarthritis/osteoporosis against disability study. J Bone Miner Metab 27:620–628
Committee for the Development of Guidelines for Prevention and Treatment of Osteoporosis (Japan Osteoporosis Society, The Japanese Society for Bone and Mineral Research and Japan Osteoporosis Foundation) (2015) Guidelines for prevention and treatment of osteoporosis (in Japanese). Life Science Publishing Co., Ltd., Tokyo
Kumamoto K, Nakamura T, Suzuki T, Gorai I, Fujinawa O, Ohta H, Shiraki M, Yoh K, Fujiwara S, Endo N, Matsumoto T (2010) Validation of the Japanese Osteoporosis Quality of Life Questionnaire. J Bone Miner Metab 28:1–7
Hagino H, Sawaguchi T, Endo N, Ito Y, Nakano T, Watanabe Y (2012) The risk of a second hip fracture in patients after their first hip fracture. Calcif Tissue Int 90:14–21
Tsukutani Y, Hagino H, Ito Y, Nagashima H (2015) Epidemiology of fragility fractures in Sakaiminato, Japan: incidence, secular trends, and prognosis. Osteoporos Int 26:2249–2255
Kamatari M, Koto S, Ozawa N, Urao C, Suzuki Y, Akasaka E, Yanagimoto K, Sakota K (2007) Factors affecting long-term compliance of osteoporotic patients with bisphosphonate treatment and QOL assessment in actual practice: alendronate and risedronate. J Bone Miner Metab 25:302–309
Adler RA, El-Hajj Fuleihan G, Bauer DC, Camacho PM, Clarke BL, Clines GA, Compston JE, Drake MT, Edwards BJ, Favus MJ, Greenspan SL, McKinney R Jr, Pignolo RJ, Sellmeyer DE (2016) Managing osteoporosis in patients on long-term bisphosphonate treatment: report of a Task Force of the American Society for Bone and Mineral Research. J Bone Miner Res 31:16–35
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397. https://doi.org/10.1007/s00198-007-0543-5
Orimo H, Nakamura T, Fukunaga M, Ohta H, Hosoi T, Uemura Y, Kuroda T, Miyakawa N, Ohashi Y, Shiraki M, A-TOP (Adequate Treatment of Osteoporosis) Research Group (2011) Effects of alendronate plus alfacalcidol in osteoporosis patients with a high risk of fracture: the Japanese Osteoporosis Intervention Trial (JOINT)—02. Curr Med Res Opin 27:1273–1284
Nakamura T, Osawa M, Itoh M, Yamaguchi H, Iinuma N, Hayakawa Y, Suzuki H, Kamisaki T, Iwayama S, Nishikawa M (2012) The effect of risedronate (17.5 mg/week) treatment on quality of life in Japanese women with osteoporosis: a prospective observational study. J Bone Miner Metab 30:715–721
Ohta H, Uemura Y, Nakamura T, Fukunaga M, Ohashi Y, Hosoi T, Mori S, Sugimoto T, Itoi E, Orimo H, Shiraki M, Adequate Treatment of Osteoporosis (A-TOP) Research Group (2014) Serum 25-hydroxyvitamin D level as an independent determinant of quality of life in osteoporosis with a high risk for fracture. Clin Ther 36:225–235
Carmel AS, Shieh A, Bang H, Bockman RS (2012) The 25(OH)D level needed to maintain a favorable bisphosphonate response is ≥ 33 ng/ml. Osteoporos Int 23:2479–2487
Institute of Medicine, Food and Nutrition Board (2010) Dietary reference intakes for calcium and vitamin D. National Academy Press, Washington, DC
Fujikawa A, Suzue T, Jitsunari F, Hirao T (2011) Evaluation of health-related quality of life using EQ-5D in Takamatsu, Japan. Environ Health Prev Med 16:25–35
Acknowledgements
The authors thank all investigators who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was funded by the Japan Association of Health Service.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Hagino, H., Soen, S., Sugimoto, T. et al. Changes in quality of life in patients with postmenopausal osteoporosis receiving weekly bisphosphonate treatment: a 2-year multicenter study in Japan. J Bone Miner Metab 37, 273–281 (2019). https://doi.org/10.1007/s00774-018-0914-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-018-0914-3