Abstract
Pre-clinical in vitro tests are needed to evaluate the biomechanical performance of new spinal implants. For such experiments large animal models are frequently used. Whether these models allow any conclusions concerning the implant’s performance in humans is difficult to answer. The aim of the present study was to investigate whether calf, pig or sheep spine specimens may be used to replace human specimens in in vitro flexibility and cyclic loading tests with two different implant types. First, a dynamic and a rigid fixator were tested using six human, six calf, six pig and six sheep thoracolumbar spine specimens. Standard flexibility tests were carried out in a spine tester in flexion/extension, lateral bending and axial rotation in the intact state, after nucleotomy and after implantation. Then, the Coflex interspinous implant was tested for flexibility and intradiscal pressure using another six human and six calf lumbar spine segments. Loading was carried out as described above in the intact condition, after creation of a defect and after implantation. The fixators were most easily implantable into the calf. Qualitatively, they had similar effects on ROM in all species, however, the degree of stability achieved differed. Especially in axial rotation, the ROM of sheep, pig and calf was partially less than half the human ROM. Similarly, implantation of the Coflex interspinous implant caused the ROM to either increase in both species or to decrease in both of them, however, quantitatively, differences were observed. This was also the case for the intradiscal pressure. In conclusion, animal species, especially the calf, may be used to get a first idea of how a new pedicle screw system or an interspinous implant behaves in in vitro flexibility tests. However, the effects on ROM and intradiscal pressure have to be expected to differ in magnitude between animal and human. Therefore, the last step in pre-clinical implant testing should always be an experiment with human specimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
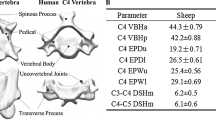
New spinal implants generally need to be tested in vitro before they go into clinical use. For such tests, spine specimens from human donors are preferably used. However, the availability of human specimens is limited, there is a potential risk of infection and most of them show various signs of degeneration. Therefore, animal models are regularly used instead, most commonly calf, pig and sheep. Whether these models allow any conclusions concerning the implant’s performance in humans is difficult to answer. Comparative studies showed that the motion characteristics of the intact spines of calf and sheep are surprisingly similar to those of the human [20, 22]. Also, qualitatively, the anatomy of the lumbar spine of these species is similar, yet the sizes partially differ considerably [5, 21]. Even based on such comparative data, it is difficult to predict whether a certain species is suitable to test a certain implant because a complex combination of various morphological and functional parameters needs to be considered. Furthermore, it cannot be predicted whether an implant, which does not perfectly fit the anatomy of the chosen animal model, yields misleading results. Some of these questions could probably be answered if additional comparative implant tests were available. These, however, are rare and, to date, only cover single species and single types of implants [15, 16].
The aim of the present study therefore was to carry out comparative implant tests in order to investigate whether calf, pig or sheep spine specimens may be used to replace human specimens in in vitro flexibility and cyclic loading tests with two different implant types: internal fixators and interspinous spacers.
Materials and methods
This study is composed of two independent experiments on very different implants since it is suspected that the suitability of animal species differs between different implant types. For the same reason, the parameters evaluated in the two experiments also differed to cover a larger range of what can possibly be evaluated in biomechanical in vitro experiments.
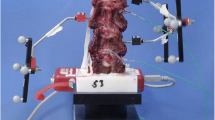
In the first part of this study a dynamic and a rigid internal fixator were tested. For both fixators the same polyaxial pedicle screws were used (tangoRS, Ulrich medical, Ulm, Germany) (Fig. 1). They were available in lengths of 30, 35, 40 and 45 mm and a diameter of 5.5 mm. In case of the dynamic fixator these screws were longitudinally connected using flexible rods made of a hollow, metallic spiral while in case of the rigid fixator solid rods were used. Both had a diameter of 6 mm.
They were implanted into the segment L1–2 of six human (all under 60 years of age), six calf (9–12 months old), six pig (6–9 months old) and six sheep (2–6 years old) thoracolumbar spine specimens. The specimens covered the last thoracic vertebra to L3 in the three animal groups and the last thoracic vertebra to L5 in the human group. Note that calf, sheep and pig have various numbers of thoracic vertebrae, mostly 13–16. All specimens were freshly dissected and frozen at −20°C for storage. Before testing the specimens were thawed and all soft tissue was removed taking care to preserve the intervertebral disc, ligaments and joints capsules. The upper part of the most cranial vertebra and the lower part of the most caudal vertebra were embedded in polymethylmetacrylate in order to allow fixation in the testing devices.
The specimens were tested for flexibility in a spine tester [19] using pure moments of ±7.5 N m in flexion/extension, lateral bending and axial rotation in the intact state, after nucleotomy at L1–2 and after bridging this level with the dynamic and the rigid fixator in alternating sequence. For the calf the 45 mm screws were used, for the pig the 35 mm screws and for the sheep the 30 mm screws. Nucleotomy was carried out from a right posterolateral approach after partial resection of the facet joint and fenestration of the flaval ligament. As recommended, the specimens were allowed to move unconstrained in the five uncontrolled degrees of freedom during loading [23]. The three-dimensional flexibility of the bridged segment was continuously recorded using an ultrasound based motion analysis system (WinChain, Zebris, Isny, Germany, resolution 0.1 mm). From the load-deformation curves, range of motion (ROM) was determined as the rotation at +7.5 N m and −7.5 N m load.
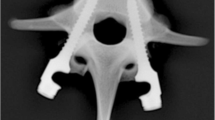
In the second part of this study the Coflex interspinous implant (Paradigm Spine, Wurmlingen, Germany) was tested. This implant has the shape of a “U” and is placed between two adjacent spinous processes (Fig. 2). After implantation, the lateral wings are crimped towards the spinous processes to improve fixation. The Coflex implant was available in five different heights between 8 and 16 mm.
Six human (age 29–67 years) and six calf (age 9–12 months) lumbar spine segments (three L2–3 and three L4–5) were harvested, stored and prepared as described above. Pig and sheep could not be tested in this part of the study since the Coflex interspinous spacer did not fit the interspinous space and spinous process thickness of these two species. Before testing, a pressure transducer (FMSPEZ50, MIPM GmbH, Mammendorf, Germany) was implanted into the nucleus pulposus to record the intradiscal pressure (IDP) during loading. Loading was carried out in the spine tester as described above under pure moments of ±7.5 N m in the intact condition, after creation of a standardised defect and after implantation. The defect consisted of a bilateral hemifacetectomy with resection of the flaval ligaments. For implantation, additionally, the supra- and interspinous ligaments had to be resected. From the load–deformation curves range of motion (ROM) and the kyphotic tilt caused by creation of the defect and by implantation were determined.
Wilcoxon rank sum tests were used to statistically compare the animals species with the human. Wilcoxon signed rank tests were applied to check for differences within each group. The P values were not corrected for multiple comparisons since this study was explorative.
Results
The fixators were easily implantable into the calf. Implantation into the pig was more difficult due to the prominent facet joints. For the sheep even the smallest screws (30 mm length, 5.5 mm diameter) tended to be too long and too large in diameter, yet, implantation was still possible.
The intact segments L1–2 of the sheep and pig had a much larger ROM than the human in all three loading planes (P < 0.05) (Table 1). This was also the case for the calf but only in lateral bending. These different “starting positions” made comparisons between the four species difficult. To overcome this problem, the ROM after nucleotomy and after implantation was normalised to the intact ROM within each species group.
Nucleotomy caused the normalised ROM to increase in all species. However, in all loading directions this increase was much larger for the human than for the calf, pig and sheep (P < 0.05) except for the calf in flexion and extension (P > 0.05) (Figs. 3, 4 and 5). Thus, similar to the intact ROM, the calf was the animal, which was closest to the human. Yet, it was still far from identical.
The two fixators had similar effects on the normalised ROM in all species: their stabilising effect was smallest in axial rotation and the dynamic fixator resulted in a larger ROM than the rigid one. However, quantitatively, the degree of stability achieved with the two fixators tended to differ between the three animal species and the human. This was most obvious for the dynamic fixator and in axial rotation (Fig. 5). In this loading direction, the normalised ROM of the animal species was partially less than half the ROM of the human. In contrast, using the rigid fixator the differences were much smaller (P > 0.05). Neither for the dynamic nor for the rigid fixator, one of the three animal species was found to be generally closer to the human than the others.
The Coflex interspinous implant was easily implantable into the calf lumbar spine segments. However, even the largest implant (16 mm) tended to be too small concerning height and width.
Again, the ROM of the intact segments differed between calf and human (Fig. 6). However, within both species groups implantation had similar effects. Both, the human and the calf segments become kyphotic by in median 1.3° (Fig. 6). Also, in both species groups, the ROM tended to increase in flexion, axial rotation and lateral bending but decreased in extension. However, the statistical evaluation within each group yielded different results.
ROM in flexion/extension in the intact condition, after creation of the defect (bilateral hemifacetectomy with resection of the flaval ligaments), and after implantation of the Coflex interspinous implant. The border between the light and dark parts of each bar represent the median kyphotic tilt of the segments caused by creation of the defect and by implantation. Median with range. *P < 0.05
The pressure measured in the calf intervertebral disc nucleus showed smaller interindividual differences than the pressure measured in the human specimens (for technical reasons IDP could be measured in only four human specimens) (Fig. 7). Qualitatively, the pressure curves were similar for calf and human. In both species implantation of the Coflex interspinous implant had almost no effect in flexion, lateral bending and axial rotation but suppressed the increase in IDP in extension (Fig. 7). Quantitatively, however, differences were found. In some cases the calf had higher pressure values in some the human.
Individual intradiscal pressure curves during flexion/extension loading of four human and six calf lumbar spine specimens in the intact condition and after implantation of the Coflex interspinous implant. Numbers indicate the median intradiscal pressure in MPa at −7.5 N m (extension), 0 N m (unloaded condition) and + 7.5 N m (flexion)
Discussion
In the first part of this biomechanical in vitro study specimens from calf, pig and sheep and specimens from human donors were used to test a rigid and a dynamic pedicle screw system. In the second part, calf and human specimens were used to test an interspinous spacer. The aim was to more objectify the suitability of these animal species for pre-clinical flexibility tests with spinal implants. Whether these and other animal species may also be suitable to test other types of implants such as disc or nucleus prostheses in other types of experiments such as cyclic loading or fatigue tests should be the subject of future investigations.
The first implant type––the fixator––was implantable in the segment L1–2 in all three animal species, however, most easily into the calf. Using the pig, the prominent facet joints did not allow an ideal placement of the screws and rods while using the sheep the small pedicle diameter and vertebral body size was problematic. For the sheep even the smallest screws tended to be too large concerning both, length and diameter. From an anatomical point of view, the calf therefore proved to be a better model to test pedicle screw systems than the pig and the sheep. This observation probably also applies for the segments L2–3, L3–4 and L4–5 since these levels have the same main anatomical characteristics. Also, the three-dimensional flexibility is known to be very similar for all these levels [20, 22]. Therefore, if any of the segments L2–3, L3–4 or L4–5 would have been tested instead of L1–2, very similar differences and similarities between either of the three animals and the human would have been expected.
The calf also tended to be superior to pig and sheep concerning its flexibility in the intact and nucleotomised condition. Yet, even using the calf the intact ROM stayed overestimated except for flexion+extension while the effect of the nucleotomy stayed underestimated. In contrast, after implantation, in some cases the pig and in some the sheep was closer to the human. Thus, the above-mentioned problems with pedicle screw placement in the pig and the sheep did not seem to cause the biomechanical results to become less human-like than those obtained with the calf.
From a quantitative perspective, the three animal species and the human in some cases considerably differed. Similar results were reported by Riley et al. [15] who investigated the effect of various defects and implantation of an internal fixator with and without interbody graft on the flexibility of calf compared to human lumbar spine specimens. The authors found that, using the calf, in some cases the stabilising effect of the instrumentation was overestimated and in some underestimated.
The differences between the three animal species and the human were smaller for the rigid than for the dynamic fixator. This observation can be explained by the degree of flexibility allowed by the implant. The less flexibility it allows, the more load is transferred through the implant and the less the anatomical and functional characteristics of the segment play a role. Hence, in general, animal species may be more suitable to test the primary stabilising effect of rigid implants such as implants for spinal fusion than to test motion preserving implants such as dynamic fixators. However, differences concerning the magnitude of the implant’s effects on ROM still have to be expected.
The second implant type––the Coflex implant as a representative of interspinous implants––was also easily implantable into the calf lumbar spine segments L2–3 and L4–5. Yet, due to the larger gap between the calf spinous processes and their larger width even the largest implants tended to be too small. Nevertheless, the Coflex implant had still an acceptable fit.
Implantation of the Coflex implant caused the ROM to either increase in both species groups, or decrease in both of them. Effects in opposite directions, e.g., an increase in the calf but a decrease in humans, were not observed. Yet, quantitatively the ROM differed between calf and human. Also the statistical evaluation within each species group yielded different results. Thus, similar to the pedicle screw systems, general tendencies concerning the primary stabilising effect of an interspinous implant can be transferred from calf to human but neither the magnitude of this effect nor the statistical results.
The intradiscal pressure measurements carried out in the present study yielded smaller interindividual differences for the calf than for the human specimens. This was not surprising since the calf specimens all had healthy, not degenerated discs, which was not the case for the human specimens [2, 10]. Small interindividual differences are advantageous since implant-related trends such as the suppression of the pressure increase in extension with the Coflex implant can more clearly be depicted. Animal species with not degenerated discs therefore have the potential to even better depict the implant’s general effects on intradiscal pressure than the human.
Calf, pig and sheep are regularly used models to test spinal implants. However, the type of experiment preferably carried out varies from species to species. The calf is the species mainly used in vitro. Tests with pedicle screw systems are counted among these experiments [3, 4, 6, 9, 11, 17, 18]. According to the results of the present study, these experiments reveal the right trends but should not be interpreted quantitatively. So far, interspinous implants have not yet been tested using the calf or any other animal model. Yet, the present study indicates that the calf may well be used to reveal the general performance of this implant type. Similar to the calf, the pig is also often used in vitro. Both calf and pig are models used to measure IDP [1, 8, 12–14, 18]. These measurements reveal the implant’s general effects on intradiscal pressure expected in healthy human intervertebral discs but may differ from the human in magnitude. In contrast to the calf, the pig has additionally been used in numerous in vivo studies, which is also the case for the sheep. These in vivo studies often include biomechanical experiments after sacrifice of the animals using methods like those reported in the present study. From an anatomical point of view, however, implants developed for human use cannot always be used for the sheep or pig without modifications. Pedicle screws for example need to be shortened to fit the sheep vertebral dimensions and interspinous implants would need to be smaller in width for the pig. Only if the dimensions of the implant can be adapted to the anatomical dimensions of the respective animal model, successful implantation will be possible. The biomechanical performance of such an implant after a certain healing period, however, is difficult to predict from the data reported in this study since it also depends on the healing potential of the respective species.
In conclusion, the calf may be used to get a first idea of how a new lumbar pedicle screw system or interspinous implant tends to behave in flexibility tests concerning the parameters primary stability and intradiscal pressure. For pedicle screw systems the pig may be an alternative to the calf while the sheep seems to be too small for human implant sizes. However, neither from a quantitative nor from a statistical point of view the results are identical to those obtained with human specimens. Therefore, final pre-clinical experiments with pedicle screw systems focussing on primary or long-term flexibility or with insterspinous spacers focussing on primary stability or intradiscal pressure should only be carried out using human specimens. Overall, this study helps to plan in vitro experiments with transpedicular screw systems or interspinous spacers and to interpret all those in vitro animal studies already published on this topic.
References
Abe E, Nickel T, Buttermann GR, Lewis JL, Transfeldt EE (1999) The effect of spinal instrumentation on lumbar intradiscal pressure. Tohoku J Exp Med 187(3):237–247
Adams MA, Bogduk N, Burton K, Dolan P (2002) The biomechanics of back pain. Churchill Livingstone, Edinburgh
An HS, Singh K, Vaccaro AR, Wang G, Yoshida H, Eck J, McGrady L, Lim TH (2004) Biomechanical evaluation of contemporary posterior spinal internal fixation configurations in an unstable burst-fracture calf spine model: special references of hook configurations and pedicle screws. Spine 29(3):257–262
Brodke DS, Bachus KN, Mohr RA, Nguyen BK (2001) Segmental pedicle screw fixation or cross-links in multilevel lumbar constructs. A biomechanical analysis. Spine J 1(5):373–379
Cotterill PC, Kostuik JP, D’Angelo G, Fernie GR, Maki BE (1986) An anatomical comparison of the human and bovine thoracolumbar spine. J Orthop Res 4:298–303
Dick JC, Jones MP, Zdeblick TA, Kunz DN, Horton WC (1994) A biomechanical comparison evaluating the use of intermediate screws and cross-linkage in lumbar pedicle fixation. J Spinal Disord 7(5):402–407
Kettler A, Wilke HJ, Haid C, Claes L (2000) Effects of specimen length on the monosegmental motion behavior of the lumbar spine. Spine 25(5):543–550
Lee SH, Derby R, Chen Y, Seo KS, Kim MJ (2004) In vitro measurement of pressure in intervertebral discs and annulus fibrosus with and without annular tears during discography. Spine J 4(6):614–618
Lim TH, Kim JG, Fujiwara A, Yoon TT, Lee SC, Ha JW, An HS (2001) Biomechanical evaluation of diagonal fixation in pedicle screw instrumentation. Spine 26(22):2498–2503
McNally DS, Adams MA (1992) Internal intervertebral disc mechanics as revealed by stress profilometry. Spine 17(1):66–73
Nohara H, Kanaya F (2004) Biomechanical study of adjacent intervertebral motion after lumbar spinal fusion and flexible stabilization using polyethylene-terephthalate bands. J Spinal Disord Tech 17(3):215–219
Park C, Kim YJ, Lee CS, An K, Shin HJ, Lee CH, Kim CH, Shin JW (2005) An in vitro animal study of the biomechanical responses of anulus fibrosus with aging. Spine 30(10):E259–E265
Rao RD, David KS, Wang M (2005) Biomechanical changes at adjacent segments following anterior lumbar interbody fusion using tapered cages. Spine 30(24):2772–2776
Rao RD, Wang M, Singhal P, McGrady LM, Rao S (2002) Intradiscal pressure and kinematic behavior of lumbar spine after bilateral laminotomy and laminectomy. Spine J 2(5):320–326
Riley LH 3rd, Eck JC, Yoshida H, Koh YD, You JW, Lim TH (2004) A biomechanical comparison of calf versus cadaver lumbar spine models. Spine 29(11):E217–E220
Schmidt R, Richter M, Claes L, Puhl W, Wilke HJ (2005) Limitations of the cervical porcine spine in evaluating spinal implants in comparison with human cervical spinal segments: a biomechanical in vitro comparison of porcine and human cervical spine specimens with different instrumentation techniques. Spine 30(11):1275–1282
Scifert JL, Sairyo K, Goel VK, Grobler LJ, Grosland NM, Spratt KF, Chesmel KD (1999) Stability analysis of an enhanced load sharing posterior fixation device and its equivalent conventional device in a calf spine model. Spine 24(21):2206–2213
Sudo H, Oda I, Abumi K, Ito M, Kotani Y, Hojo Y, Minami A (2003) In vitro biomechanical effects of reconstruction on adjacent motion segment: comparison of aligned/kyphotic posterolateral fusion with aligned posterior lumbar interbody fusion/posterolateral fusion. J Neurosurg 99(2 Suppl):221–228
Wilke HJ, Claes L, Schmitt H, Wolf S (1994) A universal spine tester for in vitro experiments with muscle force simulation. Eur Spine J 3(2):91–97
Wilke HJ, Kettler A, Claes LE (1997) Are sheep spines a valid biomechanical model for human spines? Spine 22(20):2365–2374
Wilke HJ, Kettler A, Wenger KH, Claes LE (1997) Anatomy of the sheep spine and its comparison to the human spine. Anat Rec 247(4):542–555
Wilke HJ, Krischak ST, Wenger KH, Claes LE (1997) Load-displacement properties of the thoracolumbar calf spine: experimental results and comparison to known human data. Eur Spine J 6(2):129–137
Wilke HJ, Wenger K, Claes L (1998) Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J 7(2):148–154
Acknowledgments
This work was supported by AOSpine. The implants were provided by Ulrich medical (Ulm, Germany) and Paradigm Spine (Wurmlingen, Germany).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kettler, A., Liakos, L., Haegele, B. et al. Are the spines of calf, pig and sheep suitable models for pre-clinical implant tests?. Eur Spine J 16, 2186–2192 (2007). https://doi.org/10.1007/s00586-007-0485-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-007-0485-9