Abstract
Purpose
The purpose of the study is to describe the biomechanical theory explaining junctional breakdowns in thoraco-lumbar fusions, by taking the example of vertebral compression fractures. Also, a new angle, the cervical inclination angle (CIA), describing the relative position of the head at each vertebral level, is presented.
Methods
For the CIA, the data were collected from 137 asymptomatic subjects of a prospective database, containing clinical and radiologic informations. All the 137 subjects have an Oswestry score less than 15% and a pain score less than 2/10 and were part of a previously published study describing the Odontoïd-hip axis angle (ODHA). For each vertebral level from T1 to T12, the CIA as well as the vertical and horizontal distances was measured in reference to the sella turcica (ST), and a vertical line drawn from the ST. Average values and correlation coefficients were calculated.
Results
The CIA is an angle whose average value varies very little between T1 and T5 (74.9°–76.85°), and then increases progressively from T6 to T12. T1–T5 vertebra are always in line within the thoracic spine for each subject and can be considered as a straight T1–T5 segment. In addition, it was found that the vertical inclination of T1–T5 segment is correlated with the C7 slope (R 2 = 0.6383).
Conclusion
The T1–T5 segment inclination is correlated with the C7 slope, and because the latter defines the cervical curve as previously shown, the T1–T5 segment can be considered as the base from which the cervical spine originates. Its role is, thus, similar to the pelvis and its sacral slope, which is the base from which the lumbar spine originates. The CIA along with the ODHA, which describes the adequacy of the global balance in young and elderly asymptomatic populations, are two important parameters that could help us to better understand junctional breakdowns in thoraco-lumbar fusion surgeries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Junctional kyphosis (JK) or failure (JF) can be defined as an abnormal change in the degree of kyphosis, or angulation, than that seen in the early post-operative period, from either failure of the vertebrae, the soft tissues or the bone–implant interface in thoraco-lumbar fusion surgery. The complication can take place at the proximal or distal end of the construct [1]. In most cases, it is the proximal form, which is observed (PJK: proximal junctional kyphosis, or PJF: proximal junctional failure).
PJK is a radiographic finding and is defined as a proximal junctional sagittal Cobb angle (PJA) between upper instrumented vertebra (UIV) and two levels above the UIV, greater than 10° or at least 10° greater than the corresponding preoperative measurement [1,2,3].
PJK or PJF can occur early, during the postoperative period (up to 12 weeks post-op) or more progressively during months or even years [4]. Incidence of PJK/PJF varies widely in the literature with authors reporting rates ranging from 17 to 61%, due to different definitions and study designs [2].
PJF has been defined as a symptomatic form of PJK surgery and with an increased PJA greater than 15°, possibly needing revision [5].
As reported by Hostin et al., fracture is the most common PJF mode (47%), followed by soft-tissue failure (44%), screw pullout and trauma [6]. However, there is evidence that the mode of failure depends on the location of UIV. More fractures are seen in thoracolumbar failures in contrast with upper thoracic failures, which are more frequently seen as soft-tissue failure and compression fractures of various degrees [6].
Clinically, PJF manifests with pain, neurological deficit, gait difficulties, sagittal imbalance and social isolation [7].
In general, PJF requires revision surgery. Treatment depends on the flexibility of the spine. For a flexible and harmonious kyphotic spine, extension of the instrumentation to the next stable level, alone or associated with a Smith Peterson osteotomy (SPO) can be recommended. For a rigid spine containing ankylosing lesions, flat back sequelae, or with localized angular kyphosis, extension of instrumentation may have to be combined with a three-column osteotomy such as Pedicle Subtraction osteotomy (PSO) to correct spinal deformity, pain and neurological deficit [1, 4, 8].
Reports on the prevalence, outcomes, possible risk factors, and prevention of PJK in adult spinal deformity surgery have already been attempted. However, available data remain controversial and pathogenesis of the complication not fully understood [7]. For this reason, it is difficult to anticipate this complication.
From this background analysis, we conclude that current status of the literature reflects the misunderstanding of the exact patho-mechanism of junctional failure.
As mentioned above, junctional kyphosis can present as two major modes [6]: vertebral fractures and soft-tissue failure. When it manifests mainly as soft tissue failure, the etiology is certainly to be found in the deleterious effect of surgical approaches on adjacent levels such as facet joint injury, inter- and supra-spinous ligaments tears, muscle detachment and other anatomical damage [1, 2, 4,5,6,7, 9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27]. This is clearly understandable and supports the fact that extensive surgical approaches should be avoided, although in some cases, there can also be genuine failure through uninjured soft tissue. In some cases, the aging-related muscular degeneration or the neuromuscular dysfunction seen in Parkinson’s disease or camptocormia (bent spine syndrome) can explain the progressive weakening of the posterior tension band, generating overload of the anterior column. In this case, there is a risk of vertebral fracture. When presenting as a fracture, the mechanism of failure is similar to compression fractures. This is further explained here below.
Biomechanics of vertebral compression fractures
Junctional failures are clearly the result of an imbalance between anterior column compression forces and posterior column tension band strength. In other words, there is an excessive bending moment, a mechanism very similar to what is seen in vertebral compression fracture (VCF), a common pathology of the elderly population. VCF can occur after minor trauma or even fortuitously discovered on systematic X-rays. It has been shown that kyphotic patients have higher risk of VCF than the normal population [28].
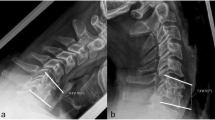
Alf Nachemson and other authors previously reported that a lumbar functional spinal unit (SFU) can support a maximum axial weight of 500 kg, but a bending moment of only 20 Nm in flexion [29, 30]. Consequently, if the lever arm length is increased by only 10 cm, the maximal weight supported by the SFU will be reduced to 20 kg [30]. It is, thus, important to restore the anterior wall height of a fractured vertebra, to prevent the risk of additional adjacent fractures or domino effect (DE) [31] (Fig. 1). Disc height loss due to degeneration at several levels increases thoracic kyphosis and results in a similar biomechanical condition for the upper adjacent vertebra than a VCF.
The biomechanical consequence of an increased thoracic kyphosis is an anterior trunk shift (TS), anteriorly shifting the center of gravity, leading to a domino effect (DE), further increasing the kyphosis [31]. This has been observed in the older study group of asymptomatic patients describing the ODHA angle [32].
The DE and the TS are directly related to the bending moment (BM), which is the product of the weight force (constant) and the arm length (variable) (Fig. 1). The arm length is the horizontal distance between the weight and the gravitational axis, and depends on the degree of kyphosis (greater kyphosis = greater lever arm).
In patients without sagittal imbalance, minor muscular efforts are sufficient to maintain the upright position (head and trunk weigh 35 kg in average, at 1 cm lever arm = 3.5 Nm as shown in example of Fig. 2): the balance is ‘‘ergonomic’’. In case of increased kyphosis (Fig. 2), with a 10-cm lever arm distance increase from the gravity line (GL), the bending moment becomes theoretically high enough to damage the vertebra (35 Nm). VCF can occur in this configuration and with a higher risk if the subject is osteoporotic.
Thoraco-lumbar bending moment increases with aging. With aging, disc degeneration induces loss of lumbar lordosis and increase of thoracic kyphosis, resulting in a forward shift of the center of gravity and a consequent increase of bending moments. Under adequate conditions (loss of muscular function and osteoporosis for example), bending moments can reach critical values and create vertebral fractures
In the static standing position, the weight of the overlying body segment, the compression and shear forces acting on the intervertebral discs are counterbalanced by the abdominal and paravertebral muscle efforts (posterior tension band, Fig. 3).
Paravertebral muscles are more solicited (up to 60%) in an imbalanced spine compared to the ergonomic spinal posture, to counterbalance the increased bending moment (Fig. 4). This muscular effort of counterbalancing induces an increase in compressive and shear forces by 20% on the lumbar discs due to small lever arms. When this becomes permanent, muscle fatigue sets in, leading to a reduction of the muscular compensatory capacity and potential additional degradation of the spinal functional unit.
Muscle work under abnormal balance conditions. Under abnormal conditions like sagittal imbalance due to disc degeneration or iatrogenic flatback, resultant bending moment increases and muscular work also has to increase. In this example, a 1 cm forward displacement of a 400 N weight induces a 60% increase of muscle work
Mechanically, decreasing the excessive thoracic kyphosis is surely a key factor in creating backward bending moments, resulting in reduced local stresses. As an example (Fig. 5), if the trunk is rocked forward, tilting the thoracic spine by 15°, then the bending moment in the T11 vertebra is about 22 Nm, which is excessive and may lead to a fracture. Restoring vertebral height in the case of a VCF cannot alone eliminate the risk of DE. However, an angular re-balancing of 1° creates a biomechanically more favorable bending moment by about 1.5 Nm.
Effect of angular correction on bending moments. In this example, a 15° post-traumatic kyphotic deformity is simulated at T11. The bending moment is about 22 Nm. Restoration of height only, does not change the bending moment, where as correcting the kyphotic deformity by 9.5° results in a 14Nm bending moment decrease (1.5 Nm per degree of correction)
Thus, compared with the mean critical fracture threshold (20 Nm), 1 mm anterior height correction reduces by 13% the risk of subsequent vertebral compression fracture; 2 mm by 25%, etc. This biomechanical reasoning provides much information to understand the mechanisms of PJK/PJF above a fusion. The segment of the spine and body located on top of the UIV has a mass and a center of gravity that can be determined with a barycentremeter as described by Duval-Beaupere et al. [33]. Therefore, it is possible to evaluate the moment of forces applied on the first vertebra above the UIV knowing its distance from the center of gravity of the body part above it (Fig. 6).
Cervical inclination angle (CIA): a new sagittal parameter of economical balance assessment in the asymptomatic population
In static position, there is a balance between the weight of the overlying body segment, the compression and shear loads on the intervertebral discs, and the muscle counterbalancing efforts (tension of the spinal muscles and posterior ligaments). We analyzed the full spine EOS X-rays of an asymptomatic population in the upright standardized posture to find an anatomical parameter that could help to predict overstress at each segment of the thoraco-lumbar area.
The position of the center of gravity of the head was studied in several papers and has been located just behind the sella turcica, close to Center of the Acoustic Meati (CAM) and on top of the dens of C2 [34]. The sella turcica is a very easily identifiable anatomical landmark on lateral full spine standing X-rays and located on the midline in the coronal view. Knowing that the odontoid-hip axis angle (ODHA) reliably reflects a globally balanced spine [32, 35], we decided to measure an anatomical angle at each level of the thoracic spine vertebra from T1 to T12, using a 3D reconstruction of the spine with EOS technology. This angle is the cervical inclination angle or CIA, and is described below.
Materials and methods
The EOS data of 137 asymptomatic voluntary subjects were extracted from a prospective database, after ethics committee approval (ID-RCB 2010-A01248-31). All X-rays were obtained in the standardized standing position as defined by Faro [36, 37]. The usual sagittal parameters such as pelvic parameters, lumbar lordosis, thoracic kyphosis, and cervical angles were measured. Those results have already been reported in a previous article [38].
The CIA was measured and is described as follows: for each thoracic vertebra from T1 to T12, we measured the angle between the mid-point of the sella turcica (ST), the mid-point of the thoracic vertebra and the horizontal line to each thoracic vertebral endplate mid-point (Fig. 7). The distance between the vertical line from the ST and the center of the endplate of each thoracic vertebra was also measured, as well as the vertical distance. The vertical and horizontal distances allowed us to spatially localize each vertebra. Two orthopaedic fellows did all the measurements twice independently. We also used values of the C7 slope, previously described, to calculate correlations [39].
Study measurements. CIA: angle between a line joining the center of ST to the center of the superior endplate of each thoracic vertebra, and a line drawn horizontally from the endplate center. For each level, the vertical distance was measured between the center of ST and the crossing point with the horizontal line drawn from the center of the superior endplate. Similarly, the horizontal distance was measured from the endplate center to the crossing point with the vertical ST line
Statistical analysis
Average values and standard deviations of CIA were calculated for each vertebral level from T1 to T12.
Correlations were calculated for T1–T5 alignment and T1–T5 segment inclination versus C7 slope, using linear regression and Pearson coefficient.
Results
The CIA average values for each thoracic vertebra of the 137 study subjects are reported in Table 1. The CIA average value progressively increases from T1 to T12, ranging from 74.83° for the lowest value to 83.82° for the highest. However, it appeared that the average values of the T1–T5 segment varied very little, between 74.9° and 76.85°, compared to the rest of the thoracic spine where there was a constant increase (Table 1 and Fig. 8).
CIA average value versus vertebral level (T1–T12). This graph shows the values for each of the 137 subjects. The line in red represents the average values calculated from the 137 subjects. It clearly stands out that the T1–T5 segment has an average CIA value that varies very little, as shown also in Table 1. It was thus hypothesized that T1–T5 vertebrae follow a straight line in all the subjects (see Fig. 9)
Further analysis of the vertical and horizontal distances of each thoracic vertebra in reference to the ST vertical line showed that the vertebrae from T1 to T5 were in a straight line within the thoracic spine, as shown in Fig. 9.
T1–T5 alignment in a sample of study subjects. Using the vertical and horizontal distance measurements for each vertebra from T1 to T5, it was possible to localize them in reference to the ST vertical line. This graph clearly shows that T1–T5 vertebrae follow a straight line, with an average correlation coefficient, above 0.8 in the worst case (Pearson R 2 > 0.8)
Figure 10 describes the correlation between the C7 slope and the vertical inclination of the T1–T5 segment (R 2 = 0.6383).
Correlation of T1–T5 segment inclination versus C7 slope. The vertical inclination of the T1–T5 segment appeared to be correlated with the C7 slope for all the 137 subjects (Pearson R 2 = 0.6383). This means that any change in the vertical inclination of the T1–T5 segment will likely result in a modification of the C7 slope, which in turn will modify the cervical curve
Discussion
Sagittal vertical axis (SVA) is commonly used and considered as an important predictive factor for junctional construct failure [20, 21]. However, it does not take into consideration capital parameters, which are the head and neck and their weight. SVA is an adequate parameter to compare a patient balance over time but is not adequate to analyze the balance between patients. In some circumstances, the shoulders and upper limbs might also play a role. The CIA reflects the necessary harmony of the spinal curves and its importance for a balanced upright posture, as already supported by the concept of the conus of economy of Jean Dubousset [40].
The terms PJK (less deformity, non or less symptomatic) and PJF (more deformity, more symptomatic) do not reflect the biomechanical understanding we expose above. The main mechanism in both conditions is an excessive biomechanical stress as exposed at the beginning of this article (bending moment). However, the magnitude of the stress can be more or less important, which explains why some patients develop acute forms of junctional breakdowns (JBD) like fractures (thus a PJF) or a more progressive disease like adjacent segment degeneration (thus a PJK). This theory is further developed in part II of this article.
The analysis of the CIA shows that the T1–T5 segment is particular in the thoracic spine. The average value varies very little, between 74.9° and 76.85°, depending on the vertebral level (Table 1 and Fig. 8). In addition, Figs. 9 and 10 show us that T1–T5 vertebrae are very well aligned, and that there is a correlation between the T1–T5 segment inclination and the C7 slope (R 2 = 0.6383): if C7 slope increases, the T1–T5 segment is more horizontal and vice versa. This means that the T1–T5 segment can be considered as the base on which the cervical spine lies, just like the pelvis is the base of the lumbar spine. The T1–T5 segment defines the C7 slope, which in turn defines the cervical curve as shown in a previous publication [39]. This information is of paramount importance for the comprehension of junctional failures in the proximal and mid-thoracic spine.
Conclusion
This study shows that the T1–T5 segment can be considered as the base of the cervical spine. Its inclination defines the C7 slope and thus the type of cervical spine curve. The adequacy of the global balance in young and elderly asymptomatic populations can be determined with the ODHA [32]. Combining those two angles could allow us predict the risk of JBD in a population of patients with long lumbo-sacral fusions. A detailed analysis of 12 patients with thoraco-lumbar JBD is presented in part II of this article.
References
Cho SK, Shin JI, Kim YJ (2014) Proximal junctional kyphosis following adult spinal deformity surgery. Eur Spine J 23:2726–2736. https://doi.org/10.1007/s00586-014-3531-4
Hyun SJ, Kim YJ, Rhim SC (2016) Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J 16:1095–1101. https://doi.org/10.1016/j.spinee.2016.05.008
Mummaneni PV, Park P, Fu KM, Wang MY, Nguyen S, Lafage V, Uribe JS, Ziewacz J, Terran J, Okonkwo DO, Anand N, Fessler R, Kanter AS, LaMarca F, Deviren V, Bess RS, Schwab FJ, Smith JS, Akbarnia BA, Mundisjr GM, Shaffrey CI (2016) Does minimally invasive percutaneous posterior instrumentation reduce risk of proximal junctional kyphosis in adult spinal deformity surgery? A propensity-matched cohort analysis. Neurosurgery 78:101–108. https://doi.org/10.1227/neu.0000000000001002
Nguyen NL, Kong CY, Hart RA (2016) Proximal junctional kyphosis and failure-diagnosis, prevention, and treatment. Curr Rev Musculoskelet Med 9:299–308. https://doi.org/10.1007/s12178-016-9353-8
Yagi M, Rahm M, Gaines R, Maziad A, Ross T, Kim HJ, Kebaish K, Boachie-Adjei O, Complex Spine Study G (2014) Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine (Phila Pa 1976) 39:E607–E614. https://doi.org/10.1097/brs.0000000000000266
Hostin R, McCarthy I, O’Brien M, Bess S, Line B, Boachie-Adjei O, Burton D, Gupta M, Ames C, Deviren V, Kebaish K, Shaffrey C, Wood K, Hart R, International Spine Study G (2013) Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine 38:1008–1015. https://doi.org/10.1097/brs.0b013e318271319c
Ha Y, Maruo K, Racine L, Schairer WW, Hu SS, Deviren V, Burch S, Tay B, Chou D, Mummaneni PV, Ames CP, Berven SH (2013) Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine 19:360–369. https://doi.org/10.3171/2013.5.spine12737
Le Huec JC, Leijssen P, Duarte M, Aunoble S (2011) Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J 20(Suppl 5):669–680. https://doi.org/10.1007/s00586-011-1935-y
Bridwell KH, Lenke LG, Cho SK, Pahys JM, Zebala LP, Dorward IG, Cho W, Baldus C, Hill BW, Kang MM (2013) Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery 72:899–906. https://doi.org/10.1227/NEU.0b013e31828bacd8
Cammarata M, Aubin CE, Wang X, Mac-Thiong JM (2014) Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine (Phila Pa 1976) 39:E500–E507. https://doi.org/10.1097/brs.0000000000000222
Denis F, Sun EC, Winter RB (2009) Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine (Phila Pa 1976) 34:E729–E734. https://doi.org/10.1097/brs.0b013e3181ae2ab2
Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C 2nd (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 30:1643–1649
Yanik HS, Ketenci IE, Polat A, Ulusoy A, Deniz G, Kose O, Erdem S (2015) Prevention of proximal junctional kyphosis after posterior surgery of Scheuermann kyphosis: an operative technique. J Spinal Disord Tech 28:E101–105. https://doi.org/10.1097/BSD.0000000000000157
Kim HJ, Bridwell KH, Lenke LG, Park MS, Song KS, Piyaskulkaew C, Chuntarapas T (2014) Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976) 39:E576–E580. https://doi.org/10.1097/brs.0000000000000246
Kim HJ, Yagi M, Nyugen J, Cunningham ME, Boachie-Adjei O (2012) Combined anterior–posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res 470:1633–1639. https://doi.org/10.1007/s11999-011-2179-1
Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G (2008) Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 33:2179–2184. https://doi.org/10.1097/brs.0b013e31817c0428
Kim YJ, Bridwell KH, Lenke LG, Kim J, Cho SK (2005) Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine (Phila Pa 1976) 30:2045–2050
Kim YJ, Lenke LG, Bridwell KH, Kim J, Cho SK, Cheh G, Yoon J (2007) Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976) 32:2731–2738. https://doi.org/10.1097/brs.0b013e31815a7ead
Lau D, Clark AJ, Scheer JK, Daubs MD, Coe JD, Paonessa KJ, LaGrone MO, Kasten MD, Amaral RA, Trobisch PD, Lee JH, Fabris-Monterumici D, Anand N, Cree AK, Hart RA, Hey LA, Ames CP, Committee SRSASD (2014) Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976) 39:2093–2102. https://doi.org/10.1097/brs.0000000000000627
Liu FY, Wang T, Yang SD, Wang H, Yang DL, Ding WY (2016) Incidence and risk factors for proximal junctional kyphosis: a meta-analysis. Eur Spine J 25:2376–2383. https://doi.org/10.1007/s00586-016-4534-0
Maruo K, Ha Y, Inoue S, Samuel S, Okada E, Hu SS, Deviren V, Burch S, William S, Ames CP, Mummaneni PV, Chou D, Berven SH (2013) Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 38:E1469–E1476. https://doi.org/10.1097/brs.0b013e3182a51d43
Mendoza-Lattes S, Ries Z, Gao Y, Weinstein SL (2011) Proximal junctional kyphosis in adult reconstructive spine surgery results from incomplete restoration of the lumbar lordosis relative to the magnitude of the thoracic kyphosis. Iowa Orthop J 31:199–206
O’Leary PT, Bridwell KH, Lenke LG, Good CR, Pichelmann MA, Buchowski JM, Kim YJ, Flynn J (2009) Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs: a matched cohort analysis performed at a single center. Spine (Phila Pa 1976) 34:2134–2139. https://doi.org/10.1097/brs.0b013e3181b2e17e
Park SJ, Lee CS, Chung SS, Lee JY, Kang SS, Park SH (2016) Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery. https://doi.org/10.1227/NEU.0000000000001240
Wang J, Zhao Y, Shen B, Wang C, Li M (2010) Risk factor analysis of proximal junctional kyphosis after posterior fusion in patients with idiopathic scoliosis. Injury 41:415–420. https://doi.org/10.1016/j.injury.2010.01.001
Yagi M, Akilah KB, Boachie-Adjei O (2011) Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976) 36:E60–E68. https://doi.org/10.1097/brs.0b013e3181eeaee2
Yagi M, King AB, Boachie-Adjei O (2012) Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976) 37:1479–1489. https://doi.org/10.1097/brs.0b013e31824e4888
Fechtenbaum J, Etcheto A, Kolta S, Feydy A, Roux C, Briot K (2016) Sagittal balance of the spine in patients with osteoporotic vertebral fractures. Osteoporos Int 27:559–567. https://doi.org/10.1007/s00198-015-3283-y
Nachemson A (1965) The effect of forward leaning on lumbar intradiscal pressure. Acta Orthop Scand 35:314–328
Skalli W, Champain S, Mosnier T (2007) Biomécanique du Rachis. In: Elsevier (ed) Cahiers d’enseignement de la SOFCOT, pp 8–17
Nardi A, Tarantino U, Ventura L, Armotti P, Resmini G, Cozzi L, Tonini G, Ramazzina E, Rossini M (2011) Domino effect: mechanic factors role. Clin Cases Miner Bone Metab 8:38–42
Amabile C, Le Huec JC, Skalli W (2016) Invariance of head–pelvis alignment and compensatory mechanisms for asymptomatic adults older than 49 years. Eur Spine J. https://doi.org/10.1007/s00586-016-4830-8
Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20:451–462
Vital JM, Senegas J (1986) Anatomical bases of the study of the constraints to which the cervical spine is subject in the sagittal plane. A study of the center of gravity of the head. Surg Radiol Anat 8:169–173
Amabile C, Pillet H, Lafage V, Barrey C, Vital JM, Skalli W (2016) A new quasi-invariant parameter characterizing the postural alignment of young asymptomatic adults. Eur Spine J 25:3666–3674. https://doi.org/10.1007/s00586-016-4552-y
Morvan G, Mathieu P, Vuillemin V, Guerini H, Bossard P, Zeitoun F, Wybier M (2011) Standardized way for imaging of the sagittal spinal balance. Eur Spine J 20(Suppl 5):602–608. https://doi.org/10.1007/s00586-011-1927-y
Faro FD, Marks MC, Pawelek J, Newton PO (2004) Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 29:2284–2289
Le Huec JC, Hasegawa K (2016) Normative values for the spine shape parameters using 3D standing analysis from a database of 268 asymptomatic Caucasian and Japanese subjects. Eur Spine J. https://doi.org/10.1007/s00586-016-4485-5
Le Huec JC, Demezon H, Aunoble S (2015) Sagittal parameters of global cervical balance using EOS imaging: normative values from a prospective cohort of asymptomatic volunteers. Eur Spine J 24:63–71. https://doi.org/10.1007/s00586-014-3632-0
Dubousset J (1994) Three-dimensional analysis of the scoliotic deformity. In: Weinstein SL (ed) Pediatric spine: principles and practice. Raven Press, New York, pp 480–481
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Le Huec, JC., Richards, J., Tsoupras, A. et al. The mechanism in junctional failure of thoraco-lumbar fusions. Part I: Biomechanical analysis of mechanisms responsible of vertebral overstress and description of the cervical inclination angle (CIA). Eur Spine J 27 (Suppl 1), 129–138 (2018). https://doi.org/10.1007/s00586-017-5425-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5425-8