Abstract
Growth hormone/insulin-like growth factor (IGF) axis may play a role in maintaining glucose homeostasis in synergism with insulin. IGF-1 can directly stimulate glucose transport into the muscle through either IGF-1 or insulin/IGF-1 hybrid receptors. In severely decompensated diabetes including diabetic ketoacidosis, plasma levels of IGF-1 are low and insulin delivery into the portal system is required to normalize IGF-1 synthesis and bioavailability. Normalization of serum IGF-1 correlated with the improvement of glucose homeostasis during insulin therapy providing evidence for the use of IGF-1 as biomarker of metabolic control in diabetes. Taking apart the inherent mitogenic discussion, diabetes treatment using insulins with high affinity for the IGF-1 receptor may act as an endocrine pacer exerting a cardioprotective effect by restoring the right level of IGF-1 in bloodstream and target tissues, whereas insulins with low affinity for the IGF-1 receptor may lack this positive effect. An excessive and indirect stimulation of IGF-1 receptor due to sustained and chronic hyperinsulinemia over the therapeutic level required to overtake acute/chronic insulin resistance may act as endocrine disruptor as it may possibly increase the cardiovascular risk in the short and medium term and mitogenic/proliferative action in the long term. In conclusion, normal IGF-1 may be hypothesized to be a good marker of appropriate insulin treatment of the subject with diabetes and may integrate and make more robust the message coming from HbA1c in terms of prediction of cardiovascular risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a chronic illness that requires continuing medical care and ongoing patient self-management education and support to prevent acute complications and to reduce the risk of long-term complications [1]. Although therapeutic strategies of diabetes mellitus are manifold and attention to the problem is growing in the scientific community, the incidence of the disease is alarmingly increasing. In fact, approximately 360 million people had diabetes in 2011, of whom more than 95 % with type 2 diabetes. This number is estimated to increase to 552 million by 2030, and it is thought that about half of those will be unaware of their diagnosis [2, 3]. It is also estimated that about 300 million of people may have alteration of glucose metabolism such as impaired fasting glucose, glucose intolerance, both often referred as “prediabetes,” gestational diabetes and euglycemic insulin resistance [4, 5]. A total of 281 million men and 317 million women worldwide died with diabetes mellitus in 2011, most from cardiovascular diseases related to diabetes. The healthcare expenditure for diabetes in Europe was about 75 billion euros in 2011 and is projected to increase to 90 billions by 2030 [3]. In the USA, the estimated national cost of diabetes in 2012 was 245 billion dollars, of which 176 billions (72 %) representing direct healthcare expenditures attributed to diabetes [6]. Based on these epidemiological data, a first challenge is to prevent diabetes in the general population by implementing beneficial lifestyle interventions [7]. In patients with diabetes, however, the challenge for clinicians is to choose the best therapeutic approach which should be at the same time effective and safe (e.g., the possible association recently hypothesized of insulin exposure and cancer risk). As a matter of fact, type 2 diabetes is not just dysglycemia but a complex interplay of pathophysiological mechanisms which operate involving multiple organs. Management of this complexity is difficult because such interplay differs in each patient and reliable clinical and biochemical markers of individual diabetic phenotypes are still largely lacking [8, 9]. Moreover, there is also a need for new and precocious biomarkers able to identify early patients at risk to develop chronic and irreversible complications of diabetes.
Over the recent years, several studies have investigated the interplay existing between growth hormone (GH)/insulin-like growth factor-1 (IGF-1) axis and diabetes mellitus and its treatment. GH and IGF-I secretions are influenced by metabolic signals [10] and derangements of GH/IGF-1 axis may occur in patients with diabetes mellitus potentially influencing the response to anti-diabetic treatments and the outcome of disease [11, 12].
This review will deal with the physiology of insulin and GH/IGF-1 actions, the pathophysiological and clinical aspects correlated with the derangement of GH/IGF-1 axis in patients with diabetes mellitus with focus on the interplay between insulin and IGF-1 in modulating glucose metabolism and influencing cardiovascular and neoplastic risk of patients with diabetes.
Insulin central and peripheral actions: physiology and pathophysiology
Insulin is generally treated as a peripheral hormone controlling glucose metabolism and glucose transport in the liver and muscles. In reality, although glucose metabolism in the brain is largely non-insulin dependent, insulin may exert a relevant activity also in the central nervous system, where insulin receptors (IRs) are located. In fact, insulin crosses the blood–brain barrier with a carrier-mediated process by a specific transport system coupled to IRs in cerebral microvessels [13–17]. IR is a member of protein kinase receptor family that is composed of two α-subunits and two β-subunits which are linked by disulfide bonds. Binding of insulin to α-subunits eventually leads to the activation of tyrosine kinase activity and initiation of insulin actions [18]. Also the IGF-1 receptor (IGF-1R) is a tetrameric glycoprotein that belongs to the receptor tyrosine (Tyr) kinase superfamily. It is composed of two α (120–135 kDa) and two β (95 kDa) subunits [19–22]. Due to structural and functional homology, insulin and IGF-1 can bind to (and activate) both IR and IGF-1R [23].
Insulin can also be synthesized in specific areas of the brain in small quantities [24, 25]. Studies suggest that cerebral glucose metabolism may be controlled in part directly or indirectly by neuronal insulin/IR signaling pathways [26–30]. Insulin signaling in the brain limits food intake. In fact, insulin secretion over the long term may function as a negative feedback signal of recent energy intake and body adiposity [31]. Under supra-physiological glucose levels, brain insulin signaling activation could result in hyperpolarization of glucose-sensing neurons decreasing body weight [20, 32, 33]. Conversely, impairment of brain insulin signaling (as it occurs in peripheral insulin resistance) might promote a feedback inhibition of IR. This leads to increased body weight by the activation of arcuate neurons containing NPY, AgRP and GABA [20, 31, 32, 34]. Interestingly, long-term central insulin signaling on body weight in humans has been suggested to have sex-dependent results. In fact, it may cause weight loss in men and inducing increase in water storage and weight gain in women [35]. Insulin was also hypothesized to play a role in protecting the neurons from oxidative stress and apoptotic death [36, 37]. In type 2 diabetes, insulin resistance is accompanied by down-regulation of insulin transport into the brain. Consequently, decreased cerebral blood flow, impairment of oxidative glucose metabolism and possibly progressive impairment in learning, memory and cognition may occur [32, 38–42]. The effects exerted by insulin at the peripheral level are better known with respect to the central ones. Insulin binding to the IR regulates the uptake of glucose from the circulation by inducing the translocation of glucose transporters from the cytoplasm toward the plasma membrane [39, 40, 43]. Insulin promotes glucose uptake in fat and muscle tissue, stimulates glycogen synthesis in liver and muscle and hepatic and adipocyte lipogenesis, and inhibits hepatic glucose production and adipocyte lipolysis. Finally, insulin is also a growth factor which determines cell growth and inhibits cellular apoptosis via the Ras–Raf–mitogen-activated protein kinase signaling pathway [44–46]. The mechanism of insulin resistance involves only the metabolic pathway of insulin signaling and not the mitogenic pathway [47]. Several studies demonstrated that inappropriate fat accumulation in muscle cells or the release of inflammatory cytokines by fat cells may affect the GLUT-4 pathway [48–51]. When the adipose tissue cannot fulfill its normal storage and lipo-regulatory function, insulin action could be compromised and insulin resistance may develop [48, 52–55].
GH/IGF-1 axis and insulin in physiology
Growth hormone is produced and secreted by somatotropes in the anterior pituitary in a pulsatile manner, mainly under hypothalamic control. The hypothalamic factors involved in GH regulation include GH-releasing hormone and somatostatin, which stimulate and inhibit secretion, respectively [10]. In addition to classic and non-classic hypothalamic peptides, many other neuropeptides (such as galanin), neurotransmitters (e.g., acetylcholine), metabolic signals (such as hypoglycemia, amino acids and free fatty acids) and peripheral hormones (e.g., IGF-1, thyroid and sex hormones and glucocorticoids) are involved in the modulation of GH secretion [56–61]. GH acts by inducing the synthesis of IGF-1 in the liver [10]. IGF-1 is a peptide hormone that shares nearly 50 % amino acid sequence homology with proinsulin, and, like insulin, is composed of an alpha and a beta chain connected by disulfide bonds [62]. Besides GH, the liver synthesis of IGF-1 is regulated by insulin. Studies in vitro demonstrated that insulin stimulates IGF-1 synthesis by hepatocytes in the absence of GH and the effects of insulin are additive to those of GH by increasing liver GH receptors and acting at post-receptor level [63].
The physiology of IGF-1 is complex because it acts as a circulating hormone and as a local growth factor [64]. In contrast to insulin, which is largely unbound to any transport molecules, as much as 99 % of IGF-I in circulation is bound to one of the six IGF-binding proteins (IGFBPs), mainly IGFBP-3 and IGFBP-5 [65]. Under normal circumstances, IGFBP-3 and IGFBP-5 are saturated. Therefore, abrupt changes in IGFBP-1 and IGFBP-2 that are not saturated and that occur as a result of changes in either nutrient intake or insulin secretion can result in major changes in free IGF-I and thereby regulate tissue responsiveness [66]. Indeed, insulin down regulates the synthesis of IGFBP-1, IGFBP-2, and, although to a lesser extent, IGFBP-3 from the liver leading to an increase in free IGF-1. From this point of view, insulin increases both synthesis and bioavailability of IGF-1.
IGF-1R and IR show 48 % amino acid sequence homology [67]. Despite these similarities, the ligand-binding specificity is strict. The affinity for the IGF-1R is 1,000 times greater for IGF-1 than for insulin, and the IR has a 100-fold greater affinity for insulin as compared to IGF-1 [68]. Upon ligand binding, the IGF-1R dimerizes and undergoes auto-phosphorylation, leading to the activation of the insulin receptor substrate (IRS)-1 and IRS-2, with the latter being more preferentially activated by IGF-1 after interaction with its receptor [69, 70]. Given the high degree of homology, the insulin and IGF-1 half-receptors (composed of one α- and one β-subunit) can heterodimerize, leading to the formation of insulin/IGF-1 hybrid receptors (hybrid-Rs) which in many tissues are the most represented receptor subtypes [71–74]. The human IR exists in two isoforms (IR-A and IR-B), generated by alternative splicing of the insulin receptor gene that either excludes or includes 12 amino acid residues encoded by a small exon (exon 11) at the carboxyl terminus of the IR α-subunit. Predominant IR-A expression in cells coexpressing the IGF-1R leads to an increased formation of hybrid-Rs, which up-regulate the IGF system binding with high affinity by both IGF-1 and IGF-2, and activation of the IGF-1R pathway also after insulin binding [75]. In contrast, predominant IR-B expression leads to high-binding specificity whereby insulin activates only its own receptor and post-receptor signaling. Indeed, IR-B is the classical receptor for metabolic effects of insulin in muscle, liver and adipose tissues.
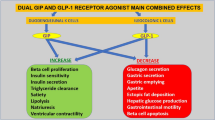
Growth hormone/IGF axis may play a role in maintaining glucose homeostasis in synergism with insulin. IGF-1R is expressed in skeletal muscle [76, 77] and IGF-1 was shown to promote glucose uptake in this tissue [78–83]. IGF-1 can directly stimulate glucose transport into the muscle through either IGF-1 or insulin/IGF-1 hybrid-R [84, 85], although this requires high concentrations of free IGF-1. The GH/IGF-1 axis may also affect lipid metabolism. Specifically, IGF-1 may have insulin-like effects in promoting the uptake of free fatty acids mainly in muscle, whereas at physiological concentration, IGF-1 does not exert direct effects on mature adipocytes. By contrast, GH has direct effects on mature adipocytes that result in stimulation of lipolysis with the release of free fatty acids following triglyceride breakdown [86]. Under physiologic conditions, therefore, it has been hypothesized that IGF-1 might influence glucose homeostasis largely through its insulin-like effects on muscle. After a meal, there is a significant increase in free IGF-1 via an insulin-induced suppression of IGFBP-1 secretion [68]. The IGFBP-1 gene is transcriptionally regulated by insulin; thus, the meal-induced increase in insulin leads to an increase in free IGF-1. This change may be adequate to stimulate fatty acid oxidation in muscle and suppress GH, and these changes may occur at physiologic IGF-1 levels.
GH/IGF-1 axis in diabetes mellitus
The GH/IGF-I axis is variably deranged in patients with diabetes mellitus. In type 1 diabetes, spontaneous and stimulated GH secretion is increased with reduced GH auto-feedback [87, 88] as effect of an impairment of somatostatin tone [89] likely due to a reduced GABA-ergic stimulation at the hypothalamic level [90]. Conversely, serum IGF-1 remains within the low range of healthy age-matched controls reflecting a state of hepatic GH resistance, as already described in other clinical conditions such as renal and heart failure [11, 91], likely due to an insufficient portal delivery of insulin to the liver [92]. Indeed, in type 1 diabetes IGF-1 bioavailability is low because IGFBP-1 production by the liver is increased due to insulin deprivation. The low IGF-1 availability contributes to sustain the relative GH hypersecretion due to the lack of the feedback negative signal at the hypothalamus–pituitary axis [93]. In type 2 diabetes, chronic hyperglycemia in the presence of normal or increased insulin causes an increase in hypothalamic somatostatin tone with consequent impairment of GH secretion [94]. In this clinical context, IGF-1 values are variable in relationship with different degrees of insulin resistance and pancreatic beta cell dysfunction which reduce the ability of insulin to suppress IGFBP-1 synthesis by the liver [95].
Abnormalities of GH/IGF-1 axis in diabetes mellitus: clinical implications
The main challenge in the treatment of diabetes is represented by the prevention of microvascular and macrovascular complications in order to reduce morbidity, mortality, disability and costs [96]. For many years, a strict glycemic control has been considered the most important method to achieve sustained reduction in the occurrence of diabetic complications, even if recent intervention trials have given questionable results for macrovascular complications, especially when very tight diabetes control was pursued. HbA1c is usually used to estimate glycemic control, since this biomarker correlates very well with mean glucose levels. Intervention trials have shown that the closer HbA1c is to normal values, the better is the prevention of the microvascular complications. Even if the reduction of HbA1c to 7 % has been seen associated with a reduction in the development of macrovascular complications, an additional reduction in these complications was not achieved with a tighter glycemic control [96]. This suggests that other mechanisms and biomarkers should be taken into account in the prevention of macrovascular complications. Among them, post-prandial glycemia, glycemic variability, hypoglycemias, the so-called metabolic memory, other metabolic and vascular risk factors, such as lipids and hypertension which can play a major role [97, 98]. However, we hypothesize that also abnormalities of the GH/IGF-1 axis may play a role and that low-circulating IGF-1 may be an interesting marker of cardiovascular risk in type 2 diabetes.
In fact, low IGF-1 secretion and availability contribute to insulin resistance in diabetes [99], consistently with the experimental evidence that animals with the absence of liver-specific IGF-1 gene are characterized by hyperinsulinemia and skeletal muscle insulin resistance [100]. The mechanisms underlying the association between low IGF-1 and insulin resistance are largely unknown, but it could be hypothesized that the increase in GH secretion, consequent to the loss of IGF-1 feedback signal, may play an important role in favoring the persistence of insulin resistance [100]. Indeed, the augmented GH secretion, which occurs in patients with type 1 diabetes, may also contribute in the development of late diabetic complications, such as diabetic nephropathy and retinopathy [10, 11, 101]. This latter complication is also favored by the low IGF-1 synthesis and availability [102]. In fact, IGF-1 is essential for normal retinal vascular development and maintenance [103], and the hypoinsulinemia-induced IGF-1 deficiency of diabetes impairs pericyte replication, regeneration and survival with consequent loss of pericytes. This latter abnormality is the first morphological finding in diabetic retinopathy [104]. However, when serum IGF-1 values are restored by treatment of diabetes, neovascularization is favored and progression of retinopathy may occur [102].
IGF-1 was shown to exert mitogenic actions on vascular system, including stimulation of vascular smooth muscle cell proliferation and migration [105–107], which may prompt to the formation of atherosclerotic plaques supporting the hypothesis of a detrimental role of IGF-I in the development of cardiovascular disease [108]. More recently, however, the balance of experimental and clinical evidence appeared to contradict this view and several studies have clarified that IGF-1 may be instead a vascular protective factor, by several effects on the endothelial cells. In fact, IGF-1 stimulates nitric oxide production from endothelial cells, induces vasodilatation through the activation of potassium channels, with a consequent reduction in intracellular calcium [109], protects against plaque instability and ruptures by counteracting oxidized LDL-induced cytotoxicity and vascular smooth muscle cell apoptosis [108]. Consistently with these concepts, low-circulating IGF-1 has been associated with angiographically documented coronary artery disease [110, 111] and carotid intima-media thickness, a recognized surrogate marker for subclinical atherosclerosis [112]. This association was also demonstrated for patients with diabetes mellitus [108]. In patients with diabetes mellitus with a polymorphism in the promoter region of the IGF-1 gene creating an environment of chronic exposure to low IGF-1 levels, the risk of myocardial infarction was about threefold increased as compared to the patients harboring the wild-type allele [113]. Moreover, in patients with diabetes experiencing an acute myocardial infarction, high IGFBP-1, that is the expression of low IGF-1 availability, was shown to be associated with increased risk for cardiovascular mortality and morbidity [114]. Therefore, it is intriguing to hypothesize that one of the targets of the treatment of diabetes should be the normalization of circulating IGF-1. As for GH-deficient subjects, an IGF-1 level in the low-normal range for age should probably be safely targeted [115]. In fact, also a sustained increase in circulating IGF-1 such as found in untreated acromegaly may be linked to not only increased oncological but even cardiovascular risk [116, 117].
Abnormalities of GH/IGF-1 axis in diabetes mellitus: effects of insulin therapy
It is still uncertain whether the metabolic control in diabetes may have per se an impact on the IGF system. In severely decompensated diabetes including diabetic ketoacidosis, plasma levels of IGF-1 were low [118]. By contrast, other studies did not demonstrate any significant correlation between HbA1c and IGF-1 [119–121].
Insulin delivery into the portal system is required to normalize IGF-1 synthesis and bioavailability. In fact, serum free IGF-1 tends to normalize rapidly after starting insulin therapy, whereas normalization of total IGF-1 was shown to require several weeks to occur [122]. Consistently with the concept that IGF-1 synthesis and bioavailability are influenced by intraportal insulin delivery, intraperitoneal insulin administration was shown to be more effective than subcutaneous route in normalizing the alterations of IGF-1 system in type 1 diabetes [121]. It is noteworthy that normalization of serum IGF-1, accompanied by a decrease in serum IGFBP-1, was shown to be closely correlated with the improvement of glucose homeostasis during insulin therapy providing evidence for the use of IGF-1 and IGFBP-1 as biomarkers of metabolic control in diabetes [123].
In addition to the effects on IGF synthesis and bioavailability, exogenous insulin may also activate IGF-1 signal in target tissues although, at physiological concentrations, little receptor cross talk occurs [124]. Another consequence of the structural homology of IR and IGF-1R is the formation of hybrid receptors which are highly expressed in patients with diabetes [125–130] and behave like full IGF-1R with regard to binding affinities for IGF-1 and insulin, as well as downstream signaling [131]. It is noteworthy that insulin analogs used in the clinical practice, such as insulin glargine, may have higher affinity for IGF-IR and hybrid receptors as compared to native insulin with potential promitogenic effects of these drugs [132, 133]. Preclinical studies showed that insulin glargine increases resistance to apoptosis in several tumor cell lines including colorectal, breast and prostate cancers [134], although the affinity of insulin analogs for IGF-1R was shown to be much lower than that of native IGF-1 [135]. The clinical relevance of these in vitro data is still uncertain. Although some studies reported an overall increased cancer risk associated with high doses of insulin glargine [136, 137], at the current time there is still inconclusive evidence to support the hypothesis that insulin glargine at physiological doses may increase the risk of tumors in clinical practice [138–140]. Notably, there are available new insulin analogs that, unlike insulin glargine, showed lower IGF-1R binding affinity and a low mitogenic/metabolic potency ratio [141–144].
Each insulin analog has an own affinity for IR, when compared to human “regular” insulin [145]. In addition, in vitro each analog has shown a specific affinity for IGF-1R and accordingly a different mitogenic power [145]. Insulin glargine in vitro showed an affinity for IGF-1R sixfold higher than that of human insulin, while other analogs had affinities for IGF-1R similar or even lower than those of the insulin reference. In addition, glargine showed in vitro a mitogenic power about eightfold greater than human insulin. Therefore, it has been hypothesized that glargine may increase cancer risk because of its IGF-1R affinity and mitogenic power. Really, several subsequent clinical studies did not confirm these data, and a specific large randomized controlled trial, designed to test cardiovascular and cancer risk of glargine, did not show any increase in cancer risk in patients treated with glargine [146]. This has been confirmed by other several large studies [147–149]. In particular, the use of glargine was not associated with either an increased mortality for cancer [147] or a higher incidence of malignancies [148, 149].
These results may be easily explained by the fact that after the subcutaneous administration of glargine, the real exposure to glargine is marginal, even at supra-therapeutic doses, as glargine is quickly processed to the so-called Metabolite 1 (M1), which mediates all metabolic effects of glargine [150]. There is another metabolite, called Metabolite 2 (M2), which is not virtually present in plasma. It is important to remember that both M1 and M2 have even lower binding to IGF-1R and less mitogenic potential when compared to human “regular” insulin [151].
Therefore, it is unlikely that glargine U100 or U300 (slow release from injection site depot) or other insulins such as detemir or degludec (acylated insulin and plasma albumin bound based mechanism of action) or human insulin [152] can increase in vivo mitogenesis. However, two considerations should be made: All insulins can exert an action on IGF-1R, albeit with different affinities, and this effect may be even positive. Indeed, it may promote all effects of IGF-1 that are decreased in diabetes. Therefore, therapy in diabetes with insulin with high affinity for the IGF-1R may exert a cardioprotective effect by restoring the right level of IGF-1 in bloodstream and target tissues, whereas insulins with low affinity for the IGF-1R may lack this positive effect. Furthermore, an excessive and indirect stimulation of IGF-1R due to sustained and chronic hyperinsulinemia (therefore likely not due to a specific insulin), over the therapeutic level required to overtake an acute/chronic insulin resistance status (what we can call the “individual critical threshold”), may be deleterious as it may increase the cardiovascular risk in the short and medium term and mitogenic/proliferative action in the long term.
Treatment of diabetes with IGF-1
Exogenous IGF-1 administration was shown to reduce serum glucose levels in healthy individuals as well as in patients with insulin resistance, type 1 and type 2 diabetes [78, 82, 153–163]. Interestingly, IGF-1-induced reduction in serum glucose levels was accompanied by an improvement in insulin sensitivity [156, 162, 163]. These studies provide indirect evidence that relatively high endogenous levels of IGF-1 may reduce insulin resistance and, thereby, lower the risk of type 2 diabetes. The predominant effect of IGF-1 on carbohydrate metabolism seems to be secondary to its effects on lipid metabolism. Because suppression of insulin and GH secretion occurs at pharmacologic levels of IGF-1, it is difficult to extrapolate from the results of most published studies and conclude that these effects can occur at normal physiologic levels. However, GH suppression would be expected to lead to decreased free fatty acid flux in liver and reduced antagonism of insulin action on gluconeogenesis [68].
Although most of the effects of IGF-1 on glucose homeostasis are mediated by its action on IR pathways, there is also evidence that IGF-1 may directly act on the endocrine pancreas variably influencing β-cells survival, replication and hormonal synthesis as well as suppressing glucagon [164–175]. Several attempts of administration of IGF-1 in patients with diabetes have been made, both in type 1 and type 2 diabetes, with the aim of a metabolic improvement of the disease. In general, in type 1 diabetes HbA1c was improved and insulin requirements were decreased accompanied by an enhanced insulin sensitivity, the latter effect due to the action of IGF-1 per se rather than by the reduction of GH values [176–178]. In type 2 diabetes, IGF-1 administration enhanced insulin sensitivity with decreases in glucose, endogenous insulin, C-peptide secretion and, in some cases, an improved area under the curve after oral glucose administration [160, 179, 180]. As most of the patients studied were obese with low GH concentrations, it is highly likely that the enhanced insulin sensitivity was caused by an effect on free fatty acid metabolism in muscle and by a suppression of renal gluconeogenesis and not simply by suppression of GH secretion [68].
Perspectives
The GH/IGF-1 axis is regulated in a complex manner by the metabolic alterations occurring in diabetes mellitus and is very sensitive to changes in endocrine milieu determined by insulin treatment. Particularly, in decompensated diabetes, IGF-1 levels are low and insulin administration may have beneficial effects by acting at the IGF-1R level. Different affinities for this latter receptor may lead to variable degrees of IGF-1 restoration with different insulin preparations. From lessons learned in GHD and acromegaly patients [115–117], we now know that both very low and high IGF-1 levels are related to increased cardiovascular risk. Therefore, insulin may be considered an endocrine pacer of the GH/IGF-1 axis in diabetes and restored-to-normal IGF-1 may be hypothesized to be a good marker of appropriate insulin treatment of the subject and may integrate and make more robust the message coming from HbA1c in terms of prediction of cardiovascular risk. We expect that in near future, a diabetes clinical research focus will challenge the superiority or non-inferiority of new insulin analogs and of their biosimilars, back-grounding on their specific mechanism of action [149], on combined biochemical end points including HbA1c, GH and IGF-1 in each personalized treatment at same fixed stage points. In fact, we need to focus on the concept that exogenous insulins or incretins, directly or indirectly, may exert their either metabolic or proliferative effects with different magnitude, and therefore act as either endocrine pacers or disruptors, in the same people with diabetes who during their lifecycle physiologically undergo relevant changes in the hormonal status [181]. A new era in the approach to monitoring diabetes treatment can start not only by measuring HBA1c or glucose circadian fluctuations [182, 183] but also by evaluating the impact of personalized treatment of diabetes on the ancestral balance between metabolic and proliferative effect of the integrated system constituted by insulin, GH and IGF-1 in the circulation and at the tissue level.
References
WHO Consultation (1999) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Geneva: World Health Organization; Report no. 99.2. http://whqlibdoc.who.int/hq/1999/who_ncd_ncs_99.2.pdf
ESC (2013) Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 34:3035–3087
International Diabetes Federation (2011) Global burden: prevalence and projections, 2011 and 2030. http://www.diabetesatlas.org/content/diabetes-and-impairedglucose-tolerance
Bergman M (2013) Inadequacies of current approaches to prediabetes and diabetes prevention. Endocrine 44:623–633
Bergman M (2013) Pathophysiology of prediabetes and treatment implications for the prevention of type 2 diabetes mellitus. Endocrine 43:504–513
American Diabetes Association (2013) Economic costs of diabetes in the U.S. in 2012. Diabetes Care 36:1033–1046
Esposito K, Giugliano D (2014) Healthy lifestyle for metabolic health: no more excuse! Endocrine 46:176–178
Maddaloni E, Pozzilli P (2014) SMART diabetes: the way to go (safe and multifactorial approach to reduce the risk for therapy in diabetes). Endocrine 46:3–5
Esposito K, Maiorino MI, Bellastella G, Giugliano D (2014) New guidelines for metabolic targets in diabetes: clinician’s opinion does matter. Endocrine. doi:10.1007/s12020-014-0205-2
Giustina A, Veldhuis JD (1998) Pathophysiology of the neuroregulation of growth hormone secretion in experimental animals and the human. Endocr Rev 19:717–797
Kamenický P, Mazziotti G, Lombès M, Giustina A, Chanson P (2014) Growth hormone, insulin-like growth factor-1, and the kidney: pathophysiological and clinical implications. Endocr Rev 35:234–281
Rajpathak SN, Gunter MJ, Wylie-Rosett J, Ho GY, Kaplan RC, Muzumdar R, Rohan TE, Strickler HD (2009) The role of insulin-like growth factor-I and its binding proteins in glucose homeostasis and type 2 diabetes. Diabetes Metab Res Rev 25:3–12
Woods SC, Porte D Jr (1977) Relationship between plasma and cerebrospinal fluid insulin levels of dogs. Am J Physiol 233:331–334
Banks WB (2004) The source of cerebral insulin. Eur J Pharmacol 490:5–12
Ghasemi R, Haeri A, Dargahi L, Mohamed Z, Ahmadiani A (2013) Insulin in the brain: sources, localization and functions. Mol Neurobiol 47:145–171
Havrankova J, Schmechel D, Roth J, Brownstein M (1978) Identification of insulin in rat brain. Proc Natl Acad Sci USA 75:5737–5741
Duarte AI, Moreira PI, Oliveira CR (2012) Insulin in central nervous system: more than just a peripheral hormone. J Aging Res 2012:384017
LeRoith D, Lowe WL Jr, Shemer J, Raizada MK, Ota A (1988) Development of brain insulin receptors. Int J Biochem 20:225–230
Schlessinger J (2000) Cell signaling by receptor tyrosine kinases. Cell 103:211–225
Wada A, Yokoo H, Yanagita T, Kobayashi H (2005) New twist on neuronal insulin receptor signaling in health, disease, and therapeutics. J Pharmacol Sci 99:128–143
Brummer T, Schmitz-Peiffer C, Daly RJ (2010) Docking proteins. FEBS J 277:4356–4369
Boura-Halfon S, Zick Y (2009) Chapter 12 serine kinases of insulin receptor substrate proteins. In: Gerald L (ed) Vitamins and hormones, vol 80. Academic, London, pp 313–349
Banks WA, Kastin AJ (1988) Differential permeability of the blood-brain barrier to two pancreatic peptides: insulin and amylin. Peptides 19:883–889
Clarke DW, Mudd L, Boyd FT Jr (1986) Insulin is released from rat brain neuronal cells in culture. J Neurochem 47:831–836
Hoyer S (2003) Memory function and brain glucose metabolism. Pharmacopsychiatry 36:S62–S67
Zhao W, Chen H, Xu H, Moore E, Meiri N, Quon MJ, Alkon DL (1999) Brain insulin receptors and spatial memory. Correlated changes in gene expression, tyrosine phosphorylation, and signaling molecules in the hippocampus of water maze trained rats. J Biol Chem 274:34893–34902
Bingham EM, Hopkins D, Smith D, Pernet A, Hallett W, Reed L, Marsden PK, Amiel SA (2002) The role of insulin in human brain glucose metabolism: an 18fluoro-deoxyglucose positron emission tomography study. Diabetes 51:3384–3390
Schulingkamp RJ, Pagano TC, Hung D, Raffa RB (2000) Insulin receptors and insulin action in the brain: review and clinical implications. Neurosci Biobehav Rev 24:855–872
McCall AL (2004) Cerebral glucose metabolism in diabetes mellitus. Eur J Pharmacol 490:147–158
Ghosh A, Yuk YC, Mansfield BC, Chou JY (2005) Brain contains a functional glucose-6-phosphatase complex capable of endogenous glucose production. J Biol Chem 280:11114–11119
Giustina A, Braunstein G (2014) Hypothalamic syndromes. In: Jameson L, De Groot L (eds) Endocrinology: adult and pediatric, 7th edn. Elsevier, Philadelphia (in press)
Plum L, Belgardt BF, Brüning JC (2006) Central insulin action in energy and glucose homeostasis. J Clin Invest 116:1761–1766
Levin BE (2006) Metabolic sensing neurons and the control of energy homeostasis. Physiol Behav 89:486–489
Morton GJ, Cummings DE, Baskin DG, Barsh GS, Schwartz MW (2006) Central nervous system control of food intake and body weight. Nature 443:289–295
Havel PJ (2001) Peripheral signals conveying metabolic information to the brain: short-term and long-term regulation of food intake and energy homeostasis. Exp Biol Med 226(11):963–977
Fulop T, Larbi A, Douziech N (2003) Insulin receptor and ageing. Pathol Biol 51:574–580
Duarte AI, Santos MS, Oliveira CR, Rego AC (2005) Insulin neuroprotection against oxidative stress in cortical neurons—involvement of uric acid and glutathione antioxidant defenses. Free Rad Biol Med 39:876–889
Craft S (2005) Insulin resistance syndrome and Alzheimer’s disease: age- and obesity-related effects on memory, amyloid, and inflammation. Neurobiol Aging 26:S65–S69
Ristow M (2004) Neurodegenerative disorders associated with diabetes mellitus. J Mol Med 82:510–529
Watson GS, Craft S (2004) Modulation of memory by insulin and glucose: neuropsychological observations in Alzheimer’s disease. Eur J Pharmacol 490:97–113
Piroli GG, Grillo CA, Charron MJ, McEwen BS, Reagan LP (2004) Biphasic effects of stress upon GLUT8 glucose transporter expression and trafficking in the diabetic rat hippocampus. Brain Res 1006:28–35
Mayer G, Nitsch R, Hoyer S (1990) Effects of changes in peripheral and cerebral glucose metabolism on locomotor activity, learning and memory in adult male rats. Brain Res 532:95–100
Saltiel AR, Pessin JE (2002) Insulin signaling pathways in time and space. Trends Cell Biol 12:65–71
Medema RH, de Vries-Smits AM, van der Zon GC, Maassen JA, Bos JL (1993) Ras activation by insulin and epidermal growth factor through enhanced exchange of guanine nucleotides on p21ras. Mol Cell Biol 13:155–162
Goalstone M, Carel K, Leitner JW, Draznin B (1997) Insulin stimulates the phosphorylation and activity of farnesyltransferase via the Ras-mitogen-activated protein kinase pathway. Endocrinology 138:5119–5124
Shulman GI (2000) Cellular mechanisms of insulin resistance. J Clin Invest 106:171–176
Draznin B (2010) Mitogenic action of insulin: friend, foe or ‘frenemy’? Diabetologia 53:229–233
Tsatsoulis A, Mantzaris MD, Bellou S, Andrikoula M (2013) Insulin resistance: an adaptive mechanism becomes maladaptive in the current environment—an evolutionary perspective. Metabolism 62:622–633
Schenk S, Saberi M, Olefsky JM (2008) Insulin sensitivity: modulation by nutrients and inflammation. J Clin Invest 118:2992–3002
Hotamisligil GS (2006) Inflammation and metabolic disorders. Nature 444:860–867
Savage DB, Petersen KF, Shulman GI (2007) Disordered lipid metabolism and the pathogenesis of insulin resistance. Physiol Rev 87:507–520
Unger RH, Scherer PE (2010) Gluttony, sloth and the metabolic syndrome: a roadmap to lipotoxicity. Trends Endocrinol Metab 21:345–352
Sims EA, Danforth E Jr, Horton ES, Bray GA, Glennon JA, Salans LB (1973) Endocrine and metabolic effects of experimental obesity in man. Recent Prog Horm Res 29:457–496
Garg A, Misra A (2004) Lipodystrophies: rare disorders causing metabolic syndrome. Endocrinol Metab Clin N Am 33:305–331
Heilbronn LK, Gan SK, Turner N, Campbell LV, Chisholm DJ (2007) Markers of mitochondrial biogenesis and metabolism are lower in overweight and obese insulin-resistant subjects. J Clin Endocrinol Metab 92:1467–1473
Giustina A, Licini M, Schettino M, Doga M, Pizzocolo G, Negro-Vilar A (1994) Physiological role of galanin in the regulation of anterior pituitary function in humans. Am J Physiol 266:E57–E61
Giustina A, Girelli A, Alberti D, Bossoni S, Buzi F, Doga M, Schettino M, Wehrenberg WB (1991) Effects of pyridostigmine on spontaneous and growth hormone-releasing hormone stimulated growth hormone secretion in children on daily glucocorticoid therapy after liver transplantation. Clin Endocrinol 35:491–498
Giustina A, Bossoni S, Bodini C, Girelli A, Balestrieri GP, Pizzocolo G, Wehrenberg WB (1992) Arginine normalizes the growth hormone (GH) response to GH-releasing hormone in adult patients receiving chronic daily immunosuppressive glucocorticoid therapy. J Clin Endocrinol Metab 74:1301–1305
Giustina A, Wehrenberg WB (1995) Influence of thyroid hormones on the regulation of growth hormone secretion. Eur J Endocrinol 133:646–653
Wehrenberg WB, Giustina A (1992) Basic counterpoint: mechanisms and pathways of gonadal steroid modulation of growth hormone secretion. Endocr Rev 13:299–308
Mazziotti G, Giustina A (2013) Glucocorticoids and the regulation of growth hormone secretion. Nat Rev Endocrinol 9:265–276
Rinderknecht E, Humbel RE (1978) The amino acid sequence of human insulin-like growth factor I and its structural homology with proinsulin. J Biol Chem 253:2769–2776
Böni-Schnetzler M, Schmid C, Meier PJ, Froesch ER (1991) Insulin regulates insulin-like growth factor I mRNA in rat hepatocytes. Am J Physiol 260:E846–E851
Giustina A, Mazziotti G, Canalis E (2008) Growth hormone, insulin-like growth factors, and the skeleton. Endocr Rev 29:535–559
Juul A (2003) Serum levels of insulin-like growth factor I and its binding proteins in health and disease. Growth Horm IGF Res 13:113–170
Janssen JA, Lamberts SW (1999) Is the measurement of free IGF-I more indicative than that of total IGF-I in the evaluation of the biological activity of the GH/IGF-I axis? J Endocrinol Invest 22:313–315
Ullrich A, Gray A, Tam AW et al (1986) Insulin-like growth factor I receptor primary structure: comparison with insulin receptor suggests structural determinants that define functional specificity. EMBO J 5:2503–2512
Clemmons D (2012) Metabolic actions of insulin-like growth factor-I in normal physiology and diabetes. Endocrinol Metab Clin N Am 41:425–443
Kim JJ, Accili D (2002) Signalling through IGF-I and insulin receptors: where is the specificity? Growth Horm IGF Res 12:84–90
Zapf J, Schmid C, Froesch ER (1984) Biological and immunological properties of insulin-like growth factors (IGF) I and II. Clin Endocrinol Metab 13:3–30
Soos MA, Whittaker J, Lammers R, Ullrich A, Siddle K (1990) Receptors for insulin and insulin-like growth factor-I can form hybrid dimers. characterisation of hybrid receptors in transfected cells. Biochem J 270:383–390
Kasuya J, Paz IB, Maddux BA, Goldfine ID, Hefta SA, Fujita-Yamaguchi Y (1993) Characterization of human placental insulin-like growth factor-I/insulin hybrid receptors by protein microsequencing and purification. Biochemistry 32:13531–13536
Seely BL, Reichart DR, Takata Y, Yip C, Olefsky JM (1995) A functional assessment of insulin/insulin-like growth factor-I hybrid receptors. Endocrinology 136:1635–1641
Bailyes EM, Nave BT, Soos MA, Orr SR, Hayward AC, Siddle K (1997) Insulin receptor/IGF-I receptor hybrids are widely distributed in mammalian tissues: quantification of individual receptor species by selective immunoprecipitation and immunoblotting. Biochem J 327:209–215
Pandini G, Frasca F, Mineo R, Sciacca L, Vigneri R, Belfiore A (2002) Insulin/insulin-like growth factor I hybrid receptors have different biological characteristics depending on the insulin receptor isoform involved. J Biol Chem 277:39684–39695
LeRoith D, Werner H, Beitner-Johnson D, Roberts CT Jr (1995) Molecular and cellular aspects of the insulin-like growth factor I receptor. Endocr Rev 16:143–163
Alexandrides T, Moses AC, Smith RJ (1989) Developmental expression of receptors for insulin, insulin-like growth factor I (IGF-I), and IGF-II in rat skeletal muscle. Endocrinology 124:1064–1076
Russell-Jones DL, Bates AT, Umpleby AM et al (1995) A comparison of the effects of IGF-I and insulin on glucose metabolism, fat metabolism and the cardiovascular system in normal human volunteers. Eur J Clin Invest 25:403–411
Boulware SD, Tamborlane WV, Rennert NJ, Gesundheit N, Sherwin RS (1994) Comparison of the metabolic effects of recombinant human insulin-like growth factor-I and insulin. Dose-response relationships in healthy young and middle-aged. J Clin Invest 93:1131–1139
Elahi D, McAloon-Dyke M, Fukagawa NK et al (1993) Effects of recombinant human IGF-I on glucose and leucine kinetics in men. Am J Physiol 265:E831–E838
Laager R, Ninnis R, Keller U (1993) Comparison of the effects of recombinant human insulin-like growth factor-I and insulin on glucose and leucine kinetics in humans. J Clin Invest 92:1903–1909
Guler HP, Zapf J, Froesch ER (1987) Short-term metabolic effects of recombinant human insulin-like growth factor I in healthy adults. N Engl J Med 317:137–140
Frystyk J, Grofte T, Skjaerbaek C, Orskov H (1997) The effect of oral glucose on serum free insulin-like growth factor-I and -II in health adults. J Clin Endocrinol Metab 82:3124–3127
Furling D, Marette A, Puymirat J (1999) Insulin-like growth factor I circumvents defective insulin action in human myotonic dystrophy skeletal cells. Endocrinology 140:4244–4250
Henry RR, Abrams L, Nikoulina S, Ciaraldi TP (1995) Insulin action and glucose metabolism in nondiabetic control and NIDDM subjects. Diabetes 44:936–946
DiGirolamo M, Eden S, Enberg O, Isaksson O, Lönnroth P, Hall K, Smith U (1986) Specific binding of human growth hormone but not insulin-like growth factors by human adipocytes. FEBS Lett 205:15–19
Giustina A, Bossoni S, Cimino A, Pizzocolo G, Romanelli G, Wehrenberg WB (1990) Impaired growth hormone (GH) response to pyridostigmine in type 1 diabetic patients with exaggerated GH-releasing hormone-stimulated GH secretion. J Clin Endocrinol Metab 71:1486–1490
Giustina A, Bossoni S, Bodini C, Cimino A, Pizzocolo G, Schettino M, Wehrenberg WB (1991) Effects of exogenous growth hormone pretreatment on the pituitary growth hormone response to growth hormone-releasing hormone alone or in combination with pyridostigmine in type I diabetic patients. Acta Endocrinol 125:510–517
Giustina A, Desenzani P, Perini P, Deghenghi R, Bugari G, Wehrenberg WB, Giustina G (1996) Hypothalamic control of growth hormone (GH) secretion in type I diabetic men: effect of the combined administration of GH-releasing hormone and hexarelin, a novel GHRP-6 analog. Endocr Res 22:159–174
Giustina A, Desenzani P, Perini P, Bazzigaluppi E, Bodini C, Bossoni S, Poiesi C, Wehrenberg WB, Bosi E (1997) Glutamate decarboxylase autoimmunity and growth hormone secretion in type I diabetes mellitus. Metabolism 46:382–387
Giustina A, Lorusso R, Borghetti V, Bugari G, Misitano V, Alfieri O (1996) Impaired spontaneous growth hormone secretion in severe dilated cardiomyopathy. Am Heart J 131:620–622
Bereket A, Lang CH, Wilson TA (1999) Alterations in the growth hormone-insulin-like growth factor axis in insulin dependent diabetes mellitus. Horm Metab Res 31:172–181
Giustina A, Wehrenberg WB (1994) Growth hormone neuroregulation in diabetes mellitus. Trends Endocrinol Metab 5:73–78
Giustina A, Bresciani E, Tassi C, Girelli A, Valentini U (1994) Effect of pyridostigmine on the growth hormone response to growth hormone-releasing hormone in lean and obese type II diabetic patients. Metabolism 43:893–898
Friedrich N, Thuesen B, Jørgensen T, Juul A, Spielhagen C, Wallaschofksi H, Linneberg A (2012) The association between IGF-I and insulin resistance: a general population study in Danish adults. Diabetes Care 35:768–773
Singh A, Donnino R, Weintraub H, Schwartzbard A (2013) Effect of strict glycemic control in patients with diabetes mellitus on frequency of macrovascular events. Am J Cardiol 112:1033–1038
Bianchi C, Miccoli R, Del Prato S (2013) Hyperglycemia and vascular metabolic memory: truth or fiction? Curr Diab Rep 13:403–410
Johnson EL (2012) Glycemic variability in type 2 diabetes mellitus: oxidative stress and macrovascular complications. Adv Exp Med Biol 771:139–154
Sesti G, Sciacqua A, Cardellini M, Marini MA, Maio R, Vatrano M, Succurro E, Lauro R, Federici M, Perticone F (2005) Plasma concentration of IGF-I is independently associated with insulin sensitivity in subjects with different degrees of glucose tolerance. Diabetes Care 28:120–125
Yakar S, Liu JL, Fernandez AM, Wu Y, Schally AV, Frystyk J, Chernausek SD, Mejia W, Le Roith D (2001) Liver-specific IGF-1 gene deletion leads to muscle insulin insensitivity. Diabetes 50:1110–1118
Arnqvist HJ (2008) The role of IGF-system in vascular insulin resistance. Horm Metab Res 40:588–592
Chantelau E, Kimmerle R, Meyer-Schwickerath R (2008) Insulin, insulin analogues and diabetic retinopathy. Arch Physiol Biochem 114:54–62
Smith LEH (2005) IGF-1 and retinopathy of prematurity in the preterm infant. Biol Neonate 88:237–244
Hammes HP (2005) Pericytes and the pathogenesis of diabetic retinopathy. Horm Metab Res 37:39–43
Bornfeldt KAH (1993) Actions of insulin-like growth factor I and insulin in vascular smooth muscle: receptor interaction and growth-promoting effects. In: Flyvbjerg HOKAA, Orskov H, Alberti KGGM (eds) Growth hormone and insulin-like growth factor-I. Wiley, Chichester
Bennett MR, Evan GI, Schwartz SM (1995) Apoptosis of human vascular smooth muscle cells derived from normal vessels and coronary atherosclerotic plaques. J Clin Invest 95:2266–2274
Du J, Delafontaine P (1995) Inhibition of vascular smooth muscle cell growth through antisense transcription of a rat insulin-like growth factor I receptor cDNA. Circ Res 76:963–972
Ezzat VA, Duncan ER, Wheatcroft SB, Kearney MT (2008) The role of IGF-I and its binding proteins in the development of type 2 diabetes and cardiovascular disease. Diabetes Obes Metab 10:198–211
Izhar U, Hasdai D, Richardson DM, Cohen P, Lerman A (2000) Insulin and insulin-like growth factor-I cause vasorelaxation in human vessels in vitro. Coron Artery Dis 11:69–76
Juul A, Scheike T, Davidsen M, Gyllenborg J, Jorgensen T (2002) Low serum insulin-like growth factor I is associated with increased risk of ischemic heart disease: a population-based case–control study. Circulation 106:939–944
Spallarossa P, Brunelli C, Minuto F, Caruso D, Battistini M, Caponnetto S, Cordera R (1996) Insulin-like growth factor-I and angiographically documented coronary artery disease. Am J Cardiol 77:200–202
van den Beld AW, Bots ML, Janssen JA, Pols HA, Lamberts SW, Grobbee DE (2003) Endogenous hormones and carotid atherosclerosis in elderly men. Am J Epidemiol 157:25–31
Vaessen N, Heutink P, Janssen JA, Witteman JC, Testers L, Hofman A, Lamberts SW, Oostra BA, Pols HA, van Duijn CM (2001) A polymorphism in the gene for IGF-I: functional properties and risk for type 2 diabetes and myocardial infarction. Diabetes 50:637–642
Wallander M, Norhammar A, Malmberg K, Ohrvik J, Rydén L, Brismar K (2007) IGF binding protein 1 predicts cardiovascular morbidity and mortality in patients with acute myocardial infarction and type 2 diabetes. Diabetes Care 30:2343–2348
Gazzaruso C, Gola M, Karamouzis I, Giubbini R, Giustina A (2014) Cardiovascular risk in adult patients with growth hormone (GH) deficiency and following substitution with GH—an update. J Clin Endocrinol Metab 99:18–29
Maison P, Tropeano AI, Macquin-Mavier I, Giustina A, Chanson P (2007) Impact of somatostatin analogs on the heart in acromegaly: a metaanalysis. J Clin Endocrinol Metab 92:1743–1747
Giustina A, Casanueva FF, Cavagnini F, Chanson P, Frohman LA, Gaillard R, Ghigo E, Ho K, Jaquet P, Kleinberg DL, Lamberts SW, Lombardi G, Sheppard M, Strasburger CJ, Vance ML, Wass JA, Melmed S, Pituitary Society and the European Neuroendocrine Association (2003) Diagnosis and treatment of acromegaly complications. J Endocrinol Invest 26:1242–1247
Rieu M, Binoux M (1985) Serum levels of insulin-like growth factor (IGF) and IGF binding protein in insulin-dependent diabetics during an episode of severe metabolic decompensation and the recovery phase. J Clin Endocrinol Metab 60:781–785
Ekman B, Nystrom F, Arnqvist HJ (2000) Circulating IGF-I concentrations are low and not correlated to glycaemic control in adults with type 1 diabetes. Eur J Endocrinol 143:305–310
Hanaire-Broutin H, Sallerin-Caute B, Poncet MF, Tauber M, Bastide R, Chalé JJ, Rosenfeld R, Tauber JP (1996) Effect of intraperitoneal insulin delivery on growth hormone binding protein, insulin-like growth factor (IGF)-I, and IGF-binding protein-3 in IDDM. Diabetologia 39:1498–1504
Hedman CA, Frystyk J, Lindström T, Oskarsson P, Arnqvist HJ (2014) Intraperitoneal insulin delivery to patients with type 1 diabetes results in higher serum IGF-I bioactivity than continuous subcutaneous insulin infusion. Clin Endocrinol 81:58–62
Bereket A, Lang CH, Blethen SL, Ng LC, Wilson TA (1996) Insulin treatment normalizes reduced free insulin-like growth factor-I concentrations in diabetic children. Clin Endocrinol 45:321–326
Ekström K, Salemyr J, Zachrisson I, Carlsson-Skwirut C, Ortqvist E, Bang P (2007) Normalization of the IGF-IGFBP axis by sustained nightly insulinization in type 1 diabetes. Diabetes Care 30:1357–1363
Chisalita SI, Arnqvist HJ (2004) Insulin-like growth factor I receptors are more abundant than insulin receptors in human micro- and macrovascular endothelial cells. Am J Physiol Endocrinol Metab 286:E896–E901
Federici M, Zucaro L, Porzio O, Massoud R, Borboni P, Lauro D, Sesti G (1996) Increased expression of insulin/insulin-like growth factor-I hybrid receptors in skeletal muscle of noninsulin-dependent diabetes mellitus subjects. J Clin Invest 98:2887–2893
Belfiore A, Frasca F, Pandini G, Sciacca L, Vigneri R (2009) Insulin receptor isoforms and insulin receptor/insulin-like growth factor receptor hybrids in physiology and disease. Endocr Rev 30:586–623
Federici M, Porzio O, Lauro D, Borboni P, Giovannone B, Zucaro L, Hribal ML, Sesti G (1998) Increased abundance of insulin/insulin-like growth factor-I hybrid receptors in skeletal muscle of obese subjects is correlated with in vivo insulin sensitivity. J Clin Endocrinol Metab 83:2911–2915
Federici M, Porzio O, Zucaro L, Giovannone B, Borboni P, Marini MA, Lauro D, Sesti G (1997) Increased abundance of insulin/IGF-I hybrid receptors in adipose tissue from NIDDM patients. Mol Cell Endocrinol 135:41–47
Federici M, Giaccari A, Hribal ML, Giovannone B, Lauro D, Morviducci L, Pastore L, Tamburrano G, Lauro R, Sesti G (1999) Evidence for glucose/hexosamine in vivo regulation of insulin/IGF-I hybrid receptor assembly. Diabetes 48:2277–2285
Federici M, Lauro D, D’Adamo M, Giovannone B, Porzio O, Mellozzi M, Tamburrano G, Sbraccia P, Sesti G (1998) Expression of insulin/IGF-I hybrid receptors is increased in skeletal muscle of patients with chronic primary hyperinsulinemia. Diabetes 47:87–92
Belfiore A (2007) The role of insulin receptor isoforms and hybrid insulin/IGFI receptors in human cancer. Curr Pharm Des 13:671–686
Kurtzhals P, Schaffer L, Sorensen A, Kristensen C, Jonassen I, Schmid C, Trub T (2000) Correlations of receptor binding and metabolic and mitogenic potencies of insulin analogs designed for clinical use. Diabetes 49:999–1005
Pierre-Eugene C, Pagesy P, Nguyen T, Neuille M, Tschank G, Tennagels N, Hampe C, Issad T (2012) Effect of insulin analogues on insulin/IGF1 hybrid receptors: increased activation by glargine but not by its metabolites M1 and M2. PLoS ONE 7:e41992
Weinstein D, Simon M, Yehezkel E, Laron Z, Werner H (2008) Insulin analogues display IGF-1-like mitogenic and anti-apoptotic activities in cultured cancer cells. Diabetes Metab Res Rev 25:41–49
Ciaraldi TP, Carter L, Seipke G, Mudaliar S, Henry RR (2001) Effects of the long-acting insulin analog insulin glargine on cultured human skeletal muscle cells: comparisons to insulin and IGF-I. J Clin Endocrinol Metab 86:5838–5847
Hemkens LG, Grouven U, Bender R, Gunster C, Gutschmidt S, Selke GW, Sawicki PT (2009) Risk of malignancies in patients with diabetes treated with human insulin or insulin analogues: a cohort study. Diabetologia 52:1732–1744
Mannucci E, Monami M, Balzi D, Cresci B, Pala L, Melani C, Lamanna C, Bracali I, Bigiarini M, Barchielli A, Marchionni N, Rotella CM (2010) Doses of insulin and its analogues and cancer occurrence in insulin-treated type 2 diabetic patients. Diabetes Care 33:1997–2003
Slawik M, Schories M, Grawitz AB, Reincke M, Petersen KG (2006) Treatment with insulin glargine does not suppress serum IGF-1. Diabet Med 23:814–817
Home PD, Lagarenne P (2009) Combined randomised controlled trial experience of malignancies in studies using insulin glargine. Diabetologia 52:2499–2506
Edwards KL, Riche DM, Stroup JS, Goldman-Levine JD, Padiyara RS, Cross LB, Kane MP (2010) Insulin glargine and cancer risk: an opinion statement of the Endocrine and Metabolism Practice and Research Network of the American College of Clinical Pharmacy. Pharmacotherapy 30:955–965
Nishimura E, Sorensen AR, Hansen BF et al (2010) Insulin degludec: a new ultra-long, basal insulin designed to maintain full metabolic effect while minimizing mitogenic potential. Diabetologia 53(Suppl 1):S388
Nishimura E, Sorensen A, Hansen BF et al (2010) Insulin degludec is a new generation ultra-long acting basal insulin designed to maintain full metabolic effect while minimizing mitogenic potential. Diabetes 59(Suppl 1):A375
Wang F, Surh J, Kaur M (2012) Insulin degludec as an ultralong-acting basal insulin once a day: a systematic review. Diabetes Metab Syndr Obes 5:191–204
Pollak M, Russell-Jones D (2010) Insulin analogues and cancer risk: cause for concern or cause celebre? Int J Clin Pract 64:628–636
Zib I, Raskin P (2006) Novel insulin analogues and its mitogenic potential. Diabetes Obes Metab 8:611–620
Bordeleau L, Yakubovich N, Dagenais GR, Rosenstock J, Probstfield J, Chang YuP, Ryden LE, Pirags V, Spinas GA, Birkeland KI, Ratner RE, Marin-Neto JA, Keltai M, Riddle MC, Bosch J, Yusuf S, Gerstein HC, for the ORIGIN Trial Investigators (2014) The association of basal insulin glargine and/or n-3 fatty acids with incident cancers in patients with dysglycemia. Diabetes Care 37:1360–1366
Ioacara S, Guja C, Ionescu-Tirgoviste C, Fica S, Roden M (2014) Cancer specific mortality in insulin-treated type 2 diabetes patients. PLoS ONE 9:e93132
Simo R, Plana-Ripoli O, Puente D, Morros R, Mundel X, Vilca LM, Hernandez C, Fuents I, Procupet A, Tabernero JM, Violan C (2013) Impact of glucose-lowering agents on the risk of cancer in type 2 diabetic patients. The barcelona case–control study. PLoS ONE 8:e79968
Sturmer T, Marquis MA, Zhou H, Meigs JB, Lim S, Blonde L, Macdonald E, Wang R, Lavange LM, Pate V, Buse JB (2013) Cancer incidence among those initiating insulin therapy with glargine versus human NPH insulin. Diabetes Care 36:3517–3525
Bolli GB, Hahn AD, Schmidt R, Eisenblaetter T, Dahmen R, Heise T, Becker RH (2012) Plasma exposure to insulin glargine and its metabolites M1 and M2 after subcutaneous injection of therapeutic and supratherapeutic doses of glargine in subjects with type 1 diabetes. Diabetes Care 35:2626–2630
Sommerfel MR, Müller G, Tschank G, Seipke G, Habermann P, Kurrle R, Tennagels N (2010) In vitro metabolic and mitogenic signaling of insulin glargine and its metabolites. PLOsONE 5:e9540
Owens DR, Matfin G, Monnier L (2014) Basal insulin analogues in the management of diabetes mellitus: what progress have we made? Diabetes Metab Res Rev 30:104–119
Schalch DS, Turman NJ, Marcsisin VS, Heffernan M, Guler HP (1993) Short-term effects of recombinant human insulin-like growth factor I on metabolic control of patients with type II diabetes mellitus. J Clin Endocrinol Metab 77:1563–1568
Carroll PV, Umpleby M, Alexander EL, Egel VA, Callison KV, Sönksen PH, Russell-Jones DL (1998) Recombinant human insulin-like growth factor-I (rhIGF-I) therapy in adults with type 1 diabetes mellitus: effects on IGFs, IGF-binding proteins, glucose levels and insulin treatment. Clin Endocrinol 49:739–746
Zenobi PD, Graf S, Ursprung H, Froesch ER (1992) Effects of insulin like growth factor-I on glucose tolerance, insulin levels, and insulin secretion. J Clin Invest 89:1908–1913
Schmid C, Bianda T, Zwimpfer C, Zapf J, Wiesli P (2005) Changes in insulin sensitivity induced by short-term growth hormone (GH) and insulin-like growth factor I (IGF-I) treatment in GH deficient adults are not associated with changes in adiponectin levels. Growth Horm IGF Res 15:300–303
Zenobi PD, Glatz Y, Keller A, Graf S, Jaeggi-Groisman SE, Riesen WF, Schoenle EJ, Froesch ER (1994) Beneficial metabolic effects of insulin-like growth factor I in patients with severe insulin resistant diabetes type A. Eur J Endocrinol 131:251–257
Morrow LA, O’Brien MB, Moller DE, Flier JS, Moses AC (1994) Recombinant human insulin-like growth factor-I therapy improves glycemic control and insulin action in the type A syndrome of severe insulin resistance. J Clin Endocrinol Metab 79:205–210
Cheetham TD, Holly JM, Clayton K, Cwyfan-Hughes S, Dunger DB (1995) The effects of repeated daily recombinant human insulin-like growth factor I administration in adolescents with type 1 diabetes. Diabet Med 12:885–892
Moses AC, Young SC, Morrow LA, O’Brien M, Clemmons DR (1996) Recombinant human insulin-like growth factor I increases insulin sensitivity and improves glycemic control in type II diabetes. Diabetes 45:91–100
Pratipanawatr T, Pratipanawatr W, Rosen C, Berria R, Bajaj M, Cusi K, Mandarino L, Kashyap S, Belfort R, DeFronzo RA (2002) Effect of IGF-I on FFA and glucose metabolism in control and type 2 diabetic subjects. Am J Physiol Endocrinol Metab 282:E1360–E1368
Saukkonen T, Amin R, Williams RM, Fox C, Yuen KC, White MA, Umpleby AM, Acerini CL, Dunger DB (2004) Dose-dependent effects of recombinant human insulin-like growth factor (IGF)-I/IGF binding protein-3 complex on overnight growth hormone secretion and insulin sensitivity in type 1 diabetes. J Clin Endocrinol Metab 89:4634–4641
Zenobi PD, Jaeggi-Groisman SE, Riesen WF, Roder ME, Froesch ER (1992) Insulin-like growth factor-I improves glucose and lipid metabolism in type 2 diabetes mellitus. J Clin Invest 90:2234–2241
Thankamony A, Capalbo D, Marcovecchio ML, Sleigh A, Jørgensen SW, Hill NR, Mooslehner K, Yeo GS, Bluck L, Juul A, Vaag A, Dunger DB (2014) Low circulating levels of IGF-I in healthy adults are associated with reduced β-cell function, increased intramyocellular lipid and enhanced fat utilisation during fasting. J Clin Endocrinol Metab 99:2198–2207
Ripa P, Robertson I, Cowley D, Harris M, Masters IB, Cotterill AM (2002) The relationship between insulin secretion, the insulin-like growth factor axis and growth in children with cystic fibrosis. Clin Endocrinol 56:383–389
Rennert NJ, Caprio S, Sherwin RS (1993) Insulin-like growth factor I inhibits glucose-stimulated insulin secretion but does not impair glucose metabolism in normal humans. J Clin Endocrinol Metab 76:804–806
Porksen N, Hussain MA, Bianda TL, Nyholm B, Christiansen JS, Butler PC, Veldhuis JD, Froesch ER, Schmitz O (1997) IGF-I inhibits burst mass of pulsatile insulin secretion at supraphysiological and low IGF-I infusion rates. Am J Physiol Endocrinol Metab 272:E352–E358
Xuan S, Kitamura T, Nakae J, Politi K, Kido Y, Fisher PE, Morroni M, Cinti S, White MF, Herrera PL, Accili D, Efstratiadis A (2002) Defective insulin secretion in pancreatic beta cells lacking type 1 IGF receptor. J Clin Invest 110:1011–1019
Kulkarni RN (2005) New insights into the roles of insulin/IGF-I in the development and maintenance of beta-cell mass. Rev Endocr Metab Disord 6:199–210
Ueki K, Okada T, Hu J, Liew CW, Assmann A, Dahlgren GM, Peters JL, Shackman JG, Zhang M, Artner I, Satin LS, Stein R, Holzenberger M, Kennedy RT, Kahn CR, Kulkarni RN (2006) Total insulin and IGF-I resistance in pancreatic beta cells causes overt diabetes. Nat Genet 38:583–588
van Haeften TW, Twickler TB (2004) Insulin-like growth factors and pancreas beta cells. Eur J Clin Invest 34:249–255
Jones PM, Persaud SJ (1994) Tyrosine kinase inhibitors inhibit glucose-stimulated insulin secretion. Biochem Soc Trans 22:209S
Persaud SJ, Harris TE, Burns CJ, Jones PM (1999) Tyrosine kinases play a permissive role in glucose-induced insulin secretion from adult rat islets. J Mol Endocrinol 22:19–28
Lu Y, Herrera PL, Guo Y, Sun D, Tang Z, LeRoith D, Liu JL (2004) Pancreatic-specific inactivation of IGF-I gene causes enlarged pancreatic islets and significant resistance to diabetes. Diabetes 53:3131–3141
Liu JL (2007) Does IGF-I stimulate pancreatic islet cell growth? Cell Biochem Biophys 48:115–125
Simpson HL, Jackson NC, Shoejaee-Moradie F, Jones RH, Russell-Jones DL, Sönksen PH, Dunger DB, Umpleby AM (2004) Insulin-like growth factor I has a direct effect on glucose and protein metabolism, but no effect on lipid metabolism in type 1 diabetes. J Clin Endocrinol Metab 89:425–432
Williams RM, Amin R, Shojaee-Moradie F, Umpleby AM, Acerini CL, Dunger DB (2003) The effects of a specific growth hormone antagonist on overnight insulin requirements and insulin sensitivity in young adults with type 1 diabetes mellitus. Diabetologia 46:1203–1210
Saukkonen T, Shojaee-Moradie F, Williams RM, Amin R, Yuen KC, Watts A, Acerini CL, Umpleby AM, Dunger DB (2006) Effects of recombinant human IGF-I/IGF-binding protein-3 complex on glucose and glycerol metabolism in type 1 diabetes. Diabetes 55:2365–2370
Cusi K, DeFronzo R (2000) Recombinant human insulin-like growth factor I treatment for 1 week improves metabolic control in type 2 diabetes by ameliorating hepatic and muscle insulin resistance. J Clin Endocrinol Metab 85:3077–3084
Rh in NIDDM Study Group (1996) Evidence from a dose ranging study that recombinant insulin-like growth factor-I (RhIGF-I) effectively and safely improves glycemic control in the noninsulin dependent diabetes mellitus. Diabetes 45:91–100
Giustina A, Licini M, Bussi AR, Girelli A, Pizzocolo G, Schettino M, Negro-Vilar A (1993) Effects of sex and age on the growth hormone response to galanin in healthy human subjects. J Clin Endocrinol Metab 76:1369–1372
Mauras N, Fox L, Englert K, Beck RW (2013) Continuous glucose monitoring in type 1 diabetes. Endocrine 43:41–50
Higgins T (2013) HbA1c for screening and diagnosis of diabetes mellitus. Endocrine 43:266–273
Conflict of interest
A. Giustina, R. Berardelli, C. Gazzaruso and G. Mazziotti declare that they have no conflict of interest.
Human and animal rights disclosure
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Managed by Massimo Federici.
Rights and permissions
About this article
Cite this article
Giustina, A., Berardelli, R., Gazzaruso, C. et al. Insulin and GH–IGF-I axis: endocrine pacer or endocrine disruptor?. Acta Diabetol 52, 433–443 (2015). https://doi.org/10.1007/s00592-014-0635-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0635-6