Abstract
Background
There is evidence for an association between Modic type 1 and pain in patients with low back pain (LBP), but little knowledge about its effect on clinical outcomes.
Purpose
(1) To assess the prevalence of Modic changes, (2) to determine if Modic changes influence the clinical course of LBP, and (3) to identify prognostic factors for recovery.
Study design/setting
Prospective clinical cohort study, with a 1-year follow-up. The treatment consisted of brief intervention and instruction in stretching.
Patient’s sample
Two hundred and sixty-nine patients with chronic low back pain.
Outcome measures
Socio-demographic variables, education, profession, self-reported measures, degenerative changes on MRI.
Methods
Linear growth model and Cox regression analysis.
Results
Five percent had a normal MRI, 14 and 50% had Modic 1 and Modic 2 changes. Modic changes were not significant covariates for the clinical course of pain, function or fear avoidance beliefs. Education was a strong prognostic factor for recovery.
Conclusions
Modic changes did not influence the clinical course of back pain and were not prognostic factors for recovery. Education was strongly associated with recovery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Low back pain (LBP) is defined as pain, muscle tension and/or stiffness localized below the costal margin and above the inferior gluteal folds, with or without leg pain radiating to the knee [1]. In most cases no specific pathological causes can be detected and these are designated as non-specific LBP [2].
Individuals with LBP often request an examination by magnetic resonance imaging (MRI) in order to determine a cause for their back pain. International guidelines discourage routine use of MRI in individuals with non-specific LBP, because of the high prevalence of degenerative changes in asymptomatic individuals [3]. These degenerative changes are only weakly associated with symptoms; but, there is strong evidence that a particular structural change, Modic type 1 (MT1), is associated with the prevalent LBP [4].
There are three different types of Modic changes. MT1 changes correspond to edema of the vertebral endplates and subchondral bone, which is caused by endplate cracks. This is accompanied by increased vascular density, increased number of nerve endings and increased levels of proinflammatory biochemical mediators [5], which might be of pathogenic importance for the development of pain [6]. Generally, Modic type 2 (MT2) and type 3 changes are thought to represent the end stage of the degenerative process, and are not assumed to cause symptoms [7].
For chronic LBP, there is strong evidence that function, depression, education and professional status are strong prognostic factors for recovery [8] and this raises the question if MT1 is a prognostic factor, when combined with these variables.
In this study, we present the outcomes in a clinical cohort of patients with chronic non-specific LBP, receiving a brief intervention and instruction in self-care techniques. The purpose was three-fold: (1) to investigate the prevalence of Modic changes, (2) to investigate if Modic changes influence the clinical course, and (3) to identify prognostics factors for recovery, including Modic changes, socio-demographic, socio-economic variables (SES) and self-reported measures at baseline.
Materials and methods
Design
A prospective observational study of a clinical cohort of patients referred by general practitioners to the Neck and Back Clinic, in the Department of Physical Medicine and Rehabilitation, Oslo University Hospital (OUS), Oslo, Norway.
Patients
Patients from Oslo with non-specific LBP from 20 to 60 years of age. Patients with previous back surgery, spinal stenosis, cauda equina syndrome, spondylolisthesis grades II–IV, disc herniation with symptomatic nerve root irritation, serious somatic or psychiatric disease, osteoporosis, currently pregnant or receiving other treatment were excluded. In addition, patients that did not speak, write or read Norwegian were also excluded.
Magnetic resonance imaging (MRI)
MRI was performed at the Department of Neuroradiology, OUS, or at two private radiological institutes in Oslo. All MRIs were less than 6-month old. MRIs were performed with a Siemens Avanto 1.5T Magnetom (Siemens AG, Erlangen, Germany) and a Signa EXCITE HD 1.5T, General Electric Medical Systems (Milwaukee, Wisconsin, USA). A spine matrix coil was used with the participants lying in supine position. The following sequences were used for the Siemens Avanto 1.5T Magnetom (Signa EXCITE HD 1.5T): (1) a localizer sequence of 5 images, (TR/TE/flip angle, 1,500, 101, and 90°) consisting of 13 coronal images, 4 sagittal images and 3 axial images. (2) Sagittal T1-weighted turbo spin echo, (TR/TE 590/11 ms (474/10 ms), 320 × 240 matrix, 280 mm field of view, 11 (15) slices of 4 mm thickness, one acquisition, scan time 1 min 13 s. (3) Sagittal 2-weighted turbo spin echo, (TR/effective TE 3500/89 (2300/86 ms), 320 × 240 matrix, FOV 280 mm, 11 (15) slices of 4 mm thickness, one acquisition, scan time 1 min 50 s). (4) Axial T2-weighted turbo spin echo, (TR/effective TE 5000/89 (3130/91 ms), 320 × 240 matrix, FOV 240 (200) mm, 18 slices of 4 mm thickness, one acquisition, scan time 2 min 7 s).
An experienced radiologist (TAS) evaluated the MRIs. The following MRI findings were recorded at the three lower levels in lumbar spine: disc degeneration, disc herniation/bulging disc, disc height, Modic changes and High Intensity Zone (HIZ).
Disc degeneration was visually graded on sagittal T2-weighted images, using CSF (cerebrospinal fluid) as intensity reference as 0: bright, 1: gray, 2: dark, 3: black. [9].
Modic changes were evaluated according to the Modic classification system: Type 1—Hypointense T1 signal and hyperintense T2 signal, Type 2—Hyperintense T1 signal and iso or slightly hyperintense T2 signal [9].
A posterior HIZ was defined as an area of high signal intensity in the posterior annulus fibrosus that was brighter than nucleus pulposus on T2-weighted images [9].
For the analysis, the MRI-changes were dichotomized and transformed into a new binary variable of “present” or “not present”.
Study measures
Age, sex, marital status, highest level of education completed, profession and sick leave information were collected at baseline, Table 1. Highest level of completed education was defined as (1) vocational training, (2) 1-year education after 9 years of school attendance, (3) university <4 years, (4) university ≥4 years, and (5) other education. Profession was categorized according to International Standard Classifications of occupations (ISCO-88) [10] Table 1.
Various self-report functional measures were measured at baseline, at 6 weeks, at 6 months and at 1-year follow-up. These include pain during activity and pain at rest during the previous week measured using an 11 point Numeric Rating Scale (NRS) of 0–10, where ‘10’ reflects the worst pain imaginable and ‘0’ no pain. The validity and reliability of NRS has been well documented [11]. The Norwegian version of the original Oswestry Disability Index (ODI version 1.0) was used to evaluate function. The ODI is comprised of 10 items, categorizes from 0 to 6. The sum of the response scores is presented as a percentage, where 0% represents no disability and 100% represents the maximal disability. The validity and reliability of the ODI are documented in several studies [12]. The Norwegian version of Waddell’s Fear-Avoidance Belief Questionnaire (FABQ) was also used. It has two sub-scales, one for physical activity (FABQ-PA) and one for work (FABQ-Work). Each item is categorized from 0 to 6, with higher ratings indicating increased levels of fear-avoidance beliefs. Seven of the eleven items in the FABQ-Work are summed and ranged from 0 to 42, and four in the FABQ-PA are summed and ranged from 0 to 24 [2]. The validity and reliability of this scale are good [13].
Subjective health complaints (SHC) were measured by a SHC inventory, which is a list of 29 items of common complaints, including depression and anxiety. The sum is normally 29; however, we excluded two questions about ‘back pain’. Therefore, the maximum sum of SHC in our patients was 27 [14].
The Patient’s Global Impression of Improvement scale (PGI-I) was obtained at the 6-week, 6-month and 1-year follow up. This is a 7-item global change scale for back pain with the following categories: (1) completely recovered, (2) much better, (3) a little better, (4) no change, (5) a little worse, (6) much worse, and (7) very much worse. The scale has been validated, and we used the ratings of “much better” or “completely recovered” to define recovery [11]. We used this categorization as our main outcome.
Treatment
Patients received a one-to-one consultation with a specialist in Physical Medicine and Rehabilitation at the Neck and Back Clinic, which included clinical examination; brief intervention and instruction in self-care technique. Brief intervention included explanation about their back pain and changes at the MRI. They were assured that normal activities would not damage their back and they were encouraged to return to daily activities and work as soon as possible. The physician instructed patients in the stretching of the big muscle group, which they were recommended to do once a day for 1 min.
Follow-up
The patients were followed up by consultation with the specialist in Physical Medicine and Rehabilitation after 6 weeks, and after 6 months and after 1 year by mail using a self-report questionnaire.
Data analyses
Our data were analyzed using descriptive statistics with the mean (±standard deviation) for variables with normal distribution and median (range) for variables with a skewed distribution. The prevalence rates of MRI-changes were reported as no changes, or changes at 1, 2 or 3 levels, respectively. Education was collapsed into three categories: (1) vocational training and 1-year education, (2) university education, and (3) other education.
A linear growth model (the random-effects mixed model) was applied to the follow-up data. The assumptions of the linear growth model were checked prior to model building [15]. The presence of MT1 and MT2 changes were modeled separately, and they were added as fixed factors in each model.
Cox’s proportional hazard regression models were built to determine the influence of age, gender, education, pain, function, fear avoidance beliefs and SHC on the relationship between Modic changes and rate of recovery on the PGI-I. A baseline variable was considered to be a confounder, if the regression coefficient of the Modic change variable varied by more than 10%, when the covariate was added (or deleted) to the model [16]. The number of variables included in the multivariate model with a sample size of 107, was estimated to 9 (including ‘Dummy variables’) according to the criteria of 10 events for each independent predictor variable [16]. In the case, that more than 9 variables changed the regression coefficient, those that changed the regressions coefficient with the least value were excluded from the analysis.
Statistical analyses were performed using SPSS for Windows, version 16 (SPSS Inc., Chicago, IL, USA).
Participation
Participation was investigated by comparing patients who declined to participate with participating patients with respect to age and sex. Attrition bias was investigated by comparing baseline variables of patients who dropped out at 6 weeks, 6 months and 1 year, with respect to age, sex, education and MRI.
Ethics
The Committee for Medical Research Ethics in Health Region South East (Norway) and Research Ethics Board of the University Health Network, Toronto (Canada) approved the study.
Results
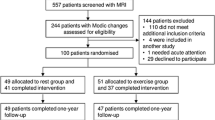
Our study included 269 chronic back pain patients, who were included from July 2007 to July 2009. Their baseline variables are presented in Table 1. Fourty-six of the included patients dropped out at 6 week follow-up and 29 patients did not attend at this follow-up, but attended the follow-up after 6 months. At 6-month follow-up, 26 patients dropped out, 14 did not attend, but attended the 1-year follow-up. Thus, at 1-year follow-up, 107 patients were followed up (Fig. 1). We did not obtain MRI images from five patients, as these patients had their MRI examinations performed at private radiological institutes and the patients did not bring the CD with their MR-scan. These patients were excluded from the analysis. All analyses were performed with and without these five patients, and there were no major differences in baseline variables or recovery-rate between them and the other participants.
There were no significant differences between patients who declined to participate and those that did with respect to age and sex. Fifty-five percent of the included patients dropped out over the course of the study. However, participants did not differ from non-participants with respect to age, sex, education, MRI, and work/sick-leave status (data not shown).
Mean duration of back pain was 3.7 years, which classifies them as chronic low back pain patients [1]. Degenerative changes detected on MRI are presented in Table 2. There were no significant associations between MRI-changes and pain, ODI, FABQ and SHC at baseline (data not shown).
For all self-reported variables, all assumptions for linear mixed models were satisfied. Neither MT1 nor MT2 were significantly associated with the clinical course of pain, ODI, FABQ-PA or FABQ-Work (Table 3).
At 1-year follow-up, 40% of patients rated themselves as recovered. Neither Modic changes nor other degenerative changes on MRI were associated with recovery in the univariate Cox’s models. In the examination of confounders, 10 variables changed the regression coefficient for MT1 more than 10%, with the greatest change in the following order: education, FABQ-work, pain at activity, ODI, FABQ-PA, pain at rest, and SHC (Table 4). The least change in these estimates was for SHC and pain at rest which both was 15%. Because the previous studies have shown correlation between pain and MT1 changes, we excluded SHC from the multivariable models. Education was the only significant covariate in the final multivariable model, with a HRR of 2.20 (95% CI [1.04–4.70]). Patients with a university level education were more likely to recover compared to patients having less education (Table 4).
The following six variables changed the regression coefficient for MT2 more than 10%: age, pain at activity, FABQ-Work, FABQ-PA and education. In the multivariable analysis, educational level was approaching a significant association with recovery in the Modic 2 model with HRR at 2.1 (95% CI [1.00–4.27]) (Table 4).
Discussion
The main result in this study is that neither MT1 nor MT2 changes were significantly associated with the clinical course of pain, function and FABQ in our population of chronic non-specific LBP patients. Our recovery rate was 40%, which might seem poor, but it agrees with the available evidence for patients with chronic LBP [17]. Education was a prognostic factor, which means that the patients with education at the university level had a higher rate of recovery, than the patients with lower education. Lower education is often associated to low-decision authority and heavy physical work, which are well-known prognostic factors for poor recovery [18].
The prevalence of MT1 changes in our study was 14%, which is comparable to some studies [19], while in other studies the prevalence varied from 43 to 59% [4]; however, these studies included patients who had undergone discography, which is known to accelerate Modic changes [11].
Although, there is general agreement that MT1 changes are strongly associated with pain [4], we did not find any association to the clinical course or to patients’ self-reported recovery rate. Modic-associated proinflammatory biochemical mediators have been suggested to be a major origin of pain [6]. MT1 converts to either MT2 or to a normal stage from 14 months to 3 years [20]. However, one possible explanation is that the acute inflammation may have resolved, even though MT1 was still present on the MRI. Moreover, several structures in the spine other than the disc can contribute to pain, including the muscles, ligaments, facet joints and discs [21].
Our brief intervention and self-care technique is recommended by the European Guidelines [1]. In this study, it included fear reduction by reassurance that patients could not hurt their back, and encouragement to return to daily activities and work. However, the success is dependent on the patient’s ability to process this information. Health literacy is an individual’s capacity to seek, understand and utilize health information, [22] and it has been well documented that higher levels of education increase the likelihood of obtaining and understanding health-related information [23]. This means that the level of education needs to be considered when designing effective educational interventions for low back pain.
Age, gender, pain, function and SHC, which include depression, were not associated with recovery. When identifying prognostic factors, it is recommended to address all risk domains, including biological, medical, psychological, socio-economic and occupational in prognostic models [24]. This study confirms this statement, as it demonstrates, that variables might be significant in crude analyses, but not in the multivariate analyses, when the effects of variables from all domains are combined.
There are limitations to our study. There were a substantial number of dropouts at all time-points, which is an inevitable problem in the clinical cohort studies. The treatment patients received (brief intervention and instruction in stretching), might be less binding for the patients, than for instance surgery, where it is obvious for the patients that follow-up is both necessary and important.
However, there were no significant differences in sex, age, education, MRI-changes or patients working or on sick-leave status between participants and non-participants. Another limitation is that we did not do a power analysis prior to the study. However, according to Guyatt et al. [25] the sample size is adequate if the upper boundary of the confidence interval (CI) is less than the minimal clinical important difference (MCID). The MCID for ‘Pain at rest’ is 2 points and for ‘ODI’ 9 points [26] and the upper boundaries of the CIs were less than the (MCID) for both variables (Table 3). The CIs in the cox regression analysis were all narrow. Thus, it seems that the sample size was adequate according to the above-mentioned considerations.
Conclusion
In a cohort of patients with chronic LBP, the prevalence of MT1 was 14%, which is comparable with other studies. Neither MT1 nor MT2 changes influenced the clinical course of pain and function and they were not prognostic factors for recovery. Educational level was a strong predictor of recovery. Clinicians need to be reminded to approach patients with chronic LBP using a biopsychosocial model of recovery.
References
Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G (2006) Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 15(Suppl 2):S192–S300
Waddell G (1987) 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine 12(7):632–644
Sheehan NJ (2010) Magnetic resonance imaging for low back pain: indications and limitations. Ann Rheum Dis 69(1):7–11
Jensen TS, Karppinen J, Sorensen JS, Niinimaki J, Leboeuf-Yde C (2008) Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J 17(11):1407–1422
Burke JG, Watson RW, McCormack D, Dowling FE, Walsh MG, Fitzpatrick JM (2002) Intervertebral discs which cause low back pain secrete high levels of proinflammatory mediators. J Bone Joint Surg Br 84(2):196–201
Schmid G, Witteler A, Willburger R, Kuhnen C, Jergas M, Koester O (2004) Lumbar disk herniation: correlation of histologic findings with marrow signal intensity changes in vertebral endplates at MR imaging. Radiology 231(2):352–358
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR (1988) Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 166(1 Pt 1):193–199
Holtermann A, Hansen JV, Burr H, Sogaard K (2010) Prognostic factors for long-term sickness absence among employees with neck-shoulder and low-back pain. Scand J Work Environ Health 36(1):34–41
Carrino JA, Lurie JD, Tosteson AN, Tosteson TD, Carragee EJ, Kaiser J, Grove MR, Blood E, Pearson LH, Weinstein JN, Herzog R (2009) Lumbar spine: reliability of MR imaging findings. Radiology 250(1):161–170. doi:10.1148/radiol.2493071999
Revised International Standard Classification of Occupations: (ISCO-88) (1987) [S.I]: International Labour Office, Bureau of Statistics
Farrar JT, Pritchett YL, Robinson M, Prakash A, Chappell A (2010) The clinical importance of changes in the 0 to 10 numeric rating scale for worst, least, and average pain intensity: analyses of data from clinical trials of duloxetine in pain disorders. J Pain 11(2):109–118
Roland M, Fairbank J (2000) The Roland-Morris disability questionnaire and the Oswestry disability questionnaire. Spine 25(24):3115–3124
Grotle M, Brox JI, Vollestad NK (2006) Reliability, validity and responsiveness of the fear-avoidance beliefs questionnaire: methodological aspects of the Norwegian version. J Rehabil Med 38(6):346–353. doi:10.1080/16501970600722403
Eriksen HR, Ihlebaek C, Ursin H (1999) A scoring system for subjective health complaints (SHC). Scand J Public Health 27(1):63–72
West B, Welch K, Galecki A (2006) Linear mixed models: a practical guide using statistical software. Chapman Hall/CRC Press, London
Rothman K, Greenland S, Lash T (2008) Modern epidemiology, 1st edn. Lippincott Williams & Wilkins, Boston
Hayden JA, Dunn KM, van der Windt DA, Shaw WS (2010) What is the prognosis of back pain? Best Pract Res Clin Rheumatol 24(2):167–179
Chibnall JT, Tait RC (2009) Long-term adjustment to work-related low back pain: associations with socio-demographics, claim processes, and post-settlement adjustment. Pain Med 10(8):1378–1388
Modic MT, Ross JS (2007) Lumbar degenerative disk disease. Radiology 245(1):43–61
Kuisma M, Karppinen J, Niinimaki J, Kurunlahti M, Haapea M, Vanharanta H, Tervonen O (2006) A three-year follow-up of lumbar spine endplate (Modic) changes. Spine 31(15):1714–1718
Beresford ZM, Kendall RW, Willick SE (2010) Lumbar facet syndromes. Curr Sports Med Rep 9(1):50–56
Health literacy and the Millennium (2010) Development goals: United Nations Economic and Social Council (ECOSOC) regional meeting background paper (abstracted). J Health Commun 15(Suppl 2):211–223. doi:10.1080/10810730.2010.499996
Services USDoHaH (2000) Healthy people 2010, understanding and improving health. Washington, DC, US Government Printing Office
Altman DG, Lyman GH (1998) Methodological challenges in the evaluation of prognostic factors in breast cancer. Breast Cancer Res Treat 52(1–3):289–303
Guyatt G, Jaeschke R, Heddle N, Cook D, Shannon H, Walter S (1995) Basic statistics for clinicians: 2. Interpreting study results: confidence intervals. CMAJ 152(2):169–173
Maughan EF, Lewis JS (2010) Outcome measures in chronic low back pain. Eur Spine J 19(9):1484–1494. doi:10.1007/s00586-010-1353-6
Acknowledgments
The authors wish to acknowledge Dr. Sophie Soklaridis, Research Manager, Department of Surgery, Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, Ontario, Canada for constructive criticism during preparation of this manuscript. We also acknowledge the assistance of Marianne Landa, MRI-technologist, Section of Neuroradiology, Oslo University Hospital, Ullevaal Oslo, Norway.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keller, A., Boyle, E., Skog, T.A. et al. Are Modic changes prognostic for recovery in a cohort of patients with non-specific low back pain?. Eur Spine J 21, 418–424 (2012). https://doi.org/10.1007/s00586-011-1964-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-011-1964-6