Abstract
Purpose
To clarify the advantages and disadvantages of stenting as a bridge to surgery (BTS) by comparing the clinical features and outcomes of patients who underwent BTS with those of patients who underwent emergency surgery (ES).
Methods
We assessed technical success, clinical success, surgical procedures, stoma formation, complications, clinicopathological features, and Onodera’s prognostic nutritional index (OPNI) in patients who underwent BTS and those who underwent ES.
Results
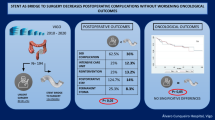
Twenty-six patients underwent stenting, which was successful in 22 (BTS group). The remaining four patients with unsuccessful stenting underwent emergency surgery. A total of 22 patients underwent emergency surgery (ES group). The rates of technical and clinical success were 85.0 and 81.0 %, respectively. The proportion of patients able to be treated by laparoscopic surgery (P = 0.0001) and avoid colostomy (P = 0.0042) was significantly higher in the BTS group. Although the incidence of anastomotic leakage in the two groups was not significantly different, it was significantly reduced by colonoscopic evaluation of obstructive colitis (P = 0.0251). The mean number of harvested lymph nodes (P = 0.0056) and the proportion of D3 lymphadenectomy (P = 0.0241) were significantly greater in the BTS group. Perineural invasion (PNI) was noted in 59.1 and 18.2 % of the BTS group and ES group patients, respectively (P = 0.0053). OPNI and serum albumin decreased significantly after stenting (P = 0.0084).
Conclusions
The advantages of stenting as a BTS were that it avoided colostomy and allowed for laparoscopic surgery and lymphadenectomy, whereas its disadvantage lay in the decreased PNI and OPNI levels. A larger study including an analysis of prognosis is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is one of the most common cancers in the world. Obstruction is a frequent clinical presentation and the incidence of obstructive colorectal cancer has remained unchanged for decades [1]. Obstructive colorectal cancer, reported to account for about 10–29 % of all colorectal cancers [1–3], is a common emergency that requires decompression to prevent perforation, bacterial translocation, and ischemia, especially in the left-side colon. The rates of mortality and complications associated with emergency surgery for obstructive colorectal cancer are higher than those associated with elective surgery [1, 4–6]. In an emergency surgical situation, it is difficult to evaluate the patient’s general condition and treat comorbidities and malnutrition. The metallic colonic stent, which was introduced clinically in the 1990s [7, 8], is an alternative tool for avoiding emergency surgery, and applied for palliation or as a bridge to surgery (BTS) [9–11]. While it is generally accepted that stenting for obstructive colorectal cancer can achieve decompression of bowel obstruction and avoid a stoma, while providing time for medical examination and stabilization of the patient’s general condition [12–15], the advantages of stenting as a BTS have not fully clarified. In relation to avoiding the need for colostomy, a review and meta-analysis study showed no significant differences between a stent group and a surgery group [16]. Anastomotic leakage can cause lethal complications, necessitating reoperation for stoma formation. Successful decompression by stent insertion should prevent anastomotic leakage, but again, its true efficiency in achieving this has not been established [16–18]. The postoperative prognosis of patients who undergo BTS also remains to be clarified [16, 19, 20]. Although stenting has been applied widely for obstructive colorectal cancer, many questions remain unanswered.
We conducted this study to clarify the advantages and disadvantages of colonic stenting by comparing patients who underwent BTS with those who underwent emergency surgery (ES), focusing on operative methods, postoperative complications, and clinicopathological factors. We also assessed the utility of colonoscopic evaluation of obstructive colitis for reducing the risk of anastomotic leakage.
Methods
Patients
Between December 2012 and December 2014, 26 patients underwent stenting for obstructive colon cancer at Osaka National Hospital. Stenting for obstructive colon cancer was approved for medical insurance cover in Japan in 2012. Thus, since 2012, stenting has been performed all patients who require emergency bowel decompression for obstructive colon cancer, except those with suspected or impending perforation, enteral ischemia, or intra-abdominal abscess. Stenting as a BTS was performed successfully in 22 patients (BTS group), but was unsuccessful in four patients, who subsequently underwent ES. Between January 2009 and November 2012, 18 patients underwent ES for obstructive colon cancer at Osaka National Hospital. With the additional four patients from the latter period, ES was performed on a total 22 patients between January 2009 and July 2014 (ES group). All patients in the BTS and ES groups required a continuous bowel decompressive procedure.
Endoscopic procedures
A SEMS (self-expandable metallic stent) was inserted via colonoscopy under fluoroscopic guidance by experienced gastroenterology physicians at Osaka National Hospital [8]. Contrast was introduced from the catheter to identify the appropriate length of the narrowed segment, and determine the length of the WallFlex Colonic Stents (Boston Scientific). To confirm the extension and position of the stent, abdominal X-rays were taken the day after stenting. Clinical and technical success was defined by the alleviation of clinical obstructive symptoms and sufficient dilation of the stenosis [9, 10]. Pre-operative colonoscopy was done in only one patient, who underwent polypectomy before surgery in early 2014. All patients who had a SEMS inserted after May 2014 underwent colonoscopy to evaluate the obstructive colitis.
Assessment of tumor stage
Tumor stages were defined according to the TNM Classification of Malignant Tumors 7th edition published from the Union Internationale Contre le Cancer (UICC).
Analysis of prognostic nutritional index
The Onodera’s prognostic nutritional index (OPNI) was calculated using the following formula: 10 × serum albumin value (g/dl) + 0.005 × lymphocyte count in peripheral blood [21–23].
Statistical analysis
Results are expressed as the mean ± standard deviation (SD) or median. Student’s t test and Mann–Whitney U test were used to assess statistical significance. Statistical distributions of data were confirmed with the Gaussian distribution. All statistical analyses were performed using JMP 11.0.0 software (SAS Institute, Cary, NC). Results were considered significant at P < 0.05.
Results
Technical and clinical success rates of stent insertion
Stenting was successful in 22 of 26 patients. The other four patients required ES. The rates of technical success and clinical success were 85.0 % (22/26) and 81.0 % (21/26), respectively. Technical success was defined as the successful insertion of a stent with sufficient dilation of the stenosis at the stenosis location, whereas clinical success was defined as the alleviation of clinical obstructive symptoms [9, 10]. Re-obstruction by compressive tumor growth occurred in one patient and accidental stent migration caused by colonoscopic polypectomy performed after stenting occurred in one. This accidental stent migration was excluded from the clinically unsuccessful cases. During the preoperative period, stent-associated complications such as perforation, ischemia, and intraperitoneal abscesses were not observed. Oral intake was started after the passing of flatus, defecation, alleviation of obstructive symptoms, and confirmation of sufficient stent location on abdominal X-rays. All but 1 of the 22 patients recommenced oral intake 3 ± 1.7 days after stent insertion (range days 1–6). The remaining patient required ongoing total-parenteral nutrition.
Baseline characteristics of patients
Patients were divided into two groups: a BTS group (n = 22) and an ES group (n = 22). All of the patients required a procedure for continuous decompression and could not tolerate any oral intake. Surgery was performed 12.7 ± 4.8 days after stenting (range 2–21 days). The mean age of the patients in the BTS and ES groups was 67 ± 11.0 years (12 men and 10 women) and 68 ± 10.0 years (15 men and 7 women), respectively There were no significant differences in tumor location, tumor stage, node status, distant metastasis, UICC clinical stage, or maximal tumor diameter between the groups (Table 1).
Analysis of operative procedures and perioperative complications
In the BTS group, laparoscopic surgery was performed for 20 patients (91 %), while two required laparotomy: for posterior pelvic exenteration in one patient with sigmoid colon cancer with uterus invasion, and for sigmoidectomy in one patient with sigmoid colon cancer with liver metastases and main portal vein tumor thrombus. In the ES group, laparoscopic surgery was performed only for three patients (13.7 %). A permanent stoma was required in only 3 (13.6 %) of the 22 BTS patients, but in 12 (54.5 %) of the 22 ES patients. When limited to left side of the colon, the stoma rate was 14.3 % (3/21) in the BTS group and 63.2 % (12/19) in the ES group.
In relation to perioperative complications, anastomotic leakage was recognized in three (13.6 %) patients from the BTS group and two (9.1 %) from the ES group. When restricted to the left side of the colon with primary anastomosis, the rates of anastomotic leakage were 11.1 % (2/18) and 28.6 % (2/7) in the BTS and ES groups, respectively (P = 0.2850). One patient from the ES group suffered perforation after Hartmann’s operation and the pathological findings of the resected perforated colon indicated obstructive colitis. Surgical site infection (SSI) [24, 25] developed in two patients (9.1 %) from the BTS group and four patients (18.2 %) from the ES group (P = 0.3796). Post-operative bowel obstruction developed in one patient from the ES group.
Importance of preoperative colonoscopy for reducing the risk of anastomotic leakage
We performed colonoscopy to evaluate obstructive colitis and mucosal edema in every patient from June, 2014. There were three cases of anastomotic leakage between December, 2012 and May, 2014, and all three resected primary tumor specimens were found to have obstructive colitis with a longitudinal ulcer and inflammatory change; hence, we started performing preoperative colonoscopy to evaluate the mucosal condition of the oral side of the colon (Table 2). To assess the importance of preoperative colonoscopic surveillance, the BTS group was divided into two sub-groups: with or without preoperative colonoscopy. Colonoscopy was performed in 13 patients (CS group; 59 %) and not performed in 9 (non-CS group; 41 %). We performed primary anastomosis in 12 (92.3 %) of the 13 CS group patients and 7 (77.8 %) of the 9 non-CS group patients (Table 3). There was no case of anastomotic leakage (0 %) in the CS group, but three cases (33.3 %) in the non-CS group (P = 0.0251). Anastomotic leakage was assessed using the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. Basically, anastomotic leakage occurred only after primary anastomosis in the non-CS group (42.9 %) in patients who underwent laparoscopic sigmoidectomy (CTCAE grade 4), low anterior resection (CTCAE grade 4), or right hemicolectomy (CTCAE grade 2). Preoperative colonoscopy allowed us to detect obstructive colitis in one patient (1/13; 7.7 %) and anastomotic leakage was circumvented by performing careful anastomosis, after the obstructive colitis lesion had been included in the resection area.
Assessing the clinicopathological findings of the BTS and ES groups
Because there was no significant difference in the depth of the tumor, lymph node metastasis, metastatic status, or UICC stage between the BTS and ES groups (Table 1), we assessed the pathological findings including venous invasion, lymphatic invasion and perineural invasion (PNI). There was no significant difference in lymphatic invasion or venous invasion between the BTS and ES groups (Table 4). The incidence of PNI was significantly higher in the BTS group than in the ES group (P = 0.0053), being identified in 13 (59.1 %) vs. 4 (18.2 %) cases, respectively. The PNI-positive cases in the BTS group comprised seven cases of T3, three of T4a, and three of T4b, with clinical stages of II (n = 7), III (n = 4), and IV (n = 2). Two of four PNI-positive cases in the ES group involved patients who had unsuccessful stent insertion: one with sigmoid colon cancer (T4a, stage II) and one with rectosigmoid colon cancer (T4a, stage II). The other two cases were a patient with upper rectal cancer (T3, stage II) and one with rectosigmoid cancer (T4a, stage IV). There was no significant relationship between PNI and tumor stage (T factor, P = 0.8740).
Analysis of the extent of lymphadenectomy
We assessed the extent of lymphadenectomy in the BTS and ES groups. In the BTS group, 90.9 % of the patients underwent lymphadenectomy at the root of the primary feeding artery (D3) and 9.1 % underwent high mesenteric artery ligation (D2). In the ES group, 54.5 % of the patients underwent D3 lymphadenectomy, 41.0 % underwent D2 lymphadenectomy, and 4.5 % underwent lymphadenectomy in the marginal area (D1). The extent of lymphadenectomy was significantly greater in the BTS group (P = 0.0241). The number of harvested lymph nodes was significantly higher in the BTS group than in the ES group, at 37.5 ± 23.2 vs. 22.9 ± 13.8, respectively (P = 0.0056; Table 4).
Analysis of serum albumin level and Onodera’s prognostic nutritional index
Stenting is done to provide time for the patient’s general condition to stabilize [9–11]. Successful stenting is considered pivotal to improving malnutrition. To assess whether stenting improves the nutritional status of patients with bowel obstruction, we looked at the changes in serum albumin levels after stenting in 20 of the 22 BTS patients who underwent stenting. One was excluded because of the lack of data and one was on continuous total-parenteral nutrition. All 20 patients were allowed oral intake and were not receiving an infusion. Serum albumin levels were measured on the day of stenting and 1 day before surgery, and the levels 1 day before surgery were significantly decreased despite sufficient oral intake (P = 0.0210). We then compared the serum albumin levels in these 20 patients from the BTS group with those in the 22 patients from the ES group, and found no significant difference (P = 0.5786; Fig. 1a, b).
Analysis of levels of serum albumin and Onodera’s prognostic nutritional index. Levels of serum albumin before stenting and before emergency surgery were not significantly different (P = 0.5786) (a). In the 20 BTS group patients, the serum albumin level decreased significantly after stenting (P = 0.0210) (b). Onodera’s prognostic nutritional indexes of the patients before stenting and before emergency surgery were not significantly different (P = 0.3205) (c). Onodera’s prognostic nutritional indexes decreased significantly after stenting compared with those before stenting (P = 0.0326) (d)
The OPNI was assessed in these 20 patients from the BTS group and found to be significantly lower 1 day before surgery than just before stenting (44.22 ± 6.95 vs. 39.35 ± 6.88, respectively; P = 0.0326). Conversely, the OPNI in the ES group was 42.41 ± 6.23, which was not significantly different from that just before stenting in the BTS group (P = 0.3205).
Discussion
The colonic stent was introduced in the 1990s for both palliation and as a BTS [7, 8]. The major complications associated with colonic stent placement are perforation, re-obstruction, and migration [9, 10]. While some reviews and a single center study reported 47.0–96.7 % technical success and 70.2–100 % clinical success, with perforation and re-obstruction rates of 2–12 and 10–14 %, respectively [9, 26, 27], certain studies were terminated because patients suffered serious complications. The Dutch Stent-in I study (ISRCTN01790428) was terminated prematurely because of a 40 % incidence of perforation, resulting in the death of 30 % of these patients [17]. In 2011, a European multi-center randomized trial was also suspended for a high rate of perforation (12.8 %) and those authors proposed that colonic stenting has no decisive clinical advantages over ES [28]. In the present series, there was 85.0 % technical success and 81.0 % clinical success, with 4.5 % migration and 4.5 % re-obstruction, but no perforation. In recent years, stent insertion has become safer with better techniques, improved training and experience of the physicians who perform this procedure, and more defined guidelines [29, 30]. However, larger studies are necessary to clarify its safety for obstructive colon cancer.
The advantage of BTS to avoid the need for colostomy is controversial. One review and meta-analysis study showed no significant differences in the incidence of permanent stoma between a stent group and a surgical group [16], but other studies, including ours showed that BTS had a significant advantage for avoiding colostomy [12, 13, 17, 19, 26, 31]. The advantage of stenting for preventing anastomotic leakage is also controversial, as some meta-analyses showed no significant difference between BTS groups and ES groups in relation to anastomotic leakage [16, 17, 32], whereas other reports documented a significant advantage of stenting for preventing anastomotic leakage [18, 19]. In our study, the incidence of anastomotic leakage did not differ significantly between the BTS and ES groups. Obstructive colitis sometimes involves a skipped lesion; hence, it is difficult to identify mucosal change in the whole colon from examining the resected stump. Indeed, one of our patients suffered perforation of the residual colon with obstructive colitis after Hartmann’s operation. Moreover, all three cases of anastomotic leakage in the BTS group were associated with obstructive colitis, suggesting that evaluating mucosal changes helps prevent anastomotic leakage. The sub-group analysis of the BTS group revealed that the incidence of anastomotic leakage was significantly less in the patients who had undergone preoperative colonoscopy. Obstructive colitis was found in one patient by preoperative colonoscopic surveillance and anastomotic leakage was circumvented by careful anastomosis after the obstructive colitis lesion was included in the resection area. Preoperative or intraoperative colonoscopy for evaluating mucosal changes including obstructive colitis and mucosal edema may be helpful for preventing anastomotic leakage. Since long-term stenting is considered to increase the risk of perforation, the timing of surgery should be planned promptly after the evaluation of obstructive colitis.
Malnutrition is well known to be a risk factor for anastomotic leakage [33]. In this study, despite sufficient nutritional intake, the serum albumin level decreased significantly after stenting, suggesting that stent insertion increased the risk of anastomotic leakage. Considering that the half-life of serum albumin is about 21 days and surgery was performed 12.7 ± 4.8 days after stenting, albumin levels may not define the nutritional condition after stenting. It is necessary to evaluate nutritional status using rapid turnover protein.
Successful decompression by stenting provides time to allow the patient’s systemic and surgical condition to improve, promoting surgical quality. In our study, the number of harvested lymph nodes was significantly higher and the incidence of D2 or D3 lymphadenectomy was significantly greater in the BTS group than in the ES group. Moreover, stenting made elective radical surgery possible: one patient underwent colectomy with hepatectomy and another underwent posterior pelvic exenteration.
Distended small bowel is a major deterrent to laparoscopic surgery because it obscures the visual field and occludes the space for forceps manipulation. In the present study, sufficient intestinal decompression enabled laparoscopic surgery to be carried out in 91 % of the patients. As laparoscopic surgery is minimally invasive surgery, it is an attractive option after stenting. Although there was no significant difference in the development of SSI in our study, laparoscopic surgery has been reported to reduce the risk of SSI. Of course it is necessary to confirm the benefit, feasibility, and safety of laparoscopic surgery after stenting in a large sample study because there are few reports on laparoscopic surgery after stenting [34–36].
Despite the benefits of stenting for obstructive colorectal cancer, there are still issues that need to be clarified. The prognostic impact of stenting remains unclear as some reviews and meta-analyses reported no significant difference in prognosis between BTS and ES groups [16, 19, 20, 37], but one retrospective study showed inferior overall survival of a stenting group [38]. We could not assess prognosis, but we assessed clinicopathological factors and found that the incidence of PNI was increased after stenting. PNI is known to be a marker for a more aggressive tumor phenotype and poor prognosis in colorectal cancer [39–41]. In our study, 18.2 % of patients from the ES group were PNI-positive, which is consistent with the findings of a previous report that PNI was positive in 22 % of colorectal cancer cases [39]. The finding that 59.1 % of patients in the BTS group were PNI-positive suggests that the stent insertion potentially induces tumor cell invasion to peripheral nerves. The reason why stenting induces perineural invasion has not been clarified, although it could be attributable to the pressure effect of a self-expandable stent inducing the invasion of cancer cells into perineural space [42]. The OPNI [21–23], an established assessment tool for the nutritional status and prognosis of patients with malignancy, was also decreased in the patients who underwent stenting for BTS. A low OPNI of around 40 in patients with colon cancer has been associated with poor prognosis.
In the European Society of Gastrointestinal Endoscopy (ESGE) clinical guidelines [29], self-expandable metallic stent placement as a bridge to elective surgery is not recommended as a standard treatment for symptomatic left-sided malignant colonic obstruction. These clinical guidelines also state that stent placement for patients with potentially curable but obstructing left-sided colonic cancer may be considered as an alternative to ES for those at increased risk of postoperative mortality; namely, those with American Society of Anesthesiologists (ASA) physical status ≥III and/or an age >70 years.
In conclusion, although stenting as a BTS for obstructive colon cancer has some advantages, its oncological risks and long-term prognosis have not clarified. A large randomized controlled study is necessary to clarify the safety, feasibility, and long-term prognosis of stenting as a BTS.
References
Cheynel N, Cortet M, Lepage C, Benoit L, Faivre J, Bouvier AM. Trends in frequency and management of obstructing colorectal cancers in a well-defined population. Dis Colon Rectum. 2007;50(10):1568–75.
Tuca A, Guell E, Martinez-Losada E, Codorniu N. Malignant bowel obstruction in advanced cancer patients: epidemiology, management, and factors influencing spontaneous resolution. Cancer Manag Res. 2012;4:159–69.
Ripamonti C, De Conno F, Ventafridda V, Rossi B, Baines MJ. Management of bowel obstruction in advanced and terminal cancer patients. Ann Oncol. 1993;4(1):15–21.
Runkel NS, Schlag P, Schwarz V, Herfarth C. Outcome after emergency surgery for cancer of the large intestine. Br J Surg. 1991;78(2):183–8.
Leitman IM, Sullivan JD, Brams D, DeCosse JJ. Multivariate analysis of morbidity and mortality from the initial surgical management of obstructing carcinoma of the colon. Surg Gynecol Obstet. 1992;174(6):513–8.
Chen HS, Sheen-Chen SM. Obstruction and perforation in colorectal adenocarcinoma: an analysis of prognosis and current trends. Surgery. 2000;127(4):370–6.
Keen RR, Orsay CP. Rectosigmoid stent for obstructing colonic neoplasms. Dis Colon Rectum. 1992;35(9):912–3.
Tejero E, Mainar A, Fernández L, Tobío R, De Gregorio MA. New procedure for the treatment of colorectal neoplastic obstructions. Dis Colon Rectum. 1994;37(11):1158–9.
Khot UP, Lang AW, Murali K, Parker MC. Systematic review of the efficacy and safety of colorectal stents. Br J Surg. 2002;89(9):1096–102.
Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M. Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol. 2004;99(10):2051–7.
Tilney HS, Lovegrove RE, Purkayastha S, Sains PS, Weston-Petrides GK, Darzi AW, et al. Comparison of colonic stenting and open surgery for malignant large bowel obstruction. Surg Endosc. 2007;21(2):225–33.
Law WL, Choi HK, Chu KW. Comparison of stenting with emergency surgery as palliative treatment for obstructing primary left-sided colorectal cancer. Br J Surg. 2003;90(11):1429–33.
Martinez-Santos C, Lobato RF, Fradejas JM, Pinto I, Ortega-Deballón P, Moreno-Azcoita M. Self-expandable stent before elective surgery vs. emergency surgery for the treatment of malignant colorectal obstructions: comparison of primary anastomosis and morbidity rates. Dis Colon Rectum. 2002;45(3):401–6.
Xinopoulos D, Dimitroulopoulos D, Theodosopoulos T, Tsamakidis K, Bitsakou G, Plataniotis G, et al. Stenting or stoma creation for patients with inoperable malignant colonic obstructions? Results of a study and cost-effectiveness analysis. Surg Endosc. 2004;18(3):421–6.
Baqué P, Chevallier P, Karimdjee Solihi F, Rahili MA, Iannelli A, Benizri EI, et al. Colostomy vs self-expanding metallic stents: comparison of the two techniques in acute tumoral left colonic obstruction. Ann Chir. 2004;129(6–7):353–8.
Cirocchi R, Farinella E, Trastulli S, Desiderio J, Listorti C, Boselli C, et al. Safety and efficacy of endoscopic colonic stenting as a bridge to surgery in the management of intestinal obstruction due to left colon and rectal cancer: a systematic review and meta-analysis. Surg Oncol. 2013;22(1):14–21.
van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Lutke Holzik MF, Grubben MJ, et al. Colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol. 2011;12(4):344–52.
Saida Y, Sumiyama Y, Nagao J, Uramatsu M. Long-term prognosis of preoperative “bridge to surgery” expandable metallic stent insertion for obstructive colorectal cancer: comparison with emergency operation. Dis Colon Rectum. 2003;46:S44–9.
Zhang Y, Shi J, Shi B, Song CY, Xie WF, Chen YX. Self-expanding metallic stent as a bridge to surgery versus emergency surgery for obstructive colorectal cancer: a meta-analysis. Surg Endosc. 2012;26(1):110–9.
Tan CJ, Dasari BV, Gardiner K. Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg. 2012;99(4):469–76.
Kanda M, Fujii T, Kodera Y, Nagai S, Takeda S, Nakao A. Nutritional predictors of postoperative outcome in pancreatic cancer. Br J Surg. 2011;98(2):268–74.
Ikeya T, Shibutani M, Maeda K, Sugano K, Nagahara H, Ohtani H, et al. Maintenance of the nutritional prognostic index predicts survival in patients with unresectable metastatic colorectal cancer. J Cancer Res Clin Oncol. 2015;141(2):307–13.
Maeda K, Shibutani M, Otani H, Nagahara H, Sugano K, Ikeya T, et al. Low nutritional prognostic index correlates with poor survival in patients with stage IV colorectal cancer following palliative resection of the primary tumor. World J Surg. 2014;38(5):1217–22.
Tajima Y, Ishida H, Yamamoto A, Chika N, Onozawa H, Matsuzawa T, et al. Comparison of the risk of surgical site infection and feasibility of surgery between sennoside versus polyethylene glycol as a mechanical bowel preparation of elective colon cancer surgery: a randomized controlled trial. Surg Today. 2015 [Epub ahead of print].
Ojima H, Sohda M, Ando H, Sano A, Fukai Y, Ogawa A, et al. Relationship between functional end-to-end anastomosis for colon cancer and surgical site infections. Surg Today. 2015;45(12):1489-92.
Currie A, Christmas C, Aldean H, Mobasheri M, Bloom IT. Systematic review of self-expanding stents in the management of benign colorectal obstruction. Colorectal Dis. 2014;16(4):239–45.
Saida Y, Enomoto T, Takabayashi K, Otsuji A, Nakamura Y, Nagao J, et al. Outcome of 141 cases of self-expandable metallic stent placements for malignant and benign colorectal strictures in a single center. Surg Endosc. 2011;25(6):1748–52.
van Hooft JE, Fockens P, Marinelli AW, Bossuyt PM, Bemelman WA, Dutch Stent-In Study Group. Premature closure of the Dutch Stent-in I study. Lancet. 2006;368(9547):1573–4.
van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RG, DeWitt JM, Donnellan F, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2014;46(11):990–1053.
Saito S, Yoshida S, Isayama H, Matsuzawa T, Kuwai T, Maetani I, et al. A prospective multicenter study on self-expandable metallic stents as a bridge to surgery for malignant colorectal obstruction in Japan: efficacy and safety in 312 patients. Surg Endosc. 2015 [Epub ahead of print].
van den Berg MW, Sloothaak DA, Dijkgraaf MG, van der Zaag ES, Bemelman WA, Tanis PJ, et al. Bridge-to-surgery stent placement versus emergency surgery for acute malignant colonic obstruction. Br J Surg. 2014;101(7):867–73.
Huang X, Lv B, Zhang S, Meng L. Preoperative colonic stents versus emergency surgery for acute left-sided malignant colonic obstruction: a meta-analysis. J Gastrointest Surg. 2014;18(3):584–91.
Morse BC, Simpson JP, Jones YR, Johnson BL, Knott BM, Kotrady JA. Determination of independent predictive factors for anastomotic leak: analysis of 682 intestinal anastomoses. Am J Surg. 2013;206(6):950–5.
Rho SY, Bae SU, Baek SJ, Hur H, Min BS, Baik SH, et al. Feasibility and safety of laparoscopic resection following stent insertion for obstructing left-sided colon cancer. J Korean Surg Soc. 2013;85(6):290–5.
Arai T, Sakon M, Fujii T, Sawano S, Nagano S, Umegaki M, et al. Efficacy of self-expanding metallic stent for right-sided colonic obstruction due to carcinoma before 1-stage laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2014;24(6):537–41.
Law WL, Poon JT, Fan JK, Lo OS. Colorectal resection after stent insertion for obstructing cancer: comparison between open and laparoscopic approaches. Surg Laparosc Endosc Percutan Tech. 2013;23(1):29–32.
Gorissen KJ, Tuynman JB, Fryer E, Wang L, Uberoi R, Jones OM, et al. Local recurrence after stenting for obstructing left-sided colonic cancer. Br J Surg. 2013;100(13):1805–9.
Sabbagh C, Browet F, Diouf M, Cosse C, Brehant O, Bartoli E, et al. Is stenting as “a bridge to surgery” an oncologically safe strategy for the management of acute, left-sided, malignant, colonic obstruction? A comparative study with a propensity score analysis. Ann Surg. 2013;258(1):107–15.
Liebig C, Ayala G, Wilks J, Verstovsek G, Liu H, Agarwal N, et al. Perineural invasion is an independent predictor of outcome in colorectal cancer. J Clin Oncol. 2009;27(31):5131–7.
Quah HM, Chou JF, Gonen M, Shia J, Schrag D, Landmann RG, et al. Identification of patients with high-risk stage II colon cancer for adjuvant therapy. Dis Colon Rectum. 2008;51(5):503–7.
Fujita S, Shimoda T, Yoshimura K, Yamamoto S, Akasu T, Moriya Y. Prospective evaluation of prognostic factors in patients with colorectal cancer undergoing curative resection. J Surg Oncol. 2003;84(3):127–31.
Maxwell P, Hamilton PW, Sloan JM. Three-dimensional reconstruction of perineural invasion in carcinoma of the extrahepatic bile ducts. J Pathol. 1996;180(2):142–5.
Acknowledgments
We thank all the medical staff who assisted in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Haraguchi, N., Ikeda, M., Miyake, M. et al. Colonic stenting as a bridge to surgery for obstructive colorectal cancer: advantages and disadvantages. Surg Today 46, 1310–1317 (2016). https://doi.org/10.1007/s00595-016-1333-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-016-1333-5