Abstract
The primary aim of the study was to evaluate the range of motion and complications after Genesis II total knee arthroplasty with high-flexion tibia insert (TKA–HF). Furthermore, difference in knee flexion between high flexion and standard inserts was compared. The hypothesis was that knee flexion is better after high-flexion TKA. A total of 292 TKA–HF were retrospectively reviewed. Mean follow-up was 24.3 months. The range of motion was compared between TKA–HF (high-flexion group) and a comparable cohort of 86 Genesis II TKA with a standard tibia insert (control group). Surgeries were performed by one experienced knee orthopedic surgeon. Knee flexion in the high-flexion group increased from 114.8° preoperatively to 118.0° postoperatively (P < 0.01). Knee extension in the high-flexion group increased from −4.5° preoperatively to −0.4° after surgery (P < 0.01). Mean knee flexion was 5.52° (±1.46°) better in the high-flexion group compared with the control group (P < 0.01). Preoperative range of motion, body mass index, diabetes mellitus and patellofemoral pain significantly influenced range of motion. Few complications occurred after TKA–HF. The Genesis II TKA–HF showed good short-term results with limited complications. Knee flexion after Genesis II TKA–HF was better compared with a standard tibia insert.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is a successful surgery for end-stage knee osteoarthritis. Pain relief and optimal range of motion are important goals of TKA. These goals are also important for patient satisfaction [1, 2]. Many factors influence the range of motion after TKA: preoperative flexion, surgical indication, coronal alignment, patient age, body weight, Knee Society knee score, wound closure technique and prosthetic design [3–9]. Postoperative pain and knee ligamentous stability are also important factors for a successful TKA [10, 11].
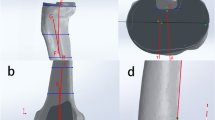
Since January 2005, the senior author (R.J.) uses the Genesis II posterior stabilized TKA with a high-flexion tibia insert (Smith & Nephew, Memphis Tennessee, USA). The high-flexion tibia insert has several design modifications in comparison with the standard insert (Fig. 1). This leads to a decreased impingement potential of both patella and patellar ligament on the posterior stabilized cam in case of deep knee flexion [12]. The primary aim of the present study was to assess the range of motion and complications after Genesis II posterior stabilized TKA with high-flexion tibia insert (TKA–HF, Smith & Nephew, Memphis Tennessee, USA). Furthermore, range of motion was compared between Genesis II posterior stabilized TKA–HF and a comparable cohort of Genesis II TKA with standard tibia insert. The hypothesis was that knee flexion is better after high-flexion TKA.
Materials and methods
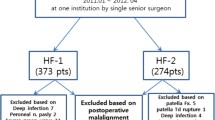
We retrospectively reviewed the data of 307 primary cemented Genesis II TKA–HF (282 patients) operated between January 2005 and May 2009.
Inclusion criteria were primary TKA–HF, follow-up ≥10 months and surgery by a single surgeon (R.J.).
Exclusion criteria were unknown preoperative range of motion of the knee, follow-up <10 months, surgery by a different orthopedic surgeon and revision surgery.
Fifteen patients (15 TKA) of the 307 TKA were excluded. Reasons for exclusion were unknown preoperative range of motion (3), follow-up <10 months [non-related deaths (7), patients who could not be traced or contacted for follow-up examinations (5)]. Mean follow-up period was 24.3 (10–61) months.
In order to compare range of motion outcomes between a posterior stabilized high flexion and standard tibia inserts, the group of 292 Genesis II TKA–HF was compared with a cohort of patients operated by the same surgeon with a Genesis II TKA with standard insert in the years prior to 2005 (control group). The control group consisted of 102 patients. In the control group, 16 TKA were excluded because of a follow-up <10 months [non-related deaths (2) and patients who could not be traced or contacted for follow-up examinations (14)].
Patient demographics are presented in Table 1. To determine their role in final range of motion after TKA, the following factors were analyzed: gender, age, BMI, tibial-femoral angle, co-morbidity (diabetes mellitus and rheumatoid arthritis) and preoperative range of motion.
Standardized weight-bearing long leg radiographs were obtained to measure the mechanical tibial–femoral angle. A single independent researcher (M.F.) performed all examinations. Range of motion of the knee was measured using a goniometer. Patients were placed supine. Center of rotation was determined as the lateral femur epicondyle. One arm of the goniometer was placed parallel to the shaft of the femur in line with the greater trochanter of the hip, and the other arm was placed parallel to the shaft of the tibia in line with the lateral malleolus at the ankle.
Surgical technique
A combined spinal and epidural anesthesia was preferred in all patients. Prophylactic parenteral antibiotics (first generation cephalosporin) were administered 30–60 min prior to the skin incision, continued for 24 h after surgery. A tourniquet was inflated with the knee in maximum flexion prior to the surgery.
An anterior midline incision was followed by a medial mid-vastus arthrotomy. After lateral subluxation of the patella, the anterior cruciate ligament and menisci were dissected. The valgus angle for the intramedullary femur guidance can be set between 5° and 7° of valgus. The amount of valgus of the femoral component was measured on the weight-bearing long leg X-ray, as the angle between the mechanical and anatomical femoral axis. On the same X-ray, the point of intersection of the anatomical femoral axis and the distal femoral joint line determined the entry point of the femoral guidance rod at the distal femur. The rotation of the femoral component was determined by the A–P axis (Whiteside’s line) marked during surgery. Posterior femoral offset was restored as much as possible by choosing the largest femoral component if in between sizes, never exceeding the femoral medial–lateral size. Anterior referencing femoral blocks were used to guide the anterior and posterior femoral resections. After all femoral chamfer cuts were made, the tibia was exposed and osteophytes removed. The extramedullary tibial alignment guide was mounted on the lower leg. The distal portion of the guide was centered over the ankle and the proximal part aligned with the tibial crest in a frontal plane. A second long straight rod was held parallel to the fibula in the sagittal plane to set tibial slope. Rotation of the tibial resection guide was set over the medial third of the tibial tubercle. This technique has previously been reported as reliable by the senior author [13]. The tibial resection was made using the correct right or left resection guide, after sizing the amount of tibial resection by means of a 9 mm stylus. Finally, trial component implantation and ligament balancing in flexion and extension were performed. A high flexion- or standard posterior stabilized tibial component was inserted in all patients. Final rotation of the tibial component was set in full extension, aligning the tibial and femoral components after range of motion control. Both femoral and tibial components were cemented. The patella was not routinely resurfaced.
Tourniquet was released, and patellar tracking evaluated. Wound closure was performed in 90° of knee flexion. A closed drainage system was left in situ for 24–48 h after surgery. A compressive bandage of the leg was removed on the first day after surgery.
The epidural anesthesia was continued for 48 h after surgery. Thereafter, patients received oral analgesia. Low molecular heparin was used as thrombosis prophylaxis for 6 weeks after surgery. The first day after surgery, patients started with exercises on the continuous passive motion machine (OrthoRehab, Oakville, Ontario, Canada). The second day, patients started walking with crutches or walker and continued active and passive range of motion exercises. Weight-bearing was allowed as tolerated. In severe valgus osteoarthritis, patients were instructed to 50 % weight-bearing for 6 weeks. After discharge, mostly after 4 days, patients received outpatient physiotherapy for a minimum of 6 weeks. Clinical and radiological evaluations were done at 6 weeks, 3–6 months, and yearly thereafter, and collateral ligamentous stability and postoperative patellofemoral pain were identified as possible factors affecting range of motion.
Patient dossiers were used for the present study. If the patients did not attend the regular follow-up examinations, they were contacted by telephone or letter. In these patients, new X-rays were obtained and all follow-up examinations were done.
Statistical analyses
Statistical analysis was performed with IBM SPSS Statistics 19.0. Normal distributed scores were compared with the paired t test or ANOVA test. Not normally distributed scores were compared with the Wilcoxon test or the Kruskal–Wallis H test. Distribution was tested with skewness and kurtosis. Significance was set at <0.05. Regression analysis was used to correct for demographic factors and to analyze the factors that influenced postoperative range of motion.
Results
In the TKA–HF, the flexion and extension increased significantly postoperatively compared with preoperative values (Table 2).
After correcting for the preoperative flexion and patellofemoral resurfacing, there was still a significant increase in mean flexion of 5.52° (±1.46°, P < 0.01) of the high-flexion group compared with the control group [mean postoperative flexion of 111.7° (35°–140°)]. There was no significant difference in extension −0.35° (−10° to 0°, P = 0.75).
In the present study, several factors significantly affected final range of motion after TKA: preoperative flexion and preoperative extension (Table 3), diabetes and obesity (Table 4) and patellofemoral pain (Table 5). For obesity, comparison was made between the postoperative results of non-obese (BMI < 30) versus obese (BMI > 30) patients [14].
For preoperative flexion contracture, there was a significant difference between the patient group without a flexion contracture and the patient group with a contracture more than 10° (Table 4). There was no significant difference between patients without a flexion contracture and patients with a contracture between 0° and 5° (n = 61 TKA, P = 0.52) or 5° and 10° (n = 41 TKA, P = 0.40).
Complications
Complications found in present study are presented in Table 6.
Discussion
The most important finding of the present study was a significant increase in flexion and extension after TKA with a high-flexion tibia component. Compared with a cohort with TKA with standard insert, we also found a significantly better flexion. In the present study, preoperative flexion, preoperative extension, BMI > 30, diabetes mellitus and postoperative patellofemoral pain were significant factors that influenced postoperative range of motion after TKA.
One of the many factors affecting the outcome of the TKA is the implant design. The principal goal of high-flexion TKA is an increase in postoperative flexion. In the present study, there was a significantly better mean flexion in the high-flexion Genesis II TKA compared with the same prosthesis with a standard insert (5.52° ± 1.46°). Murphy et al. [16] have performed a systematic review on high-flexion TKA. Their results showed a variable range of motion: 106°–133° of flexion and −0.7° to 1.0° of extension after a follow-up <35 months. Other authors compared the high-flexion insert with the standard and cruciate retaining insert. Mehin et al. [17] concluded in a meta-analysis of five randomized controlled trials (RCT) that there was no significant improvement in the postoperative range of motion. Hamilton et al. [18] found similar results in a focused review of five prospective RCT. In the reviews, different types TKA were used. Focusing on the Genesis II TKA, McCalden et al. compared, in a RCT study, the range of motion between the TKA–HF (50) and TKA standard insert (50). There was no significant difference in flexion after 2 years (124° ± 7° vs. 123° ± 7°) [19]. Laskin [20] compared a group of 40 Genesis II TKA–HF with a cohort of 40 Genesis II standard TKA. After 2-year follow-up, they found a significant difference in flexion in the TKA–HF group (133° vs. 118°). Compared with the present study, the patient groups in the studies by McCalden et al. and Laskin et al. were smaller. Other in- and exclusion criteria were used in the study of McCalden. McCalden et al. [19] excluded patients with a preoperative flexion <90°. Laskin [20] did not describe their in- and exclusion criteria. Preoperative range of motion is an important factor for postoperative range of motion after TKA [3–5]. This has also been demonstrated in the present study. The differences in flexion after Genesis II TKA–HF in the present study (mean postoperative flexion 118.0°), in comparison with the previous studies with the same prosthesis by McCalden et al. (mean postoperative flexion 124°) and Laskin et al. (mean postoperative flexion 133°), may be explained by these differences.
Zeh et al. [21] evaluated the Genesis II posterior stabilized high-flexion TKA. They found a mean postoperative flexion of 120.7° and extension contracture of 0.1° with mean follow-up of 1.25 years in 64 primary cemented prostheses. In the present study, similar results were found.
Do patients need high flexion after TKA or is pain relief the most important goal for patients? A few studies have evaluated the necessity of knee motion during daily living. They found that different cultures have different requirements regarding knee flexion angles. In the western culture, knee flexion of 110°–115° is sufficient for most activities of daily living. One needs 90° of flexion to descend stairs, 93° to raise from a chair, and 117° to lift an object [22]. People in Asian or Middle East cultures need a greater degree of flexion for activities such as kneeling or sitting in cross-legged positions in order to eat, pray, or socialize [23, 24]. The average flexion of 118° obtained in the present study may be considered a good result for the western patient population. The studies of Meneghini and Ghandi concluded that there is no significant functional difference between knee flexion of 115° versus a flexion of >125° in the western population [25, 26].
Frosch et al. [27] reported the complications of 512 TKA at 1-year follow-up. Compared with the present study, they found higher complication rates. Cusher et al. [28] described, in a multinational observational study, the complications of 8325 TKA at 3–12 months follow-up. The complications in the present study compare favorably with these findings.
There are limitations to the present study. The retrospective setting of the present study only allowed a descriptive conclusion of the complication rate after TKA–HF. We agree with the conclusion in the study by [27] that comparison of complications after TKA between different publications is difficult. Another possible limitation of the present study is the comparison of results between the study group and a cohort control group. However, comparable demographics between both groups as well as an identical surgical technique by a single surgeon did allow the conclusions as proposed.
In conclusion, the Genesis II TKA–HF showed good short-term results with limited complications. Knee flexion after Genesis II TKA was better with a high-flexion posterior stabilized tibia insert compared with a standard posterior stabilized insert.
References
Robertsson O, Dunbar M, Pehrsson T et al (2002) Patient satisfaction after knee arthroplasty, a report on 27,372 knees operated between 1981 and 1995 in Sweden. Acta Orthop Scand 71(3):262–267
Bourne R, Chesworth B, Davis A et al (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not. Clin Orthop Relat Res 468:57–63
Harvey I, Barry K, Kirby S et al (1993) Factors affecting the range of movement of total knee arthroplasty. J Bone Joint Surg Br 75-B(6):950–955
Kawamura H, Bourne R (2001) Factors affecting range of flexion after total knee arthroplasty. J Orthop Sci 6:248–252
Ritter MA, Harty LD, Davis KE et al (2003) Predicting range of motion after total knee arthroplasty. Clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am 85A(7):1278–1285
Bong M, Di Cesare P (2004) Stiffness after total knee arthroplasty. J Am Acad Orthop Surg 12(3):164–171
Li P, Wong Y, Wai Y (2007) Knee flexion after total knee arthroplasty. J Orthop Surg 15(2):149–153
Moon HK, Han CD, Yang IH et al (2008) Factors affecting outcome after total knee arthroplasty in patients with diabetes mellitus. Yonsei Med J 49(1):129–137
Seon JK, Park JK et al (2011) Comparisons of kinematics and range of motion in high-flexion total knee arthroplasty: cruciate retaining vs. substituting designs. Knee Surg Sports Traumatol Arthrosc 19:2016–2022
Clarke H, Scuderi G (2003) Flexion instability in primary total knee replacement. J Knee Surg 16(2):123–128
Graichen H, Strauch M, Katzhammer T et al (2007) Ligament instability in total knee arthroplasty-causal analysis. Orthopade 36(7):650–652
McCalden RW, MacDonald SJ, Charron KD et al (2010) The role of polyethylene design on postoperative TKA flexion: an analysis of 1534 cases. Clin Orthop Relat Res 468:108–114
Kroon KE, Houterman S, Janssen RP (2012) Leg alignment and tibial slope after minimal invasive total knee arthroplasty: a prospective, randomized radiological study of intramedullary versus extramedullary tibial instrumentation. Knee 19:270–274
(1998) National Institutes of Health, National Heart, Lung, and Blood Institute. Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Obes Res 6(2):51S–209S
Rutten SG, Janssen RP (2009) Spontaneous late dislocation of the high flexion tibial insert after Genesis II total knee arthroplasty. A case report. Knee 16(5):409–411
Murphy M, Journeaux S, Russel T (2009) High-flexion total knee arthroplasty: a systematic review. Int Orthop 33:887–893
Mehin R, Burnett R, Brseher P (2010) Does the new generation of high-flex knee prosthesis improve the post-operative range of movement. J Bone Joint Surg Br 92B(10):1429–1434
Hamilton WG, Sritulanondha S, Engh CAJ (2011) Results of prospective, randomized clinical trials comparing standard and high-flexion posterior-stabilized TKA: a focused review. Orthopaedics 34(9):e500–e503
McCalden R, MacDonald S, Bourne R et al (2009) A randomized controlled trial comparing “high-flex” vs. “standard” posterior cruciate substituting polyethylene tibial inserts in total knee arthroplasty. J Arthroplast 24(6):33–38
Laskin R (2007) The effect of a high-flex implant on postoperative flexion after primary total knee arthroplasty. Orthopedics 30(8):86–88
Zeh A, Davis J, Laskin R et al (2009) Early results with the Genesis II posterior stabilized high flexion knee prosthesis a one year follow-up study. Acta Orthop Belg 75(6):792–800
Laubenthal K, Smidt G, Kettelkamp D (1972) A quantitative analysis of knee motion during activities of daily living. Phys Ther 52:34–42
Mulholland SJ, Wyss UP (2001) Activities of daily living in non-western cultures: range of motion requirements for hip and knee joint implants. Int J Rehabil Res 24:191–198
Kurosaka M, Yoshiya S, Mizuno K et al (2002) Maximizing flexion after total knee arthroplasty: the need and the pitfalls. J Arthroplast 17(4):59–62
Meneghini RM, Pierson JL, Bagsby D et al (2007) Is there a functional benefit to obtaining high flexion after total knee arthroplasty? J Arthroplast 22(6):43–46
Gandhi R, Tso P, Davey JR et al (2009) High-flexion implants in primary total knee arthroplasty: a meta-analysis. Knee 16:14–17
Frosch P, Decking J, Theis C et al (2004) Complications after total knee arthroplasty. A comprehensive report. Acta Orthop Belg 70:565–569
Cushner F, Agnelli G, FitzGerald G et al (2010) Complications and functional outcomes after total hip arthroplasty and total knee arthroplasty: results from the global orthopaedic registry (GLORY). Am J Orthop 39(9):22–28
Acknowledgments
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fuchs, M.C.H.W., Janssen, R.P.A. Clinical evaluation of 292 Genesis II posterior stabilized high-flexion total knee arthroplasty: range of motion and predictors. Eur J Orthop Surg Traumatol 25, 161–166 (2015). https://doi.org/10.1007/s00590-014-1467-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-014-1467-3