Abstract
Purpose
The human standing position requires permanent reciprocal spino-pelvic adjustments to obtain a dynamic and economic posture. This study focuses on a hypokyphotic Lenke 1 adolescent idiopathic scoliosis (AIS) patients cohort and points out their particular lumbo-pelvic adaptive mechanisms to maintain a neutral sagittal balance.
Methods
Preoperative retrospective analysis of prospectively collected data on a monocentric cohort of 455 AIS patients planned for corrective surgery. Radiological low-dose system coupled with a validated clinical routine software allowed to obtain data from eighty-four hypokyphotic [thoracic kyphosis (TK) <20°] Lenke 1 patients and were separately analyzed. Bilateral Student and one-way ANOVAs were conducted for statistical analysis.
Results
Mean Cobb angle was 46.3° (±7.2), TK was 11° (±7.1), sagittal vertical axis (SVA) was −10.1 mm (±30.9), pelvic incidence (PI) was 55.7° (±12.9). Fifty percents of patients were posteriorly imbalanced. Among them, patients with a low PI used an anteversion of their pelvis [indicated by a high pelvic tilt (PT) angle] but were not able to increase their lumbar lordosis (LL) to minimize the posterior spinal shift.
Conclusions
Hypokyphotic Lenke 1 AIS patients use lumbo-pelvic compensatory mechanisms to maintain their global balance with a poor effectiveness. Subjects with a low PI have a restricted range of LL adaptation. Attention should be paid during surgical planning not to overcorrect lordosis in the instrumented levels in case of non-selective fusion, that may induce posterior shift of the fusion mass and expose to junctional syndromes and poor functional outcomes in this particular patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human standing position requires subtle and permanent reciprocal spino-pelvic adjustments to obtain and maintain a dynamic and economic posture [1, 2]. Correlations between pelvic parameters and lumbar sagittal alignment in healthy adults and children have been widely investigated during the last decade [3–5], and need to be considered for any surgical correction of spinal deformity and particularly adolescent idiopathic scoliosis (AIS) and degenerative deformities [6, 7]. Asymptomatic subjects have a lumbar lordosis (LL) which is directly correlated to pelvic incidence (PI) (LL° = PI° ± 10°) and thoracic kyphosis (TK) equaling LL in order to keep a neutral global sagittal balance [8]. In spine deformity surgery, attention must be paid to restore sufficient lumbar lordosis, adapted to the pelvic incidence, to avoid flat back syndrome and poor functional outcomes [9].
In Lenke 1 curves, which are the most frequent, thoracic alignment is often flattened [10], and the adjacent non-structural curves need to adapt with more or less lordosis/kyphosis in order to maintain the patient’s neutral balance. The sagittal lumbar alignment is, therefore, determined by both anatomical fixed pelvic parameters and the position of progressive scoliotic thoracic spine. The aim of the present study was to assess the lumbo-pelvic alignment and the global sagittal balance in Lenke 1 hypokyphotic AIS patients, and to determine the nature of the compensatory mechanisms playing a role into maintenance of a neutral sagittal balance.
Materials and methods
Patients
After Institution’s Ethics Committee approval, 455 patients followed for progressive AIS and planned for surgery in a single institution were prospectively included between 2010 and 2015. Curves were classified according to the Lenke’s system and Lenke 1 with thoracic kyphosis lower than 20° were kept for the study. Exclusion criteria were non-idiopathic scoliosis or any past medical history of spine surgery.
Imaging
All patients underwent standing biplanar stereoradiographs (EOS Imaging, Paris, France). Acquisitions were performed according to a previously validated protocol [11], in a position of straight-ahead look and fists on orbits to avoid superposition of the arms over the spine.
A validated radiological analysis tool (Kodak Carestream, Rochester, NY, USA) [12], used in routine clinical practice, allowed to perform measurements of angles and distances.
In the frontal plane, main Cobb angle and location of the apical vertebra were recorded.
In the sagittal plane, the following parameters were collected in order to appreciate segmental and global spinal balance:
-
Pelvic incidence (PI) and pelvic tilt (PT). PI was considered low for values below 44°, moderate for values between 44° and 62° and high for values above 62° as recommended by Duval-Beaupère et al. [1].
-
Lumbar lordosis (LL) measured from cranial endplate of L1 to cranial endplate of S1. Lumbar lordosis was considered adapted to PI for PI + 10° > LL > PI − 10° [8].
-
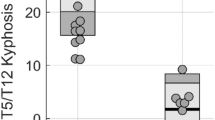
Thoracic kyphosis (TK) measured from cranial endplate of T1 to caudal endplate of T12, subdivided into proximal TK (T1T5) and distal TK (T5T12).
-
Global sagittal balance evaluated by the C7-plumb line (SVA): horizontal distance between the posterosuperior edge of S1 and a vertical line through the center of C7. A positive SVA distance represented a C7 placed forward S1. Patients were considered neutrally balanced for SVA values comprised between −10 and +10 mm [13].
-
Transitional vertebra between functional lumbar lordosis and functional thoracic kyphosis according to the Roussouly et al. [3]: noted 0 when in L1, −1 when in T12, −2 when in T11, +1 when in L2, +2 when in L3.
The cohort was divided into three balance groups: neutral balance for −10 mm < SVA < 10 mm (N), posterior imbalance for SVA <−10 mm (POST) and anterior imbalance for SVA >10 mm (ANT). The different components of their respective sagittal alignment were studied and compared to identify compensatory mechanisms.
Statistical analysis
Statistical analysis was performed on Graphpad Prism v5 (GraphPad Software Inc., La Jolla, CA, USA). Bilateral Student t test were used to compare two groups of patients. One-way ANOVAs with Tukey post-tests were used to compare three or more groups. When required, one sample t tests were also used to test a sample against a theoretical value. Statistical significance was set at p < 0.05.
Results
Eighty-four Lenke 1 patients (66 girls and 18 boys) with hypokyphosis (TK <20°) were identified. Mean age was 15.2 years (±1.9). Demographic results are summarized in Table 1.
Transitional vertebras are summarized in Fig. 1. Mean transitional vertebra score was −0.06 (±0.41). One sample t test against the theoretical value of 0 (i.e., L1) found p = 0.09, indicating that in hypokyphotic scoliotic patients, L1 could be considered as the upper limit of the functional lumbar lordosis and L1S1 sagittal Cobb angle could, therefore, effectively estimate their lumbar lordosis.
Hypokyphotic Lenke 1 AIS patients were posteriorly imbalanced in more than half cases (Table 2). In the POST group, 23 patients (51.1 %) had a LL value correlated to their PI and 22 patients (48.9 %) had a hypolordotic lumbar profile (LL <PI − 10). The comparison of posteriorly imbalanced hypokyphotic Lenke 1 AIS sagittal parameters according to their LL is summarized in Table 3.
Still in the POST group, 10 patients (22.2 %) had a low PI and 35 (77.8 %) had a moderate or high PI. The comparison of posteriorly imbalanced hypokyphotic Lenke 1 AIS sagittal parameters according to their PI is summarized in Table 4.
PI was significantly lower in the POST group than in the N group (p = 0.02) (Fig. 2). LL was found to be lower in the POST group than in the N group (p = 0.04) (Fig. 3). TK (global, proximal and distal) was not different between the three groups.
Global sagittal balance according to LL was studied. SVA was neutral for hypolordotic patients whereas patients with LL adapted to PI were in a posterior imbalance position (SVA = −2.6 ± 30 mm vs SVA = −18.8 ± 29 mm, p = 0.02). This result indicates that hypokyphotic patients could adapt their LL to maintain a neutral sagittal balance.
Discussion
Sagittal functional curvatures
It is commonly accepted to measure lumbar lordosis as the sagittal Cobb angle between upper endplate of L1 and upper endplate of S1. Since transitional anomalies (defined by more or less than five lumbar vertebrae) are becoming increasingly prevalent in the human general population (6.6 % of transitional anomalies at lumbo-sacral junction [14, 15]) and in the AIS population (10 % of thoracolumbar/lumbo-sacral transitional anomalies [1]), and taking into account the functional sagittal curves, some authors have proposed a geometric definition to lumbar lordosis [16]. This cohort study found no difference for lumbar lordosis between the two methods (Cobb and geometric).
Global balance
The present study demonstrated that more than 50 % of Lenke 1 hypokyphotic patients were posteriorly imbalanced. This proportion seems to be very high and probably depends on defined SVA limits; however, similar results have been reported on hypokyphotic Lenke 1 AIS patients using other global balance criteria [17]. Our patients used compensatory mechanisms to shift their trunk forward, and therefore reduced their LL, which was no longer adapted to their PI. This mechanism was poorly efficient since only 20 % of the hypolordotic–hypokyphotic patients were able to maintain a neutral sagittal balance. Another compensatory mechanism is a PT increase as shown in Table 3. Clement et al. found the same trends and showed that LL was influenced by both the PI and the TK in main thoracic AIS patients [18]. Their hypothesis was that a change in the sagittal functional transitional levels occurred in AIS patients but our results do not support this statement, possibly due to a difference into the lumbar modifier between the two cohorts according to Lenke’s classification. This difference could interestingly be investigated in further studies.
Posteriorly imbalanced patients with a low PI had an adapted LL but a high PT, indicating that these subjects try to compensate their posterior imbalance using a pelvic anteversion mechanism, whereas patients with a moderate to high PI had a non-adapted LL (lower than the theoretical lowest value of LL = PI − 10) and a low PT, indicating that these subjects try to compensate their posterior imbalance into their lumbar spine rather than into the pelvis.
Low PI appeared to be a risk factor for posterior imbalance since only 6.7 % of patients were adequately balanced in this subgroup. This could be explained by their poor compensation ability with a low amplitude of pelvic ante- or retroversion as described by Roussouly et al. [19] combined with the natural segmental extension deformity in thoracic AIS [20].
Consequences in preoperative planning
In Lenke 1 AIS surgical correction, several authors have raised the interest of using long constructs distally anchored on a stable and not rotated vertebra (which can be L2 or L3) to avoid adding-on and distal junctional kyphosis phenomena during follow-up [21]. Planning of the sagittal distal rod-bending, fixing segmental LL in such constructs extending to lumbar spine must take into account not only PI but also the expected postoperative CT, which is unfortunately to date impossible to predict.
In AIS surgical correction using posteromedial translation, recent studies [22] have shown that LL was able to secondarily adapt to TK correction within 3 months after surgery.
Hypokyphotic profile correction is a raising challenge in scoliosis surgery and modern techniques and instrumentations still fail to restore a normal TK (approximately equal to LL [6]), independently from the type of thoracic device or surgical approach [23, 24].
Since maximum TK obtained in hypokyphotic thoracic scoliosis usually remains in the lower range of normality, attention should be paid not to overcorrect lumbar lordosis by only considering a sagittal correction goal based on PI. This way of planning sagittal correction may induce a posterior shift of the fusion mass that could be responsible for proximal junctional kyphosis when fusion extends to lumbar levels. Patients with a low PI, who are unable to increase their PT enough to maintain a neutral sagittal balance, are particularly exposed to this type of complication. Figures 4, 5, 6 and 7 illustrate this proposition in a patient who had adapted and stabilized her pelvic version 6 months after surgery [lumbar counter curve was very stiff on the lateral bending films, with a wedging L3L4 disc (>10° on left bending film) and vertebral rotation on L2 and L3. A selective Cobb-to-Cobb fusion (T4 to L1) may have been performed, but with an uncertain result on the frontal plane outcomes].
Same patient as Fig. 4, standing lateral radiograph. SVA = 8 mm (N), thoracic kyphosis TK = 16° (proximal thoracic kyphosis T1T5 = 14°, distal thoracic kyphosis T5T12 = 0°), PI = 38° (low PI), LL = 25°, pelvic tilt PT = −12°. The patient has a low PI and a retroverted pelvis, and compensates with a hypolordosis to maintain a neutral sagittal balance
Two years postoperative low-dose radiographic controls of Fig. 4 patient. Main Cobb is 22°
Same patient as Fig. 5. SVA = −20 mm, TK = 41° (proximal thoracic kyphosis T1T5 = 30°, distal thoracic kyphosis T5T12 = 10°), PI = 38°, LL = 40°, PT = −4°. The increase of TK and LL come along with an increase of pelvic anteversion. A posterior shift of the fusion mass appears, and an increase of segmental lordosis at cervicothoracic junction, may indicate a future proximal junctional kyphosis
On the contrary, a careful correction of LL and TK in such patients can lead to restore a neutral global sagittal balance, as illustrated on Figs. 8, 9, 10 and 11.
Same patient as Fig. 8, standing lateral radiograph. SVA = −18 mm (POST), thoracic kyphosis TK = 2°, PI = 32° (low PI), LL = 36°, pelvic tilt PT = 2°. This patient has an adapted LL. The posterior imbalance is partly compensated by a pelvic anteversion
Two years postoperative low-dose radiographic controls of Fig. 8 patient. Main Cobb is 25°
Same patient as Fig. 8. SVA = −8 mm (N), TK = 22°, PI = 32°, LL = 38°, PT = 2°. TK has been corrected to normal values, LL has not been modified. Global sagittal balance is restored
Limitations of the study
The present study detailed sagittal spinal balance focusing on the relative adjustments of the segmental curvatures (TK/LL/PI and PT) in hypokyphotic Lenke 1 patients. It did not take into account the participation of the cervical spine into the global sagittal balance because cervical sagittal measurements have been shown to be extremely variable for the same subject in a standing position [25]. Further investigations need to be conducted in order to be able to optimally quantify and analyze adaptive behavior of this particularly mobile segment.
Sagittal plane analysis usually stands on measurements performed on standing radiographs and the results are the reflect of a static and plural position. The same patient having the same lateral radiograph at two different timepoints will have slightly different sagittal angles and distances values, included into what Dubousset called the sustentation conus [26]. Analyzing the spinal sagittal alignment on unique radiographs is a rough approximation of the sagittal balance that does not take into account, for instance, proximo-distal spinal flexibility during a walking period. Dynamic measurements using gait analysis procedures would be mandatory for the evaluation of the global spinal balance in AIS and would be particularly useful for the spino-pelvic analysis. Gait analysis would allow to appreciate the sagittal spino-pelvic alignment modifications due to the rotation of the pelvis around the center of rotation of the hips during a cycle of walk and compare AIS characteristics to asymptomatic subjects [27].
Only severe Lenke 1 curves have been analyzed in the present study, which represents an important pitfall if we want to identify and understand the mechanisms and the genesis of the compensatory sagittal adaptations.
Conclusion
The present work found that the actual LL in hypokyphotic Lenke 1 AIS patients was lower than the theoretical one based on their PI. LL behaved as an adjustable parameter which modifications aimed to maintain global sagittal balance.
This finding is particularly relevant for the preoperative surgical planning of such patients with low PI: attention should be paid not to give too much lordosis in the instrumented levels in case of fusion extending to the lumbar spine that may theoretically induce a posterior shift of the fusion mass and expose the patient to junctional syndromes and poor functional outcomes.
References
Duval-Beaupère G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20:451–462
Steffen JS, Obeid I, Aurouer N et al (2010) 3D postural balance with regard to gravity line: an evaluation in the transversal plane on 93 patients and 23 asymptomatic volunteers. Eur Spine J 19:760–767
Roussouly P, Gollogly S, Berthonnaud E et al (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 30:346–353
Mac-Thiong JM, Labelle H, Berthonnaud E et al (2007) Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J 16:227–234
Vialle R, Levassor N, Rillardon L et al (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am 87:260–267
Lamartina C, Berjano P, Petruzzi M, Sinigaglia A, Casero G, Cecchinato R, Damilano M, Bassani R (2012) Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis. Eur Spine J 21:27–31
Schwab F, Patel A, Ungar B, Farcy JP, Lafage V (2010) Adult spinal deformity postoperative standing imbalance: how much can you tolerate? An overview of key parameters assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 35:2224–2231
Sanchez-Mariscal F, Gomez-Rice A, Izquierdo E, Pizones J et al (2012) Correlation of radiographic and functional outcomes in patients who underwent primary scoliosis surgery in adult age. Spine (Phila Pa 1976) 37:592–598
Ilharreborde B, Morel E, Mazda K, Dekutoski MB (2009) Adjacent segment disease after instrumented fusion for idiopathic scoliosis: review of current trends and controversies. J Spinal Disord Tech 22:530–539
Luk KD, Vidyadhara S, Lu DS et al (2010) Coupling between sagittal and frontal plane deformity correction in idiopathic thoracic scoliosis and its relationship with postoperative sagittal alignment. Spine (Phila Pa 1976) 35:1158–1164
Ilharreborde B, Sebag G, Skalli W, Mazda K (2013) Adolescent idiopathic scoliosis treated with posteromedial translation: radiologic evaluation with a 3D low-dose system. Eur Spine J 22:2382–2391
Vidal C, Ilharreborde B, Azoulay R et al (2013) Reliability of cervical lordosis and global sagittal spinal balance measurements in adolescent idiopathic scoliosis. Eur Spine J 22:1362–1367
Lamartina C, Berjano P (2014) Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur Spine J 23:1177–1189
Apazidis A, Ricart PA, Diefenbach CM et al (2011) The prevalence of transitional vertebrae in the lumbar spine. Spine J 11:858–862
Ibrahim DA, Myung KS, Skaggs DL (2013) Ten percent of patients with adolescent idiopathic scoliosis have variations in the number of thoracic or lumbar vertebrae. J Bone Joint Surg Am 95:828–833
Vaz G, Roussouly P, Berthonnaud E et al (2002) Morphology and equilibrium of pelvis and spine. Eur Spine J 11:80–87
La Maida GA, Zottarelli L, Mineo GV, Misaggi B (2013) Sagittal balance in adolescent idiopathic scoliosis: radiographic study of spino-pelvic compensation after surgery. Eur Spine J 22:S859–S867
Clément J, Geoffray A, Yagoubi F et al (2013) Relationship between thoracic hypokyphosis, lumbar lordosis and sagittal pelvic parameters in adolescent idiopathic scoliosis. Eur Spine J 22:2414–2420
Roussouly P, Pinheiro-Franco JL (2011) Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 20:609–618
Kouwenhoven JW, Castelein RM (2008) The pathogenesis of adolescent idiopathic scoliosis: review of the literature. Spine (Phila Pa 1976) 33:2898–2908
Erdemir C, Musaoglu R, Selek O, Gok U, Sarlak AY (2015) Distal fusion level selection in Lenke 1A curves according to axial plane analyses. Spine J 15:2378–2384
Blondel B, Lafage V, Schwab F et al (2012) Reciprocal sagittal alignment changes after posterior fusion in the setting of adolescent idiopathic scoliosis. Eur Spine J 21:1964–1971
Sucato DJ, Agrawal S, O′Brien MF et al (2008) Restoration of thoracic kyphosis after operative treatment of adolescent idiopathic scoliosis: a multicenter comparison of three surgical approaches. Spine (Phila Pa 1976) 33:2630–2636
Crawford AH, Lykissas MG, Gao X et al (2013) All-pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery: a comparative radiographic study with a minimum 2-year follow-up. Spine (Phila Pa 1976) 38:1199–1208
Abelin-Genevois K, Idjerouidene A, Roussouly P, Vital JM, Garin C (2014) Cervical spine alignment in the pediatric population: a radiographic normative study of 150 asymptomatic patients. Eur Spine J 23:1442–1448
Dubousset J, Lavaste F, Skalli W, Lafage V (2011) Modeling the spine and spinal cord. Bull Acad Natl Med 195:1831–1842
Paul JC, Patel A, Bianco K, Godwin E, Naziri Q, Maier S, Lafage V, Paulino C, Errico TJ (2014) Gait stability improvement after fusion surgery for adolescent idiopathic scoliosis is influenced by corrective measures in coronal and sagittal planes. Gait Posture 40(4):510–515
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This work has been approved by the Institution’s Ethics Committee.
Conflict of interest
No direct or indirect benefits consecutive to this work have been or will be received by any of the authors. No author received or will receive any form of financial or material support consecutive to the present work.
Rights and permissions
About this article
Cite this article
Vidal, C., Mazda, K. & Ilharreborde, B. Sagittal spino-pelvic adjustment in severe Lenke 1 hypokyphotic adolescent idiopathic scoliosis patients. Eur Spine J 25, 3162–3169 (2016). https://doi.org/10.1007/s00586-016-4681-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4681-3