Abstract
Purpose
To investigate whether the presence of Modic changes type I (MC I) found on preoperative MRI scans represent a risk factor for persistent back pain 12 months after surgery amongst patients operated for lumbar disc herniation.
Methods
Cohort study of 178 consecutive patients operated with lumbar microdiscectomy. Preoperative MRI scans were evaluated by two independent neuroradiologists. Primary outcome measure was the visual analogue scale (VAS) for back pain. Secondary outcome measures were; VAS for leg pain, physical function (Oswestry Disability Index), and health-related quality of life (EQ-5D), self-reported benefit of the operation and employment status. The presence of MC I was used as exposition variable and adjusted for other risk factors in multivariate analyses.
Results
The Modic classification showed a high inter-observer reproducibility. Patients with MC I had less improvement of back pain 12 months after surgery, compared to those who had no or other types of MC, but this negative association no longer showed statistical significance when adjusted for smoking, which remained the only independent risk factor for persistent back pain.
Conclusions
Patients with preoperative MC I can expect less but still significant improvement of back pain 1 year after microdiscectomy, but not if they smoke cigarettes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 1988, Modic et al. [1] characterised T1 and T2 weighted signal changes in the vertebral endplates on magnetic resonance images (MRI) most frequently referred to as Modic changes (MC) type I, II and III. MC, regardless of type, have been shown to coincide with with degenerative changes of intervertebral disc and chronic low back pain (CLBP) [2–5]. MC I refers to an edema-like signal intensity (hypointense T1 and hyperintense T2 signal), MC II refers to fat-like signal intensity (hyperintense T1 and isointense or slightly hyperintense T2), and MC III refers to a sclerosis-like signal intensity (hypointense T1 and T2. MC II and III changes are thought to represent the end stage of the degenerative process [1]. In the general population, MC I seem to have the strongest association, both to an active inflammatory process and CLBP [3–7].
Lumbar disc degeneration and herniation is regarded as a risk factor for developing MC, especially MC I [7–9]. Patients with lumbar disc herniation often have a combination of low back pain and radicular pain. They are more likely to improve from the radicular pain than the back pain after surgery, and it is difficult to predict which patients are at risk for developing CLBP after the operation. Some patients with CLBP and MC I changes are operated with total disc replacement [10, 11]. It has also been suggested that MC I is associated with hypermobility which could indicate the need for additional fusion surgery amongst these patients [12]. Previous studies with small smaples evaluating a possible association between MC and reduced recovery of back pain after lumbar microdiscectomy present conflicting results [11, 12].
The aim of this study was to investigate whether the presence of MC I on preoperative MRI scans represents a risk factor for less improvement of back pain 1 year after lumbar microdiscectomy. Such information could be used in the decision-making process prior to surgery.
Materials and methods
Patient population
This is a prospective study of 178 consecutive patients operated with unilateral microdiscectomy for a one level lumbar disc herniation. Follow up time was 1 year.
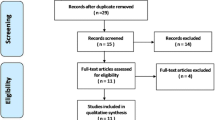
Patients who did not have preoperative MRI scans, had been operated in the lumbar region previously or were reoperated during the follow-up, were excluded (Fig. 1).
The cohort was recruited from a clinical registry, intended for quality control and research, at the Department of Neurosurgery, University Hospital of North-Norway (UNN), between 1 January 2000 and 31 December 2003. The registry comprised all patients operated for degenerative disease in the lumbar spine during the period [13, 14].
Informed consent was obtained from all participants and The Data Inspectorate of Norway approved the registration and management of data.
Surgery
All patients were operated with microscopic technique, using Caspar self retaining retractors and with preoperative or peroperative fluoroscopy for level ascertainment.
Radiological assessments
After the follow-up period, two independent neuroradiologists (both working at another university hospital) evaluated the preoperative MRI scans using the “Nordic Modic Classification” for investigating vertebral endplate signals [7, 15]. The radiologists were blinded regarding patient history, clinical outcome and each other’s evaluations. In case of disagreement between the radiologists, the interpretation of the most experienced radiologist was used.
For each patient the MRI findings at all visible levels were characterised into four groups; no MC, MC type I, II and mixed type I/II.
MC I has been shown to have the strongest correlation to CLBP [6], we therefore split the patient population into two groups: patients with type I and/or mixed I/II changes at any level (“MC I group”) and patients without any MC I (“no MC I group”), i.e. the rest of the study population. We also made subgroup analyses between patients with or without any type of MC (type I or type II).
Data collection
The self-administered questionnaires, completed at admission for surgery (baseline) and follow up, were identical and used for outcome assessments. The baseline questionnaire contained additional questions about demographics and lifestyle issues. During the hospital stay, the surgeon recorded data concerning diagnosis and treatment. All patients were summoned for follow up visits at 12 months at an outpatient clinic. Questionnaires were distributed by mail and completed at home by the patients. An independent observer, a research nurse, responsible for all follow up visits, collected and checked all questionnaires and interviewed the patients about employment status and complications.
Outcomes
Primary outcome measure was the visual analogue scale (VAS) for back pain. Secondary outcome measures were: VAS for leg pain, Oswestry Disability Index (ODI), the EuroQol-5D (EQ-5D), self-reported benefit of the operation and employment status.
Back pain and leg pain
Leg and back pain intensity were graded by the patient in two separate 100 mm VAS. (0 = no pain).
ODI
The ODI is a functional score, based on the Oswestry Low Back Disability Questionnaire which contains ten questions on limitations of activities of daily living [16]. Each item is rated on a 0–5 point scale and transferred into a percentage score, the ODI (ref). The range of possible values is from 0 to 100 (0 = no disability).
EQ-5D
EQ-5D is a generic and preference-weighted measure of health-related quality of life (HRQL). It evaluates five dimensions: mobility, self-care, activities of daily life, pain and anxiety and/or depression. For each dimension, the patient describes three possible levels of problems (no, mild to moderate and severe). Hence, this descriptive system contains 243 (35) combinations or index values for health states [17]. We used the value set based on the main survey from the EuroQol group [18], which has been validated for this patient population [13]. Total score range is from −0.594 to 1, where 1 corresponds to perfect health, and 0 to death.
Perceived benefit of the operation
At follow up the patients were asked: “How much benefit have you had from the operation?”. The response alternatives were: “Very much”, “Much”, “Some”, “None at all” or “Uncertain”. We dichotomized the patients according to their responses into those who had a substantial benefit of the operation (“Very much” and “Much”), and those who had not (the rest) [13].
ASA grade (the American Society of Anaesthetists grading system (I–V))
ASA grade was registered for each patient by a doctor or a specialised nurse before surgery. ASA grade classifies patients according to their vulnerability, i.e. physical condition (from no to life-threatening systemic disease) [19].
Statistical analyses
We tested if within group changes in outcome from baseline to follow up were statistically significant (p < 0.05) using paired t test. Differences between groups were assessed by independent samples t test, Mann–Whitney U tests or Chi square tests depending on the distribution of the data. Central tendency is presented as mean and standard deviation (SD) when normally distributed, and as median and interquartile range (IQR) when skewed (Kolmogorov–Smirnov’s test).
Predictors for improvement in back pain were assessed using the change in VAS from baseline to 12 months of follow up as dependent variable and MC I (yes/no) as exposition variable. We adjusted for covariates obtained from baseline data (Table 1) if the covariates were judged to be clinically relevant and if baseline values differed significantly (level 0.1) between the two subgroups of the exposition variable, using a linear regression model.
We tested inter-rater reliability for the evaluation of MC by computing Kappa values (Jacob Cohen, 1960).
The Statistical Package for the Social Sciences (SPSS for Windows, version 16.0, Chicago IL) was used in all analyses.
Results
Characteristics of the study population at baseline are shown in Table 1.
Amongst patients with MC I there were more smokers and fewer patients with high body mass index (BMI) compared to patients without MC I. No other statistically significant differences between the groups were found at baseline. There was no difference in back pain (median, IQR) between smokers (48, 41) and non-smokers (53, 44), p = 0.47. At baseline patients with any type of MC (type I or type II) had a mean (SD) age of was 44.0 (10.6) years compared to 37.3 (13.0) amongst patients without any MC, p < 0.001. For the other baseline characteristics, including smoking, there were no significant differences (data not shown).
Patients who were investigated by CT had the same amount of back pain at baseline (mean = 52.1, SD = 30.6) compared to the patients investigated with MRI (mean = 49.3, SD = 26.5), who were included in the study, p = 0.60.
Radiological assessments
The Kappa values of the inter-rater reliability of Modic change evaluations were 0.81 in both the levels of L5/S1 and L4/L5 and 0.66 in L3/L4.
104 patients (58 %) had some sort of MC and 36 (20 %) had MC I or mixed I/II MC at any level. Table 2 shows the distribution of MC seen on the preoperative high field MRIs. No MC type III were found.
Outcome assessment
Both patients with and without MC I improved in all outcome measures at 12 months of follow up. Patients with MC I had less improvement of back pain, Eq-5D and ODI score, but for the ODI statistical significance was not reached (Table 3). The improvement in leg pain was equal in both groups. Five patients (2.8 %) had complications to the surgery (Table 1). The complications (n) were: superficial wound infection (1), discitis (1) and dural tear (3) (all of which were repaired preoperatively).
A subgroup analysis of smokers and non-smokers with MC I showed that the non-smokers had an improvement of back pain (SD), of 26.9 (25.8), whereas smokers had an improvement of only 8.1 (28.6), p = 0.009 (Fig. 2). Smokers with MC I did not have a statistically significant improvement of back pain.
On including the whole cohort, 115 (81.0 %) of the patients without MC I stated that they had a substantial benefit (“much” or “very much”) from the operation, compared to 24 (66.7 %) of the patients with MC I (P = 0.06). Of the non-smokers, 83 (83.8 %) reported a substantial benefit, compared to 55 (70.5 %) of the smokers (p = 0.034). Of the whole cohort, 126 (74.1 %) out of 170 patients (missing data = 8) had returned to work, and 12 (34.3 %) of patients with MC I and 32 (23.7 %) without MC I still received sickness benefit (p = 0.20). Of the smokers 25 (33.3 %) received sickness benefit, compared to 19 (20.2 %) of non-smokers (p = 0.05).
We found no difference in outcomes between patients with any type of MC and the rest of the patient population (data not shown).
Risk factors
The results of uni- and multi-variate analyses are shown in Table 4. Smoking was the only independent risk factor for less improvement of back pain. As illustrated in Fig. 2 there seems to be an interaction between smoking and MC I, probably best explained by an additive effect of these two risk factors.
Discussion
Our principle finding is that patients with MC I who are operated for lumbar disc herniation have less improvement of back pain 12 months after surgery, compared to those who have no or other types of MC. However, in the multivariate analyses, this negative association no longer showed statistical significance when adjusted for smoking, which remained the only independent risk factor. The radicular pain improved significantly in all patients, regardless of the presence of preoperative MC I or smoking habits. Our study confirms the results of previous studies, that the Nordic Modic Consensus Group classification has a high inter-observer reproducibility [15].
Two recent studies have evaluated the influence of Modic changes on improvement of LBP after lumbar microdiscectomy; Chin et al. [11] found a trend toward greater improvement in patients without any MC. Ohtori et al. [12] recently compared outcomes after microdiscectomy amongst patients with or without MC I, but found no statistically significant difference. These studies were probably underpowered and smoking habits were not evaluated. Another cohort study found no association between MC I and recovery of non-specific back pain after non-surgical treatment, but again smoking habits were not reported [20].
This study indicates that both smoking and MC I seem to have a negative impact on recovery of back pain after surgery. There seems to be an interaction between smoking and preoperative MC I, and they might affect recovery by different mechanisms. The study was not designed to evaluate the aetiology of MC. Our results should be interpreted with caution and regarded as hypothesis generating. The sample size might have been too small to recognise MC I as an independent risk factor for persisting back pain. Our findings should therefore be evaluated in a larger cohort.
Two studies of healthy Scandinavians reported an association between the prevalence of MC and smoking [5, 21], but in a later Danish study, smoking did not seem to predispose for developing MC [9] and the exact biological mechanism behind development of MC remains obscure. In our study neither MC I nor smoking was associated to back pain at baseline. This is not surprising, since the presence of disc herniation could overshadow the LBP due to MC I.
In contrast to other studies, we found no association between Body mass index (BMI) and MC [22]. Heavy physical workload has been linked to development of MC [21]. We had no exact data on work load, only on educational level which was evaluated in the multivariate analyses. Another weakness of our study is that 42 % of the patients operated were excluded because they only had preoperative CT scans and not MRI. Many of the patients were admitted from other hospitals in rural areas, where MRI was not readily available. We cannot rule out that this might have introduced a selection bias. However, our data concerning frequency and distribution of MC seems to be in accordance with the findings of previous studies [7], and we found no differences in back pain at baseline between patients investigated with CT and with MRI.
We have no MRI scans at follow up which could be valuable for evaluating the influence of smoking on radiological findings, e.g. transformation of MC I. This could also be addressed in further studies.
The presence of preoperative MC I did not influence the improvement of radicular pain, for which the patients primarily were operated, and most of the patients with MC I had a significant improvement of back pain. Patients with MC I would therefore be good candidates for microdiscectomy alone. When evaluating the need for additional surgery for these patients, it is important to acknowledge the interaction between smoking and MC I, and that smoking is a modifiable lifestyle factor. Several studies have shown a negative effect of smoking on outcomes after low back surgery including more complex procedures, and some studies indicate that smoking cessation may reduce CLBP and improve outcomes [23–29]. In general, patients operated with lumbar microdiscectomy could be advised to quit smoking, especially in cases of concomitant MC I changes, but the efficacy of a smoking prevention programme has yet to be evaluated.
Conclusions
Patients with preoperative MC I can expect less but still significant improvement of back pain 1 year after microdiscectomy, but not if they smoke cigarettes.
References
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR (1988) Degenerative disc disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 166:193–199
Jensen TS, Karppinen J, Sorensen JS, Niinimaki J, Leboeuf-Yde C (2008) Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J 17:1407–1422
Pinheiro-Franco JL (2008) Modic changes: “age, si quid agis”. Eur Spine J 17:1766–1768
Toyone T, Takahashi K, Kitahara H, Yamagata M, Murakami M, Moriya H (1994) Vertebral bone-marrow changes in degenerative lumbar disc disease. An MRI study of 74 patients with low back pain. J Bone Joint Surg Br 76:757–764
Kuisma M, Karppinen J, Haapea M, Niinimaki J, Ojala R, Heliovaara M, Korpelainen R, Kaikkonen K, Taimela S, Natri A, Tervonen O (2008) Are the determinants of vertebral endplate changes and severe disc degeneration in the lumbar spine the same? A magnetic resonance imaging study in middle-aged male workers. BMC Musculoskelet Disord 9:51
Kjaer P, Leboeuf-Yde C, Korsholm L, Sorensen JS, Bendix T (2005) Magnetic resonance imaging and low back pain in adults: a diagnostic imaging study of 40-year-old men and women. Spine 30:1173–1180
Albert HB, Kjaer P, Jensen TS, Sorensen JS, Bendix T, Manniche C (2008) Modic changes, possible causes and relation to low back pain. Med Hypotheses 70:361–368
Albert HB, Briggs AM, Kent P, Byrhagen A, Hansen C, Kjaergaard K (2011) The prevalence of MRI-defined spinal pathoanatomies and their association with Modic changes in individuals seeking care for low back pain. Eur Spine J 20:1355–1362
Jensen TS, Kjaer P, Korsholm L, Bendix T, Sorensen JS, Manniche C, Leboeuf-Yde C (2010) Predictors of new vertebral endplate signal (Modic) changes in the general population. Eur Spine J 19:129–135
Siepe CJ, Mayer HM, Wiechert K, Korge A (2006) Clinical results of total lumbar disc replacement with ProDisc II: three-year results for different indications. Spine 31:1923–1932
Chin KR, Tomlinson DT, Auerbach JD, Shatsky JB, Deirmengian CA (2008) Success of lumbar microdiscectomy in patients with Modic changes and low-back pain: a prospective pilot study. J Spinal Disord Tech 21:139–144
Ohtori S, Yamashita M, Yamauchi K, Inoue G, Koshi T, Suzuki M, Orita S, Eguchi Y, Ochiai N, Kishida S, Takaso M, Aoki Y, Ishikawa T, Arai G, Miyagi M, Kamoda H, Nakamura J, Takahashi K (2010) Low back pain after lumbar discectomy in patients showing endplate Modic type 1 change. Spine 35:E596–E600
Solberg TK, Olsen JA, Ingebrigtsen T, Hofoss D, Nygaard OP (2005) Health-related quality of life assessment by the EuroQol-5D can provide cost-utility data in the field of low-back surgery. Eur Spine J 14:1000–1007
Solberg TK, Sorlie A, Sjaavik K, Nygaard OP, Ingebrigtsen T (2011) Would loss to follow-up bias the outcome evaluation of patients operated for degenerative disorders of the lumbar spine? Acta Orthop 82:56–63
Jensen TS, Sorensen JS, Kjaer P (2007) Intra- and interobserver reproducibility of vertebral endplate signal (Modic) changes in the lumbar spine: the Nordic Modic Consensus Group classification. Acta Radiol 48:748–754
Fairbank JC, Couper J, Davies JB, O’Brien JP (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66:271–273
The EuroQol Group (1990) EuroQol–a new facility for the measurement of health-related quality of life. The EuroQol Group. Health Policy 16:199–208
Dolan P, Gudex C, Kind P, Williams A (1996) The time trade-off method: results from a general population study. Health Econ 5:141–154
Dripps R (1963) New classification of physical status. Anesthesiology 24:111
Keller A, Boyle E, Skog TA, Cassidy JD, Bautz-Holter E (2012) Are Modic changes prognostic for recovery in a cohort of patients with non-specific low back pain? Eur Spine J 21:418–424
Leboeuf-Yde C, Kjaer P, Bendix T, Manniche C (2008) Self-reported hard physical work combined with heavy smoking or overweight may result in so-called Modic changes. BMC Musculoskelet Disord 9:5
Karchevsky M, Schweitzer ME, Carrino JA, Zoga A, Montgomery D, Parker L (2005) Reactive endplate marrow changes: a systematic morphologic and epidemiologic evaluation. Skeletal Radiol 34:125–129
Sanden B, Forsth P, Michaelsson K (2011) Smokers show less improvement than nonsmokers two years after surgery for lumbar spinal stenosis: a study of 4555 patients from the Swedish spine register. Spine 36:1059–1064
Andersen T, Christensen FB, Laursen M, Hoy K, Hansen ES, Bunger C (2001) Smoking as a predictor of negative outcome in lumbar spinal fusion. Spine 26:2623–2628
Glassman SD, Anagnost SC, Parker A, Burke D, Johnson JR, Dimar JR (1976) The effect of cigarette smoking and smoking cessation on spinal fusion. Spine 25:2608–2615
Trief PM, Ploutz-Snyder R, Fredrickson BE (1976) Emotional health predicts pain and function after fusion: a prospective multicenter study. Spine 31:823–830
Cobo SJ, Sendino RM, Fabregate FM, Cimarra DI, Martinez UP, Deglane MR (2010) Predictors of outcome after decompressive lumbar surgery and instrumented posterolateral fusion. Eur Spine J 19:1841–1848
Wai EK, Rodriguez S, Dagenais S, Hall H (2008) Evidence-informed management of chronic low back pain with physical activity, smoking cessation, and weight loss. Spine J 8:195–202
Choma TJ, Schuster JM, Norvell DC, Dettori JR, Chutkan NB (2011) Fusion vs. non-operative management for chronic low back pain: do co-morbid diseases or general health factors affect Outcome? Spine 36(21 Suppl):87–95
Conflict of interest
None of the authors has any potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sørlie, A., Moholdt, V., Kvistad, K.A. et al. Modic type I changes and recovery of back pain after lumbar microdiscectomy. Eur Spine J 21, 2252–2258 (2012). https://doi.org/10.1007/s00586-012-2419-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2419-4