Abstract
Purpose
This study aims to determine whether outcomes following vertebroplasty with high viscosity cement are superior to low viscosity cement and non-inferior to kyphoplasty in the setting of vertebral compression fractures.
Methods
We searched for randomized controlled trials and cohort studies assessing cement leakage rate in adult patients with VCFs who underwent vertebroplasty with high (HVCV) or low viscosity cement (LVCV) augmentation, or kyphoplasty (KP) in PubMed, Embase, Ovid, The Cochrane Library, and Web of Science from inception up to December 2019. Two authors extracted data and appraised risk of bias. We performed pairwise meta-analyses in R to compare differences between three treatments and network meta-analysis using frequentist random-effects models for indirect comparison. We used P-score to rate the overall certainty of evidence. The primary outcome was cement leakage rate.
Results
Five RCTs and eight cohort studies with 840 patients and a total of 1280 vertebral bodies were included in the systematic review and network meta-analysis. Compared to LVCV, the relative risk for cement leakage following HVCV and KP was 0.42 (95% CI 0.28–0.61) and 0.83 (95% CI 0.40–1.68), respectively. Our pooled results suggested that HVCV (P-score = 0.99) was better than KP (P-score = 0.36) in cement leakage rate.
Conclusions
The present network meta-analysis demonstrated that HVCV may be associated with lower risk of cement leakage among patients with VCFs as compared to other augmentation techniques. Future prospective studies will validate the findings of this analysis and further elucidate the risk of symptomatic cement leakage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vertebral compression fractures (VCFs) lead to severe back pain, loss of mobility, spinal deformities, neural compromise, and even paralysis [1]. The most common cause of vertebral compression fracture is due to osteoporosis [2]. By 2025, 3 million osteoporotic fractures and $25 billion in related health care costs will occur in the USA [3]. Of these, vertebral compression fractures account for one-fourth of all osteoporosis-related fractures [4].
Percutaneous vertebroplasty (PVP) and kyphoplasty (KP) are preferred procedures in treating vertebral compression fractures due to faster recovery, pain relief, and restoration of vertebral height [4]. However, cement leakage remains an important complication following these procedures with an incidence rate as high as 63–87% reported in the literature [5]. Cement extravasation can occur through fracture fissures or through the vertebral vein fissures [2]. This may result in infection, paralysis, vessel damage, pulmonary embolism, or even death [2]. Several studies have shown that cement viscosity is the main factor determining cement leakage [6,7,8,9,10,11,12,13,14,15,16,17,18]. High viscosity cement product softens faster, requires less mixing time, provides a more sufficient working phase [19], and thus reduces the chance of extravasation. Kyphoplasty, on the other hand, has also been suggested to be a solution to this issue.
Direct comparison between high viscosity cement vertebroplasty and kyphoplasty has been sparsely reported in the literature. In the relative absence of direct comparisons, network meta-analyses offer a potential solution by allowing pooling of both direct and indirect evidence, thus allowing for more precise estimation of effect sizes. Hence, the aim of this study was to perform a systematic review and network meta-analysis to compare the rate of cement leakage following high viscosity cement vertebroplasty, low viscosity cement vertebroplasty and kyphoplasty.
Methods
Research protocol and search question
The search protocol was based on the following PICO question: for patients with vertebral compression fractures (population of interest), does vertebroplasty with high viscosity cement augmentation provide lower cement leakage rate compared to vertebroplasty with low viscosity cement augmentation (comparator) and kyphoplasty (comparator). The review protocol was developed as indicated by the PRISMA statement guidelines and was registered with PROSPERO (ID: CRD42020187185). Both cohort studies and randomized controlled studies were included.
Eligibility criteria and primary outcome
Studies were eligible if they met the following criteria: (1) included patients with vertebral compression fractures who underwent vertebroplasty or kyphoplasty; (2) provided information on cement viscosity used in augmentation; (3) observational or interventional studies published in the English language till December 2019; and (4) reported the primary outcome of interest: cement leakage rate (defined as number of leakage levels/fractured vertebral levels). Relevant exclusion criteria included: (1) single-arm follow-up studies, case reports, case series, reviews, basic science experiments, and animal or cadaver studies; (2) studies including vertebral compression fractures caused by infection or immunosuppression; (3) conference abstracts.
Search strategy and study selection
We searched PubMed, Embase, Ovid, The Cochrane Library, and Web of Science for articles in a systematic approach utilizing the combination of keyword and Medical Subject Heading (MeSH) terms adjusted for each database. The most recent search was performed on 7 January 2020. Recursive search using bibliographies of obtained articles was also performed.
Two reviewers independently evaluated titles and abstracts for eligibility and full-text evaluation. All disagreements between reviewers were resolved through discussion.
Data collection and quality assessment
The following data were extracted by two reviewers: study characteristics (author, year of publication, region of study, data source, study design, period of study), study arms, sample size, patient age, cement leakage rate, complications from cement leakage, inclusion criteria of each study, and the specific definition of each treatment arm.
Risk of bias and study quality was assessed by two reviewers independently using Newcastle–Ottawa Scale, while GRADE assessment was performed to evaluate confidence in effect estimates. All discrepancies were resolved by discussion.
Statistical analysis and quantitative data synthesis
We performed network meta-analysis using the “netmeta” statistical package (version 1.2-0, https://cran.r-project.org/web/packages/netmeta/index.html) [20, 21] in R (R version 3.6.0) and estimated network meta-analysis models with a frequentist approach derived from graph theoretical methods [22]. The raw data were transformed into a contrast-based format and was used to estimate the relative risk and 95% CI for each pairwise comparison. We used these data to conduct a network meta-analysis using random-effects modelling by adding the estimated heterogeneity τ2, based on the Dersimonian–Laird estimator [23], to the variance of each comparison. Direct comparisons were depicted in the form of network graphs, with vertices demonstrating treatments and thickness of edges corresponding to number of studies. Comparison-adjusted funnel plots were constructed to assess publication bias and small study effects [24].
As for binary outcome assessment, we calculated a pooled relative risk with 95% CI to summarize the relative efficacy of each treatment. The results were visualized using forest plot with LVCV as the reference group. Ranking of treatment was generated using P-score, which has been shown to be equivalent to the SUCRA score [25], ranging from 0 to 1. A higher P-score indicates a higher probability of being the best treatment option. Forest plots were divided into a direct, indirect, and network estimate to evaluate the consistency between direct and indirect evidence in our network meta-analysis. Since I2 value was found to increase with larger pooled samples [26], we used τ2 to measure heterogeneity, with 0.04, 0.16, and 0.36 corresponding to a low, moderate, and high degree of heterogeneity, respectively [27]. We further performed subgroup analyses based on treatment comparison to evaluate heterogeneity within studies. Sensitivity analyses were also performed in the presence of publication bias, significant heterogeneity, or estimate effect size in different diagnosis groups.
Results
Literature search and selection process
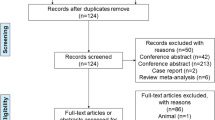
A total of 280 articles were identified through database searching. After removal of duplicates and screening for titles and abstracts, 28 full-text articles were reviewed for eligibility, with 13 studies included for quantitative synthesis (Fig. 1).
Study characteristics
Our network meta-analysis included five randomized controlled trials and eight cohort studies (two prospective, six retrospective) with a total of 840 patients. Across studies, the mean patient age ranged between 65 and 80 years, and while on average, 70% were females (range 44–93%) (Table 1). The included studies were conducted in China (7 studies, n = 575) [9, 13,14,15,16, 18], Italy (2 studies, n = 74) [7, 10], USA (1 study, n = 80) [8], Germany (1 study, n = 60) [6], Greece (1 study, n = 47) [12], and Netherlands (1 study, n = 64) [11]. Eleven articles included patients with osteoporotic VCF (OVCF), others included VCF caused by multiple myeloma [10], other malignant tumours [12], and symptomatic angioma (Table 2) [7]. All studies were active comparator, with eight articles comparing HVCV and LVCV [6, 7, 9, 11, 14, 16,17,18], three comparing HVCV and KP [8, 13, 15], and two comparing KP and LVCV [10, 12]. Inclusion criteria, criteria used to determine cement leakage, and follow-up period for each individual study are listed in Supplemental Table 1.
Cohort description and treatment definition
In one of the eight studies comparing HVCV to LVCV, the authors used medium viscosity cement: Disc-O-Tech (Disc-O-Tech Medical Technologies Ltd., Israel) [11]. In one of the three studies comparing HVCV to kyphoplasty, the author used radiofrequency targeted vertebral augmentation (RF-TVA) instead of original vertebroplasty [8]. In one of the two studies comparing KP to LVCV, the authors utilized high viscosity cement (HVC) in the KP arm [12]. Table 1 summarizes treatment details, while product and brand of cement used in each study are summarized in Table 2. In HVCV arm, five studies used Confidence delivery system [6, 7, 13, 15, 17], and three studies used Heraeus product [9, 14, 18]. Further details for definition of HVC as provided in each study are shown in Supplemental Table 2.
Methodological quality and assessment of risk of bias
The methodological quality of included studies was assessed using Newcastle–Ottawa Quality Assessment Scale (Supplemental Table 4). Strength of evidence was assessed using the GRADE approach; confidence in estimates was found to be moderate (Supplemental Table 5). Network graph demonstrated the structure of our network meta-analysis, with width of the edge corresponding to number of studies (Supplemental Fig. 1). When the data were pooled, moderate heterogeneity was observed (τ2 = 0.22), and no significant inconsistency was noted between treatment designs (P = 0.95). Subgroup analysis revealed low heterogeneity for “HVCV versus LVCV” and “HVCV versus KP” pairwise comparisons (τ2 = 0.09 and 0.07, respectively) and high heterogeneity for “KP versus LVCV” (τ2 = 1.59) (Fig. 2). Egger’s test revealed significant asymmetry (P = 0.03), indicating the presence of publication bias (Supplemental Fig. 2).
Cement leakage rate
Cement extravasation was detected using X-ray or computed tomography or both in the included studies (Supplemental Table1). Crude cement leakage rate for HVCV, LVCV, and KP was 0.24, 0.57, and 0.19, respectively. Table 3 summarizes the rate of cement leakage reported by each study. Effect estimates from direct and network comparisons, along with the ranking of treatment, are summarized in Table 4, while Fig. 3 demonstrates consistency in direct, indirect, and network comparisons. HVCV was found to have a lower risk of cement leakage than LVCV by direct comparison (RR = 0.40; 95% CI = 0.28–0.61). However, indirect pairwise comparisons did not reveal a significant difference between any treatment. After pooling direct and indirect estimates, HVCV was found to be associated with lower leakage as compared to KP (RR = 0.51; 95% CI = 0.26–0.98). HVCV was also associated with a lower risk of cement leakage as compared to LVCV (RR = 0.42; 95% CI = 0.28–0.61) and was ranked first (P-score = 0.99) among all three treatments (Fig. 4). KP was associated with lower cement leakage as compared to LVCV but was not statistically significant (RR = 0.83; 95% CI = 0.40–1.68) and was ranked second (P-score = 0.36). Most studies reported higher rate of complications related to cement leakage following LVCV (Supplemental Table 3).
Sensitivity analyses
We performed sensitivity analysis after determination of publication bias (exclusion of one study comparing MVCV to LVCV [11]). The treatment ranking remained the same, with P-score of 1.00, 0.47, and 0.03, respectively (Supplemental Fig. 3). We further excluded Georgy 2013 [8] (comparing RF-TVA to KP) and Korovessis 2014 [12] (comparing KP to Kiva with LVC) to conduct more precise sensitivity analyses. No significant heterogeneity or inconsistency was found, and the ranking of treatment remained the same, with P-scores of 0.99, 0.49, 0.02, respectively (Supplemental Fig. 4). To find out whether cohort studies influenced the result, sensitivity analysis including only RCTs was performed, which showed HVCV provided the lowest cement leakage rate (Supplemental Fig. 5). Similar results were found in sensitivity analyses with studies including OVCF patients only (Supplemental Fig. 6), studies utilizing Confidence product in HVCV cohort only (Supplemental Fig. 7), and following exclusion of studies using RF-TVA in HVCV group (Supplemental Fig. 8).
Discussion
Although direct and indirect comparisons were not significant due to scarcity of studies, our study generated network effects and demonstrated that the risk for cement leakage seems to be higher following kyphoplasty as compared to HVC vertebral augmentation. This is the first network meta-analysis to indirectly compare kyphoplasty versus vertebroplasty with high viscosity cement augmentation. Studies have shown a higher risk of cement leakage due to intravertebral cleft, cortical disruption, low cement viscosity, and high volume of injected cement [28].
Yeom et al. [29] described cement leakage and classified it into three types: via basivertebral vein, via segmental vein, and through cortical defect and revealed that cortical fracture of the vertebral body is the main cause of leakage. Lower viscosity cement would have higher propensity to leak through an endplate fracture [30].
HVC, due to a low Reynolds number, stabilizes the forces underlying cement flow, thus spreading more uniformly than low viscosity cements that follow the path of least resistance [31]. The current literature shows significant heterogeneity in the definition of high and low viscosity cement. Some define HVC according to manufacturer’s classification, while other studies base it on the surgeon’s subjective definition. Among HVC products, there remains a significant variability in the commercial brand utilized [6,7,8,9, 14,15,16,17]. Variation in brands may be responsible for differences in working time to achieve high viscosity from one product compared to another. Confidence (Depuy) showed a working time at a high viscosity for 9 min immediately after mixing [32], while Osteopal (Heraeus) has a working time ranging from 1.5 min to 11 min depending on room temperature [33]. Variability in working times might be responsible for differences observed in rate of cement leakage. On the other hand, surgeon protocol for HVC, if not using a HVC product, may or may not have been provided in detail in each study. The lack of a clear definition might have decreased objectiveness and generalizability and may have also influenced the differences observed in cement leakage rates. Although HVCV has lower cement leakage from our direct and indirect evidence, LVCV may also have advantages such as increased middle vertebral body height [13], equivalent pain relief [16], and similar improvement in ODI score as compared to HVCV [9].
Most of the studies (a total of 8) comparing HVC to LVCs found that high viscosity cement (HVC) has reduced leakage rate compared with low viscosity cement (LVC). However, there was a variability observed in the location of leakage. Zhang et al. and Wang et al. [15, 17] reported a lower leakage rate of cement in the disc space, but not the epidural space, paravertebral area, and peripheral vein. Further, Zhang et al. [18] showed that HVC reduced leakage within the paravertebral area and vein but not the disc or intraspinal space. Anselmetti et al. [7] indicated that the leakages in the vein and the disc space were also significantly lower with HVC as compared to LVC. The advantage of KP is the ability to restore vertebral height through destruction of the trabeculae and expanding the segment with a balloon before adding the cement, allowing a potentially better reduction of the fracture [34]. This, however, might increase operative time as compared to vertebroplasty alone [35]. Chen et al. [1] also demonstrated higher subsequent vertebral compression fractures following kyphoplasty. While our results demonstrate that HVCV provided the lowest cement leakage rate, available evidence also indicates it may also be associated with fewer complications related to cement leakage as compared to KP [15]. Also, the shorter operative time following HVCV may allow time to tackle serious complications associated with cement leakage. The procedural cost is also an important consideration for decision-making.
Three studies directly compared HVCV to kyphoplasty. All studies had a minimum of 1-year follow-up data available for comparison [8, 13, 15]. Only Wang et al. [10, 12] showed a decreased cement leakage from high viscosity cement vertebroplasty compared to kyphoplasty [15]. Differences in primary pathology (neoplastic as compared to osteoporosis) must also be taken into consideration for interpretation of these results. Only two studies directly compared LVCV to kyphoplasty and demonstrated that LVCV was non-inferior to kyphoplasty in rate of cement leakage. Korovessis et al. [12] demonstrated similar leakage rates with Kiva implant (low viscosity PMMA) compared to balloon kyphoplasty among patients with spinal metastasis. LaMada et al. [10] showed similar cement leakage in multiple myeloma patients.
Due to the lack of studies directly comparing HVCV and kyphoplasty, our aim was to pool the limited evidence from the literature to allow a network comparison. Different techniques have been described to prevent cement leakage in the literature. Besides the use of high viscosity cement, radiopaque substances, such as tungsten, tantalum powder, barium sulphate, or zirconium dioxide, can be added to PMMA, to improve fluoroscopic visualization as well as monitor any potential cement extravasation [36]. Another technique described is the eggshell procedure: after reduction with the KP balloon, a small amount of doughy cement is injected into the cavity, and then the balloon is reinserted and reinflated. Once the cement hardens, the cavity can be filled with cement, whose leak is prevented by the eggshell structure [37].
The complexity of cement leakage includes not only the technique, but also yield stress, viscoelastic properties, and/or cohesiveness of the fluid. Besides viscosity as a primary factor for cement leakage, the injection device and technique also are important factors for leakage. It is described that the diffusion of cement within the vertebral body should be a “uniformly expanding cloud” rather than the “fingers of a glove”, which indicates uncontrolled spread due along paths of lower resistance in the vertebral body [31]. In vitro experiments have demonstrated that HVC may achieve this more effectively [38].
Strengths and limitations
Most of the existing studies provided pairwise comparisons only. Our network meta-analysis leveraged direct and indirect evidence to perform multiple treatment comparison and addressed the current paucity of evidence comparing HVCV and KP. The systematic search strategy allowed us to identify qualified articles and to summarize surgical technique as well as brands of cement used in the procedure.
However, the patient population included in our study implied a certain heterogeneity. Although most patients were operated due to OVCF, some were operated for tumour metastasis, multiple myeloma, or symptomatic angioma. We attempted to address this using sensitivity analyses, which demonstrated consistent results. Among studies comprised of OVCF patients, two included patients with severe OVCF: defined as the vertebral body collapsed to less than one-third of the original height. Besides, specific nuances in treatment procedure, chosen cement, and operative setting could also impact the final outcome. Lastly, although we included five randomized controlled trials, it was nearly impossible to accomplish truly blinded randomization for both operator and patient. Nevertheless, our study did illustrate promising findings and paved the road for further prospective studies in the future.
Conclusion
Our network meta-analysis demonstrated that HVCV, compared with other treatment options, has the lowest relative risk of cement leakage for patients with vertebral compression fractures. Similar results were found in sensitivity analyses, with lower heterogeneity and inconsistency. Future prospective studies will validate these findings and further elucidate if HVCV may be superior to KP.
Abbreviations
- CI:
-
Confidence interval
- HVC:
-
High viscosity cement
- HVCV:
-
High viscosity cement vertebroplasty
- KP:
-
Kyphoplasty
- LVC:
-
Low viscosity cement
- LVCV:
-
Low viscosity cement vertebroplasty
- MCVC:
-
Medium viscosity cement vertebroplasty
- MM:
-
Multiple myeloma
- ODI:
-
Oswestry Disability Index
- OVCF:
-
Osteoporotic vertebral compression fracture
- PMMA:
-
Polymethyl methacrylate
- PVP:
-
Percutaneous vertebroplasty
- RF-TVA:
-
Radiofrequency targeted vertebral augmentation
- RR:
-
Relative risk
- VCF:
-
Vertebral compression fracture
References
Chen AT, Cohen DB, Skolasky RL (2013) Impact of nonoperative treatment, vertebroplasty, and kyphoplasty on survival and morbidity after vertebral compression fracture in the medicare population. J Bone Jt Surg - Ser A 95:1729–1736. https://doi.org/10.2106/JBJS.K.01649
Garfin SR, Yuan HA, Reiley MA (2001) New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine 26:1511–1515. https://doi.org/10.1097/00007632-200107150-00002
Cauley JA (2013) Public health impact of osteoporosis. J Gerontol A Biol Sci Med Sci 68(10):1243–1251. https://doi.org/10.1093/gerona/glt093
Burge R, Dawson-Hughes B, Solomon DH et al (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475. https://doi.org/10.1359/jbmr.061113
Schmidt R, Cakir B, Mattes T et al (2005) Cement leakage during vertebroplasty: an underestimated problem? Eur Spine J 14:466–473. https://doi.org/10.1007/s00586-004-0839-5
Alhashash M, Shousha M, Barakat AS, Boehm H (2019) Effects of polymethylmethacrylate cement viscosity and bone porosity on cement leakage and new vertebral fractures after percutaneous vertebroplasty: a prospective study. Glob Spine J 9:754–760. https://doi.org/10.1177/2192568219830327
Anselmetti GC, Zoarski G, Manca A et al (2008) Percutaneous vertebroplasty and bone cement leakage: clinical experience with a new high-viscosity bone cement and delivery system for vertebral augmentation in benign and malignant compression fractures. Cardiovasc Intervent Radiol 31:937–947. https://doi.org/10.1007/s00270-008-9324-6
Georgy BA (2013) Comparison between radiofrequency targeted vertebral augmentation and balloon kyphoplasty in the treatment of vertebral compression fractures: addressing factors that affect cement extravasation and distribution. Pain Physician 16:513–518
Guo Z, Wang W, Gao W-SS et al (2017) Comparison the clinical outcomes and complications of high-viscosity versus low-viscosity in osteoporotic vertebral compression fractures. Med United States)\ 96:2–6. https://doi.org/10.1097/MD.0000000000008936
La Maida GA, Giarratana LS, Acerbi A et al (2012) Cement leakage: Safety of minimally invasive surgical techniques in the treatment of multiple myeloma vertebral lesions. Eur Spine J 21:61–68. https://doi.org/10.1007/s00586-012-2221-3
Nieuwenhuijse MJ, Muijs SPJ, van Erkel AR, Dijkstra SPD (2010) A clinical comparative study on low vs. medium viscosity pmma bone cement in percutaneous vertebroplasty: viscosity associated with cement leakage. Spine J 10:S118–S119. https://doi.org/10.1016/j.spinee.2010.07.310
Korovessis P, Vardakastanis K, Vitsas V, Syrimpeis V (2014) Is Kiva implant advantageous to balloon kyphoplasty in treating osteolytic metastasis to the spine? comparison of 2 percutaneous minimal invasive spine techniques: a prospective randomized controlled short-term study. Spine 39:E231–E239. https://doi.org/10.1097/BRS.0000000000000112
Sun K, Liu Y, Peng H et al (2016) A comparative study of high-viscosity cement percutaneous vertebroplasty vs. low-viscosity cement percutaneous kyphoplasty for treatment of osteoporotic vertebral compression fractures. J Huazhong Univ Sci Technol - Med Sci 36:389–394. https://doi.org/10.1007/s11596-016-1597-4
Tang S, Fu W, Zhang HH et al (2019) Efficacy and safety of high-viscosity bone cement vertebroplasty in treatment of osteoporotic vertebral compression fractures with intravertebral cleft. World Neurosurg 132:e739–e745. https://doi.org/10.1016/j.wneu.2019.08.029
Wang C-HH, Ma J-ZZ, Zhang C-CC, Nie L (2015) Comparison of high-viscosity cement vertebroplasty and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Pain Physician 18:E187–E194
Zeng T-HH, Wang Y-MM, Yang X-JJ et al (2015) The clinical comparative study on high and low viscosity bone cement application in vertebroplasty. Int J Clin Exp Med 8:18855–18860
Zhang L, Wang J, Feng X et al (2015) A comparison of high viscosity bone cement and low viscosity bone cement vertebroplasty for severe osteoporotic vertebral compression fractures. Clin Neurol Neurosurg 129:10–16. https://doi.org/10.1016/j.clineuro.2014.11.018
Zhang fei Z-F, Yang long J-L, Jiang chang H-C et al (2017) An updated comparison of high- and low-viscosity cement vertebroplasty in the treatment of osteoporotic thoracolumbar vertebral compression fractures: a retrospective cohort study. Int J Surg 43:126–130. https://doi.org/10.1016/j.ijsu.2017.05.067
Vaishya R, Chauhan M, Vaish A (2013) Bone cement J Clin Orthop. J Clin Orthop Trauma 4:157–163. https://doi.org/10.1016/j.jcot.2013.11.005
Schwarzer G (2015) Package ‘ netmeta ’. https://cran.r-project.org/web/packages/netmeta/netmeta.pdf. Accessed 27 March 2020
Harrer M, Cuijpers P, Furukawa TA, Ebert DD (2019) Doing Meta-Analysis in R: A Hands-on Guide. doi:10.5281/zenodo.2551803
Rücker G (2012) Network meta-analysis, electrical networks and graph theory. Res Synth Methods 3:312–324. https://doi.org/10.1002/jrsm.1058
Jackson D, White IR, Riley RD (2013) A matrix-based method of moments for fitting the multivariate random effects model for meta-analysis and meta-regression. Biometrical J 55:231–245. https://doi.org/10.1002/bimj.201200152
Salanti G, Del Giovane C, Chaimani A et al (2014) Evaluating the quality of evidence from a network meta-analysis. PLoS ONE 9:e99682. https://doi.org/10.1371/journal.pone.0099682
Rücker G, Schwarzer G (2015) Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol 15:58. https://doi.org/10.1186/s12874-015-0060-8
Rücker G, Schwarzer G, Carpenter JR, Schumacher M (2008) Undue reliance on I(2) in assessing heterogeneity may mislead. BMC Med Res Methodol 8:79. https://doi.org/10.1186/1471-2288-8-79
Bruno R, da Costa PJ (2014) Systematic reviews and meta-analyses of randomized trials: principles and pitfalls. Eur Hear J 35(47):3336–3345. https://doi.org/10.1093/eurheartj/ehu424
Zhan Y, Jiang J, Liao H et al (2017) Risk factors for cement leakage after vertebroplasty or kyphoplasty: a meta-analysis of published evidence. World Neurosurg 101:633–642. https://doi.org/10.1016/j.wneu.2017.01.124
Yeom JS, Kim WJ, Choy WS et al (2003) Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Jt Surg Br 85:83–89. https://doi.org/10.1302/0301-620x.85b1.13026
Tanigawa N, Kariya S, Komemushi A et al (2009) Cement leakage in percutaneous vertebroplasty for osteoporotic compression fractures with or without intravertebral clefts. AJR Am J Roentgenol 193:W442–W445. https://doi.org/10.2214/AJR.09.2774
Baroud G, Crookshank M, Bohner M (2006) High-viscosity cement significantly enhances uniformity of cement filling in vertebroplasty: an experimental model and study on cement leakage. Spine 31:2562–2568. https://doi.org/10.1097/01.brs.0000240695.58651.62
Confidence; DePuy Spine, Raynham, MA. https://synthes.vo.llnwd.net/o16/LLNWMB8/US Mobile/Synthes North America/Product Support Materials/Brochures/Confidence Brochure VB01–00–001.pdf?fbclid=IwAR3Sw-JDGkNFa7XWo2P7PkioFZhB4gULGu-o6M8LRpov0s6izTVvfJX4ixY. Accessed 27 March 2020
Osteopal V, Heraeus Medical GmbH, Wehrheim, Germany. https://www.heraeus.com/media/media/hme/doc_hme/products_us/OSTEOPAL_V_IFU.pdf. Accessed 27 March 2020
Lador R, Liberman S, Ben-Galim P et al (2013) A cadaver study to compare vertebral augmentation with a high-viscosity cement to augmentation with conventional lower-viscosity cement. J Spinal Disord Tech 26:68–73. https://doi.org/10.1097/BSD.0b013e3182337d69
Chandra RV, Maingard J, Asadi H et al (2018) Vertebroplasty and kyphoplasty for osteoporotic vertebral fractures: what are the latest data? Am J Neuroradiol 39:798–806. https://doi.org/10.3174/ajnr.A5458
Lieberman IH, Togawa D, Kayanja MM (2005) Vertebroplasty and kyphoplasty: filler materials. Spine J 5:305S-316S. https://doi.org/10.1016/j.spinee.2005.02.020
Greene DL, Isaac R, Neuwirth M, Bitan FD (2007) The eggshell technique for prevention of cement leakage during kyphoplasty. J Spinal Disord Tech 20:229–232. https://doi.org/10.1097/01.bsd.0000211276.76024.30
Habib M, Serhan H, Marchek C, Baroud G (2010) Cement leakage and filling pattern study of low viscous vertebroplastic versus high viscous confidence cement. SAS J 4:26–33. https://doi.org/10.1016/j.esas.2010.01.001
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, W.C., Tsai, S.H.L., Goyal, A. et al. Comparison between vertebroplasty with high or low viscosity cement augmentation or kyphoplasty in cement leakage rate for patients with vertebral compression fracture: a systematic review and network meta-analysis. Eur Spine J 30, 2680–2690 (2021). https://doi.org/10.1007/s00586-020-06636-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06636-9