Abstract
Percutaneous vertebroplasty, comprising an injection of polymethylmethacrylate (PMMA) into vertebral bodies, is a practical procedure for the stabilization of osteoporotic compression fractures as well as other weakening lesions. Cement leakage is considered to be one of the major and most severe complications during percutaneous vertebroplasty. The viscosity of the material plays a key role in this context. In order to enhance the safety for the patient, a rheometer system was developed to measure the cement viscosity intraoperatively. For this development, it is of great importance to know the proper viscosity to start the procedure determined by experienced surgeons and the relation between the time period when different injection devices are used and the cement viscosity. The purpose of the study was to investigate the viscosity ranges for different injection systems during conventional vertebroplasty. Clinically observed viscosity values and related time periods showed high scattering. In order to get a better understanding of the clinical observations, cement viscosity during hardening at different ambient temperatures and by simulation of the body temperature was investigated in vitro. It could be concluded, that the direct viscosity assessment with a rheometer during vertebroplasty can help clinicians to define a lower threshold viscosity and thereby decrease the risk of leakage and make adjustments to their injection technique in real time. Secondly, the acceleration in hardening of PMMA-based cements at body temperature can be useful in minimizing leakages by addressing them with a short injection break.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last 10 years, percutaneous vertebroplasty has become one of the most important techniques for the stabilization of osteoporotic compression fractures as well as other weakening lesions, such as angioma or metastatic tumors, and therefore an indispensable tool in the fight against the pains induced by osteoporosis and other conditions [10]. In this procedure, the vertebral body is augmented with bone cement. Most common used cements are acrylic cements. The bone cement polymerizes and hardens on injection into the vertebral body and stabilizes it. Typically, the cements are prepared directly prior to injection by mixing powder [polymethylmethacrylate (PMMA), X-ray contrast agent (e.g., barium sulfate)] and liquid [methylmethacrylate monomer (MMA)] to form a fluid mixture. Percutaneous vertebroplasty, comprising an injection of PMMA into vertebral bodies leads to immediate pain relief in 80–90% of patients [8, 10, 16]. However, cement leakage is a common occurrence and represents the main complication risk for vertebroplasty [14]. Cement leakage from the vertebral body is reported to be 20–65% [6, 10]. While most leakages are asymptomatic, serious complications can arise if the cement causes nerve root or spinal cord compression or pulmonary embolism [5, 11, 12, 15].
During the procedure, bone cement is injected through a cannula into a vertebral body. Different injection systems are available from the market, e.g., simple syringes (1–5 ml, connected to the cannula) to inject the cement by applying manual force, or injection devices using force amplification allowing higher forces being applied to the cement during injection. A surgeon survey showed that the majority prefer simple syringe systems, which give the surgeon a force feedback during injection and, therefore, a good tactile feeling for the procedure. There are many factors that influence the injection biomechanics and, ultimately, whether or not cement leakage occurs. Factors affecting injection biomechanics include cement viscosity, pressure, injection speed, volume injected and local tissue morphology. Local tissue morphology includes the apparent bone density, which depends on the state of osteoporosis and fracture patterns, e.g., typical osteoporotic sintering fractures or tumor tissue, which presents a high variability in cement infiltration behavior in general. Among these factors, cement viscosity has been identified as an especially important parameter, in relation to cement leakage, which may be used for controlling the risk of cement leakage [1, 3, 4]. The risk of cement leakage is shown to be reduced at high cement viscosity injection. During polymerization of commonly used PMMA cements, the viscosity steadily increases. Hence, the cement should be injected at the latest time point possible in order to prevent leakage and extravasation. This, however, leads to high injection forces that may not be overcome anymore using simple manual injection systems [1]. Bohner et al. [1, 3, 4] show the significance of understanding viscosity during vertebroplasty. It is also important to understand how this information can be applied clinically.
Clinically the proper injection viscosity was determined by visual assessment of the flow characteristics of freshly exposed cement from the tip of a syringe by the surgeon. The elapsed time after starting to mix the cement was also considered as a measure of the degree to which the cement had polymerized by the surgeon and the OR personnel.
In order to enhance the safety for the patient, it was decided to develop a rheometer system, which could be used intra-operatively to measure cement viscosity and allow access to this value by the surgeon. This would help the surgeon to perform vertebroplasty in a more standardized manner.
The goal of this study was to determine the range of injection viscosities during conventional vertebroplasty interventions. A further goal was to determine the usable viscosity limit for a variety of injection devices.
Methods
First, clinical observations were performed to investigate the cement viscosity ranges for different injection systems used during conventional vertebroplasty. Afterwards, cement viscosity during hardening at different ambient temperatures and by simulation of the body temperature was investigated in vitro to get a better base for the conclusions made in the presented study.
Clinical measurements
A total of 18 vertebroplasty surgeries were visited to observe and record the viscosity of the cement during hardening in the clinical setting. Eighteen patients (eight female, ten male; mean age 75.6 ± 7.9 years) were selected from patients admitted to the Orthopedic Department of the Inselspital (Bern, Switzerland) for vertebroplasty. Surgeries were performed by experienced spine surgeons. The technique used for augmenting the vertebral bodies is outlined by Heini et al. [10]. The used cement was a PMMA bone cement, specially formulated for vertebroplasty (Powder w/w: methylmethacrylate polymer 56.8%, methylmethacrylate-styrene copolymer 14.2%, benzoyl peroxide 0.4%, barium sulfate 28.6%. Liquid v/v: methylmethacrylate monomer 95.05%, ethylene dimethacrylate monomer 4.28%, dimethyl-p-toluidine 0.67%, hydroquinone 20 ppm, 4-methoxyphenol 12 ppm). The augmentation was performed using standard 1 and 2 ml polypropylene syringes (Codan, Codan Medical, Denmark) to inject the PMMA cement through standard 8 gauge, 150 mm-bone biopsy needles (Trapsystem, HS Hospital Service S.p.A., Italy) under fluoroscopic control. Cement preparation was done by different nurses by manually mixing the cement ingredients in a polypropylene beaker using a spatula. The needle’s stylet was also used to inject cement into the vertebral body by inserting and clearing the cement from the needle as a last injection step if needed. The inner diameter of the injection devices used were 8.5, 4.5 and 3.4 mm for the 2 ml syringe, 1 ml syringe and stylet, respectively. One to six vertebral bodies were augmented in each patient (mean 3.4 ± 1.2 vertebrae) requiring one to two portions of cement per patient (injected cement volume per vertebrae, 3.0 ± 1.3 ml).
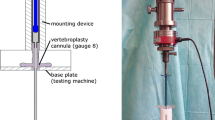
To investigate the hardening behavior of the cement used, 3 ml of the prepared cement was used for viscosity determination during hardening. For measuring the viscosity, the freshly mixed cement was placed in a rotational rheometer (RheolabQC, Anton Paar, Graz, Austria). The rheometer is equipped with a custom-designed double-gap measurement system of PMMA-resistant polypropylene (Fig. 1), and rheological data were recorded directly to a PC. The rheometer was calibrated with standard silicon oils (12, 30, 56 Pa s, Brookfield Engineering Laboratories, Middleboro, MA) and was set to operate with an oscillatory frequency of 1 Hz and a maximum torque of 3 mNm. Real viscosity (η′) and ambient temperature (T) were recorded directly in a PC for 24 portions of cement during the 18 vertebroplasty procedures. Data were recorded at a sampling rate of 0.2 Hz. Other recorded data included the time at which the rheometer was started and when each injection instrument was used for the first time. Recorded times were always related as time after starting the mix of the cement. The time when the rheometer was started for data acquisition differed from 90 to 150 s after mixing the cement.
Clinical investigation, using in situ viscosity measurement of the used cement, was conducted in three distinct phases. In phase 1, the surgical technique was observed and data were recorded without reporting to the surgeon any viscosity information. The proper injection viscosity was determined by predefined time after starting the mixing as a measure of the degree to which the cement had polymerized. Afterwards, the flow characteristics of freshly exposed cement from the tip of a syringe were visually assessed by the surgeons before starting cement injection. For phases 2 and 3, previous viscosity data were discussed with the surgeons and a pre-operation lower threshold viscosity was set for the following phase. Predefined lower threshold viscosities were 23 and 30 Pa s for the second and third phase, respectively. In these phases, the proper injection viscosity was determined using a combination of the techniques described above and reporting of the real-time viscosity data at regular intervals. Adherence to the pre-operative target injection viscosity was optional.
The time index from the rheometer was used to determine at which viscosity each of the three injection instruments were used for the first time. Ambient temperatures recorded during the surgery are presented as mean ± standard deviation for the observation phases, respectively. Viscosity and time ranges, when using the respective injection instruments first, are presented as mean ± standard deviation. Mean of the resulting viscosity range determined for the last use of the instruments was used for estimating the approximate maximal force needed to inject the cement. This was done using the Law of Hagen-Poiseuille [4]. For this analysis, a constant flow rate of 0.1 ml/s was assumed [13].
Clinical assessment of the cement viscosity as function of time showed a high variability. Because the ambient temperature defines mainly the polymerization rate of the exothermic polymerization, the mentioned relation was analyzed in more detail. The ambient temperature during the surgeries was between 19.3 and 22.7°C. Therefore, the dependence of viscosity versus time on ambient temperature was analyzed by a method suggested by Farrar et al. [7]. This method was derived by the Arrhenius equation (1), which describes the rate k, at which a chemical reaction will proceed. Rate of the cement polymerization is defined by the time t v needed to reach the given cement viscosity after starting the mixing (2) [7].
where t v is the time taken to reach a given viscosity, A is a constant, E the activation energy, R the universal gas constant and T the ambient temperature. Logarithmic transformation of equation (2) leads to a linear relation of ln (t v) to 1/T. Hence, for a predetermined viscosity, 1/T versus ln t v was plotted and analyzed for linearity, and thereby proofing the model suggested by Farrar et al. [7] by revealing a high linear correlation coefficient. Results of the mentioned correlation of the viscosity during hardening to the ambient temperature measured during the surgeries was not found to be high (r 2 = 0.63). Therefore, a more standardized investigation in the lab was performed to prove the usability of the model to describe the hardening dependence on ambient temperature.
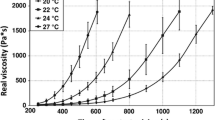
Laboratory measurements of ambient temperature dependence on cement viscosity during hardening
In vitro experiments were conducted to investigate the influence of ambient temperature on the viscosity profile of the PMMA cement in a more standardized laboratory setting. The rotational rheometer was retrofitted with a custom temperature chamber (Fig. 1) controlled by a thermostatic circulating water bath (Ecoline RE306, Lauda GmbH, Germany) to simulate different ambient temperatures. Additionally, a lid was used to keep the monomer from evaporating and developing a thick cement surface layer, while the majority of the cement mass remained fluid-like. Test samples and all materials that came into contact with the cement samples were allowed to equilibrate at the testing temperature for at least 6 h using a climate chamber (KBF, WTB Binder GmbH, Germany). The samples were removed from the climate chamber and mixed with a beaker and spatula for 60 s. A 3.0 mL sample was placed in the custom measurement system and the rheological testing began 2 min after the start of mixing. Data were recorded at temperatures of 20, 22, 24 and 27°C and were repeated eight times at each temperature. The mean of real viscosity (η′) was analyzed at regular intervals for each temperature set. These averaged curves were then used to determine the dependence of viscosity on temperature (Arrhenius correlation) as described previously. Determined viscosity values for the correlation analysis was 30; 100; 150; 500; 1,000 and 1,500 Pa s.
Laboratory measurements of cement viscosity behavior at temperature profile jumping from ambient to body temperature
The effect of body temperature on cement viscosity was examined and presented for a representative measurement. The custom temperature chamber and thermostat were retrofitted with a fluid bypass system. The bypass system allows the chamber to be left at room temperature, while heated fluid flows through the system without entering the chamber. When the predetermined cement viscosity of 40 Pa s was reached, the bypass was removed and the chamber was flooded with the fluid, pre-heated to 37°C. An aluminum measurement system was used for better heat transfer between the temperature chamber and cement (Fig. 1).
The experiment was as follows: as a control, one portion of cement was mixed and measured as described earlier at room temperature. A second portion of the cement was also measured at room temperature starting in the same way as for the first control portion, with 37°C fluid flowing in the bypass system (Fig. 1). After reaching a viscosity of 40 Pa s, the fluid was redirected, forcing the 37°C water through the measuring chamber (Fig. 1). The value of 40 Pa s was chosen as a relevant value based on results from clinical investigations performed in the study herein. To monitor the chamber temperature, a thermocouple and data logger (Almemo-2390, Ahlborn GmbH, Germany) were used to record data at a sampling of 1 Hz.
Results
Clinical measurements
A sampling of hardening curves, including both extremes, measured during vertebroplasty is shown in Fig. 2. A typical hardening curve is flat in the first few minutes after mixing. After reaching a viscosity of 25–50 Pa s, the viscosity starts to increase at an-ever increasing rate for 2–3 min. At a viscosity of about 150 Pa s, the rate at which viscosity increases is very high as the suspension polymerizes.
In the clinic, a high variability in the hardening behavior was observed and is illustrated in Fig. 2. For example, the time required for the cement to reach 20 Pa s ranged from 350 to 550 s and the time required to reach 100 Pa s ranged from 530 to 840 s, which corresponds to a range of 3.3 and 5.2 min, respectively. Data on the first injection of each portion of cement for all phases is shown in Table 1. For all phases, the mean first injection viscosity was 23.7 ± 4.4 Pa s. The time required for all 24 portions of cement to reach the first injection viscosity was 430 ± 51 s with a range of 350–550 s. The ambient temperature for all intra-operative measurements was 21.3 ± 0.8°C with a range of 19.8–22.6°C. Mean of the viscosity range determined for the last use of the instruments and the estimation of the approximate maximal forces are reported in Table 2, together with the inner diameter of each injection instrument. The highest injection viscosity recorded was 2,400 Pa s, which was accomplished by clearing the injection needle with the stylet. Using the Arrhenius equation (1), only a weak correlation (r 2 = 0.63) between polymerization time and ambient temperature could be found for the measurements taken intra-operatively.
Laboratory measurements
Temperature-controlled viscosity measurements conducted in vitro are shown in Fig. 3. The general shape of the hardening curve is similar to what is seen in the clinic. In the laboratory setting, it was confirmed that the PMMA cement is highly temperature sensitive. Table 3 shows the average time required to reach various viscosities.
In Fig. 4, the Arrhenius correlation for temperature-controlled experiments is shown. Figure 4 represents the dependence of time until a viscosity on average of 1,500 Pa s was reached at different controlled temperatures. A linear regression (r 2 = 0.9945) shows a strong correlation and therefore a high dependency between the polymerization rate and the ambient temperature. Dependencies for other viscosities evaluated (100, 500, 1,000 Pa s) revealed also a high linear correlation (r 2 > 0.99), showing the consistency of the data received and the conformity of the applied model described by the Arrhenius equation on the hardening behavior of the PMMA cement investigated.
In Fig. 5, the simulation of cement injection into the body is shown. The primary y-axis shows the viscosity of the two cements: cement (1) at room temperature and cement (2) at room temperature and then switched to 37°C. The secondary y-axis shows the temperature of the fluid chamber in which the cement was measured. Simulated body temperature was reached within approximately 30 s. From this result, it is evident that the cement viscosity inside the vertebral body and needle will be at a higher viscosity than the cement left at ambient room temperature.
Discussion
During the preparations of this study, literature review and personal experience led the investigators to infer that the initial injection viscosity would be in the range of 20–50 Pa s. The rheometer in question was therefore designed and calibrated to be most accurate at this interval. Measurements at viscosities greater than 500 Pa s are inherently less accurate by design of the measurement system. As the viscosity increases, the constant shear stress applied to the sample yields an ever-decreasing shear strain, which is the value used by the rheometer software to calculate viscosity. At viscosity values more than 500 Pa s, the shear strain is no longer visible to the naked eye. The method used herein is less accurate at higher viscosity levels more than 500 Pa s. However, the results presented show a high regression coefficient of the Arrhenius plot and very little scattering of the data at high viscosities. This demonstrates that this method of viscosity measurement is still sensitive enough to discriminate between very high cement viscosities.
During the clinical investigation, there was only a weak correlation found between viscosity during hardening and ambient temperature. This is contrary to the more standardized laboratory investigations, which reveal a high correlation between cement viscosity during hardening and the ambient temperature. The scattering in the clinical setting is likely due to the number of other influences on hardening behavior such as atmospheric conditions [9] (e.g., oxygen concentration, humidity, temperature), variation of the cement composition (e.g., fluid to powder ratio) due to preparation, method of mixing [2] and others. The time needed to reach 20 Pa s was in a relatively high range of 200 s and had high variation. Although the mixing procedures were essentially the same, small differences in mixing techniques among the different nurses involved in the study may have influenced cement hardening [2].
The trend seen in Table 2 that the maximum injectable viscosity is inversely proportional to syringe diameter was expected. The equivalent force required to inject cement at these viscosities relates quite well to the proposed limit of 150 N for syringe-type injections [4].
Many factors are involved in determining the viscosity of PMMA other than just the composition of the cement and polymerization time. After mixing, swelling of the PMMA polymer beads has been identified to cause the initial rise in viscosity. In the later stages of hardening, the polymerization rate becomes the dominant factor in determining cement viscosity [7].
Because of the high variability and numerous influences in hardening behavior, direct assessment of cement viscosity appears to be of great importance for a safe injection. At a minimum, cement should be appraised visually before starting the injection. Visual appraisal is however subjective and difficult to standardize. An objective and reproducible viscosity assessment with a rheometer during vertebroplasty procedure provides many benefits. Real-time viscosity measurements can prompt a surgeon when a predetermined minimum viscosity has been reached. In addition, the risk of cement leakage depends on the bone structure (fracture pattern, tissue morphology inside the vertebral body). Viscosity prompts could possibly be used for specific indications. Yet another use is to estimate the amount of time remaining to complete injection before the cement becomes too hard.
When cement injection has been started an accelerated hardening behavior of the cement reaching the body temperature either in the cannula or the vertebral body has to be taken into account as shown in the study presented. However, this effect of the exothermic reactions underlying PMMA hardening can be beneficial in clinical practice. If cement leakage is observed it can be addressed by stopping the injection for around 30–60 s, leading to a blocking of the leakage pathway by the faster hardening of the cement at body temperature.
Conclusion
Time after mixing is not a sufficient measure for determining PMMA viscosity. The complexity and amount of influence factors do not allow the user to accurately predict the hardening behavior of PMMA cements. Direct viscosity assessment with a rheometer during vertebroplasty can help clinicians to better control the risk of cement leakage and make adjustments to their injection technique in real time. Acceleration in the hardening of PMMA-based cements at body temperature can be useful in minimizing the occurrence of leakage by addressing them with a short injection break.
References
Baroud G, Bohner M, Heini P, Steffen T (2004) Injection biomechanics of bone cements used in vertebroplasty. Biomed Mater Eng 14(4):487–504
Baroud G, Matsushita C, Samara M, Beckman L, Steffen T (2004) Influence of oscillatory mixing on the injectability of thee acrylic and two calcium-phosphate bone cements for vertebroplasty. J Biomed Mater Res 68B(1):105–111. doi:10.1002/jbm.b.20010
Baroud G, Crookshank M, Bohner M (2006) High-viscosity cement significantly enhances uniformity of cement filling in vertebroplasty: an experimental model and study on cement leakage. Spine 31(22):2562–2568. doi:10.1097/01.brs.0000240695.58651.62
Bohner M, Gasser B, Baroud G, Heini P (2003) Theoretical and experimental model to describe the injection of a polymethylmethacrylate cement into a porous structure. Biomaterials 24:2721–2730. doi:10.1016/S0142-9612(03)00086-3
Burton AW, Rhines LD, Mendel E (2005) Vertebroplasty and kyphoplasty: a comprehensive review. Neurosurg Focus 18:1–9. doi:10.3171/foc.2005.18.3.2
Cortet B, Cotton A, Boutry N, Flipo RM, Duguesnoy B, Chastanet P, Delcambre B (1999) Percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures: an open prospective study. J Rheumatol 26(10):2222–2228
Farrar DF, Rose J (2001) Rheological properties of PMMA bone cements during curing. Biomaterials 22:3005–3013. doi:10.1016/S0142-9612(01)00047-3
Grados F, Depriester C, Cayrolle G, Hardy N, Deramond H, Fardellone P (2000) Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford) 39:1410–1414. doi:10.1093/rheumatology/39.12.1410
He S, Scott C, Higham P (2003) Mixing of acrylic bone cement: effect of oxygen on setting properties. Biomaterials 24:5045–5048. doi:10.1016/S0142-9612(03)00406-X
Heini PF, Wälchli B, Berlemann U (2000) Percutaneous transpedicular vertebroplasty with PMMA, operative technique and early results: a prospective study for the treatment of osteoporotic compression fractures. Eur Spine J 9:445–450. doi:10.1007/s005860000182
Hulme PA, Krebs J, Ferguson SJ, Berlemann U (2006) Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine 31:1983–2001. doi:10.1097/01.brs.0000229254.89952.6b
Jang JS, Lee SH, Jung SK (2002) Pulmonary embolism of polymethylmethacrylate after percutaneous vertebroplasty. Spine 27(19):E416–E418. doi:10.1097/00007632-200210010-00021
Krebs J, Ferguson SJ, Bohner M, Baroud G, Steffen T, Heini P (2005) Clinical measurements of cement injection pressure during vertebroplasty. Spine 30(5):E118–E122. doi:10.1097/01.brs.0000154670.49227.65
Laredo JD, Hamze B (2004) Complications of percutaneous vertebroplasty and their prevention. Skeletal Radiol 33:493–505. doi:10.1007/s00256-004-0776-8
Lee BJ, Lee SR, Yoo TY (2002) Paraplegia as a complication of percutaneous vertebroplasty with polymethylmethacrylate. Spine 27(19):E419–E422. doi:10.1097/00007632-200210010-00022
Mathis JM, Deramond H, Belkoff SM (2002) Percutaneous vertebroplasty, 1st edn. Springer, New York
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boger, A., Wheeler, K.D., Schenk, B. et al. Clinical investigations of polymethylmethacrylate cement viscosity during vertebroplasty and related in vitro measurements. Eur Spine J 18, 1272–1278 (2009). https://doi.org/10.1007/s00586-009-1037-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-009-1037-2