Abstract
We have already established that a short cationic peptide (CM11) has high antimicrobial activity against a number of bacterial pathogens. Considering the untreatable problem of burn infections caused by Pseudomonas aeruginosa and Acinetobacter baumannii, this study evaluated and compared antibacterial effects of the CM11 peptide and 1% silver-doped bioactive glass (AgBG) against extensively drug-resistant strains of these bacteria which were isolated from burn patients. Accordingly, the bacteria were isolated from burn patients and their antibiotic resistance patterns and mechanisms were fully determined. The isolated bacterial from patients were resistant to almost all commonly used antibiotics and silver treatment. The isolates acquired their resistance through inactivation of their porin, the overexpression of efflux pump, and beta-lactamase. CM11 peptide and 1% AgBG had minimum inhibitory concentration (MIC) of ≥ 16 μg ml−1 and ≥ 4 mg ml−1 for clinical isolates, respectively. The minimum bactericidal concentration (MBC) of peptide and 1% AgBG for resistant bacteria was ≥ 32 μg ml−1 and ≥ 4 mg ml−1, respectively. Among the clinical isolates, two P. aeruginosa isolates and one A. baumannii isolate were resistant to 1% AgBG disk. The CM11 peptide also showed high biocompatibility in vivo and no cytotoxicity against fibroblasts and adipose-derived mesenchymal stem cells in concentrations ≤ 64 μg ml−1 and ≤ 32 μg ml−1, respectively, while the safe concentration of 1% AgBG for these cells was ≤ 16 μg ml−1. In conclusion, these findings indicated that the 1% silver is not safe and effective for treatment of such infections. The data suggest that CM11 peptide therapy is a reliable and safe strategy that can be used for the treatment of burn infections caused by antimicrobial-resistant isolates. The next stage of the study will be a multicenter clinical trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post-burn infections are considered as a major concern in burn centers. During the last years, Pseudomonas aeruginosa and Acinetobacter baumannii have been responsible for the most important hospital-borne infections and an emerging cause of antimicrobial treatment failure (Leseva et al. 2013; Aghamollaei et al. 2015; Ellis et al. 2015). These bacteria show an outstanding capacity to develop resistance against common antibiotics such as carbapenems, β-lactams, tetracyclines, fluoroquinolones, and aminoglycosides through a wide variety of mechanisms. Therefore, demand to new and effective therapies is inevitable (Bonomo and Szabo 2006). In the last years, we encountered with an improved mortality in patients with burn infections in our burn hospital (Motahari Burn Center in Tehran). These infections were caused by the resistant bacteria, which were extensively resistant to almost all commonly used antibiotics and even high concentrations of silver and fluoride (Gholipourmalekabadi et al. 2016a). Therefore, the recent researches are focusing on the development of novel antibacterial agent for protection against such resistant bacteria. Among the antibacterial materials, some metallic cations such as silver and fluoride, and antimicrobial peptides (AMPs) showed promising results (Bakal et al. 2017; Chung and Khanum 2017; Gholipourmalekabadi et al. 2016a). Silver and silver-containing wound dressings are already used in protection of burn wounds against infections (Silver et al. 2006; Lachine et al. 2016). Antibacterial activity and cytotoxicity of silver components are concentration dependent (Gholipourmalekabadi et al. 2016a; Nezafati et al. 2012).
AMPs are one of the most promising compounds used as novel antimicrobial and therapeutic agents. AMPs are important members of the host defense system in eukaryotes with a broad ability to kill microorganisms including viruses, bacteria, protozoa, and fungi with different mechanisms such as disrupting the structure or the function of microbial cell membranes or interaction with ATP and directly inhibiting the action of certain ATP-dependent enzymes especially by cationic peptides (Amani et al. 2015). The cationic antibacterial peptides (containing 12–50 amino acids) can adopt amphipathic conformations with spatially separated hydrophobic and charged regions. The main advantage of such peptides, over other defensive molecules (i.e., antibiotics), is broad-spectrum antibacterial activity with rapid onset of killing and low levels of induced resistance compared with conventional antibiotics (Amani et al. 2015; Kosikowska and Lesner 2016). Accordingly, the CM11 peptide is one of cationic antimicrobial peptides that contains 11-residue sequence (WKLFKKILKVL-NH2) derived from cecropin A (residues 2–8) and from melittin residues 6–9 that have been designed and produced to improve the properties of parent peptides. Our recent studies showed high antimicrobial effects of CM11 against several human pathogenic bacteria (Moghaddam et al. 2012; Moghaddam et al. 2014; Amani et al. 2015; Azad et al. 2017).
Despite some promising results, the biocompatibility and non-cytotoxicity as well as antibacterial activity of silver and AMPs have still remained challenging (Gholipourmalekabadi et al. 2015b; Gholipourmalekabadi et al. 2016a; Albers et al. 2013; AshaRani et al. 2008; Pelillo et al. 2014). Considering the importance of burn infections caused by P. aeruginosa and A. baumannii, in this study we evaluated and compared antibacterial effects the CM11 peptide and 1% silver-doped bioactive glass against extensively drug-resistant (XDR) strains of P. aeruginosa and A. baumannii, which were isolated from burn patients. In this regard, we isolate XDR bacteria isolates from burn patients hospitalized at our burn center during the year 2016 and fully determine their antibiotic resistance patterns and also resistance mechanisms. Then, the effectiveness and safety of cationic antimicrobial peptide as a possible and reliable treatment strategy, versus 1% silver-doped bioactive glass (AgBG) against such XDR bacteria were evaluated both in vitro and in vivo.
Materials and methods
Bacterial identification, antibiotic susceptibility tests and resistance mechanisms
Seven P. aeruginosa and four A. baumannii were isolated from the wound exudate of burn patients admitted to the Burn Unit of Shahid Motahari Hospital in Tehran, Iran (2016). Nine bacterial standard strains were also included in the study. The specimens were identified using conventional biochemical tests (Hakemi Vala et al. 2014). All the bacteria isolated from burn patients were subjected to antimicrobial susceptibility testing against commonly used antibiotics (SM-Table 1) using disk diffusion method and minimum inhibitory concentration (MIC) according to clinical and laboratory standards institute (CLSI) guidelines (2007). E. coli ATCC 25922 and P. aeruginosa ATCC 27853 served as control strains.
The antibiotic resistance mechanisms studied in the current investigation were as follows: porin and efflux pump-associated resistances for P. aeruginosa, and beta-lactamase-associated resistance for both P. aeruginosa and A. baumannii (Bonomo and Szabo 2006). The clinical isolates were screened for metallo-beta-lactamase (MBL) production by combined disk diffusion test (CDDT) using imipenem (10 μg) and meropenem (10 μg) disks (Mast Group, Merseyside, UK) alone and in combination with ethylenediaminetetraacetic acid (EDTA) (Sigma).
Also, PCR was performed to detect the beta-lactamase genes such as blaIMP, blaVIM, and blaNDM in P. aeruginosa and blaIMP, blaVIM, blaNDM, blaOXA-23-like, blaOXA-51-like, blaOXA-24-like and blaOXA-58-like in A. baumannii. PCR condition and the primers sequences are shown in SM-Table 2 and SM-Table 3, respectively. Another resistance mechanism in P. aeruginosa clinical isolates is through efflux pump-associated resistance that was investigated by carbonyl cyanide m-chlorophenylhydrazone (CCCP) (Sigma-Aldrich, ST. Louis, MO, USA) (Ardebili et al. 2014) and the expression level of mexD and mexA efflux pumps was determined by real-time PCR (RT-PCR) (Rotor-Gene 6000, Corbett Research, Germany) according to previously described protocols (Llanes et al. 2004). The list of the primers used in RT-PCR, their sequence and relevant product size are listed in SM-Table 4.
Porins are from other resistance mechanisms in P. aeruginosa clinical isolates. Porin gene from the clinical isolates was amplified by conventional PCR using oprD-specific primers (oprDF1 and oprDR1). The sequence of oprD gene was aligned and compared to that in P. aeruginosa PAO1 using multiple sequence alignment (http://multalin.toulouse.inra.fr/multalin/).
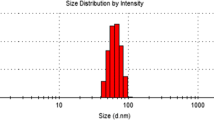
Preparation and characterization of CM11 peptide and 1% AgBG
Cationic antimicrobial peptide (CM11) was synthesized by a solid-phase synthesis method using p-methylbenzhydrylamine resin (Badosa et al. 2007; Moghaddam et al. 2014). The synthesized peptide was purified by reversed-phase semi-preparative HPLC on the C18 tracer column. 1% AgBG bioactive glass was synthesized by the sol–gel technique based on a [1 − (x + y)](58%SiO2–33%P2O5–9%CaO)–xCaF2–yAg2O system (Gholipourmalekabadi et al. 2016a).
Cellular responses to CM11 peptide and 1% AgBG
The effects of the various concentrations of peptide on cell viability and cytotoxicity of fibroblast L-929 cells and human adipose tissue-derived mesenchymal stem cells (hAT-MSCs) were studied by MTT, LDH-specific activity assay and 4′-6-diamidino-2-phenylindole (DAPI) staining.
Cell isolation and culture
Fibroblast L-929 cells were purchased from Pasteur Institute of Iran and cultured in Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 10% FBS, 1% pen/strep, nystatin and amphotericin B, 2 mM Glutamax and 1 mM l-glutamine (all from Gibco, Carlsbad, CA, USA) and maintained in a humidified atmosphere of 5% CO2 at 37 °C. The mesenchymal stem cells were isolated from human adipose tissue obtained from patients undergoing elective liposuction surgery (Gholipourmalekabadi et al. 2016b).
Characterization of hAT-MSCs
The hAT-MSCs were identified by their fibroblast-like morphology and phenotype characteristics by light microscope and flow cytometry, respectively. The CD markers used for phenotypic characterizations of the cells were as Sca1, CD44, CD90 and CD105, CD11b, CD33, CD34 and CD45 (all obtained from eBioscience, Hatfield, Ireland, UK), selected based on the International Society for Cellular Therapy (ISCT) criteria (Dominici et al. 2006).
Cell viability, cytotoxicity and density
The effects of various concentrations (4 µg ml−1, 8 µg ml−1, 16 µg ml−1, 32 µg ml−1, 64 µg ml−1, 1 mg ml−1, 2 mg ml−1, 4 mg ml−1) of CM11 peptide and 1% AgBG on the cell viability and cytotoxicity were determined by MTT and LDH assays, respectively. For this purpose, the cells were exposed to peptide and AgBG for 24, 48 and 72 h. MTT and LDH assays were carried out as described earlier (Gholipourmalekabadi et al. 2015a; Rostami et al. 2015). The density of the cells after treatment with peptide and 1% AgBG was determined by staining the cells with DAPI. The average number of the cells per high-power microscope field (HPF, n = 10; ×40 objective) was determined and compared with control.
Bacterial susceptibility to CM11 peptide and 1% AgBG
MIC and MBC assays
The MIC of peptide and 1% AgBG for all clinical isolates and bacterial standard strains was determined by microdilution broth method, according to clinical and laboratory standards institute (CLSI) guidelines (2007). Serial twofold dilutions for peptide and 1% AgBG (4 µg ml−1, 8 µg ml−1, 16 µg ml−1, 32 µg ml−1, 64 µg ml−1, 1 mg ml−1, 2 mg ml−1 and 4 mg ml−1) were prepared in cation-adjusted Mueller–Hinton broth (CAMHB). MBC was defined as the lowest concentration of peptide to have at least 99.9% killing of the initial inoculum.
In vivo biocompatibility of CM11 peptide and 1% AgBG
The biocompatibility of the CM11 peptide and 1% AgBG was assessed at 3 and 7 days after subcutaneously injection of various concentrations of peptide and 1% AgBG (ranging from 4 µg ml−1 to 4 mg ml−1) in BALB/c mice (Rostami et al. 2015). The average number of host inflammatory cells infiltrated into injected site was recorded and compared between the experimental groups. The average number of the cells of 10 high-powered field (HPF) was reported.
Results and discussion
The methodology and results of the current study are illustrated in Fig. 1.
Schematic of the current study. The bacteria were isolated from exudate of patients with burn wounds and characterized. Extensively drug-resistant (XDR) bacteria as well as standard strain bacteria were subjected to this study. Cationic antimicrobial peptide (CM11) and 1% silver-doped bioactive glass (1% AgBG) were synthesized. Antibacterial activity, in vitro and in vivo biocompatibility and safety of peptide and 1% AgBG were evaluated and compared between experimental groups
Bacterial identification, antibiotic susceptibility tests and resistance mechanisms
Seven antibiotic-resistant P. aeruginosa and four antibiotic-resistant A. baumannii strains were isolated from wound exudate of the burn patients. Antibiogram results revealed that all eleven isolates were extensively drug resistant (XDR), MBL producing and sensitive to Colistin (Fig. 2a). The results also showed that three clinical isolates (two P. aeruginosa and one A. baumannii) were resistant to 1% AgBG disk. The results obtained from this work reveal that silver may not be able to protect burn patients against the MDR bacteria and should be replaced with another efficient antibacterial agent.
Bacterial resistance tests. a Antibiogram of commonly used antibiotics and 1% AgBG for P. aeruginosa and A. baumannii. All P. aeruginosa clinical isolates were sensitive to Colistin (Col). All clinical isolates were resistant to 1% AgBG. b Resistance mediated by beta-lactamase. All isolates were positive for MBL (CDDT test). (i) IMI 10 µg disk; (ii) IMI10 µg + EDTA 10 µg disk; (iii) MEM disk; (iv) MEM 10 µg + EDTA 10 µg disk. PCR products of blaIMP genes in P. aeruginosa isolates visualized in gel electrophoresis. Lane M: 100 bp DNA size marker; Lane P: positive control; Lane N: negative control; Lane 1–3: blaIMP positive P. aeruginosa isolates. Multiplex PCR products of blaOXA-24-like, blaOXA-23-like, and blaOXA-51-like genes in A. baumannii isolates visualized in gel electrophoresis. Lane M: 100 bp DNA size marker; Lane P: positive control; Lane N: negative control; Lane 1–3: blaOXA-23-like, blaOXA-51-like and blaOXA-24-like genes positive isolates. c΄ Relative expression of mexD and mexA in P. aeruginosa clinical isolates. c΄΄ Gel electrophoresis analysis of the RT-PCR products. Lane M: DNA size marker; Lane P: positive control; Lane N: negative control; Lane 1–7: mexD-positive isolates. Gel electrophoresis analysis of the RT-PCR products. Lane M: DNA size marker; Lane P: positive control; Lane N: negative control; Lane 1–3: mexA-positive isolates. d PCR products of OprD gene. The PCR products were run on 1.5% agarose gels, the corresponding bands were characterized and their sizes were compared to that in positive sample (P. aeruginosa PAO1). Lane M: GeneRuler 100 bp DNA Ladder (Sinaclon, Iran); Lane N: negative control; Lane 1 and 3: oprD gene-positive isolates: Lane 2 and 4: oprD + IS gene with insertion sequence
The MIC results indicating the resistance of clinical isolates to these antibiotics are shown in Table 1. The seven P. aeruginosa and four A. baumannii isolates were highly resistant to carbapenem, with imipenem and meropenem MICs of ≥ 32 μg/ml. The carbapenem-resistant isolates were also resistant to ciprofloxacin and ceftazidime with MICs of ≥ 64 μg/ml. These findings indicate that carbapenem may be no longer the “gold standard” for the treatment of the infections caused by MDR bacteria isolated from burn patients.
Metallo-β-lactamases are one of the most important factors responsible for increasing prevalence of Gram-negative bacterial resistance. Despite the worldwide rise of metallo-β-lactamases (MBLs), carbapenem resistance mediated by MBLs is common in Iran (Noori et al. 2014). Resistance mediated by MBLs, able to hydrolyze all β-lactams except monobactams, is an emerging problem among P. aeruginosa isolates in many countries of Asia, Europe, Africa, and South America (Fallah et al. 2012). As shown in Fig. 2b (disk diffusion), all P. aeruginosa and A. baumannii isolates were MBL producers.
The presence of β-lactamase genes is shown in SM-Table 5, SM-Table 6 and Fig. 2b. All A. baumannii isolates were positive for blaOXA-23-like, blaOXA-51-like and blaOXA-24-like and negative for blaOXA-58-like β-lactamases (SM-Table 6 and Fig. 2b). All P. aeruginosa and two A. baumannii isolates were positive for blaIMP, while blaVIM and blaNDM genes were not observed in all clinical isolates (SM-Table 5, SM-Table 6).
Carbonyl cyanide m-chlorophenylhydrazone (CCCP) is an efflux pump inhibitor (EPI) that indirectly inhibits efflux pump through disrupting the proton motive force and subsequently facilitating proton transfer across the bacterial membrane (Ikonomidis et al. 2008). According to the CCCP results, MIC value for ciprofloxacin with CCCP showed more than fourfold reduction (in three isolates of A. baumannii and five isolates of P. aeruginosa) and eightfold reduction (in one isolate of A. baumannii and two isolates of P. aeruginosa) in comparison to MIC values of ciprofloxacin without CCCP. These findings indicate that the increased activity of efflux pumps in clinical isolates may be one of the main causes of their resistance to ciprofloxacin.
The relative expression of mexD and mexA efflux pump genes in seven P. aeruginosa isolates was determined by RT-PCR and the results were compared with those in P. aeruginosa PAO1, as control sample (Fig. 2c). The gene expression analysis showed an increased relative expression of mexD (1.3–6.77-fold) and mexA (1.1–54.9-fold) in all P. aeruginosa clinical isolates when compared to those in P. aeruginosa PAO1 (p ≤ 0.05) (Fig. 2c΄and c΄΄), indicating the important role of mexD and mexA in resistance of P. aeruginosa isolated from burn patients against antibiotics.
Insertional inactivation through insertion sequence (IS) elements is one of the most common mechanisms associated with lack of function of OprD (Evans and Segal 2007). According to our results (Fig. 2d), only two isolates showed an increased PCR product size when compared with P. aeruginosa PAO1 (control). According to the data obtained from the multiple sequence alignment analysis of the IS-positive isolates and IS finder database nomenclature (https://www-is.biotoul.fr), these bacteria carry ISPpu21 and ISPa1328 elements in their oprD gene.
Cationic AMP characterization
HPLC and electrospray ionization mass spectrometry were used for purification and to confirm peptide identity, respectively. For HPLC, the active fraction was loaded on C18 tracer column using a linear gradient from 10 to 60% acetonitrile in water with 0.1% TFA over 50 min. The active peak corresponds to the peptide control obtained with > 95% HPLC purity. Also, the molecular mass of peptide was determined to be 1415.85 Da by electrospray ionization mass spectroscopy (SM-Fig. 1A and SM-Fig. 1B).
Cell’s responses to CM11 peptide and 1% AgBG
MSC characterization
The morphology of the cells during the expansion in flask was observed under light microscope (SM-Fig. 2A). The AT-MSCs showed a spindled shape similar to fibroblast morphology. The phonotypic characterization of the isolated cells was performed by flow cytometry. The flow cytometry result is shown in SM-Fig. 2B. 98.5% and 97.9%, 98.4 and 96.5% of the isolated cells were positive for Sca1, CD44, CD90 and CD105, respectively, while the cells were almost negative for CD11b, CD31, CD34 and CD45. These results indicate that more than 95% of the isolated cells were identified as mesenchymal stem cells (Mohammadzadeh et al. 2014).
Stem cell viability and cytotoxicity
The safety of novel antimicrobial agents against human cells is critical for minimizing their side effects. High cytotoxicity of such agents profoundly limits their applications in clinic (Bem et al. 2014; Ramandi et al. 2017; Moravej et al. 2018). For example, the most important complication associated with the use of silver as an antimicrobial agent is its strong biocidal property (Gholipourmalekabadi et al. 2015b; Nezafati et al. 2012). Furthermore, silver retards wound healing and causes formation of hypertrophic scar (Qian et al. 2017).
The effects of various concentrations (ranging from 4 µg ml−1 to 4 mg ml−1) of peptide versus 1% AgBG on the AT-MSC and fibroblast viability and cytotoxicity were determined by MTT and LDH (Figs. 3 and 4). At 24-h post-incubation for both AT-MSC and fibroblast samples, no difference in cell viability and cytotoxicity levels was observed in 64 µg ml−1 of CM11 peptide and 1% AgBG (p ≥ 0.05). At 48-h exposure time interval, both CM11 peptide and 1% AgBG exhibited cytotoxicity effects at concentrations of ≥ 2 mg ml−1 and 64 µg ml−1, respectively (p ≤ 0.05). After 72 h, 1% AgBG negatively affected the cell viability of the cells in concentrations of ≥ 32 µg ml−1 (p ≤ 0.05), while at the same time, CM11 peptide in concentrations of ≤ 1 mg ml−1 showed no significant cytotoxicity against the tested cells (p ≥ 0.05). The results also indicated that AT-MSCs were a little more sensitive than fibroblast when exposed to peptide and 1% AgBG. The results revealed that the cytotoxicity effect of peptide was less than 1% AgBG. In addition, it is estimated that the cytotoxicity exhibition of 1% AgBG after 72 h will be greatly more than peptide due to the sustained release of silver from bioactive glass. All the findings obtained from MTT and LDH were confirmed by the DAPI staining of the cells and determination of the cell density.
MIC and MBC of CM11 peptide and 1% AgBG
Amphipathic cationic peptides such as the CM11 act as a cell-permeable agent. Their positive charge causes electrostatic interactions with the poly-anionic compounds in the surface of bacterial cell membranes including lipopolysaccharide in Gram-negative bacteria and teichoic acid in Gram-positive bacteria. Their hydrophobic region enables them to penetrate the cell membrane, which leads to hole formation, resulting in the leakage of essential cellular components or passage of hydrophobic compounds across the cell membrane (Shai 2002; Nguyen et al. 2011). Based on the studies reported by Shai and Ferre et al., CM11 peptide kills bacteria via a “carpet-like” mechanism. Accordingly, after carpeting and thinning of the bacteria cell membrane by peptide, at a critical threshold concentration, peptide forms toroidal transient holes in the membrane and above this concentration, the membrane disintegrates and forms micelles after disruption of the bilayer curvature (Shai 2002; Ferre et al. 2006). In general, the damaging property of AMPs depends on charge, hydrophobicity, amphipathicity, stereochemistry, and propensity of peptides to form barrels. In addition, sensitivity of eukaryotic cells to AMPs also depends on variations in membrane lipid compositions and membrane hydrophobicity. Silver ions show toxicity activity through degradation of essential molecules such as DNA and RNA (Feng et al. 2000; Jeon et al. 2003).
The MIC and MBC values of peptide and 1% AgBG for standard strains, and A. baumannii and P. aeruginosa isolates are shown in Tables 2 and 3. The results showed that CM11 peptide and 1% AgBG had MIC of ≥ 8 μg ml−1 and ≥ 1 mg ml−1 for bacterial standard strains, respectively. MBC of peptide and 1% AgBG for bacterial standard strain was ≥ 8 μg ml−1 and ≥ 2 mg ml−1, respectively (Table 2). Peptide and 1% AgBG had MIC of ≥ 16 μg ml−1 and ≥ 4 mg ml−1 for clinical isolates, respectively. In addition, MBC of peptide and 1% AgBG for these resistant bacteria was ≥ 32 μg ml−1 and ≥ 4 mg ml−1, respectively (Table 3). Among the clinical isolates, two P. aeruginosa and one A. baumannii were resistant to 1% AgBG even in 4 mg ml−1.
Our results clearly indicate that some of XDR bacteria isolated from burn patients are resistant to all antibiotics and even high masses of silver. On the other hand, the CM11 peptide in concentrations of ≤ 1 mg ml−1 did not affect the viability of both AT-MSCs and fibroblasts and showed high biocompatibility property, while the safe concentrations of 1% AgBG for AT-MSCs and fibroblasts were ≤ 16 μg ml−1. Taken together, our interesting findings reveal that unlike 1% AgBG, peptide has an efficient antibacterial activity, even for XDR clinical isolates, in its safe concentration. These data may alter the current treatment strategies that use 1% silver sulfadiazine or skin substitute transplantation with non-/weak antibacterial property and suggest that peptide therapy as a potential candidate, reliable, alternative and safe strategy can be used for the treatment of burn infections caused by multidrug-resistant bacteria.
Accordingly, Huang et al. (2013) showed that antimicrobial peptide Epinecidin-1 protects skin wounds created in mice against methicillin-resistant Staphylococcus aureus. It has also been reported the synergic anti-mycobacterial activity of cationic a-helical peptides with rifampicin (Khara et al. 2014). Immuno-modulatory and broad-spectrum antibacterial property of the antimicrobial peptide piscidin were reported by Chen et al. (2015). Non-cytotoxicity effects of antimicrobial proline-rich peptide for macrophages have been shown by Pelillo et al. (2014).
In vivo biocompatibility
The high biocompatibility of antibacterial agents is very critical and guarantees their safety. The body immune responses after subcutaneous injection of various concentrations of both peptide and 1% AgBG were investigated and the results are shown in Fig. 5. Our findings showed that CM11 peptide did not stimulate body immune system by both 3 and 7 days post-injection, as infiltration of LC, MQ and PC did not change in this group compared with control (the animals subcutaneously injected with PBS). In 1% AgBG samples, the average number of LC and MQ was significantly increased in concentrations of ≥ 64 µg ml−1 by day 3. At day 7 post-injection of 1% AgBG, the average number of LC and MQ in concentrations of ≥ 64 µg ml−1 remained significantly increased. In this time, the average number of PC in concentrations of ≥ 16 µg ml−1 was significantly higher than those in control sample. In our previous studies (Gholipourmalekabadi et al. 2016a; Nezafati et al. 2012), we showed that AgBG has a durable antibacterial activity through a sustained release of silver ions. In those studies, AgBG showed concentration-dependent antibacterial activity. In higher concentrations, silver shows cytotoxicity for eukaryote cells, as reported by many studies (Gholipourmalekabadi et al. 2016a; Nezafati et al. 2012; Franci et al. 2015). Our findings indicate that CM11 peptide has high biocompatibility and safety in all evaluated concentrations, while biocompatibility of 1% AgBG is highly dependent on its concentration.
In vivo biocompatibility. Various concentrations of CM11 peptide and 1% AgBG (ranging from 4 µm ml−1 to 4 mg ml−1) were injected subcutaneously. At 3- and 7-day post-injection interval times, infiltration of inflammatory cells was counted and reported. *Significant difference with control (p < 0.05)
Conclusion
Increasing incidence of extensively drug-resistant bacteria isolated from burn patients has become a serious problem in burn centers. In this study, we showed that clinical isolates are extensively resistant to commonly used antibiotic and 1% silver-doped bioactive glass. On the other hand, cationic antimicrobial peptide (CM11) shows to be an effective and safe antibacterial agent for the possible treatment of the infections caused by these bacteria. Our interesting results may attract the attention of many researchers in this area for clinical use of cationic AMPs such as CM11 in health centers as a prevention/treatment strategy of extensively drug-resistant bacterial infections.
References
Aghamollaei H, Moghaddam MM, Kooshki H, Heiat M, Mirnejad R, Barzi NS (2015) Detection of Pseudomonas aeruginosa by a triplex polymerase chain reaction assay based on lasI/R and gyrB genes. J Infect Public Health 8(4):314–322
Albers CE, Hofstetter W, Siebenrock KA, Landmann R, Klenke FM (2013) In vitro cytotoxicity of silver nanoparticles on osteoblasts and osteoclasts at antibacterial concentrations. Nanotoxicology 7(1):30–36
Amani J, Barjini KA, Moghaddam MM, Asadi A (2015) In vitro synergistic effect of the CM11 antimicrobial peptide in combination with common antibiotics against clinical isolates of six species of multidrug-resistant pathogenic bacteria. Protein Pept Lett 22(10):940–951
Ardebili A, Lari AR, Talebi M (2014) Correlation of ciprofloxacin resistance with the AdeABC efflux system in Acinetobacter baumannii clinical isolates. Ann Lab Med 34(6):433–438
AshaRani P, Low Kah Mun G, Hande MP, Valiyaveettil S (2008) Cytotoxicity and genotoxicity of silver nanoparticles in human cells. ACS Nano 3(2):279–290
Azad ZM, Moravej H, Fasihi-Ramandi M, Masjedian F, Nazari R, Mirnejad R, Moghaddam MM (2017) In vitro synergistic effects of a short cationic peptide and clinically used antibiotics against drug-resistant isolates of Brucella melitensis. J Med Microbiol 66(7):919–926
Badosa E, Ferre R, Planas M, Feliu L, Besalú E, Cabrefiga J, Bardají E, Montesinos E (2007) A library of linear undecapeptides with bactericidal activity against phytopathogenic bacteria. Peptides 28(12):2276–2285
Bakal SN, Bereswill S, Heimesaat MM (2017) Finding novel antibiotic substances from medicinal plants—antimicrobial properties of Nigella sativa directed against multidrug resistant bacteria. Eur J Microbiol Immunol 7(1):92–98
Bem AE, Velikova N, Pellicer MT, Pv Baarlen, Marina A, Wells JM (2014) Bacterial histidine kinases as novel antibacterial drug targets. ACS Chem Biol 10(1):213–224
Bonomo RA, Szabo D (2006) Mechanisms of multidrug resistance in Acinetobacter species and Pseudomonas aeruginosa. Clin Infect Dis 43(Supplement 2):S49–S56
Chen W-F, Huang S-Y, Liao C-Y, Sung C-S, Chen J-Y, Wen Z-H (2015) The use of the antimicrobial peptide piscidin (PCD)-1 as a novel anti-nociceptive agent. Biomaterials 53:1–11
Chung PY, Khanum R (2017) Antimicrobial peptides as potential anti-biofilm agents against multidrug-resistant bacteria. J Microbiol Immunol Infect 50(4):405–410
Clinical and laboratory standards institute (2007) Performance standards for antimicrobial susceptibility testing. Informational supplement. Wayne, PA
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop D, Horwitz E (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8(4):315–317
Ellis D, Cohen B, Liu J, Larson E (2015) Risk factors for hospital-acquired antimicrobial-resistant infection caused by Acinetobacter baumannii. Antimicrob Resist Infect Control 4(1):40
Evans JC, Segal H (2007) A novel insertion sequence, ISPA26, in oprD of Pseudomonas aeruginosa is associated with carbapenem resistance. Antimicrob Agents Chemother 51(10):3776–3777
Fallah F, Taherpour A, Vala MH, Hashemi A (2012) Global spread of New Delhi metallo-beta-lactamase-1 (NDM-1). Arch Clin Infect Dis 6(4):171–177
Feng QL, Wu J, Chen G, Cui F, Kim T, Kim J (2000) A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus. J Biomed Mater Res 52(4):662–668
Ferre R, Badosa E, Feliu L, Planas M, Montesinos E, Bardají E (2006) Inhibition of plant-pathogenic bacteria by short synthetic cecropin A-melittin hybrid peptides. Appl Environ Microbiol 72(5):3302–3308
Franci G, Falanga A, Galdiero S, Palomba L, Rai M, Morelli G, Galdiero M (2015) Silver nanoparticles as potential antibacterial agents. Molecules 20(5):8856–8874
Gholipourmalekabadi M, Bandehpour M, Mozafari M, Hashemi A, Ghanbarian H, Sameni M, Salimi M, Gholami M, Samadikuchaksaraei A (2015a) Decellularized human amniotic membrane: more is needed for an efficient dressing for protection of burns against antibiotic-resistant bacteria isolated from burn patients. Burns 41(7):1488–1497
Gholipourmalekabadi M, Nezafati N, Hajibaki L, Mozafari M, Moztarzadeh F, Hesaraki S, Samadikuchaksaraei A (2015b) Detection and qualification of optimum antibacterial and cytotoxic activities of silver-doped bioactive glasses. IET Nanobiotechnol 9(4):209–214
Gholipourmalekabadi M, Sameni M, Hashemi A, Zamani F, Rostami A, Mozafari M (2016a) Silver-and fluoride-containing mesoporous bioactive glasses versus commonly used antibiotics: activity against multidrug-resistant bacterial strains isolated from patients with burns. Burns 42(1):131–140
Gholipourmalekabadi M, Sameni M, Radenkovic D, Mozafari M, Mossahebi-Mohammadi M, Seifalian A (2016b) Decellularized human amniotic membrane: how viable is it as a delivery system for human adipose tissue-derived stromal cells? Cell Prolif 49(1):115–121
Hakemi Vala M, Hallajzadeh M, Hashemi A, Goudarzi H, Tarhani M, Sattarzadeh Tabrizi M, Bazmi F (2014) Detection of ambler class A, B and D ß-lactamases among Pseudomonas aeruginosa and Acinetobacter baumannii clinical isolates from burn patients. Ann Burns Fire Disasters 27(1):8–13
Huang H-N, Rajanbabu V, Pan C-Y, Chan Y-L, Wu C-J, Chen J-Y (2013) Use of the antimicrobial peptide Epinecidin-1 to protect against MRSA infection in mice with skin injuries. Biomaterials 34(38):10319–10327
Ikonomidis A, Tsakris A, Kanellopoulou M, Maniatis A, Pournaras S (2008) Effect of the proton motive force inhibitor carbonyl cyanide-m-chlorophenylhydrazone (CCCP) on Pseudomonas aeruginosa biofilm development. Lett Appl Microbiol 47(4):298–302
Jeon H-J, Yi S-C, Oh S-G (2003) Preparation and antibacterial effects of Ag–SiO2 thin films by sol–gel method. Biomaterials 24(27):4921–4928
Khara JS, Wang Y, Ke X-Y, Liu S, Newton SM, Langford PR, Yang YY, Ee PLR (2014) Anti-mycobacterial activities of synthetic cationic α-helical peptides and their synergism with rifampicin. Biomaterials 35(6):2032–2038
Kosikowska P, Lesner A (2016) Antimicrobial peptides (AMPs) as drug candidates: a patent review (2003–2015). Expert Opin Ther Pat 26(6):689–702
Lachine M, El-Nahas A, Elsawy E, Mosbah A, El-Kappany H (2016) 1038 A randomized controlled trial comparing antimicrobial coated (silver sulfadiazine) ureteral stents with non-coated stents. Eur Urol Suppl 15(3):e1038
Leseva M, Arguirova M, Nashev D, Zamfirova E, Hadzhyiski O (2013) Nosocomial infections in burn patients: etiology, antimicrobial resistance, means to control. Ann Burns Fire Disasters 26(1):5–11
Llanes C, Hocquet D, Vogne C, Benali-Baitich D, Neuwirth C, Plésiat P (2004) Clinical strains of Pseudomonas aeruginosa overproducing MexAB-OprM and MexXY efflux pumps simultaneously. Antimicrob Agents Chemother 48(5):1797–1802
Moghaddam MM, Abolhassani F, Babavalian H, Mirnejad R, Barjini KA, Amani J (2012) Comparison of in vitro antibacterial activities of two cationic peptides CM15 and CM11 against five pathogenic bacteria: Pseudomonas aeruginosa, Staphylococcus aureus, Vibrio cholerae, Acinetobacter baumannii, and Escherichia coli. Probiotics Antimicrob Proteins 4(2):133–139
Moghaddam MM, Barjini KA, Ramandi MF, Amani J (2014) Investigation of the antibacterial activity of a short cationic peptide against multidrug-resistant Klebsiella pneumoniae and Salmonella typhimurium strains and its cytotoxicity on eukaryotic cells. World J Microbiol Biotechnol 30(5):1533–1540
Mohammadzadeh A, Pourfathollah AA, Shahrokhi S, Hashemi SM, Moradi SLA, Soleimani M (2014) Immunomodulatory effects of adipose-derived mesenchymal stem cells on the gene expression of major transcription factors of T cell subsets. Int Immunopharmacol 20(2):316–321
Moravej H, Fasihi-Ramandi M, Moghaddam MM, Mirnejad R (2018) Cytotoxicity and antibacterial effect of Trp-substituted CM11 cationic peptide against drug-resistant isolates of Brucella melitensis alone and in combination with recommended antibiotics. Int J Pept Res Ther. https://doi.org/10.1099/jmm.0.000524
Nezafati N, Moztarzadeh F, Hesaraki S, Mozafari M, Samadikuchaksaraei A, Hajibaki L, Gholipour M (2012) Effect of silver concentration on bioactivity and antibacterial properties of SiO2–CaO–P2O5 sol-gel derived bioactive glass. In: Key engineering materials, vol 493–494. Trans Tech Publ, pp 74–79
Nguyen LT, Haney EF, Vogel HJ (2011) The expanding scope of antimicrobial peptide structures and their modes of action. Trends Biotechnol 29(9):464–472
Noori M, Karimi A, Fallah F, Hashemi A, Alimehr S, Goudarzi H, Aghamohammad S (2014) High prevalence of metallo-beta-lactamase producing Acinetobacter baumannii isolated from two hospitals of Tehran, Iran. Arch Pediatr Infect Dis 2(3):e15439
Pelillo C, Benincasa M, Scocchi M, Gennaro R, Tossi A, Pacor S (2014) Cellular internalization and cytotoxicity of the antimicrobial proline-rich peptide Bac7 (1-35) in monocytes/macrophages, and its activity against phagocytosed Salmonella typhimurium. Protein Pept Lett 21(4):382–390
Qian L-W, Fourcaudot AB, Leung KP (2017) Silver sulfadiazine retards wound healing and increases hypertrophic scarring in a rabbit ear excisional wound model. J Burn Care Res 38(1):e418–e422
Ramandi MF, Piranfar V, Nadoushan MJ, Sarshoori JR, Misialek MJ, Heiat M, Moghaddam MM (2017) Dose-response effects of the CM11 as a short cationic antimicrobial peptide on histopathological and biochemical changes in mice. Curr Chem Biol 11(2):150–157
Rostami A, Mozafari M, Gholipourmalekabadi M, Caicedo HH, Lasjerdi Z, Sameni M, Samadikuchaksaraei A (2015) Optimization of fluoride-containing bioactive glasses as a novel scolicidal agent adjunct to hydatid surgery. Acta Trop 148:105–114
Shai Y (2002) Mode of action of membrane active antimicrobial peptides. Pept Sci Orig Res Biomol 66(4):236–248
Silver S, Phung LT, Silver G (2006) Silver as biocides in burn and wound dressings and bacterial resistance to silver compounds. J Ind Microbiol Biotechnol 33(7):627–634
Acknowledgements
We wish to express our appreciation to Dr. Ali Rostami for his constructive comments on this manuscript.
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
MMM, AH and MG conceived and designed the study. MMM, ME, BF, ZL, VFO, MG, MM-M, AH and MMM performed the experiments. MG, SE, AH and HG analyzed the data. MG and AH interpreted the results. MG, SE, MMM, ME, BF and AH prepared the manuscript. MG, AMS, SE, NPS, AH and MMM reviewed the preparation of manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Ethical approval
The studies have been approved by the research ethics committee of the Shahid Beheshti University of Medical Sciences, Tehran, Iran. All procedures performed in studies involving human participants were in accordance with the ethical standards of the SBUMS research committee and have been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Also for animal studies, experiments were approved by the Institutional Animal Care and Use committee of the SBUMS, and were performed in accordance with the Guide for the Care and Use of Laboratory Animals published by the National Institutes of Health.
Formal consent
For this type of study, formal consent is not required.
Additional information
Handling Editor: F. Albericio.
Electronic supplementary material
Below is the link to the electronic supplementary material.
726_2018_2638_MOESM2_ESM.tif
(A) Analysis of synthetic peptide (CM 11) by Reverse-phase HPLC using C18 Tracer column and a linear gradient from 10 to 60% acetonitrile in water with 0.1% TFA. (B) Mass spectroscopic analysis of the CM11 peptide (MH+=1415.85) was performed by electrospray ionization mass spectrometry which confirmed peptide identity. Supplementary material 2 (TIFF 804 kb)
726_2018_2638_MOESM3_ESM.tif
Characterization of hAT-MSCs. (A) The images taken from the hAT-MSCs under light microscope by days 3, 7 and 21 post-extraction, and the fibroblast L929. (B) Flow cytometric results of the hAT-MSCs. The percentages of the cells expressing Sca1, CD44, CD90 and CD105, CD11b, CD33, CD34 and CD45 were 98.5%, 97.9%, 98.4 and 96.5%, 2.9%, 3.1%, 2.6%, 4.3%, respectively. Supplementary material 3 (TIFF 5325 kb)
Rights and permissions
About this article
Cite this article
Moosazadeh Moghaddam, M., Eftekhary, M., Erfanimanesh, S. et al. Comparison of the antibacterial effects of a short cationic peptide and 1% silver bioactive glass against extensively drug-resistant bacteria, Pseudomonas aeruginosa and Acinetobacter baumannii, isolated from burn patients. Amino Acids 50, 1617–1628 (2018). https://doi.org/10.1007/s00726-018-2638-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-018-2638-z