Abstract
Purpose
To compare the outcomes of microendoscopic discectomy and open discectomy for patients with lumbar disc herniation.
Methods
An extensive search of studies was performed in PubMed, Medline, Embase, Cochrane library and Google Scholar. The following outcome measures were extracted: visual analogue scale (VAS), Oswestry disability index (ODI), complication, operation time, blood loss and length of hospital stay. Data analysis was conducted with RevMan 5.0.
Results
Five randomized controlled trials involving 501 patients were included in this meta-analysis. The pooled analysis showed that there was no significant difference in the VAS, ODI or complication between the two groups. However, compared with the open discectomy, the microendoscopic discectomy was associated with less blood loss [WMD = −151.01 (−288.22, −13.80), P = 0.03], shorter length of hospital stay [WMD = −69.33 (−110.39, −28.28), P = 0.0009], and longer operation time [WMD = 18.80 (7.83, 29.76), P = 0.0008].
Conclusions
Microendoscopic discectomy, which requires a demanding learning curve, may be a safe and effective alternative to conventional open discectomy for patients with lumbar disc herniation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lumbar disc herniation is a common pathological change of the lumbar spine [1, 2]. Surgical discectomy is indicated for the patients who were nonresponsive to conservative management (at least 6 weeks) or had progressive neurological impairment [1–3]. The surgical approaches include open discectomy, microdiscectomy, microendoscopic discectomy and percutaneous endoscopic discectomy [4].
Conventional open discectomy (OD) has been regarded as a “standard” surgical fashion [4, 5], which was firstly described by Mixter and Barr in 1934 [6]. This technique could relieve patients’ pain and improve their nerve function. However, the greatest problem is the surgical trauma of paravertebral muscles, which is related with the failed back surgery syndrome [7, 8]. Besides, some research noticed that the long-term satisfaction of this surgical approach would obviously deteriorate due to surgical scarring and adhesion [9, 10].
Foley and Smith introduced the microendoscopic discectomy (MED) technique in 1997 [11] and reported satisfactory clinical outcomes of 100 patients who underwent this technique in the following year [12]. This minimally invasive technique was performed by a transmuscular approach with advanced optics. Some reports compared intraoperative electromyography [13] and postoperative MRI [14] in the patients who were treated with the two techniques. These results revealed that the MED approach was superior to the OD approach in muscle and soft tissue damage. In addition, the MED technique markedly reduced postoperative pain of patients and facilitated their recovery [11, 15, 16].
Most reports indicated the MED approach could reduce the surgical trauma, length of hospital stay and time to return to work/activity [9, 15, 17–21]. However, the safety of this approach has been questioned due to the small working space which might make it difficult to avoid the damage to dural and neural structures. Some studies reported that there were more dural tear, root injury and recurrent herniation in the microendoscopic group compared with the open group [21, 22]. Teli et al. [22] also noticed the length of hospital stay was longer in the microendoscopic group than in the open group. As a result, a meta-analysis of relevant studies is necessary to establish the current state of evidence. This study aims to compare the outcomes of the microendoscopic discectomy and the open discectomy.
Materials and methods
Inclusion criteria
Randomized controlled trials (RCTs) on treatment of lumbar disc herniation were reviewed. The criteria for inclusion of an article were: (1) patients were 18 years old or older; (2) patients were diagnosed with symptomatic lumbar disc herniation; (3) interventions: microendoscopic discectomy and open discectomy; (4) the study reported at least one desirable outcome; (5) all included patients were followed up at least 1 year after surgery; (6) patients were excluded if they were associated with intervertebral instability, spondylolisthesis, underwent intervertebral fusion, infection, malignancy, deformity, rheumatoid arthritis, previous surgery of lumbar spine, cauda equina symptoms, cervical or lumbar spine stenosis of any etiology.
Search strategy
A computerized search of RCT published between 1997 and September 2015 was performed in PubMed, Medline, Embase and Cochrane Central Register of Controlled Trials (CENTRAL) (Wiley Online Library) and Google Scholar. The following key words were used for search: “microendoscopic”, “endoscopic”, “discectomy”, “open”, “conventional” and “lumbar disc herniation” with various combinations of the operators “AND”, “NOT”, and “OR”. We restricted the language to English.
Selection of studies
Two reviewers (JLH and SWX) independently reviewed all subjects, abstracts, reference lists and the full text of articles that were potentially eligible based on abstract review. Then the eligible trials were selected according to the inclusion criteria. When consensus could not be reached, a third reviewer (ZCY) was consulted to resolve the disagreement.
Data extraction
Two reviewers (JLH and SWX) extracted data independently. The data extracted included the following categories: patients (selection criteria, age, sex and follow-up time), treatments (intervention details) and clinical outcomes: visual analogue scale (VAS), Oswestry disability index (ODI), complication, operation time, blood loss and length of hospital stay.
Assessment of study quality
Two reviewers (JLH and ZJW) independently assessed the quality of each study using the 12 criteria and instructions recommended by the Cochrane Back Review Group (CBRG) [23], and met to reach consensus. The items were scored with ‘yes’, ‘no’, or ‘unsure’. As before, if consensus could not be reached, a third reviewer (ZCY) was consulted to resolve the disagreement. Studies were categorized as having a “low risk of bias” when at least six criteria, and the study had no serious methodological flaws. Studies with serious flaws or those in which fewer than six of the criteria were met should be rated as having a “high risk of bias”.
Data analysis
Data analysis was performed with RevMan 5.0 (the Cochrane Collaboration). Two reviewers (JLH and SWX) monitored the data input to ensure there were no errors. Risk ratio (RR) or odds ratio (OR) was used as a summary statistic to analyze dichotomous variables, and the standardized mean difference (SMD) was used to analyze continuous variables. Both were reported with 95 % confidence intervals (CIs), and a P value of 0.05 was used as the level of statistical significance. Random-effects or fixed-effects models were used depending on the heterogeneity of the studies included. Heterogeneity was tested using I-square test, where I 2 > 50 % implied heterogeneity.
Results
Search results
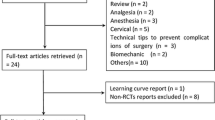
The search strategy yielded 204 relevant articles. There were only thirteen studies taken for a comprehensive evaluation. After evaluating the full article of the remaining articles, eight more studies were excluded due to data record or unsuitable interventions, four of them due to adoption of percutaneous endoscopic lumbar discectomy [15, 24–26]. As a result, a total of five randomized controlled trials (RCTs) [9, 19–22] were identified in this study. The literature search procedure is shown in Fig. 1.
Baseline characteristics and quality assessment
These RCTs included a total of 501 patients, 253 patients were treated with microendoscopic discectomy (microendoscopic group) and 248 patients underwent open discectomy (open group). These studies were performed in various countries. The demographic distribution of both groups was similar and the baseline characteristics of each study are presented in Table 1. All studies had a quality score of 7–11 (low risk of bias). The detailed risk of bias in each study is summarized in Fig. 2.
Effectiveness
Three RCTs [20–22] reported the VAS score at the latest follow-up. However, one study [21] did not provide standard deviation (SD). The pooled result revealed no significant difference between the two groups [WMD = 0.27 (−0.12, 0.65), P = 0.18, I 2 = 77 %, Fig. 3]. Four studies [9, 19, 21, 22] compared the ODI score at the final follow-up between the two groups, whereas two RCTs [19, 21] did not provide the SD, the pooled analysis also showed the difference was not significant [WMD = −19.58 (−55.98, 16.83), P = 0.29, I 2 = 100 %, Fig. 4].
Safety
With the inconsistent definition of the complication across all included studies, the meta-analysis of overall complication was inappropriate. Therefore, only the major adverse events including dural tear, root injury, recurrence, reoperation and wound infection were analyzed in the present study. All RCTs [9, 19–22] reported the complication. The qualitative analysis revealed no significant difference in the complication of dural tear, root injury, recurrence, reoperation or wound infection between the two groups (all P > 0.05, Fig. 5).
All studies [9, 19–22] reported the operation time of the two groups. The result demonstrated the microendoscopic approach resulted in significantly longer operation time compared with the open approach [WMD = 18.80 (7.83, 29.76), P = 0.0008, I 2 = 88 %, Fig. 6]. Four RCTs [9, 19–21] compared the intraoperative blood loss between the two groups, while one of them did not provide the SD [21]. The pooled analysis showed that the blood loss of the microendoscopic group was significantly less than that of the open group [WMD = −151.01 (−288.22, −13.80), P = 0.03, I 2 = 98 %, Fig. 7]. All RCTs [9, 19–22] assessed the length of hospital stay, whereas one study [21] did not provide the SD. The result also indicated the microendoscopic discectomy was correlated with significantly shorter length of hospital stay compared with the open discectomy [WMD = −69.33 (−110.39, −28.28), P = 0.009, I 2 = 100 %, Fig. 8].
Discussion
This meta-analysis compared microendoscopic discectomy with open discectomy for symptomatic lumbar disc herniation (LDH). The pooled analysis showed that there was similar improvement of clinical symptoms (VAS and ODI) of patients in the two groups. The differences of dural tear, root injury, recurrence and reoperation between the two treatment groups were not statistically significant. However, compared with the open group, the microendoscopic group resulted in less blood loss, shorter length of hospital stay, and longer operation time. The results indicated the more time-consuming technique of microendoscopic discectomy had an advantage in less surgical trauma.
The VAS and ODI scores were used for clinical effectiveness assessment in this study. The pooled analysis showed that there was no significant difference in these parameters between the two groups, indicating the ability of both approaches to decompress the nerve root was similar. However, the evaluation of the VAS and ODI is more dependent on the subjective feeling of patients and the scores might be acquired variably by different investigators [27]. Therefore, the reliability of these results was investigated and the conclusions were consistent following sensitivity analysis. Besides, these heterogeneities are large (I 2 = 77 %, 100 %, respectively).
Complication is a very important factor for assessing surgical safety. Some previous studies reported that dural tear, root injury and recurrence in the microendoscopic group were more than those in the open group [21, 22]. A possible explanation is the poor perception of depth with microendoscopic operation [16, 21, 22] and the restricting confines of tubular retractor, which limit surgeon to orientate surgical instruments [21, 28]. Iatrogenic dural tear and root injury are common complications [29–31], which might result in clinical sequelae [32–35]. However, such complications in this study were similar in the two groups (P = 0.23, 0.30, respectively). The finding indicated that the microendoscopic technique, with advanced surgical instruments, could provide sufficient space to avoid and control damage to dural and neural structures.
The recurrence of herniation at the same level of lumbar is a major problem [36, 37], which ranges from 0.5 to 10.7 % [38, 39] and has been the major cause of long-term pain and reoperation [17, 40, 41]. The limited field of tubular retractor might restrict the ability of surgeon to identify and extract the free fragments within the disc space, which ultimately leads to more recurrence in the microendoscopic group than in the open group [22]. In the present study, the recurrence rate was 4.94 % (12/243) in the microendoscopic group and 1.69 % (4/236) in the open group. There seemed to be more recurrence of LDH in the microendoscopic group than in the open group. However, the difference was not statistically significant (RR = 2.71, P = 0.06). It is important to note that the P value (0.06) was not considerably large, which meant that the result might be different if the study number and sample were to increase.
Blood loss was taken for evaluating surgical trauma in this study. The result indicated the surgical trauma of the microendoscopic discectomy was smaller than that of the open discectomy, which was comparable with the previous studies [9, 19, 20]. Furthermore, the minimally invasive technique could facilitate early recovery of the patients and shorten their time to return to work or normal activities [21, 42]. The length of hospital stay in this study was also significantly shorter in the microendoscopic group compared with the open group. Operation time was taken to assess the surgical difficulty, and the pooled analysis revealed the microendoscopic group was associated with longer time to remove the compressive pathological tissue, which was similar with the previous literature [17, 19, 20]. However, it is important to note that the surgical time would reduce gradually with the improvement of operative proficiency [9, 32]. Perez-Cruet et al. [32] reported that the mean operation time was 110 min in the first 30 cases, whereas it was only 75 min in the last 30 cases.
The microendoscopic discectomy may be a reliable technique. However, this approach also has defects. First, there is a certain difficulty to suture the dural tear properly in the limited room [43]. Secondly, there is a demanding learning curve to adapt the difference between hand and eye coupling with the three-dimensional view in the open surgical field and hand and eye spatial separation with the two-dimensional view in the microendoscopic approach [32]. Thirdly, it is a cost-consuming surgical technique when compared with the conventional open discectomy [22, 44].
This study has some limitations. It is clear that we did not comment on the subject of cost-effectiveness, which is a pity that it is a complex system. Besides, clinical heterogeneity may be caused by the various surgical instruments and operative proficiency in different treatment centers. Furthermore, only small size sample could be enrolled in these studies and the follow-up periods were various (1–8 years). Finally, all of the documents were in English, there may be language bias.
Conclusions
This study only concentrated on the difference between clinical outcomes of the two surgical approaches. As compared with open discectomy, microendoscopic discectomy was associated with similar improvement of symptoms and smaller surgical trauma. Microendoscopic discectomy, which requires a demanding learning curve, maybe a safe and effective alternative to open discectomy for the patients with symptomatic lumbar disc herniation. As there are limitations in this study, high-quality RCTs should be performed to assess this conclusion.
References
Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, Cho CH, DePalma MJ, Dougherty PN, Fernand R, Ghiselli G, Hanna AS, Lamer T, Lisi AJ, Mazanec DJ, Meagher RJ, Nucci RC, Patel RD, Sembrano JN, Sharma AK, Summers JT, Taleghani CK, Tontz WJ, Toton JF (2014) An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 14:180–191. doi:10.1016/j.spinee.2013.08.003
Postacchini F (1999) Management of herniation of the lumbar disc. J Bone Jt Surg Br 81:567–576
Maroon JC (2002) Current concepts in minimally invasive discectomy. Neurosurgery 51:S137–S145
Blamoutier A (2013) Surgical discectomy for lumbar disc herniation: surgical techniques. Orthop Traumatol Surg Res 99:S187–S196. doi:10.1016/j.otsr.2012.11.005
Gibson JN, Waddell G (2007) Surgical interventions for lumbar disc prolapse: updated Cochrane Review. Spine (Phila Pa 1976) 32:1735–1747. doi:10.1097/BRS.0b013e3180bc2431
Mixter WJ, Barr JS (1934) Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med 211:210–215
Bokov A, Isrelov A, Skorodumov A, Aleynik A, Simonov A, Mlyavykh S (2011) An analysis of reasons for failed back surgery syndrome and partial results after different types of surgical lumbar nerve root decompression. Pain Phys 14:545–557
Fritsch EW, Heisel J, Rupp S (1996) The failed back surgery syndrome: reasons, intraoperative findings, and long-term results: a report of 182 operative treatments. Spine (Phila Pa 1976) 21:626–633
Hussein M, Abdeldayem A, Mattar MM (2014) Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: a prospective, randomized, controlled study with 8 years of follow-up. Eur Spine J 23:1992–1999. doi:10.1007/s00586-014-3296-9
Salenius P, Laurent LE (1977) Results of operative treatment of lumbar disc herniation: a survey of 886 patients. Acta Orthop 48:630–634
Foley KT (1997) Microendoscopic discectomy. Tech Neurosurg 3:301–307
Jhala A, Mistry M (2010) Endoscopic lumbar discectomy: experience of first 100 cases. Indian J Orthop 44:184–190. doi:10.4103/0019-5413.62051
Schick U, Dohnert J, Richter A, Konig A, Vitzthum HE (2002) Microendoscopic lumbar discectomy versus open surgery: an intraoperative EMG study. Eur Spine J 11:20–26
Muramatsu K, Hachiya Y, Morita C (2001) Postoperative magnetic resonance imaging of lumbar disc herniation: comparison of microendoscopic discectomy and Love’s method. Spine (Phila Pa 1976) 26:1599–1605
Ruetten S, Komp M, Merk H, Godolias G (2008) Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 33:931–939. doi:10.1097/BRS.0b013e31816c8af7
Nakagawa H, Kamimura M, Uchiyama S, Takahara K, Itsubo T, Miyasaka T (2003) Microendoscopic discectomy (MED) for lumbar disc prolapse. J Clin Neurosci 10:231–235
Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RH, Tan WF, Peul WC (2011) Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Neurosurgery 69(135–144):144. doi:10.1227/NEU.0b013e318214a98c
Arts M, Brand R, van der Kallen B, Lycklama ANG, Peul W (2011) Does minimally invasive lumbar disc surgery result in less muscle injury than conventional surgery? A randomized controlled trial. Eur Spine J 20:51–57. doi:10.1007/s00586-010-1482-y
Garg B, Nagraja UB, Jayaswal A (2011) Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong) 19:30–34
Huang TJ, Hsu RW, Li YY, Cheng CC (2005) Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res 23:406–411. doi:10.1016/j.orthres.2004.08.010
Righesso O, Falavigna A, Avanzi O (2007) Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery 61(545–549):549. doi:10.1227/01.NEU.0000290901.00320.F5
Teli M, Lovi A, Brayda-Bruno M, Zagra A, Corriero A, Giudici F, Minoia L (2010) Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J 19:443–450. doi:10.1007/s00586-010-1290-4
Furlan AD, Pennick V, Bombardier C, van Tulder M (2009) 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 34:1929–1941
Lee SH, Chung SE, Ahn Y, Kim TH, Park JY, Shin SW (2006) Comparative radiologic evaluation of percutaneous endoscopic lumbar discectomy and open microdiscectomy: a matched cohort analysis. Mt Sinai J Med 73:795–801
Pan L, Zhang P, Yin Q (2014) Comparison of tissue damages caused by endoscopic lumbar discectomy and traditional lumbar discectomy: a randomised controlled trial. Int J Surg 12:534–537. doi:10.1016/j.ijsu.2014.02.015
Mayer HM, Brock M (1993) Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg 78:216–225. doi:10.3171/jns.1993.78.2.0216
Xiao SW, Jiang H, Yang LJ, Xiao ZM (2015) Comparison of unilateral versus bilateral pedicle screw fixation with cage fusion in degenerative lumbar diseases: a meta-analysis. Eur Spine J 24:764–774. doi:10.1007/s00586-014-3717-9
Schizas C, Tsiridis E, Saksena J (2005) Microendoscopic discectomy compared with standard microsurgical discectomy for treatment of uncontained or large contained disc herniations. Neurosurgery 57(357–360):357–360
Ahn Y, Lee HY, Lee S, Lee JH (2011) Dural tears in percutaneous endoscopic lumbar discectomy. Eur Spine J 20:58–64
Khazim R, Dannawi Z, Spacey K, Khazim M, Lennon S, Reda A, Zaidan A (2015) Incidence and treatment of delayed symptoms of CSF leak following lumbar spinal surgery. Eur Spine J. doi:10.1007/s00586-015-3830-4
Shriver MF, Xie JJ, Tye EY, Rosenbaum BP, Kshettry VR, Benzel EC, Mroz TE (2015) Lumbar microdiscectomy complication rates: a systematic review and meta-analysis. Neurosurg Focus 39:E6. doi:10.3171/2015.7.FOCUS15281
Perez-Cruet MJ, Foley KT, Isaacs RE, Rice-Wyllie L, Wellington R, Smith MM, Fessler RG (2002) Microendoscopic lumbar discectomy: technical note. Neurosurgery 51:S2–S129
Bosacco SJ, Gardner MJ, Guille JT (2001) Evaluation and treatment of dural tears in lumbar spine surgery: a review. Clin Orthop Relat R 389:238–247
Tsutsumimoto T, Yui M, Uehara M, Ohta H, Kosaku H, Misawa H (2014) A prospective study of the incidence and outcomes of incidental dural tears in microendoscopic lumbar decompressive surgery. Bone Jt J 96-B:641–645. doi:10.1302/0301-620X.96B5.32957
Epstein NE (2013) A review article on the diagnosis and treatment of cerebrospinal fluid fistulas and dural tears occurring during spinal surgery. Surg Neurol Int 4:S301–S317. doi:10.4103/2152-7806.111427
Berjano P, Pejrona M, Damilano M (2013) Microdiscectomy for recurrent L5–S1 disc herniation. Eur Spine J 22:2915–2917
Parker SL, Mendenhall SK, Godil SS, Sivasubramanian P, Cahill K, Ziewacz J, McGirt MJ (2015) Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res 473:1988–1999. doi:10.1007/s11999-015-4193-1
Miwa S, Yokogawa A, Kobayashi T, Nishimura T, Igarashi K, Inatani H, Tsuchiya H (2013) Risk factors of recurrent lumbar disc herniation: a single center study and review of the literature. J Spinal Disord Tech. doi:10.1097/BSD.0b013e31828215b3
Aizawa T, Ozawa H, Kusakabe T, Nakamura T, Sekiguchi A, Takahashi A, Sasaji T, Tokunaga S, Chiba T, Morozumi N, Koizumi Y, Itoi E (2012) Reoperation for recurrent lumbar disc herniation: a study over a 20-year period in a Japanese population. J Orthop Sci 17:107–113. doi:10.1007/s00776-011-0184-6
Cheng J, Wang H, Zheng W, Li C, Wang J, Zhang Z, Huang B, Zhou Y (2013) Reoperation after lumbar disc surgery in two hundred and seven patients. Int Orthop 37:1511–1517
Matsumoto M, Watanabe K, Hosogane N, Tsuji T, Ishii K, Nakamura M, Chiba K, Toyama Y (2013) Recurrence of lumbar disc herniation after microendoscopic discectomy. J Neurol Surg Part A Cent Eur Neurosurg 74:222–227
Wu X, Zhuang S, Mao Z, Chen H (2006) Microendoscopic discectomy for lumbar disc herniation: surgical technique and outcome in 873 consecutive cases. Spine (Phila Pa 1976) 31:2689–2694. doi:10.1097/01.brs.0000244615.43199.07
Chou D, Wang VY, Khan AS (2009) Primary dural repair during minimally invasive microdiscectomy using standard operating room instruments. Neurosurgery 64(356–358):358–359. doi:10.1227/01.NEU.0000338942.11337.DA
van den Akker ME, Arts MP, van den Hout WB, Brand R, Koes BW, Peul WC (2011) Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk-related sciatica: cost utility analysis alongside a double-blind randomized controlled trial. Neurosurgery 69(829–835):835–836. doi:10.1227/NEU.0b013e31822578f6
Acknowledgments
This work was supported by the Science Foundation of Guangxi (201502). The Manuscript submitted does not contain information about medical device(s)/drug(s). No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
JL. He and SW. Xiao contributed equally to this work.
Rights and permissions
About this article
Cite this article
He, J., Xiao, S., Wu, Z. et al. Microendoscopic discectomy versus open discectomy for lumbar disc herniation: a meta-analysis. Eur Spine J 25, 1373–1381 (2016). https://doi.org/10.1007/s00586-016-4523-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4523-3