Abstract
Background
To compare high- versus low-viscosity bone cement on the clinical outcomes and complications in patients with Osteoporotic vertebral compression fractures (OVCFs) who underwent percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP).
Methods
PubMed, Embase, and the Cochrane Library were searched for papers published from inception up to February 2021 for potentially eligible studies comparing high- versus low-viscosity cement for PVP/PKP. The outcomes were the leakage rate, visual analog scale (VAS), and Oswestry Disability Index (ODI).
Results
Eight studies (558 patients; 279 in each group) were included. The meta-analysis showed that the leakage rate was lower with high-viscosity cement than with low-viscosity cement (OR = 0.23, 95%CI 0.14–0.39, P < 0.001; I2 = 43.5%, Pheterogeneity = 0.088); similar results were observed specifically for the disk space, paravertebral space, and peripheral vein, but there were no differences regarding the epidural space and intraspinal space. The VAS was decreased more significantly with high-viscosity cement than with low-viscosity cement (WMD = − 0.21, 95%CI − 0.38, − 0.04, P = 0.015; I2 = 0.0%, Pheterogeneity = 0.565). Regarding the ODI, there was no difference between high- and low-viscosity cement (WMD = − 0.88, 95%CI − 3.06, 1.29, P = 0.426; I2 = 78.3%, Pheterogeneity < 0.001).
Conclusions
There were lower cement leakage rates in PVP/PKP with high-viscosity bone cement than low-viscosity bone cement. The two groups have similar results in ODI, but the VAS scores favor high-viscosity bone cement. Therefore, the administration of high-viscosity bone cement in PVP/ PKP could be a potential option for improving the complications of leakage in OVCFs, while the clinical efficacy of relieving pain is not certain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis can lead to osteoporotic vertebral fractures (OVCFs) [1,2,3]. Because of the aging population, OVCF is one of the major health problems worldwide [1,2,3]. In the United States, about 700,000 osteoporotic fractures of the thoracic and lumbar spine (most commonly in the thoracolumbar transition zone or midthoracic region) are reported annually [1]. In addition, one in six elderly patients treated in the emergency department for a condition where a lateral chest X-ray is indicated is reported to have an incidental vertebral fracture seen on X-ray [4]. About 20% of the elderly population is > 70 years of age, and 16% of postmenopausal women will experience OVCFs worldwide [5]. Percutaneous vertebroplasty (PVP) is widely used in patients with OVCFs and accompanying back pain, and percutaneous kyphoplasty (PKP) is a technique based on improved PVP [6, 7]. Bone cement is used in PVP and PKP to treat OVCFs [6, 7].
The use of high-viscosity cement does not completely prevent leakage, and low-viscosity cement is associated with some worries about possible leakage from the vertebra [8]. Previous studies reported that PVP using high-viscosity bone cement in treating OVCFs could significantly reduce the rate of cement leakage and improve operation safety [9,10,11,12]. Nevertheless, in terms of clinical efficacy, the advantages of high-viscosity cement are still controversial [8,9,10,11,12,13,14,15,16,17]. A 2018 meta-analysis (with the literature search up to 2017) showed that although high- and low-viscosity cement had similar clinical outcomes, high-viscosity cement had a lower risk of leakage in the disk space or vein [18]. Since then, new studies and trials have been performed, and including these new studies in a newly updated meta-analysis could provide additional insights into the use of bone cement. A network meta-analysis also supported the lower risk of leakage for high-viscosity cement in vertebral compression fractures [19].
The authors hypothesized that high-viscosity bone cement is superior to low-viscosity bone cement on the clinical outcome and complications in patients with OVCFs who underwent PVP or PKP. Therefore, this meta-analysis aimed to compare high- vs. low-viscosity bone cement on the clinical outcomes [visual analog scale (VAS) and Oswestry Disability Index (ODI)] and complications in patients with OVCFs who underwent PVP or PKP. The results might help determine the optimal approach for such patients.
Materials and methods
Literature search
The present systematic review and meta-analysis was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [20]. The search strategy and the eligibility criteria were designed according to the PICOS principle [21]. PubMed, Embase, and the Cochrane Library were searched for papers published from inception up to February 2021 for potentially eligible studies using the MeSH terms “Osteoporotic Fractures” and “high viscosity cement” as well as relevant key words, followed by screening based on the eligibility criteria. Two investigators performed the literature search and study selection process independently according to a pre-specified protocol. Discrepancies were solved by discussion.
Eligibility criteria
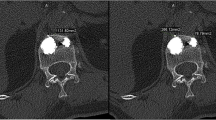
The eligibility criteria were (1) population: patients with OVCF, (2) exposure: treated with PVP/PKP and high-viscosity bone cement, (3) non-exposed control: treated with PVP/PKP and low-viscosity bone cement, (4) outcomes: leakage rate, VAS, and ODI, and (5) full-text published in English. Case reports, reviews, meta-analyses, letters to the editor, and animal studies were excluded. If more than one paper reported the same study population, only the most recent one matching the eligibility criteria was included (Fig. 1).
Data extraction
The study characteristics (authors and year of publication), patient characteristics (disease, sex, age, and follow-up time), treatment parameters (method of intervention and vertebral body position), and outcomes (leakage rate, ODI, and VAS) were extracted independently by two investigators according to a pre-specified protocol. Discrepancies were solved by discussion until a consensus was reached.
Quality of the evidence
The level of evidence of all included articles was assessed independently by two authors according to the Newcastle–Ottawa scale (NOS) for the cohort studies [22] and the Cochrane RoB 2 tool for the randomized controlled trials (RCTs) [23, 24]. Discrepancies in the assessment were resolved through discussion until a consensus was reached.
Data synthesis
For continuous outcomes, the mean values and standard deviations (SD) were used to compute the odds ratios (ORs) and weighted mean differences (WMDs) and their corresponding 95% confidence intervals (CIs) [24, 25]. The data were analyzed according to the exposure of PVP/PKP with high- versus low-viscosity bone cement.
Statistical analysis
All analyses were performed using STATA SE 14.0 (StataCorp, College Station, Texas, USA). Statistical heterogeneity among the studies was calculated using Cochran’s Q-test and the I2 index. An I2 > 50% and Q-test P < 0.10 indicated high heterogeneity, and the random-effects model was used; otherwise, the fixed-effects model was applied. P-values < 0.05 were considered statistically different. The potential publication bias was not assessed using funnel plots and Egger’s test because the number of studies included in each analysis was < 10, in which case the funnel plots and Egger’s test could yield misleading results [24]. Sensitivity analyses were performed by running the meta-analyses and sequentially excluding each study in turn (Table 1).
Results
Study selection
The initial search yielded 181 records. After removing the duplicates, 124 records were screened, and 50 were excluded. Then, 74 full-text articles or abstracts were assessed for eligibility, and 66 were excluded (animal study, n = 1; study aim/design, n = 20; intervention, n = 23; outcome, n = 8; not accessible, n = 4; not in English, n = 10).
Finally, eight papers were included [9,10,11,12, 14,15,16, 26] (Table 2). All studies were from China. There were three RCTs [11, 12, 26] and five cohort studies [9, 10, 14,15,16]. The studies included 558 patients (279 with high-viscosity cement and 279 with low-viscosity cement. All studies investigated PVP, except one retrospective study in which PVP was performed with high-viscosity cement and PKP was performed with low-viscosity cement [15]. According to the RoB 2 tool, one RCT [11] scored 4 points, and two RCTs [17, 26] scored 5 points (Supplementary Table S1). According to the NOS, one study [15] scored 7 points, and four studies [9, 10, 14, 16] scored 8 points (Supplementary Table S2).
Leakage rate
All eight studies [9,10,11,12, 14,15,16, 26] presented the total leakage rate. The meta-analysis showed that the leakage rate was lower with high-viscosity cement than with low-viscosity cement (OR = 0.23, 95%CI 0.14–0.39, P < 0.001; I2 = 43.5%, Pheterogeneity = 0.088) (Fig. 2 and Table 3). Specifically, the leakage rate was lower with high-viscosity cement than with low-viscosity cement in the disk space (OR = 0.30, 95%CI 0.17–0.54, P < 0.001; I2 = 0.0%, Pheterogeneity = 0.723), paravertebral space (OR = 0.40, 95%CI 0.22–0. 73 P = 0.003; I2 = 0.0%, Pheterogeneity = 0.842), and peripheral vein (OR = 0.28, 95%CI 0.14–0.53, P < 0.001; I2 = 0.0%, Pheterogeneity = 0.972), while there were no differences regarding the epidural space (OR = 0.25, 95%CI 0.04–1.60, P = 0.143; I2 = 0.0%, Pheterogeneity = 0.749) and intraspinal space (OR = 0.45, 95%CI 0.14–1.45, P = 0.182; I2 = 0.0%, Pheterogeneity = 0.950) (Fig. 2 and Table 3).
VAS
All eight studies [9,10,11,12, 14,15,16, 26] presented VAS data. The meta-analysis showed that the VAS was decreased more significantly with high-viscosity cement than with low-viscosity cement (WMD = − 0.21, 95%CI − 0.38, − 0.04, P = 0.015; I2 = 0.0%, Pheterogeneity = 0.565) (Fig. 3 and Table 3).
ODI
All eight studies [9,10,11,12, 14,15,16, 26] presented ODI data. The meta-analysis showed no difference between high- and low-viscosity cement (WMD = − 0.88, 95%CI − 3.06, 1.29, P = 0.426; I2 = 78.3%, Pheterogeneity < 0.001) (Fig. 4 and Table 3).
Sensitivity analysis
The sensitivity analyses showed that the meta-analyses for the total leak rate (Fig. S1), VAS (Fig. S2), and ODI (Fig. S3).
Discussion
OVCFs can be treated using PVP or PKP and either low- or high-viscosity cement. Studies suggested different outcomes and safety issues between the two types of cement [8,9,10,11,12,13,14,15,16,17]. This meta-analysis aimed to compare high- vs. low-viscosity bone cement on the clinical outcomes and complications in patients with OVCFs who underwent PVP or PKP. The results suggest lower cement leakage rates in PVP/PKP with high-viscosity bone cement than low-viscosity bone cement. PVP/PKP with high- and low-viscosity cement have similar results in ODI, but the VAS scores favor high-viscosity bone cement (Table 2).
In this meta-analysis, a lower risk of cement leakage, in general, was observed with the high-viscosity bone cement compared with the low-viscosity one. This is supported by previous meta-analyses [18, 19]. More specifically, the risk was lower regarding disk space, paravertebral space, and peripheral, while there were no differences regarding the epidural space and intraspinal space. Chen et al. [19] did not analyze the specific leakage in the vertebral compression fractures, while Zhang et al. [18] observed that high-viscosity cement had a lower risk of leakage in the disk space or vein. A retrospective study also showed that high-viscosity cement was less likely to leak in the vein but without difference for disk space, paravertebral area, or intraspinal space [10]. These results of subgroup analysis are not completely consistent with the present analysis. The anatomical characteristics and the filling volume could influence the areas where thinner cement could be more likely to leak, and discrepancies among studies could be due to the techniques used and the exact types and brands of cement being compared.
Bone- and fracture-related parameters, injection methods, and cement properties are the three most important factors influencing the risk of leakage [27]. Indeed, cortical fractures are the most likely to leak [28]. Disk space leakage is mainly due to endplate fracture [29]. Osteoporotic degeneration of the surrounding bone could also influence the leakage rate since Alhashash et al. [13] showed that patients with a T-score worse than − 1.8 had a higher risk of leakage if a low-viscosity bone cement were used. Although the methods of PVP and PKP are mature, iatrogenic injury to the endplate or the cortical body can lead to cement leakage [18]. In addition, as for any viscous fluid, the cement will spread along the paths offering the least resistance in the vertebral body and fracture [30]. High-viscosity bone cement will spread more uniformly than low-viscosity cement [30, 31], reducing the risk of a leak at one site while the fracture is still not completely filled [18]. Using a gelatin sponge can decrease the risk of vein leakage, but it increases the number of interventions [32].
Regarding the clinical outcomes, the present study showed no difference in the ODI (functional outcome) but a better VAS for pain with the high-viscosity cement. Pain after PVP/PKP can be due to cement leakage, and the present meta-analysis also showed a lower risk of leakage with high-viscosity bone cement. Still, Zhang et al. [18] showed no difference in VAS and ODI between high- or low- viscosity cement. Of course, the studies included in the meta-analyses can influence the results, as well as the evaluation timing of the included studies. Miao et al. [8] also reported no differences in VAS. On the other hand, other studies that did not meet the eligibility criteria of the present meta-analysis nevertheless support a lower VAS with high-viscosity cement [13, 33, 34] and better ODI [13]. Well-designed studies with long-term follow-up are necessary to determine the clinical outcomes between high- and low-viscosity cement in future.
There are three types of osteoporotic compression fractures: wedge, crush (or biconcave), and burst [2]. These fractures have different prognoses [35]. The non-operative management of stable thoracolumbar burst fractures has been advocated for some years [36]. Crush fractures are usually considered complicated, and non-surgical studies often exclude them for the sake of safety and only include, for example, wedge fractures [37]. Furthermore, many studies, such as the ones included in this meta-analysis, do not specify the types of fractures included. Performing a subgroup analysis based on the types of fractures would be of clinical value to determine the efficacy of PVP/PKP in such fractures, but it is impossible for now.
This study has limitations. Most of the included studies were single-center studies, and the bone cement materials they used might be different and have certain heterogeneity. This study direction is relatively new, so the number of reports was small, and there is a lack of high-quality RCT evidence. The included patients have certain heterogeneity, possibly biasing the results. Most studies did not report the exact type of OVCF, preventing a subgroup analysis of cement leakage according to the exact type of fracture. Finally, as for any meta-analysis, the quality of this meta-analysis is limited to the quality of the included studies. Indeed, no cohort study scored higher than 8 points on the NOS, and no RCT scored higher than 5 points on the RoB 2. In addition, one study used high-viscosity cement for PVP and low-viscosity cement for PKP [15], which is bound to bias the results.
In conclusion, compared with low-viscosity bone cement, PVP/PKP using high-viscosity bone cement might improve the VAS with fewer leakage complications. In terms of clinical efficacy, both cement types achieved similar ODI. Future high-quality studies with larger numbers of patients and not limited to single-level OVCFs are encouraged. Long-term follow-up will be necessary to evaluate the safety and efficacy of high-viscosity bone cement.
Data availability
The dataset(s) supporting the conclusions of this article is(are) included within the article (and its additional file(s).
Abbreviations
- OVCFs:
-
Osteoporotic vertebral compression fractures
- PVP:
-
Percutaneous vertebroplasty
- PKF:
-
Percutaneous kyphoplasty
- VAS:
-
Visual analog scale
- ODI:
-
Oswestry disability index
- PKP:
-
Percutaneous kyphoplasty
- NOS:
-
Newcastle–Ottawa scale
- RCTs:
-
Randomized controlled trials
- SD:
-
Standard deviations
- ORs:
-
Odds ratios
- WMDs:
-
Weighted mean differences
- CIs:
-
Confidence intervals
References
Ensrud KE, Schousboe JT (2011) Clinical practice: Vertebral fractures. N Engl J Med 364:1634–1642
Alexandru D, So W (2012) Evaluation and management of vertebral compression fractures. Perm J 16:46–51
McCarthy J, Davis A (2016) Diagnosis and management of vertebral compression fractures. Am Fam Physician 94:44–50
Majumdar SR, Kim N, Colman I, Chahal AM, Raymond G, Jen H et al (2005) Incidental vertebral fractures discovered with chest radiography in the emergency department: prevalence, recognition, and osteoporosis management in a cohort of elderly patients. Arch Intern Med 165:905–909
Karmakar A, Acharya S, Biswas D, Sau A (2017) Evaluation of percutaneous vertebroplasty for management of symptomatic osteoporotic compression fracture. J Clin Diagn Res. https://doi.org/10.7860/JCDR/2017/25886.10461
Long Y, Yi W, Yang D (2020) Advances in vertebral augmentation systems for osteoporotic vertebral compression fractures. Pain Res Manag 2020:3947368
Zhu RS, Kan SL, Ning GZ, Chen LX, Cao ZG, Jiang ZH et al (2019) Which is the best treatment of osteoporotic vertebral compression fractures: balloon kyphoplasty, percutaneous vertebroplasty, or non-surgical treatment? A Bayesian network meta-analysis. Osteoporos Int 30:287–298
Miao F, Zeng X, Wang W, Zhao Z (2020) Percutaneous vertebroplasty with high- versus low-viscosity bone cement for osteoporotic vertebral compression fractures. J Orthop Surg Res 15:302
Tang S, Fu W, Zhang H, Zhang H, Liang B (2019) Efficacy and safety of high-viscosity bone cement vertebroplasty in treatment of osteoporotic vertebral compression fractures with intravertebral cleft. World Neurosurg 132:e739–e745
Zhang ZF, Yang JL, Jiang HC, Lai Z, Wu F, Pan YQ et al (2017) An updated comparison of high- and low-viscosity cement vertebroplasty in the treatment of osteoporotic thoracolumbar vertebral compression fractures: a retrospective cohort study. Int J Surg 43:126–130
Guo Z, Wang W, Gao WS, Gao F, Wang H, Ding WY (2017) Comparison the clinical outcomes and complications of high-viscosity versus low-viscosity in osteoporotic vertebral compression fractures. Medicine 96:e8936
Zhang L, Wang J, Feng X, Tao Y, Yang J, Wang Y et al (2015) A comparison of high viscosity bone cement and low viscosity bone cement vertebroplasty for severe osteoporotic vertebral compression fractures. Clin Neurol Neurosurg 129:10–16
Alhashash M, Shousha M, Barakat AS, Boehm H (2019) Effects of polymethylmethacrylate cement viscosity and bone porosity on cement leakage and new vertebral fractures after percutaneous vertebroplasty: a prospective study. Glob Spine J 9:754–760
Li K, Feng H, Luo D, Zhang W, Yang K, Ji C et al (2020) Efficacy and safety of high-viscosity cement in percutaneous vertebroplasty for treatment of Osteoporotic vertebral compression fractures: a retrospective cohort study. Medicine 99:e20515
Sun K, Liu Y, Peng H, Tan JF, Zhang M, Zheng XN et al (2016) A comparative study of high-viscosity cement percutaneous vertebroplasty vs. low-viscosity cement percutaneous kyphoplasty for treatment of osteoporotic vertebral compression fractures. J Huazhong Univ Sci Technolog Med Sci 36:389–394
Zeng TH, Wang YM, Yang XJ, Xiong JY, Guo DQ (2015) The clinical comparative study on high and low viscosity bone cement application in vertebroplasty. Int J Clin Exp Med 8:18855–18860
Wang CH, Ma JZ, Zhang CC, Nie L (2015) Comparison of high-viscosity cement vertebroplasty and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Pain Physician 18:E187–E194
Zhang ZF, Huang H, Chen S, Liu DH, Feng YH, Xie CL et al (2018) Comparison of high- and low-viscosity cement in the treatment of vertebral compression fractures: a systematic review and meta-analysis. Medicine 97:e0184
Chen WC, Tsai SHL, Goyal A, Tsai-Sheng F, Lin T-Y, Bydon M (2020) Comparison between vertebroplasty with high or low viscosity cement augmentation or kyphoplasty in cement leakage rate for patients with vertebral compression fracture: a systematic review and network meta-analysis. Eur Spine J 30(9):2680–2690. https://doi.org/10.1007/s00586-020-06636-9
Selcuk AA (2019) A guide for systematic reviews: PRISMA. Turk Arch Otorhinolaryngol 57:57–58
Aslam S, Emmanuel P (2010) Formulating a researchable question: a critical step for facilitating good clinical research. Indian J Sex Transm Dis AIDS 31:47–50
Lo CK, Mertz D, Loeb M (2014) Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol 14:45
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:4898
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2019) Cochrane handbook for systematic reviews of interventions. Wiley. https://doi.org/10.1002/9781119536604
da Costa BR, Rutjes AW, Johnston BC, Reichenbach S, Nuesch E, Tonia T et al (2012) Methods to convert continuous outcomes into odds ratios of treatment response and numbers needed to treat: meta-epidemiological study. Int J Epidemiol 41:1445–1459
Gao Y, Huo M, Fan X, Zhou X, Luan J, Dong Z (2020) Effect of PVP with a Mesh-Hold bone-filling mesh bag and different viscosities of bone cement in the treatment of osteoporotic vertebral compression fractures. Int J Clin Exp Med 13:5006–5012
Loeffel M, Ferguson SJ, Nolte LP, Kowal JH (2008) Vertebroplasty: experimental characterization of polymethylmethacrylate bone cement spreading as a function of viscosity, bone porosity, and flow rate. Spine 33:1352–1359
Yeom JS, Kim WJ, Choy WS, Lee CK, Chang BS, Kang JW (2003) Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Joint Surg Br 85:83–89
Tanigawa N, Kariya S, Komemushi A, Tokuda T, Nakatani M, Yagi R et al (2009) Cement leakage in percutaneous vertebroplasty for osteoporotic compression fractures with or without intravertebral clefts. AJR Am J Roentgenol 193:W442–W445
Baroud G, Crookshank M, Bohner M (2006) High-viscosity cement significantly enhances uniformity of cement filling in vertebroplasty: an experimental model and study on cement leakage. Spine 31:2562–2568
Habib M, Serhan H, Marchek C, Baroud G (2010) Cement leakage and filling pattern study of low viscous vertebroplastic versus high viscous confidence cement. SAS J 4:26–33
Bhatia C, Barzilay Y, Krishna M, Friesem T, Pollock R (2006) Cement leakage in percutaneous vertebroplasty: effect of preinjection gelfoam embolization. Spine 31:915–919
Ying L, Chen Z, Yang G (2017) Clinical study of high viscosity bone cement in the treatment of osteoporotic vertebral compression fracture. Biomed Res 28:7837–7840
Yang J, Tang L, Yu J, Chen J, Zhou Q, Kang J (2017) Effect of high viscosity bone cement on treatment of osteoporotic vertebral compression fracture. Biomed Res 28:8954–8957
Donnally IC, DiPompeo CM, Varacallo M (2021) Vertebral Compression Fractures. StatPearls. Treasure Island (FL)
Cantor JB, Lebwohl NH, Garvey T, Eismont FJ (1993) Nonoperative management of stable thoracolumbar burst fractures with early ambulation and bracing. Spine 18:971–976
Qian L, Pan J, Liu ZD, Li LJ, Tan J, Cheng LM et al (2013) The correlation between vertebral wedge-shaped changes in X-ray imaging at supine and standing positions and the efficacy of operative treatment of thoracolumbar spinal fracture in the elderly. Spinal Cord 51:904–908
Funding
The study was supported by Beijing Hospital Clinical Research 121 Project (BJ-2018-203).
Author information
Authors and Affiliations
Contributions
QW analyzed and interpreted the patient data regarding osteoporotic vertebral compression fracture. QW performed the statistical analysis, and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, Q., Sun, C., Zhang, L. et al. High- versus low-viscosity cement vertebroplasty and kyphoplasty for osteoporotic vertebral compression fracture: a meta-analysis. Eur Spine J 31, 1122–1130 (2022). https://doi.org/10.1007/s00586-022-07150-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07150-w