Abstract
Background
Some recent studies indicate correlations between cervical alignment and clinical outcome after anterior cervical discectomy and fusion (ACDF) surgery. However, there still are no established criteria for the interpretation of alignment, fusion and subsidence in relation to clinical outcome.
Methods
A retrospective analysis of 208 radiographs of patients following ACDF with stand-alone PEEK cage implantation was performed. The measurements were obtained on plain radiographs in lateral and anteroposterior projections as well as flexion/extension radiographs. Cervical alignment was measured using the Gore, Laing and Cobb methods; fusion was evaluated by an assortment of radiographic hallmarks: the presence of bridging bone, the Cobb angle and the distances between the tips and bases of the spinous processes of the operated segments, respectively. For assessment of subsidence, we used the Mochida method in addition to ventral and dorsal segmental height reduction. Correlation analysis between the different radiological characteristics and clinical outcome at a minimum follow-up of 12 months was conducted.
Results
Two hundred and eight patients were evaluated for alignment, fusion and subsidence. Cervical alignment using the Gore and Cobb methods correlated among each other, but failed to exhibit significant correlation with clinical outcome. Interpretation of fusion rates varied greatly (43.9 to 89.4%) depending on the criteria used. Pearson coefficients between radiographic presence of pseudarthrosis and the measurements of the spinous process distances (0.595; p < 0.001), the Cobb angles (0.187; p = 0.007) and the presence of bridging bone (0.224; p < 0.001) each exhibited statistical significance. None of the methods employed significantly correlated with clinical outcome. Regarding subsidence, we found rates of 62%, 48% and 27% using the Mochida, ventral and dorsal segmental height reduction assessment methods, respectively. Pearson correlations between pairs of Mochida/ventral (r = 0.39; p = 0.66) and Mochida/dorsal (r = 0.007; p = 0.921) height reduction assessment methods were weak and no significant correlation between subsidence rates and clinical outcome was shown.
Conclusion
All measured parameters varied depending in the measurement method used. This was most pronounced for fusion. There was a moderate positive correlation between neck pain and subsidence as measured by the Mochida method.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cervical discectomy and interbody fusion (ACDF) remains the gold standard for treatment for degenerative spine conditions in western countries. Aside from decompression of the spinal cord and nerve roots, the aim of surgery is to achieve fusion of index segments and correction of sagittal cervical alignment. The assessments of fusion and alignment, however, are not standardized among professionals and there is a variety of measurement methods to evaluate these aspects of radiographic outcome [1, 23]. In general, plain radiographs in anterior-posterior as well as lateral projections with additional dynamic imaging are utilized for most measurement methods. Subsidence, fusion, angle of fused segments, global cervical lordosis and adjacent disc mid-height are the most commonly reported variables in studies concerning radiographic outcome following ACDF among others.
Aim of this study was to compare various proposed measurement methods for fusion, alignment and subsidence and correlate these with clinical outcome.
Material and methods
Patient population and procedure
We retrospectively analyzed a consecutive cohort of patients who underwent one- or two-level ACDF for degenerative cervical spine disease between 2007 and 2013. The patient cohort was selected to include those with predominant neck pain attributable to osteochondrotic degeneration of the intervertebral discs, facet joint degeneration and degeneration of the osteoligamentous apparatus, or a combination of these. Patients undergoing ACDF for clear radiculopathy without neck pain or long-standing neck pain exceeding a duration of 12 months were not included in the analysis.
Evidence of tumor, trauma and infection and patients with previous surgery on the cervical spine were not eligible. For the ACDF, surgical approach and preparation were done in the standard fashion as has been extensively described in the literature [7, 30, 39]. After discectomy, we implanted a PEEK cage (NUBIC® Cage, Signus Medizintechnik GmbH, Alzenau, Germany) packed with demineralized bone matrix in 124 patients (59.6%) and a stand-alone cage in 84 patients (40.4%; Table 1).
We have already published our results focusing on clinical outcome following ACDF with empty PEEK cages in comparison with PEEK cages filled with demineralized bone matrix [36, 37].
In all patients, visual analogue scale (VAS) scores for neck pain were polled prior to surgery and on final follow-up.
Radiographic outcome
Regional sagittal alignment
Patients received a plain radiograph imaging on the first postoperative day and on final follow-up with additional flexion and extension radiographs. Sagittal alignment measurements were assessed by three techniques. First, we calculated Cobb’s angle between the endplates of C2 and C7, as depicted in Fig. 1 [8, 12, 35].
Secondly, we used the Gore method, also called Jackson physiological stress line method (JPSLM), which aligns tangents to the posterior walls of C2 and C7 each for their respective intersecting angle (Fig. 2) [1, 19, 22, 25, 34].
The Laing method provides simple assessment of alignment of the cervical spine by connecting a line in parallel to the posterior walls of C2 and C7 (Fig. 3) [28]. Kyphotic and straight alignments of the cervical spine were interpreted as unfavorable outcome. We subtracted the angle of the final follow-up compared with the first postoperative radiographs to distinguish two groups. The group with a “negative” alignment (designated by a minus sign) was allotted to the “deterioration” group. Patients that gained in lordosis or did not experience change in alignment were allotted to the “stable” group.
Fusion
To determine the fusion rate and identify pseudarthrosis after ACDF, we used the three most commonly reported measurements obtained from flexion-extension radiographs (Table 2): the amount of angular motion in the fused segment derived from the difference of local Cobb angles (Fig. 1) and the distance between the tips of the spinous processes as well as the distance between their bases in the operated segment(s). A difference less than 2 mm between these distances in flexion and extension radiographs indicates radiographic fusion (Fig. 4). The presence of bridging bone was detected in lateral radiographs, also indicating bony fusion (Fig. 5) [38].
The difference of distances between the spinous processes on dynamic radiographs was indicative of segmental fusion when it amounted to less than 2 mm, as recommended by the joint guidelines committee of the AANS/CNS [5, 23]. For the Cobb measurements, several studies define a rather strict cut-off with angles less than 2° advocating fusion and thus radiographic success, whereas others accept a threshold of 4° [9, 21, 23, 42]. We assessed both definitions independently for correlation with clinical outcome.
Subsidence
Ventral and dorsal segmental height reduction was measured and compared between first postoperative imaging and final follow-up imaging; height reduction of more than 3 mm ventrally or dorsally was interpreted as subsidence [15, 27]. In addition, the Mochida method was used with two different thresholds of height loss of 10 and 20%, respectively (Fig. 6) [27, 31].
For the aforementioned Mochida method, the ratio between the vertebral body height and the adjacent disc height is calculated through the following sequence upon studying the plain radiograph: First, diagonals between the corners of two neighbouring vertebral bodies are constructed. A straight line through the hereby produced intersections allows for measurement of vertebral and disc heights. A quota of vertebral body height divided by disc height can now be used for comparison on follow-up (Fig. 6).
Statistical analysis
Statistics were calculated with IBM SPSS Statistics version 23. Values of α below 0.05 were indicative of a statistically significant difference between mean values with a 95% confidence interval.
Results
Study population
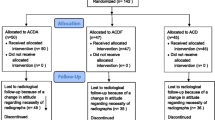
Of 218 patients included initially, 10 patients were excluded post hoc because of incomplete postoperative imaging. All other patients had received pre- and postoperative radiographs in anterior-posterior and lateral projections.
A hundred and one women (48.6%) and 107 men (51.4%) were operated on. Of these, a single segment procedure was done in 123 (59.1%) and two segments in 85 (40.9%). The median follow-up was 30 months (range 11–61; Table 1). Data on VAS scores preoperatively and on the final follow-up was complete in 176 cases (84.6%). The preoperative mean value for neck pain was 6.45 (± 2.87). On final follow-up, the mean VAS score amounted to 2.30 (± 2.57), improving by a mean 4.15 across the entire cohort.
Sagittal alignment
Assessments of the Gore and Cobb angles were possible in all but one patient (0.5%) where effacement of C7 margins due to overlying soft tissue precluded radiographic evaluation. The absolute difference between measurements by Gore and Cobb amounted to 1.03° on the first postoperative day and 0.72° on final follow-up. The Pearson coefficient showed statistically significant and strong correlation between the Gore and Cobb measurements on the first postoperative day (r = 0.856, p < 0.001) as well as on last follow-up (r = 0.828, p < 0.001).
In Table 3, information about sagittal alignment of the cervical spine on final follow-up is summarized. In general, measurements of alignment corresponded well between Gore and Cobb methods, but deviated for the Laing method.
To determine the correlation between clinical outcome and radiographic alignment on follow-up, we used linear regression with neck pain as a dependent variable (Table 4). None of the measurements showed significant correlation of neck pain with alignment as judged by the Gore and Cobb angles. Distortion of sagittal alignment was seen equally in both groups of improved and deteriorated neck pain (Table 5). For the Laing method, we found significant inverse correlation between postoperative changes of alignment and neck pain (chi-square; p = 0.049). Patients who developed radiographic deterioration of alignment postoperatively improved on the VAS more frequently than patients with stable or improved cervical alignment.
Fusion
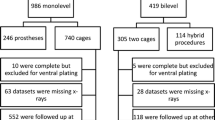
Two hundred and two cases were evaluated for fusion; in the remaining six cases, suboptimal quality of dynamic imaging rendered any measurements inconclusive.
The Cobb angles as well as distances between the tips and bases of the spinous processes of the fused segments were distributed normally according to Shapiro-Wilk testing (W = 0.797 p = 0.000; W = 0.796, p < 0.001; W = 0.698, p < 0.000).
The highest fusion rate of 85.6% was obtained by evaluation of bridging bone in lateral plain radiographs (Fig. 7). Only a third of patients had bony fusion with present bridging bone in addition to a Cobb angle of 2° or less. Evaluating fusion by measurement of interspinous distance close to the vertebral body yielded higher fusion rates than at the tips of the interspinous processes (Fig. 7).
Linear regression was employed to evaluate correlation between the method of fusion assessment and its predictive value regarding intensity of neck pain. Patients that were assigned to the fused group by definition of a Cobb angle of 4° or less showed a significant positive correlation (r = 0.04) with clinical improvement, defined as an increase of one or more points on the VAS (p = 0.035; Tables 6 and 7).
None of the other measurements showed any significant correlation between neck pain and fusion rates. The proportion of patients who experienced clinical satisfaction after surgery was 80%, irrespective of fusion rate as evaluated by any of the three methods (Table 7).
Subsidence
Subsidence was evaluated in 201 cases. Its occurrence rate varied between 8 and 51% depending on the applied method (Table 8).
In cases of subsidence, loss of height in the dorsal part of the vertebra amounted to less than in the ventral part, resulting in bias towards a higher subsidence rate for the ventral method. The Mochida method had the lowest subsidence rate when a cut-off of more than 20% height loss was predefined (Table 8). Patients with subsidence in the follow-up did not report higher scores on the VAS for neck pain and no significant correlation was found (Tables 9 and 10).
For the correlation between method of assessment and clinical outcome, no statistically significant relations for either ventral (p = 0.788) or dorsal (p = 0.445) measurements were found. Chi-square testing revealed no significant differences when employing the Mochida method (10%: p = 0.294; 20%: p = 0.270).
Discussion
Regional sagittal alignment
For comparison of postoperative regional sagittal alignment to preoperative imaging, one may find several different methods described in the literature, although there exists no “gold standard” for alignment measurement. It remains unclear whether different techniques produce corresponding and valid values or a meaningful impact on clinical outcome. Therefore, we investigated the most commonly used measurements for radiographic interpretation of sagittal alignment and fusion as well as the comparability of the results.
In general, the Cobb angle method is widely used in published works due to its simple application and high interrater reliability. Alternatively, the Gore method is an often reported measurement with comparable characteristics [1, 25, 34]. Laing et al. implemented a less popular but considerably more straightforward technique for the evaluation of alignment, prompting us to include it in this study [28]. Several other techniques, such as the Harrison method, have been described, but these seem to be rarely applied for their more intricate nature [1, 34].
Our own mean measurements of sagittal alignment as per Cobb and Gore methods were well within the range of pertinent published works [1, 34]. Both methods produced similar results, whereas our rates of kyphotic and straight malalignments were fairly high with the Laing method. This is concordant with other studies with a similar modus operandi [28, 44].
Paradoxically, patients who improved on the VAS scale had a higher proportion of deterioration of sagittal alignment according to the Laing method. Surely, this represents an unprecedented novelty and leaves us in doubt about that correlation, particularly when considering the weak correlation coefficients. In none of the patients with improved or deteriorated alignment according to Cobb angle or Gore, there was any correlation with change in VAS score.
The majority of comparable studies reported similar results, with weak correlation of sagittal alignment in imaging and development of postoperative VAS [10, 24, 32, 43]. In a group of 57 patients, Wu et al. described a moderate correlation between Japanese Orthopaedic Association score for cervical myelopathy and Cobb angle after 5 years of follow-up [44]. None of the three methods revealed any advantages and benefit in regard to interpretation of alignment and its relation to the clinical outcome. The Gore and Cobb angle methods are comparable tools with congruent results, whereas the Laing method differed. Thus, premature comparison of studies utilizing these measurements is not recommended, as it has to be questioned whether cervical alignment on its own may serve as a reliable indicator for clinical success after ACDF surgery. The evaluation of clinical and radiographic findings is more so challenged by the notion that a large proportion of asymptomatic patients develop physiological alterations of their sagittal profile during their lifetime, with pathomorphogenic changes commonly affecting several of the weight-bearing structures without consequences for the patients [16, 17]. Vice versa, radiographic phenomena may not always be pertinent to the patient’s neck pain, putting into question as to how clinical improvement in such a patient cohort best be gauged. By contrast, a clinically manifest radiculopathy regularly originates from some form of pathomorphogenic degeneration that exerts a clear neural compression, allowing for clearer clinical reasoning [18].
The majority of published literature failed to demonstrate any significant correlation between neck pain and deteriorating alignment, which may however be owed to the heterogeneity of employed methods of measurement and general scarcity of studies [11, 14, 18, 26].
Fusion
It is common practice to evaluate for radiographic fusion after ACDF surgery. Several techniques for fusion assessment have been devised, but are not employed uniformly in available literature [23]. We therefore focused our efforts on the validity of the different fusion assessment methods and their respective relation to the clinical outcome.
The first method of measuring distances between the spinous processes of the operated segment represents an often reported instrument though without clear definition as to the exact reference point [31]. By choice, we hence applied measurements at two different and extreme reference points and found that with increasing distance between these reference points and the vertebral body, values of measurements will increase correspondingly. As such, we had to consider the necessity of defining a single reference point for the spinous processes. Aside from this, the Cobb angle and presence of bridging bone were used as fusion criteria.
The applicability of the Cobb angle was limited by poor quality in the presence of extensive degenerative changes. Whilst all cases could be assessed with both other methods, assessment of the Cobb angle was not clearly evaluable in 6 cases out of 208. Sudhakar et al. reported similar problems in their analysis and discuss this as a possible factor for inferior interrater comparability [5, 40].
As expected, there was high correlation of interspinous distances in contrast to the Cobb angle method evaluated by absolute measurements which were not provided by the method of bridging bone. The estimated fusion rates varied to a considerable extent between the three measurements. A Cobb angle of less than 2° showed the lowest, whereas screening for bridging bone showed the highest fusion rates. Unsurprisingly, we acquired more fused cases with measurement of the distance between the bases of the spinous processes than with the distance that was measured further away from the vertebral body.
Even when considering our divergent definition of Cobb angle reference values, our results were comparable with other studies to a certain degree. Hipp et al. reported a rise in-fusion rates when admitting a cut-off for the Cobb angle of 1° rather than 4° [20]. Beyond that, comparability with other studies is always confounded by discrete variations of surgical techniques, types of implants and timing of follow-up of which each may produce a considerable impact on fusion rates [6, 9, 38, 40]. Our analysis of comparability showed no significant case-related correlation between the three described measurements. Regarding the measurement of Cobb’s angle, the defined cut-off value is the most crucial determinant for evaluation in addition to a clearly defined point on the spinous processes for the assessment of their distances.
Several authors sought to evaluate the reliability of different measurements for the assessment of fusion rates. Cannada et al. investigated 27 cases which were considered fused cases when bridging bone was present [5]. Nevertheless, there was no evidence for superiority of this method, which was repeated by Tuli et al. [41]
Depending on the used implants and imaging quality, the comparability and feasibility of evaluating plain radiographs for bone bridges may be impaired [23, 40].
On follow-up, we found no significant correlation between VAS scores and presence of fusion for any of the three methods, which leads us to the assumption that there is no impact of bony fusion on clinical outcome. There is no agreement in the literature resolving this supposed contradiction. Cauthen et al. report a significantly higher rate of 80% satisfaction for patients with radiographic fusion, in contrast to 68% that report clinical improvement without fusion [6]. Conversely, the studies of Moon et al. as well as Löfgren et al. found no correlation between fusion rates and clinical outcome when defining fusion in cases of an interspinous distance of less than 2 mm or using the Cobb angle and bridging bone criteria [30, 32]. Our results merely demonstrate a significant but weak correlation between a Cobb angle of 4° or less with our definition of clinical improvement, which is further undermined by the questionable relevance of a 1-point increase on the VAS for the individual.
In essence, we concur with the recommendation of the CNS/AANS joint section guidelines that dynamic radiographs be considered for evaluation of fusion [23]. Absence of motion may be indicative of fusion despite clear absence of bridging bone, necessitating computed tomography (CT) scanning for confirmation of fusion. In light of this, Buchowski et al. and Feng et al. independently employed CT scanning in their postoperative follow-up, although again no positive correlation between clinical and radiographic outcome was found [3, 13].
Subsidence
Conventional criteria for evaluating subsidence after ACDF procedure are still lacking. One of the most often reported methods is the determination of ventral and dorsal segmental height reduction.
The Mochida method, initially devised for assessment of subsidence on magnetic resonance imaging (MRI), provides a reproducible, yet more complicated alternative to the other methods [31]. According to our results, there was a strong correlation between ventral and dorsal height reduction. Expectedly, the Mochida measurement did not correlate with the other two methods. The rate of subsidence within the group of ventral height reduction was almost twice as high as in the group of dorsal height reduction, although intra-individual correlation was only moderate. Statistical analysis could not show any significant correlation of subsidence and VAS scores. This is in accordance with other studies that reported similar results [2, 4, 29, 33, 45].
In conclusion, subsidence rates are clearly dependent on the measurement that is used and lead to incomparable results between studies. More so, the correlation between the occurrence of subsidence and clinical satisfaction for the individual after ACDF remains obscure.
Study limitations
There are two shortcomings limiting the validity of this study.
First, the surrogate parameter for clinical outcome was represented by the intensity of neck pain, which was present in all included patients. This in turn neglects other hallmarks of clinical success, being the improvement of myelopathic and radiculopathic signs such as gait ataxia or pain radiating to the upper extremities. We specifically chose a common denominator as representative for clinical outcome so as to sustain comparability within a rather large cohort that reports a plethora of clinical signs and symptoms. Albeit this seems to diminish the value of determining a surgery to be successful, it allows us to reference the various radiographic assessments to one definite variable. As was outlined in this and other published works, there is hardly any consensus on what clinical parameter to attribute to radiographic outcome [14, 16, 18]. We maintain the intensity of neck pain to be the most suitable parameter representative of cervical radiographic dimensions in combination with its duration to a lesser extent, much more so than either radiating arm pain or myelopathic signs and symptoms, all of which are primarily evoked by anatomically evident neural compression. Seeking association between neck pain and sagittal alignment, fusion and subsidence remains elusive, but perhaps the most promising for lack of a better alternative.
The other shortcoming stems from the retrospective nature of this study and the absence of preoperative complete diagnostics in a high number of patients, which precluded comparisons of pre- and postoperative imaging.
Conclusion
The radiographic outcome after ACDF for degenerative cervical spine disease rests on a multitude of parameters, for which no standardized assessment or measurement methods exist. The available methods vary greatly and apart from one do not demonstrate a significant correlation between radiographic and clinical outcome.
References
Ames CP, Blondel B, Scheer JK, Schwab FJ, Le Huec JC, Massicotte EM, Patel AA, Traynelis VC, Kim HJ, Shaffrey CI, Smith JS, Lafage V (2013) Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine 38:S149–S160. https://doi.org/10.1097/BRS.0b013e3182a7f449
Bartels RH, Donk RD, Feuth T (2006) Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery 58:502–508; discussion 502-508. https://doi.org/10.1227/01.NEU.0000197258.30821.50
Buchowski JM, Liu G, Bunmaprasert T, Rose PS, Riew KD (2008) Anterior cervical fusion assessment: surgical exploration versus radiographic evaluation. Spine 33:1185–1191. https://doi.org/10.1097/BRS.0b013e318171927c
Cabraja M, Oezdemir S, Koeppen D, Kroppenstedt S (2012) Anterior cervical discectomy and fusion: comparison of titanium and polyetheretherketone cages. BMC Musculoskelet Disord 13:172. https://doi.org/10.1186/1471-2474-13-172
Cannada LK, Scherping SC, Yoo JU, Jones PK, Emery SE (2003) Pseudoarthrosis of the cervical spine: a comparison of radiographic diagnostic measures. Spine 28:46–51. https://doi.org/10.1097/01.brs.0000038157.49250.59
Cauthen JC, Kinard RE, Vogler JB, Jackson DE, DePaz OB, Hunter OL, Wasserburger LB, Williams VM (1998) Outcome analysis of noninstrumented anterior cervical discectomy and interbody fusion in 348 patients. Spine 23:188–192
Cloward RB (1958) The anterior approach for removal of ruptured cervical disks. J Neurosurg 15:602–617. https://doi.org/10.3171/jns.1958.15.6.0602
Cobb JR (1948) Outline for the study of scoliosis. The American Academy of Orthopedic Surgeons Instructional Course Lectures 5
Davis RJ, Kim KD, Hisey MS, Hoffman GA, Bae HW, Gaede SE, Rashbaum RF, Nunley PD, Peterson DL, Stokes JK (2013) Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled multicenter clinical trial: clinical article. J Neurosurg Spine 19:532–545. https://doi.org/10.3171/2013.6.SPINE12527
Di Martino A, Papalia R, Albo E, Cortesi L, Denaro L, Denaro V (2015) Cervical spine alignment in disc arthroplasty: should we change our perspective? Eur Spine J 24(Suppl 7):810–825. https://doi.org/10.1007/s00586-015-4258-6
Elias F (1958) Roentgen findings in the asymptomatic cervical spine. N Y State J Med 58:3300–3303
Faldini C, Miscione MT, Acri F, Leonetti D, Nanni M, Chehrassan M, Giannini S (2012) Single level cervical fusion by an anterior approach using autologous bone graft influences the adjacent levels degenerative changes: clinical and radiographic results at 10-year minimum follow-up. Eur Spine J 21:90–93. https://doi.org/10.1007/s00586-012-2215-1
Feng SW, Chang MC, Chou PH, Lin HH, Wang ST, Liu CL (2018) Implantation of an empty polyetheretherketone cage in anterior cervical discectomy and fusion: a prospective randomised controlled study with 2 years follow-up. Eur Spine J 27:1358–1364. https://doi.org/10.1007/s00586-017-5450-7
Fujiwara H, Oda T, Makino T, Moriguchi Y, Yonenobu K, Kaito T (2018) Impact of cervical sagittal alignment on axial neck pain and health-related quality of life after cervical laminoplasty in patients with cervical spondylotic myelopathy or ossification of the posterior longitudinal ligament: a prospective comparative study. Clin Spine Surg 31:E245–e251. https://doi.org/10.1097/bsd.0000000000000619
Gercek E, Arlet V, Delisle J, Marchesi D (2003) Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J 12:513–516. https://doi.org/10.1007/s00586-003-0539-6
Gore DR (2001) Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine 26:2463–2466. https://doi.org/10.1097/00007632-200111150-00013
Gore DR, Sepic SB, Gardner GM, Murray MP (1987) Neck pain: a long-term follow-up of 205 patients. Spine 12:1–5. https://doi.org/10.1097/00007632-198701000-00001
Grob D, Frauenfelder H, Mannion AF (2007) The association between cervical spine curvature and neck pain. Eur Spine J 16:669–678. https://doi.org/10.1007/s00586-006-0254-1
Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B (2000) Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine 25:2072–2078
Hipp JA, Reitman CA, Wharton N (2005) Defining pseudoarthrosis in the cervical spine with differing motion thresholds. Spine 30:209–210
Hisey MS, Bae HW, Davis R, Gaede S, Hoffman G, Kim K, Nunley PD, Peterson D, Rashbaum R, Stokes J (2014) Multi-center, prospective, randomized, controlled investigational device exemption clinical trial comparing Mobi-C Cervical Artificial Disc to anterior discectomy and fusion in the treatment of symptomatic degenerative disc disease in the cervical spine. Int J Spine Surg 8. https://doi.org/10.14444/1007
Jackson BL, Harrison DD, Robertson GA, Barker WF (1993) Chiropractic biophysics lateral cervical film analysis reliability. J Manip Physiol Ther 16:384–391
Kaiser MG, Mummaneni PV, Matz PG, Anderson PA, Groff MW, Heary RF, Holly LT, Ryken TC, Choudhri TF, Vresilovic EJ, Resnick DK, Joint Section on Disorders of the S, Peripheral Nerves of the American Association of Neurological S, Congress of Neurological S (2009) Radiographic assessment of cervical subaxial fusion. J Neurosurg Spine 11:221–227. https://doi.org/10.3171/2009.3.SPINE08719
Kaptain GJ, Simmons NE, Replogle RE, Pobereskin L (2000) Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg 93:199–204
Katsuura A, Hukuda S, Imanaka T, Miyamoto K, Kanemoto M (1996) Anterior cervical plate used in degenerative disease can maintain cervical lordosis. J Spinal Disord 9:470–476
Kim JH, Kim JH, Kim JH, Kwon TH, Park YK, Moon HJ (2015) The relationship between neck pain and cervical alignment in young female nursing staff. J Korean Neurosurg Soc 58:231–235. https://doi.org/10.3340/jkns.2015.58.3.231
Kim W-B, Hyun S-J, Choi H, Kim K-J, Jahng T-A, Kim H-J (2016) Long-term follow-up results of anterior cervical inter-body fusion with stand-alone cages. J Korean Neurosurg Soc 59:385–391. https://doi.org/10.3340/jkns.2016.59.4.385
Laing RJ, Ng I, Seeley HM, Hutchinson PJ (2001) Prospective study of clinical and radiological outcome after anterior cervical discectomy. Br J Neurosurg 15:319–323
Lemcke J, Menz H, Al-Zain F, Meier U (2007) Outcome after cervical anterior fusion--a clinical study of 368 patients. Z Orthop Unfall 145:744–752. https://doi.org/10.1055/s-2007-965800
Lofgren H, Johannsson V, Olsson T, Ryd L, Levander B (2000) Rigid fusion after cloward operation for cervical disc disease using autograft, allograft, or xenograft: a randomized study with radiostereometric and clinical follow-up assessment. Spine 25:1908–1916
Mochida J, Nishimura K, Nomura T, Toh E, Chiba M (1996) The importance of preserving disc structure in surgical approaches to lumbar disc herniation. Spine 21:1556–1563 discussion 1563-1554
Moon HJ, Kim JH, Kim JH, Kwon TH, Chung HS, Park YK (2011) The effects of anterior cervical discectomy and fusion with stand-alone cages at two contiguous levels on cervical alignment and outcomes. Acta Neurochir 153:559–565. https://doi.org/10.1007/s00701-010-0879-z
Pechlivanis I, Thuring T, Brenke C, Seiz M, Thome C, Barth M, Harders A, Schmieder K (2011) Non-fusion rates in anterior cervical discectomy and implantation of empty polyetheretherketone cages. Spine 36:15–20. https://doi.org/10.1097/BRS.0b013e3181cbf870
Scheer JK, Tang JA, Smith JS, Acosta FL Jr, Protopsaltis TS, Blondel B, Bess S, Shaffrey CI, Deviren V, Lafage V, Schwab F, Ames CP, Group tISS (2013) Cervical spine alignment, sagittal deformity, and clinical implications. J Neurosurg Spine 19:141–159. https://doi.org/10.3171/2013.4.SPINE12838
Shad A, Leach JC, Teddy PJ, Cadoux-Hudson TA (2005) Use of the Solis cage and local autologous bone graft for anterior cervical discectomy and fusion: early technical experience. J Neurosurg Spine 2:116–122. https://doi.org/10.3171/spi.2005.2.2.0116
Shiban E, Gapon K, Wostrack M, Meyer B, Lehmberg J (2016) Clinical and radiological outcome after anterior cervical discectomy and fusion with stand-alone empty polyetheretherketone (PEEK) cages. Acta Neurochir 158:349–355. https://doi.org/10.1007/s00701-015-2630-2
Shiban E, Meyer B, Lehmberg J (2016) Influence of demineralized bone matrix on clinical and radiological outcome in anterior cervical discectomy and fusion. Spine J 16:S354–S355. https://doi.org/10.1016/j.spinee.2016.07.467
Skolasky RL, Maggard AM, Hilibrand AS, Northrup BE, Ullrich CG, Albert TJ, Coe JD, Riley LH 3rd. (2006) Agreement between surgeons and an independent panel with respect to surgical site fusion after single-level anterior cervical spine surgery: a prospective, multicenter study. Spine 31:E503–E506. https://doi.org/10.1097/01.brs.0000224503.31608.f9
Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40-a:607–624
Sudhakar N, Laing RJC, Redfern RM (2003) Assessment of fusion after anterior cervical discectomy. Br J Neurosurg 17:54–59. https://doi.org/10.3109/02688690309177972
Tuli SK, Chen P, Eichler ME, Woodard EJ (2004) Reliability of radiologic assessment of fusion: cervical fibular allograft model. Spine 29:856–860
Upadhyaya CD, Wu JC, Trost G, Haid RW, Traynelis VC, Tay B, Coric D, Mummaneni PV (2012) Analysis of the three United States Food and Drug Administration investigational device exemption cervical arthroplasty trials. J Neurosurg Spine 16:216–228. https://doi.org/10.3171/2011.6.SPINE10623
Villavicencio AT, Babuska JM, Ashton A, Busch E, Roeca C, Nelson EL, Mason A, Burneikiene S (2011) Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery 68:1309–1316; discussion 1316. https://doi.org/10.1227/NEU.0b013e31820b51f3
Wu WJ, Jiang LS, Liang Y, Dai LY (2012) Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J 21:1374–1382. https://doi.org/10.1007/s00586-011-2131-9
Zajonz D, Franke AC, von der Hoh N, Voelker A, Moche M, Gulow J, Heyde CE (2014) Is the radiographic subsidence of stand-alone cages associated with adverse clinical outcomes after cervical spine fusion? An observational cohort study with 2-year follow-up outcome scoring. Patient Saf Surg 8:43. https://doi.org/10.1186/s13037-014-0043-4
Funding
The study was completely financed by the Department of Neurosurgery.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent was not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine degenerative
Rights and permissions
About this article
Cite this article
Obermueller, T., Wagner, A., Kogler, L. et al. Radiographic measurements of cervical alignment, fusion and subsidence after ACDF surgery and their impact on clinical outcome. Acta Neurochir 162, 89–99 (2020). https://doi.org/10.1007/s00701-019-04139-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04139-1