Abstract
Purpose
Currently, a high-flexion cruciate-retaining knee prosthesis has been designed to allow greater advantage after total knee arthroplasty (TKA). The present study was conducted to compare functional outcome, range of motion (ROM) as well as complications in subjects who underwent either a high-flexion cruciate-retaining (HFCR, Group I) or a high-flexion posterior-substituting (HFPS, Group II) prosthesis TKA.
Methods
Thirty-four subjects which had TKA with HFCR prosthesis and thirty-three subjects which had TKA with HFPS prosthesis were enrolled in our study and were assessed preoperatively and at 24 months postoperatively. For functional outcome comparison, Hospital for Special Surgery Score (HSSS), Knee Society Score (KSS, including the Mean Knee Score and the Mean Function Score) as well as SF12 Score (including Mental Health Score and Physical Health Score) were measured. For ROM comparison, the arcs of maximal non-weight-bearing passive flexion and weight-bearing flexion were detected, and the number of knees which allowed patients to kneel and sit cross-legged in comfort was determined. For complication comparison, wound necrosis/discharge, anterior knee pain, dislocation, radiolucent lines as well as osteolysis were investigated.
Results
At 24-month follow-up, no significant difference in functional outcome between the two groups was detected. The average maximal non-weight-bearing flexion was 136.2° for the knees in Group I and 135.1° for the knees in Group II (P > 0.05). The average weight-bearing flexion was 123.2° for the knees in Group I and 129.8° for the knees in Group II (P > 0.05). No significant difference, with regard to the number of knees that allowed kneeling and sitting cross-legged, was detected. Comparisons of postoperative complications between the two groups did not yield a significant difference.
Conclusions
Our study demonstrated no advantage of the high-flexion cruciate- retaining TKA over high-flexion posterior-substituting TKA with regard to functional outcome, range of motion as well as complications at short-term follow-up. However, longer follow-up is necessary to confirm whether these results are sustained.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Range of motion in TKA is established as a key determining factor in overall functional outcome. The fact that most knees fail to flex more than 120° after TKA has been investigated extensively, however, no one theory can explain this phenomenon sufficiently. To improve deep flexion after TKA, high flexion prosthesis has been developed in resent years. These designs, theoretically, may result in better postoperative ROM [1, 2]. However, conflicting reports exist in the literature on the short-term outcomes of high flexion design [1, 3, 4]. A published meta-analysis did indicate a statistical difference in favor of the high-flexion design with regard to ROM as compared with standard designs [5]. While in another systematic review, no significant difference was investigated between the two prosthesis [6].
A variety of factors can influence the ROM of knees after TKA. Functional recreation or anatomical preservation of the posterior cruciate ligament (PCL) is recognized as one of the kinematic pillars. The main function of PCL is to prevent the femur from falling off the anterior edge of the tibia and to prevent posterior translation of the tibia on the femur. According to the PCL being excised or retained, total knee prosthesis is divided into posterior-substituting (PS) or cruciate-retaining (CR) prosthesis. Although the discussion of the two designs was argued in many previous years, the superiority of one prosthesis versus the other is still controversial [7–10].
Currently, a high-flexion cruciate-retaining knee prosthesis has been designed to allow greater advantage after total knee arthroplasty [11–16]. This new designs have attracted considerable attention. However, the benefit of so-called high-flexion cruciate-retaining TKA remains a subject of debate. Varieties of studies have demonstrated no statistical difference in terms of functional outcomes and ROM between the high-flexion cruciate-retaining and the high-flexion posterior-substituting total knee arthroplasty [13, 15]. With regard to a high-flexion cruciate- retaining total knee arthroplasty, we are aware of no report comparing the complication of high-flexion cruciate-retaining and high-flexion posterior-substituting designs.
In this present study, we compared the functional outcome, range of motion as well as complications at a follow-up of 24 months in patients who had implantation of high-flexion cruciate-retaining designs and subjects managed with high-flexion posterior-substituting designs. It was hypothesized that subjects with a high-flexion cruciate-retaining TKA would possess better postoperative outcomes than those with high-flexion posterior-substituting TKA.
Materials and methods
Demographics
To verify our hypotheses, the retrospective comparative study was conducted for comparison between patients who had implantation of high-flexion cruciate-retaining designs and subjects managed with high-flexion posterior-substituting designs. From 2007 to 2011, 34 patients (Group I) underwent HFCR TKA and 33 patients (Group II) underwent HFPS TKA were enrolled in our investigation. Inclusion criteria included less than 15° valgus or less than 10° varus deformity, less than 10° flexion deformity, ROM of greater than 80°, and BMI less than 28 kg/m2. Simultaneous exclusion criteria included compromise of soft-tissue envelope, previously operated joint, and joints required a complex reconstruction with bone graft and/or prosthetic augmentation. Institutional review board approval was obtained prior to initiation of the study, and all subjects provided informed consent for participation.
Surgical technique
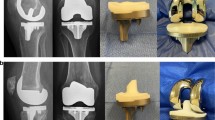
Each patient was undertaken by the senior author. Surgery was performed in the two groups using standard surgical techniques. All TKA surgeries were conducted under tourniquet. Intravenous antibiotics were given preoperation. A standard medial parapatellar approach, using patellar eversion, was taken in each case. In both the two groups, intramedullary instrumentation was used for femoral alignment and a 4°–6° valgus cut was used for all knees. Tibial cuts were conducted using extramedullary instrumentation, with 7° of posterior slope. Prostheses of both designs included NexGen CR-Flex TKA (Zimmer, Warsaw, Ind; CR-Flex) or NexGen Legacy PS TKA (Zimmer; LPS-Flex), respectively. All prostheses were fixed with cement, and patella was not resurfaced in either group.
Rehabilitation
Applied for at least 6 h per day, a continuous passive motion machine was used for each subject, starting on the second postoperative day. Also on postoperative day 2, active and passive range of motion were initiated, as well as ambulation with crutches or a walker twice a day with physical therapy supervision. The subjects used crutches or a walker with full weight-bearing for 6 weeks and used a cane as needed subsequently.
Clinical evaluation
Hospital for Special Surgery Score (HSSS), Knee Society Score (KSS), including the Mean Knee Score (MKS) and the Mean Function Score (MFS), as well as SF12 Score (Mental Health Score and Physical Health Score involved) were assessed preoperatively and at 24 months postoperatively by independent nurse practitioners.
To compare the two groups with regard to ROM, we measured the arcs of maximal non-weight-bearing passive flexion and weight-bearing flexion, as well as the numbers of joints which allowed comfortable cross-legged sitting and kneeling. Non-weight-bearing flexion was evaluated with the subject in the supine position, and with use of a goniometer, weight-bearing flexion was investigated during a lunge activity. One arm of the goniometer was placed parallel to the shaft of the femur (which was estimated from the location of the greater trochanter and the lateral femoral condyle), and the other arm of the goniometer was placed parallel to the shaft of the tibia (which was estimated from the fibular head and the lateral malleolus).
Position of individual prosthesis as well as location of radiolucent lines at the cement bone interface were detected in accordance to the guidelines of Knee Society. The aseptic loosening was diagnosed by progressive lucency of >2 mm surrounding the entire circumference of prosthesis [17], change in alignment of the prosthesis or subsidence of component as compared with its previous status. Patellar tilt, subluxation or dislocation if any was evaluated by the skyline patellar view.
Statistical analysis
Results were analyzed statistically using a statistical software package. The differences in the functional outcome and ROM between the two groups were analyzed using the non-paired. Student’s t test. Results in the same group at different time points were analyzed using the paired Student’s t test. Chi square test was used to evaluate overall complication rates and incidence of radiolucent lines in two groups. Differences of P < 0.05 were considered statistically significant.
Results
Demographic data
Demographic data were displayed in Table 1. A total of 67 patients who were enrolled in this retrospective comparative study, and 62 subjects were available for the 24-month follow-up. In Group I, there were 30 subjects (16 men and 14 women) and the mean age was 65.7 years (range 60–71 years). The dominant leg was affected in 15 subjects. In Group II, there were 32 subjects (16 men and 16 women) and the mean age was 67.1 years (range 63–69 years). The dominant leg was affected in 16 patients. No significant differences with regard to demographics were detected when the two groups were compared.
Functional outcome
Functional outcome was summarized in Table 2. The mean HSSS was 74.1 ± 3.12 (50.3–89.9) for Group I, and 79.1 ± 7.31 (51.5–88.7) for Group II at 24-month follow-up, no significant difference was detected between the two groups. As far as Knee Society Score is concerned, the mean MKS was 91.4 ± 7.7 (70.6–98.1) for Group I, and 90.9 ± 7.9 (74.6–97.2) for Group II at 24-month follow-up, no significant difference was detected between the two groups in terms MKS. The mean MFS Score at 24-month follow-up was 92.3 ± 4.2 (75.7–98.9) for Group I, and 90.2 ± 6.7 (77.5–96.2) for Group II, no significant difference was evident between the two groups with regard to MCS. The SF-12 health survey was used to measure the patients’ general health status. Values for each period were presented in the SF-36 physical component summary (PCS) and mental component summary (MCS) scores. The mean PCS Score at 24-month follow-up was 48.5 ± 7.6 (25.9–70.2) for Group I, and 49.1 ± 6.9 (23.7–71.0) for Group II, no significant difference was evident between the two groups with regard to PCS. The mean MCS Score at 24-month follow-up was 57.1 ± 5.5 (34.1–72.3) for Group I, and 54.3 ± 7.1 (35.5–74.2) for Group II, no significant difference was detected between the two groups in terms of MCS.
Range of motion
The preoperative maximal flexion and flexion contracture in Group I (mean 133.7° ± 12.1° and 7.9° ± 0.8°, respectively) and Group II (mean 132.3° ± 10.7° and 8.1° ± 0.4°, respectively) were similar (P > 0.05). At the time of the 24-month follow-up, the mean non-weight-bearing maximal flexion in Group I and Group II (136.2° ± 7.1° and 135.1° ± 9.5°, respectively) was similar (P > 0.05) (Table 3). Moreover, there was no significant difference between the two groups regarding to the average amount of weight-bearing maximal flexion at 24-month follow-up (P > 0.05) (Table 3). Twelve knees (40 %) in Group I and twelve knees (38 %) in Group II allowed the subjects to kneel comfortably. Twenty-two knees (73 %) in Group I and twenty-one knees (65 %) in Group II allowed comfortable cross-legged sitting. However, there was no significant difference between the two groups in terms of kneeling (P > 0.05) or cross-legged sitting (P > 0.05) (Table 3).
Complication
Two knees in the Group I and 2 knees in Group II developed persistent discharge from the wound within the early after-operative period (average 4th to 5th day), There was no significant difference between the two groups in terms of persistent discharge from the wound (P > 0.05) (Table 4).
At 24-month follow-up, the incidence of anterior knee pain was 10 and 8 % in Group I and Group II, respectively. No significant difference was detected (Table 4).
No evidence of dislocation of bearing or massive osteolysis (lesions of more than 1 cm), as well as aseptic loosening (progressive lucency of >2 mm) was detected in either group till 24-month follow-up (Table 4). Four knees, two in Group I and two in Group II, had a pre-operative flexion deformity of an average 14° (range from 4° to 28°). A mean flexion formity of 4° (range from 3° to 6°) persisted in Group I as well as in Group II. All these four subjects were managed with skin foam traction during night and active mobilization during day.
Discussion
A variety of designs have been introduced to recreate physiological knee joint kinematics to improve function without sacrificing prosthesis durability. The functional reproduction or anatomical preservation of the PCL is established as one of the kinematic pillars. Controversy regarding which option is best exists. Proponents of CR designs cite the potential advantages of preservation of bone, more normal knee kinematics, increased proprioception, femoral rollback on the tibia during flexion, and greater stabilization of the prosthesis, with the PCL preventing anterior translation of the femur on the tibia. On the contrary, PS advocates argue a more stable component interface, less technically demanding procedure, as well as increased range of motion.
Recently, high-flexion PS and high-flexion CR total knee arthroplasties which incorporate design features were introduced, aiming to improve knee kinematics in high flexion. Prosthesis of both designs included NexGen CR-Flex TKA (Zimmer) or NexGen Legacy PS TKA (Zimmer), respectively. The femoral posterior aspect of the prosthesis of the PS-Flex was 2 mm thicker than that of the CR-Flex, and a 2-mm thicker bone resection at femoral posterior condyle was required in the PS-Flex, which resulted in maintaining the same degree of the femoral posterior offset in both the CR-Flex and the PS-Flex prosthesis. Seon et al. [15] investigated the outcomes in TKA using high-flexion PS and the high-flexion CR prosthesis. They concluded that high-flexion PS TKA provided greater weight-bearing maximal flexion and posterior femoral rollback than high-flexion CR TKA, although no difference in clinical outcomes was observed between the two designs after a minimum duration of follow-up of 24 months. Yagishita et al. [13] performed a prospective, randomized control study for evaluation of the superiority of these designs. Their results showed that the postoperative range of motion in the high-flexion PS design was significantly greater than that of the high-flexion CR design, and there was a significant difference in patient satisfaction between the high-flexion CR and high-flexion PS designs. We performed a retrospective study for comparison with the high-flexion CR and the high-flexion PS with a follow-up duration of 24 months. The results of our present study demonstrated that the high-flexion PS and the high-flexion CR designs are similar with regarding to the amount of flexion as well as functional outcome. The mean maximal flexion for the high-flexion PS and high-flexion CR designs was similar under passive non-weight-bearing conditions. These results were different from those of the report of Yagishita et al. [13] and Seon et al. [15]. In the present work, the femoral posterior aspect of the design of the high-flexion PS is about 2 mm thicker than that of the high-flexion CR, and a 2-mm thicker bone resection at femoral posterior condyle is required in the high-flexion PS, which can result in maintaining the same degree of the femoral posterior offset in both the high-flexion PS and the high-flexion CR design.
Low BMI of the subjects in the present study may have contributed to the high levels of flexion achieved in both the two groups. Deep flexion is essential to perform key routine activities, such as squatting, kneeling, sitting with both legs crossed, gardening and bathing. Our results demonstrated that no significant difference with regard to maximal weight-bearing flexion was detected between the two groups. Both the two groups displayed smaller flexion during weight-bearing as compared to non-weight-bearing conditions, and this was comparable in both the two groups. The smaller flexion under the weight-bearing condition as compared to non-weight-bearing in knees implanted with high-flexion CR designs is believed to occur due to the abnormal knee kinematics caused by decreased femoral rollback [13, 15, 18, 19]. It has been indicated that, in the CR TKA, the femorotibial contact is translated anteriorly with increasing knee flexion [13, 15, 18, 19]. There was no significant difference in terms of the number of knees in the two groups that allowed the subject to kneel or to sit cross-legged. The results of our present work are consistent with the report of Cho et al. [20].
Two knees in the high-flexion CR group and two knee in high-flexion PS group developed persistent discharge from the wound within the early after-operative period. All these four subjects were taken into the operating theatre for debridement and irrigation of joints involved. Samples were collected from the joints and then were sent for culture and sensitivity. Subjects were continued on intravenous antibiotics for 14 days. Culture reports from all the three knees were sterile, and subjects were detected for any possible coagulation defects. The incidence of wound complication with the numbers available is not significantly different on statistical parameters (P > 0.05) (Table 4).
Early aseptic loosening, as a common consequence of high flexion prosthesis, has already been assessed in the literature [21, 22]. For instance, Han et al. [21] demonstrated that in a series of forty-seven knees implanted with high flexion prosthesis, the incidence of early aseptic loosening was about 38 % at early follow-up, and 15 of the subjects underwent revision TKA at a mean of 23 months. They also detected that subjects with aseptic loosening possessed statistically significant greater ROM and ability to kneel, squat as well as sit cross-legged when compared to standard designs. They stated that aseptic loosening was a consequence of deep flexion, where the femoral component remained on the posterior edge of the polyethylene liner and caused asymmetrical loading in the medial and lateral compartments. In contrast to the study of Han et al. [21], there were no subjects in our present study with radiographic evidence of aseptic loosening (progressive lucency of >2 mm) at 24-month follow-up. The fact that no subject had radiographic evidence of aseptic loosening in our present study is consistent with current literature [22, 23, 24]. This phenomenon reinforces the notion that the high incidence of aseptic loosening in the study of Han et al. [21] is an outlier, and may be associated with surgical technique rather than prosthetic design.
Although we aim to perform a well-designed study, some potential limitations must be acknowledged. The first limitation of our study involves the retrospective nature of this study. Prospective, randomized study designs achieve higher degrees of evidence. Second, the number of patients was small, and the results might be different from studies with larger sample sizes. Third, the follow-up period was only 24 months. Therefore, at the present time, the authors cannot speculate whether there will be differences between the two groups in regard to long-term outcome. In the future, the authors should conduct a long-term follow-up study to compare the clinical results of the two groups.
Conclusion
We conclude that there is no difference in terms of functional outcome, range of motion as well as complications between patients who received a high-flexion cruciate-retaining or a high-flexion posterior-substituting prosthesis TKA at the 24-month follow-up. Investigations assessing midterm and long-term follow-up are necessary, as differences may be seen in the long term. One can expect a satisfactory outcome at the 24-month follow-up with either one of both prosthesis, if used properly.
References
Schroer WC, Stormont DM, Pietrzak WS (2014) Seven-year survivorship and functional outcomes of the high-flexion vanguard complete knee system. J Arthroplasty 29(1):61–65
Fischer M, von Eisenhart-Rothe R, Simank HG (2013) Comparable short-term results seen with standard and high-flexion knee arthroplasty designs in European patients. J Orthop 10(3):119–122
van de Groes S, de Waal-Malefijt M, Verdonschot N (2014) Probability of mechanical loosening of the femoral component in high flexion total knee arthroplasty can be reduced by rather simple surgical techniques. Knee 21(1):209–215
Guild GN 3rd, Labib SA (2014) Clinical outcomes in high flexion total knee arthroplasty were not superior to standard posterior stabilized total knee arthroplasty. A multicenter, prospective, randomized study. J Arthroplasty 29(3):530–534
Luo SX, Su W, Zhao JM, Sha K, Wei QJ, Li XF (2011) High-flexion vs conventional prostheses total knee arthroplasty: a meta-analysis. J Arthroplasty 26(6):847–854
Long WJ, Scuderi GR (2008) High-flexion total knee arthroplasty. J Arthroplasty 23(7):6–10
Luo SX, Zhao JM, Su W, Li XF, Dong GF (2012) Posterior cruciate substituting versus posterior cruciate retaining total knee arthroplasty prostheses: a meta-analysis. Knee 19(4):246–252
Most E, Zayontz S, Li G, Otterberg E, Sabbag K, Rubash HE (2003) Femoral rollback after cruciate-retaining and stabilizing total knee arthroplasty. Clin Orthop Relat Res 410:101–113
Sierra RJ, Berry DJ (2008) Surgical technique differences between posterior-substituting and cruciate-retaining total knee arthroplasty. J Arthroplasty 23(7):20–23
Incavo SJ, Mullins ER, Coughlin KM, Banks S, Banks A, Beynnon BD (2004) Tibiofemoral kinematic analysis of kneeling after total knee arthroplasty. J Arthroplasty 19(7):906–910
Song EK, Park SJ, Yoon TR, Park KS, Seo HY, Seon JK (2012) Hi-flexion and gender-specific designs fail to provide significant increases in range of motion during cruciate-retaining total knee arthroplasty. J Arthroplasty 27(6):1081–1084
Minoda Y, Aihara M, Sakawa A, Fukuoka S, Hayakawa K, Ohzono K (2012) Range of motion of standard and high-flexion cruciate retaining total knee prostheses. J Arthroplasty 24(5):674–680
Yagishita K, Muneta T, Ju YJ, Morito T, Yamazaki J, Sekiya I (2012) High-flex posterior cruciate-retaining vs posterior cruciate-substituting designs in simultaneous bilateral total knee arthroplasty: a prospective, randomized study. J Arthroplasty 27(3):368–374
Cates HE, Komistek RD, Mahfouz MR, Schmidt MA, Anderle M (2008) In vivo comparison of knee kinematics for subjects having either a posterior stabilized or cruciate retaining high-flexion total knee arthroplasty. J Arthroplasty 23(7):1057–1067
Seon JK, Park JK, Shin YJ, Seo HY, Lee KB, Song EK (2011) Comparisons of kinematics and range of motion in high-flexion total knee arthroplasty: cruciate retaining vs. substituting designs. Knee Surg Sports Traumatol Arthrosc 19(12):2016–2022
Seon JK, Park SJ, Lee KB, Yoon TR, Kozanek M, Song EK (2009) Range of motion in total knee arthroplasty: a prospective comparison of high-flexion and standard cruciate-retaining designs. J Bone Joint Surg Am 91(3):672–679
Thadani PJ, Vince KG, Ortaaslan SG, Blackburn DC, Cudiamat CV (2000) Ten- to 12-year followup of the Insall-Burstein I total knee prosthesis. Clin Orthop Relat Res 380:17–29
van Stralen RA, Anderson PG, Wymenga AB (2013) The self-aligning knee prosthesis: clinical and radiological outcome and survival analysis of a cruciate retaining meniscal bearing knee at 10-year follow-up. Knee Surg Sports Traumatol Arthrosc [Epub ahead of print]
Peters CL, Mulkey P, Erickson J, Anderson MB, Pelt CE (2014) Comparison of total knee arthroplasty with highly congruent anterior-stabilized bearings versus a cruciate-retaining design. Clin Orthop Relat Res 472(1):175–180
Cho SH, Ha YC, Song HR, Jeong ST, Park HB, Hwang SC, Kim JS (2004) High flex knee arthroplasty and range of motion. J Korean Orthop Assoc 39:662–667
Han HS, Kang SB, Yoon KS (2007) High incidence of loosening of the femoral component in legacy posterior stabilised-flex total knee replacement. J Bone Joint Surg Br 89(11):1457–1461
Zelle J, Janssen D, Van Eijden J (2011) Does high-flexion total knee arthroplasty promote early loosening of the femoral component? J Orthop Res 29(7):976–983
Lee BS, Chung JW, Kim JM (2013) High-flexion prosthesis improves function of TKA in Asian patients without decreasing early survivorship. Clin Orthop Relat Res 471(5):1504–1511
Bin SI, Nam TS (2007) Early results of high-flex total knee arthroplasty: comparison study at 1 year after surgery. Knee Surg Sports Traumatol Arthrosc 15:350–355
Conflict of interest
None of the authors received payment or services from a third part in support of any aspect of this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Z., Zhu, W. & Zhang, W. High-flexion posterior-substituting versus cruciate-retaining prosthesis in total knee arthroplasty: functional outcome, range of motion and complication comparison. Arch Orthop Trauma Surg 135, 119–124 (2015). https://doi.org/10.1007/s00402-014-2107-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-2107-4