Abstract
Purpose
The purpose of this study was to systematically compare the effectiveness and safety of endoscopic discectomy (ED) with open discectomy (OD) for the treatment of symptomatic lumbar disc herniation (LDH).
Methods
A highly sensitive search strategy was used to identify all published randomized controlled trials up to August 2014. A criteria list taken from Koes et al. was used to evaluate the risk of bias of the included studies. The five questions that were recommended by the Cochrane Back Review Group were used to evaluate the clinical relevance. Cochrane methodology was used for the results of this meta-analysis.
Results
Nine relevant RCTs involving 1,092 patients were identified. Compared with OD, ED results in slightly better clinical outcomes which were evaluated by the Macnab criteria without clinical significance (ED group: 95.76 %; OD group: 80 %; OR: 3.72, 95 % CI: [0.76, 18.14], P = 0.10), a significantly greater patient satisfaction rate (ED group: 93.21 %; OD group: 86.57 %; OR: 2.19; 95 % CI: [1.09, 4.40]; P = 0.03), lower intraoperative blood loss volume (WMD: −123.71, 95 % CI: [−173.47, −73.95], P < 0.00001), and shorter length of hospital stay (WMD: −Table 2144.45, 95 % CI: [−239.54, −49.37], P = 0.003).
Conclusions
From the existing outcomes, ED surgery could be viewed as a sufficient and safe supplementation and alternative to standard open discectomy. The cost-effectiveness analyses still remain unproved from the existing data. More independent high-quality RCTs using sufficiently large sample sizes with cost-effectiveness analyses are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sciatica, which is caused by nerve root compression or irritation, describes the symptoms of leg pain and occasionally neurological disturbance in the dermatome of the affected nerve root. Over 90 % of cases are due to symptomatic lumbar disk herniation (LDH) [1, 2]. Symptomatic LDH, with a reported prevalence of 1–3 % [3], is the commonest pathological process leading to spinal surgery.
Surgery for symptomatic LDH can be classified into two broad categories: open versus endoscopic surgery. In 1934, Mixter and Barr were the first authors to treat symptomatic LDH surgically by performing an open laminectomy and discectomy [2]. In 2007, a Cochrane review on surgical interventions for LDH concluded that there was considerable evidence that open discectomy (OD) was effective in reducing symptoms in the short term [4]. But, in the last decades, endoscopic discectomy (ED) techniques which were developed to perform discectomy under direct view and local anesthesia have gained a growing interest. The perceived benefits are minimal muscle and soft tissue damage with excellent visualization. Yeung developed the commercially available Yeung Endoscopic Spine System (YESS) in 1997 [5], and Hoogland developed the Thomas Hoogland Endoscopic Spine System (THESSYS) in 1994. With the latter system, it is possible to enlarge the intervertebral foramen near the facet joint with special reamers to reach intracanal extruded and sequestered disk fragments and decompress foraminal stenosis [6]. Microendoscopic discectomy (MED) was first described in 1997 as a minimally invasive transmuscular approach using advanced optics [7]. Currently, OD (e.g., conventional open discectomy and open microdiscectomy) and ED (e.g., transforaminal endoscopic discectomy and MED) are the most widespread procedure among the majority of spine surgeons for surgical decompression of radiculopathy caused by symptomatic LDH.
However, previous studies that compared the clinical effects of ED with OD for treating symptomatic LDH are constituted of ambiguous results. Therefore, it is still uncertain whether ED is more effective and safer than OD. The objective of this study was to systematically compare the effectiveness and safety of ED with OD for the treatment of symptomatic LDH.
Materials and methods
Criteria for selected trials
All randomized controlled clinical trials (RCTs) comparing ED with OD for the treatment of symptomatic LDH were identified in this study. We systematically reviewed published studies according to the following criteria: (1) patients younger than 70 years of age underwent spinal ED or OD for symptomatic LDH were included in the study; (2) the interventions in this study included various types of ED and OD in the lumbar spine; (3) the study reported at least one desirable outcome; (4) all included trials were followed up at least 1 year after surgery; and (5) patients were excluded if they had an acute spinal fracture, infection, tumor, or rheumatoid arthritis. The outcomes obtained in this study were labeled as the primary outcome and the secondary outcome. The primary outcome includes: (1) the clinical outcomes evaluated by the Macnab criteria, (2) patient satisfaction with the treatment, and (3) complications. The secondary outcome includes: (1) length of hospital stay, (2) operation time and blood loss volume, (3) recurrences rate, and (4) reoperation rate.
Search methods for identification of studies
RCTs without language restrictions were identified up to August 2014 by PubMed and China National Knowledge Infrastructure (CNKI); computer searching of Ovid MEDLINE and EMBASE; the Cochrane Central Register of Controlled Trials; hand searching of European Spine Journal, Spine, The Spine Journal and Journal of Bone and Joint Surgery of abstracts from 1990; and communication with international experts. The following key words were used for search: lumbar disk herniation (protrusion or prolapse), endoscopic, discectomy, open discectomy, and randomized controlled trial. Two investigators independently reviewed all subjects, abstracts, and the full text of articles that were potentially eligible based on abstract review. Then the eligible trials were selected according to the inclusion criteria. Disagreement was resolved by discussion, if necessary, by further discussion with an independent colleague.
Data collection
The data were extracted from included reports independently by two reviewers, and further discussions would be needed to deal with the disagreements. The data extracted include the following categories: the participant characteristics, the number of participants, and the loss to follow-up; study characteristics; the intervention details; the primary and the secondary outcomes; odds ratios (OR) or mean difference (MD); and 95 % confidence limits (95 % CI) of the comparisons.
Assessment of risk of bias
Two reviewers independently assessed the risk of bias of the trials. In a subsequent meeting, the reviewers tried to reach consensus on each criterion that they initially disagreed on. A criteria list taken from Koes et al. [8] was used to evaluate it. To each criterion, a weight was attached. The maximum score was 100 points for each study. The assessments which resulted in higher scores indicate studies of lower risk of bias. The included study which scored more than 50 points was considered as best study according to the criteria [8].
Assessment of clinical relevance
Two reviewers independently assessed the clinical relevance of the included studies referring to the five questions recommended by the Cochrane Back Review Group [9, 10]. Positive (+) would be recorded for the question if the clinical relevance item is met, negative (−) for the irrelevance, and unclear (?) if the data are inadequate for answering the question.
Measures of treatment effect
Attempts were made to statistically pool the data of included studies in order to obtain the primary and the secondary outcomes. The results were expressed in terms of odds ratio (OR) and a 95 % confidence interval (95 % CI) for dichotomous outcomes, and in terms of mean difference (MD) and 95 % CI for continuous outcomes. When the same continuous outcomes are measured in different scales, standardized mean difference (SMD) and 95 % CI are calculated. If outcomes were shown as dichotomous data in some studies while in the other studies expressed as continuous data, odds ratios would be re-pressed as standardized mean difference to allow dichotomous and continuous data to be pooled together [11]. Collected data were checked and entered into the computer by the two reviewers. RevMan software (vesion5.0) was used for data analysis. We performed the Laird Q test for heterogeneity and also calculated the I 2 statistic for each analysis [12]. If the P value was 0.05 or less, indicating obvious heterogeneity between studies, a random-effects model was used to calculate the pooled OR [13], otherwise, a fixed-effects model was performed [14]. A rating system with five levels of evidence taken from the Cochrane Back Review Group was used to evaluate the level of evidence [9].
Results
Description of studies
The process of identifying eligible studies is shown in Fig. 1. After titles and abstracts evaluation, 143 references were omitted according to conditions listed in Fig. 1. The remaining 15 candidate studies were taken for a comprehensive evaluation. We excluded 6 more studies after evaluating the full article versions of the remaining articles due to unsuitable controls, data replication. Finally, nine studies with a total of 1,092 patients with symptomatic LDH entered this meta-analysis [15–23].
The characteristics of nine included studies are summarized in Table 1. In all included studies, the patients with symptomatic LDH were recruited with sample size ranging from 40 to 240 patients. All the included studies have definite inclusion/exclusion criteria. Frank et al. [17] performed the video-assisted arthroscopic microdiscectomy compared with OD. In four studies [15, 16, 18, 19], the transforaminal endoscopic discectomy (TED) was employed compared with OD (open microsurgical discectomy or standard open discectomy). In addition, in the other four studies [20–23], the MED was employed compared with OD. The clinical outcomes, surgical data, and complications were analyzed in at least 1-year follow-up period.
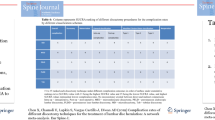
Risk of bias in included studies
Risk of bias assessment of included studies is presented in Table 2. The 2 reviewers disagreed on 8 of 72 items (11.1 %) scored. After discussing the results, they reached consensus on the scoring of all items. There were 5 best studies which scored more than 60 points, and the other 4 studies which scored more than 50 points. The median score was 62.8 points, indicating the overall lower risk of bias of the trials. The most prevalent methodologic shortcomings appeared to be (F) the small size of the study populations included, and (M) a lack of clarity regarding the outcome assessor blinded to the intervention. In four studies, there was a clear attempt at concealment of group allocation and method of randomization [15–17, 20]. There were five trials performed an intention-to-treat analysis [17–19, 21, 22]. All of the nine trials had the recommended follow-up for surgical studies of at least 1 year and had a follow-up rate of more than 87 % of each included trials.
Clinical relevance
Clinical relevance of the included studies is presented in Table 3. There was disagreement between the 2 reviewers with regard to the scoring of 2 of 20 (10 %) clinical relevance items. Consensus was reached on all scorings after discussion. All of the included trials described the interventions and treatment settings well enough to enable clinicians to replicate the treatment in clinical practice. In one study trial, the relevant outcomes, such as complications, were not reported [18], and in another study trial [19], the size of the effect was not considered to be clinically important. The consistent outcomes of all included studies suggested that the treatment benefits were likely worth the potential harms.
Meta-analysis results
At the end of follow-up point, patient satisfaction status was significantly better in ED group than OD group (OR: 2.19; 95 % CI: [1.09, 4.40]; P = 0.03, I 2 = 0 %). The patient satisfaction rates of ED group and OD group were 93.21 and 86.57 %, respectively.
Although the complication rate of OD group was slightly higher than ED group (OD: 20.12 %, ED: 16.11 %), no significant difference was found in the complication rate (OR: 0.73, 95 % CI: [0.34, 1.57], P = 0.41, I 2 = 75 %), which reflects the primary harm outcome. The primary beneficial clinical outcomes which were evaluated by the Macnab criteria of ED group were slightly higher than OD group (ED group: 95.76 %; OD group: 80 %), but no statistical significance was found between ED group and OD group in clinical outcomes evaluated by the Macnab criteria (OR: 3.72, 95 % CI: [0.76, 18.14], P = 0.10, I 2 = 62 %).
In the secondary outcomes, significant differences were found between ED group and OD group in the length of hospital stay (WMD: −144.45, 95 % CI: [−239.54, −49.37], P = 0.003, I 2 = 99 %) and the blood loss volume (WMD: −123.71, 95 % CI: [−173.47, −73.95], P < 0.00001, I 2 = 99 %). The length of hospital stay of OD group was significantly longer than ED group, and the blood loss volume of the OD group was significantly higher than ED group. No significant difference was found in the operating time (WMD: 9.27, 95 % CI: [−6.69, 25.23], P = 0.25, I 2 = 95 %), recurrences rate (OR: 1.62; 95 % CI: [0.84, 3.12]; P = 0.15, I 2 = 0 %), and the reoperation rate (OR: 0.98; 95 % CI: [0.60, 1.61]; P = 0.93, I 2 = 0 %). The recurrence rates of ED group and OD group were 5.04 and 3.35 %, respectively. The reoperation rates of ED group and OD group were 6.82 and 6.93 %, respectively. The results of meta-analysis are shown in Fig. 2.
Pooled results of endoscopic discectomy (ED) versus open discectomy (OD). The results of ED versus instrumented OD were shown as follows: the clinical outcomes evaluated by the Macnab criteria, patient satisfaction, complication rate, length of hospital stay, operation time, the blood loss volume, recurrences rate, and reoperation rate
Other results
Mohamed et al. [20] reported that the total success rate of MED group was 96.8 % (1-year postoperative) which remained unchanged till the end of the follow-up period and 71.1 % (1-year postoperative) for OD group which decreased to 55.6 % by 8 years. 98 % of MED group showed complete satisfaction with MED procedure and outcome and would undergo the surgery again for the same condition compared to 40 % of the control group. Teli et al. [23] found that MED was significantly more expensive than OD both as a single and as a repeat procedure when the cost of recurrences was taken into account (MED: 3,010 ± 450 Euros per case, OD: 2,310 ± 260–2,450 ± 340 Euros per case). Huang et al. [24] suggested that surgical trauma, as reflected by systemic IL-6 and CRP response, was significantly less following MED than following OD, and the difference in the systemic cytokine response may support that the MED procedure is less traumatic. Lee et al. [18] noted that the successful clinical outcomes were 96.7 % in ED group and 93.3 % in the OD group. Among the various radiological parameters, changes of disk height (1.41 ± 1.19 mm in ED group and 2.29 ± 2.12 mm in OD group, P = 0.024) and foraminal height (1.26 ± 0.91 mm in ED group and 1.85 ± 0.92 mm in OD group, P = 0.017) were significantly different between the two groups, and they concluded that although the clinical outcomes were similarly satisfactory in both groups, ED is a less invasive procedure than OD in selected cases. Garg et al. [21] found that both methods were equally effective in relieving radicular pain by reducing the tension on the nerve root caused by the herniated disc.
Discussion
This meta-analysis identified nine RCTs that compared ED with OD for symptomatic LDH. It revealed that ED group resulted in a higher patient satisfaction rate with clinical statistical significance when compared with OD group at the end of follow-up point. There is strong evidence that blood loss volume which reflects harm outcomes of OD group was significantly higher than ED group. Further more, the length of hospital stay of OD group was significantly longer than ED group. The cost of discectomy for LDH has rarely been the object of research, despite its need [25]. The topic of cost has been addressed in only one RCT [23], which found that MED was significantly more expensive than OD. But in several countries, the length of hospitalization is also influenced by reimbursement issues. It is supposed that shorter length of hospital stay may lead to lower cost of treatment. To assess the topic of cost, more high-quality RCTs with cost-effectiveness analyses are needed. Additionally, the primary beneficial clinical outcomes which were evaluated by the Macnab criteria of ED group were slightly higher than OD group, but no significant difference was found between them. Mohamed’s study [20], which underwent 8 years follow-up, reported that 98 % of MED group showed complete satisfaction with MED procedure and outcome, and would undergo the surgery again for the same condition compared to 40 % of the control group. The follow-up duration of the other eight studies was ranged from 1 to 3 years. Mohamed’s study was found to be highly influential to the overall results. Therefore, when analyzing patient satisfaction status, we excluded this study as making a sensitivity analysis. After omitting Mohamed’s study [20], there was no statistical statistical heterogeneity found in this meta-analysis combined result about the patient satisfaction rate, and the combined results were similar with the eligible studies. Qualitative analysis reveals that ED technique can significantly relieve the patients’ symptom.
The goal of surgical treatment of symptomatic LDH was sufficient decompression with minimization of operation-induced traumatization and its consecutive sequelae. OD has become a “gold” standard procedure in treating symptomatic LDH since Mixter and Barr’s first report it in 1934 [2]. However, optimal surgical management of symptomatic LDH remains controversial. OD has been criticized because it can cause muscle scarring, epidural fibrosis, and spinal instability. The demands of modern society create the need for faster recoveries, allowing patients to resume their normal activities sooner. Technical developments in the past decades have made the treatment of LDH safer and less invasive. Using endoscopic approaches through small incisions, nerve root decompression is achieved with minimal risk of complication and preserving normal anatomy [26]. The concept of MED was developed by Smith and Foley in 1997. This procedure allows the disk to be addressed directly through the spinal canal. This system aims to limit intraoperative soft tissue trauma while providing good illumination and visualization [27]. The possible advantages of TED are described in many articles. The procedure can be performed in an outpatient or day-surgery setting. Because of the small incision and minimal internal tissue damage, the rehabilitation period is supposed to be shorter and scar tissue fewer. The procedure can be performed in wakeful patients under local anesthesia and conscious sedation, thereby avoiding the risk of general anesthesia especially for elderly and infirm individuals [28, 29]. Another benefit of local anesthesia is the ability of surgeons to continually communicate with the patient, thus avoiding the risk of nerve damage during insertion of the working sheath [30, 31]. Despite these advantages, potential disadvantages are also reported. The potential problems of MED include a longer operating time that reflects the learning curve inherited to this video-endoscopic technique and the complex hand-eye coordination necessary for the procedure. Problems with intraoperative bleeding control, difficulty in repairing the dura tears, and fencing of instruments owing to limited working space are its disadvantages. TED also has a steep learning curve that requires patience and experience, especially for those unfamiliar with percutaneous techniques. Over all, ED technology is less traumatizing to the soft tissue, results in less blood loss, shorter hospital stay, and greater overall patient satisfaction. The current study seems to suggest that after endoscopic surgery 93.21 % of the patients experience a satisfactory outcome.
In this study, no significant difference was found in operating time. The results regarding operative times are difficult to interpret. There is considerable heterogeneity among operative times in the included studies. This may be explained by the learning curve associated with ED surgery [30], variability in the techniques used, and differences in how operative time was defined, for example, whether or not total time under anesthesia was measured. This study found no significant differences in reoperation percentages between ED group and OD group (6.82 vs. 6.93 %,). Reoperation rate of the two groups is similar with reported for OD (4.0–9.7 %) [32] and ED (4.2–11.0 %) [5, 33]. As in most surgical interventions, adequate patient selection and accurate diagnosis seem very important. Most common cause for reoperations was persistent complaints due to missed lateral bony stenosis and remnant fragments [34]. Although it was reported that, at the beginning of the learning curve, the poor perception of depth with endoscopic surgery is possibly linked to a higher incidence of iatrogenic dural and root injuries compared to OD [22], while the restricted field of work by the tubular retractor might justify a lower chance of identifying and removing free fragments within the disk space, ultimately leading to a higher incidence of LDH recurrences. In our study, complications and recurrences did not differ significantly between the ED group and OD group. Most patients after lumbar discectomy are restricted in their activities for some time by discomfort and medical advice and advised to restrict weight-bearing activities or bending over for several weeks or months [35–37]. However, the optimal time of restrictions and the clinical benefit of such restrictions remain unknown [38].
The purpose of this study was to systematically compare the effectiveness and the safety of ED with OD for the treatment of symptomatic LDH. Gibson et al. [25] have prior reviewed surgical interventions for LDH in 2007, and subsequently Nellensteijn et al. [39] reviewed TED for symptomatic LDH in 2010. Due to the lack of enough relevant RCTs, the statistically pooling results of ED versus OD were not stated in both of their reviews. In our study, nine RCTs which compare ED with OD are included to evaluate a total of 1,092 patients with symptomatic LDH. When the data from nine high-quality included studies were pooled, we found that both treatments are efficacious for symptomatic LDH. The results suggest that the patients with ED had a greater patient satisfaction rate, lower intraoperative blood loss volume, and shorter length of hospital stay. In every included study, the patients were selected carefully by means of employing the similar inclusion and exclusion criteria. These criteria did in fact result in a patient sample which could contribute to good clinical results. The benefit of both interventions may not be repeated when performing them onto every symptomatic LDH patient. Meticulous patient selection is essential to obtain a good clinical result.
Meta-analysis is a statistical analysis of data collected from several different researches and surveys on the same problem, pooling outcomes in order to arrive at a more unbiased and scientific conclusion. Ideally, each of the studies included in meta-analysis should contain large numbers of cases and have a similar validated design. In this study, only nine published RCTs on ED versus OD were analyzed. The major strength of performing this meta-analysis is that it pools RCTs and all of the included trials have high methodological qualities (score >50), which implies a lower risk of bias. The most prevalent methodological shortcomings appeared to be the small size of populations and the insufficiency regarding the outcome assessor blinding to intervention. To avoid outcomes distorted by language bias, we considered all articles without language restrictions. This study has a number of limitations that should be considered when drawing conclusions regarding the effectiveness of ED versus OD for symptomatic LDH. The small number of included studies limited our ability to assess potential publication bias by the funnel plot, and unpublished researches with negative results cannot be identified. Therefore, publication bias may exist, which could result in the overestimation of the effectiveness of interventions. Moreover, the sample size of each included study is slightly small. Due to these limitations, the combined results of this meta-analysis should be cautiously accepted. In addition, the cost-effectiveness analyses still remain unproved from the existing data. More independent high-quality RCTs using sufficiently large sample sizes with cost-effectiveness analyses are needed.
Conclusion
Compared with OD, ED results in slightly better clinical outcomes evaluated by the Macnab criteria without clinical significance, a significantly greater patient satisfaction rate, lower intraoperative blood loss volume, and shorter length of hospital stay. From the existing outcomes, ED surgery could be viewed as a sufficient and safe supplementation and alternative to standard open discectomy. More independent high-quality RCTs using sufficiently large sample sizes with cost-effectiveness analyses are needed.
References
Valat JP, Genevay S, Marty M et al (2010) Sciatica. Best Pract Res Clin Rheumatol 24:241–252
Mixter W, Barr J (1934) Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med 211:205–210
Gibson JN, Cowie JG, Iprenburg M (2012) Transforaminal endoscopic spinal surgery: the future ‘gold standard’ for discectomy?—A review. Surgeon 10:290–296
Gibson JN, Waddell G (2007) Surgical interventions for lumbar disc prolapse. Cochrane Database Syst Rev 2:CD001350
Yeung AT, Tsou PM (2002) Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine 27:722–731
Hoogland T, Schubert M, Miklitz B et al (2006) Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine 31:E890–E897
Foley KT, Smith MM, Rampersaud YR (1999) Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg Focus 7:e5
Koes BW, Scholten RJ, Mens JM et al (1995) Efficacy of epidural steroid injections for low-back pain and sciatica: a systematic review of randomized clinical trials. Pain 63:279–288
Van Tulder M, Furlan A, Bombardier C et al (2003) Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine 28:1290–1299
Furlan AD, Pennick V, Bombardier C et al (2009) 2009 updated method guidelines for systematic reviews in the cochrane back review group. Spine 34:1929–1941
Higgins JP, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated September 2011]. The cochrane collaboration. Available from URL: http://handbook.cochrane.org/
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22:719–748
Ruetten S, Komp M, Merk H et al (2008) Full-endoscopic interlaminar and transforaminal lumbar discectomy ver versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine 33:931–939
Ruetten S, Komp M, Merk H et al (2009) Recurrent lumbar disc herniation after conventional discectomy: a prospective, randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision. J Spinal Disord Tech 22:122–129
Hermantin FU, Peters T, Quartararo L et al (1999) A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am 81:958–965
Lee SH, Chung SE, Ahn Y et al (2006) Comparative radiologic evaluation of percutaneous endoscopic lumbar discectomy and open microdiscectomy: a matched cohort analysis. Mt Sinai J Med 73:795–801
Jun-liang LIU, Wan-xin ZHEN, Guo-yong GAO et al (2014) A prospective and controlled study of percutaneous transforaminal endoscopic discectomy versus fenestration discectomy for lumbar disc herniation. Chin J Bone Joint 3:245–250
Hussein M, Abdeldayem A, Mattar MMM (2014) Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: a prospective, randomized, controlled study with 8 years of follow-up. Eur Spine J 23:1992–1999
Garg B, Nagraja UB, Jayaswal A (2011) Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong) 19:30–34
Righesso O, Falavigna A, Avanzi O (2007) Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery 61:545–549
Teli M, Lovi A, Brayda-Bruno M et al (2010) Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J 19:443–450
Huang TJ, Hsu RW, Li YY et al (2005) Less systemic cytokine response in patients following micro endoscopic versus open lumbar discectomy. J Orthop Res 23:406–411
Gibson JN, Waddell G et al (2007) Surgical interventions for lumbar disc prolapse: updated cochrane review. Spine 32:1735–1747
Williams RW (1993) Lumbar disc disease microdiscectomy. Neurosurg Clin N Am 4:101–108
Perez-Cruet MJ, Foley KT, Isaacs RE et al (2002) Microendoscopic lumbar discectomy: technique note. Neurosurgery 51:129–136
Knight MT, Ellison DR, Goswami A et al (2001) Review of safety in endoscopic laser foraminoplasty for the management of back pain. J Clin Laser Med Surg 19:147–157
Knight MT, Goswami A, Patko JT et al (2001) Endoscopic foraminoplasty: a prospective study on 250 consecutive patients with independent evaluation. J Clin Laser Med Surg 19:73–81
Lee DY, Lee SH (2008) Learning curve for percutaneous endoscopic lumbar discectomy. Neuro Med Chir (Tokyo) 48:383–389
Choi G, Lee SH, Raiturker PP (2006) Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery 58:ONS59–ONS68
Goald HJ (1980) Microlumbar discectomy: follow-up of 477 patients. J Microsurg 2:95–100
Schaffer JL, Kambin P (1991) Percutaneous posterolateral lumbar discectomy and decompression with a 6.9-millimeter cannula. Analysis of operative failures and complications. J Bone Joint Surg Am 73:822–831
Kambin P (1992) Arthroscopic microdiscectomy. Arthroscopy 8:287–295
Barrios C, Ahmed M, Arrotegui JI et al (1990) Clinical factors predicting outcome after surgery for herniated lumbar disc: an epidemiological multivariate analysis. J Spinal Disord 3:205–209
Junge A, Dvorak J, Ahrens S (1995) Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine 20:460–468
Kahanovitz N, Viola K, Muculloch J (1989) Limited surgical discectomy and microdiscectomy. A clinical comparison. Spine 14:79–81
Carragee EJ, Han MY, Yang B et al (1999) Activity restrictions after posterior lumbar discectomy. A prospective study of outcomes in 152 cases with no postoperative restrictions. Spine 24:2346–2351
Nellensteijn J, Ostelo R, Bartels R et al (2010) Transforaminal endoscopic surgery for symptomatic lumbar disc herniations: a systematic review of the literature. Eur Spine J 19:181–204
Acknowledgments
This study was funded by National Natural Science Foundation of China (No: 81201419). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cong, L., Zhu, Y. & Tu, G. A meta-analysis of endoscopic discectomy versus open discectomy for symptomatic lumbar disk herniation. Eur Spine J 25, 134–143 (2016). https://doi.org/10.1007/s00586-015-3776-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-3776-6