Abstract
Purpose
Postoperative delirium is one of the most common complications after cardiovascular surgery in older adults. Benzodiazepines are a reported risk factor for delirium; however, there are no studies investigating remimazolam, a novel anesthetic agent. Therefore, we prospectively investigated the effect of remimazolam on postoperative delirium.
Methods
We included elective cardiovascular surgery patients aged ≥ 65 years at Hamamatsu University Hospital between August 2020 and February 2022. Patients who received general anesthesia with remimazolam were compared with those who received other anesthetics (control group). The primary outcome was delirium within 5 days after surgery. Secondary outcomes were delirium during intensive care unit stay and hospitalization, total duration of delirium, subsyndromal delirium, and differences in the Mini-Mental State Examination scores from preoperative to postoperative days 2 and 5. To adjust for differences in the groups’ baseline covariates, we used stabilized inverse probability weighting as the primary analysis and propensity score matching as the sensitivity analysis.
Results
We enrolled 200 patients; 78 in the remimazolam group and 122 in the control group. After stabilized inverse probability weighting, 30.3% of the remimazolam group patients and 26.6% of the control group patients developed delirium within 5 days (risk difference, 3.8%; 95% confidence interval −11.5% to 19.1%; p = 0.63). The secondary outcomes did not differ significantly between the groups, and the sensitivity analysis results were similar to those for the primary analysis.
Conclusion
Remimazolam was not significantly associated with postoperative delirium when compared with other anesthetic agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Delirium in critically ill adult patients is associated with long-term cognitive dysfunction after discharge from the intensive care unit (ICU), and delirium is a leading cause of postintensive care syndrome (PICS) [1,2,3,4]. Patients with PICS, including those with cognitive impairment, experience increased mortality rates, higher medical costs, and more significant family burdens than those experienced by patients without PICS [4]. The risk of developing delirium after cardiovascular surgery in older adults aged ≥ 65 years is higher than that in younger patients [5, 6]. Furthermore, medical advances have increased the number of cardiac surgeries performed in older adults. Therefore, delirium is a critical issue in the field of intensive care.
The Pain, Agitation/Sedation, Delirium, Immobility, and Sleep disruption guideline and the American Geriatrics Society guideline have been published, and as part of their content, avoiding benzodiazepines is a critical message for delirium prevention [7, 8]. In addition, a recent network meta-analysis investigating pharmacological interventions to prevent delirium in critically ill patients suggested that benzodiazepines are associated with a higher risk of developing delirium [9]. Benzodiazepines are also associated with postoperative delirium and cognitive dysfunction when administered during cardiac surgery [10]. However, the benzodiazepines included in these reports were relatively long-acting drugs, such as midazolam, and the studies did not include short-acting drugs.
Remimazolam besilate is a novel anesthetic agent developed in Japan that is an ultra-short-acting benzodiazepine [11, 12]. Although the chemical structure of remimazolam is similar to that of midazolam, remimazolam is rapidly hydrolyzed by hepatic carboxylesterases [13, 14]. Remimazolam also has a higher clearance, smaller volume of distribution, and shorter half life than those of midazolam [15]. Although two randomized controlled trials examining delirium with remimazolam are ongoing, the results are not yet available [16, 17]. Therefore, we conducted a prospective observational study to investigate whether general anesthesia with remimazolam is associated with the development of postoperative delirium when compared with other anesthetic agents.
Methods
We conducted a prospective cohort study at Hamamatsu University Hospital (Shizuoka, Japan) between 13 August 2020 and 15 February 2022. The study was registered in the UMIN Clinical Trials Registry (registration number, UMIN000041316; principal investigator, Yoshitaka Aoki; date of registration, 12 August 2020). The study was approved by the Ethics Review Board of Hamamatsu University School of Medicine (approval number, 20–129; date of approval, 6 August 2020). Although this was an observational study, written informed consent was obtained from all participants because of the minor invasive nature of testing using the Mini-Mental State Examination (MMSE) [18], regardless of medical treatment. This study was conducted in accordance with the STROBE checklist and complied with the tenets of the Declaration of Helsinki 1964 and its later amendments. The present study involved the primary analysis of data, and the detailed analysis process was written after the data were accessed.
Patients
We assessed all consecutive patients aged ≥ 65 years who underwent elective cardiovascular surgery and who were admitted to the ICU postoperatively. The exclusion criteria were: (i) no written informed consent obtained from the patient; (ii) patients undergoing a second elective surgery during the same hospitalization; (iii) coma and seizures after surgery; (iv) alcohol withdrawal; and (v) patients with an MMSE score of ≤ 23 preoperatively. In addition, patients who met the following criteria were excluded from the analysis: (i) patients whose surgery was cancelled after inclusion; (ii) patients who could not be admitted to the ICU postoperatively; (iii) patients who refused to continue the study after surgery; and (iv) patients who had to be reoperated within 5 days postoperatively.
Exposures and comparisons
On the basis of the maintenance anesthetics during surgery, we classified the patients into two groups: patients who received remimazolam and those who did not (control group). Cases in which remimazolam was administered continuously were included in the remimazolam group, even if multiple maintenance anesthetics were administered (as a result, no case received remimazolam for a short time; all received remimazolam for the longest duration among the anesthetics). In the control group, the anesthetic agent administered for the longest duration was considered the primary maintenance anesthetic. Agents other than the primary maintenance anesthetic agent were considered concomitant anesthetics. Anesthetic agents administered as a bolus during induction of anesthesia were recorded.
Outcomes
The primary outcome was the development of delirium within 5 days after surgery. In the ICU, we used the Confusion Assessment Method for the ICU (CAM-ICU) and the Intensive Care Delirium Screening Checklist (ICDSC) to assess patient delirium [7]. A patient was considered to have developed delirium if the CAM-ICU was positive or the ICDSC score was ≥ 4. CAM-ICU and ICDSC were assessed by ICU nurses who were blinded to the groupings in this study. The CAM-ICU and ICDSC were first assessed when the patient entered the ICU and were reassessed approximately every 4–6 h, thereafter. After leaving the ICU, patients were assessed for delirium within 5 days postoperatively by physician interview and using the electronic medical record system [19,20,21]. In the interview, the following four items describing delirium elements were identified regarding CAM: acute onset and fluctuating course, inattention, disorganized thinking, and altered level of consciousness [22].
The secondary outcomes comprised the development of delirium within the ICU or during the hospital stay, total duration of delirium, development of subsyndromal delirium, and the difference in pre- vs. postoperative MMSE scores. After the fifth postoperative day, the presence of delirium was determined by evaluating the medical records only [19], and whether the patient developed delirium before the first discharge was determined. The total duration of delirium was defined as the time from the onset of delirium until the patient became CAM-ICU negative or the ICDSC score was ≤ 3 within 5 days postoperatively. If a patient had multiple episodes of delirium, the duration of each episode of delirium was totaled. Subsyndromal delirium was defined as an ICDSC score of 1–3 [7]. MMSE scores have been reported to be significantly lower on postoperative day 2 in patients with delirium than the scores in patients without delirium, with a trend toward recovery on postoperative day 5 [1]. Therefore, the MMSE was performed three times for each patient: before surgery, on postoperative day 2, and on postoperative day 5, and the differences between the preoperative value and each postoperative value were calculated.
Data collection and variables
The following variables were prospectively collected and compared between the groups regarding the background characteristics: age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) class, comorbidities, preoperative oral medication, preoperative MMSE score, living alone, type of surgery, cardiopulmonary bypass, and scheduled surgery time. BMI was categorized in accordance with the World Health Organization definitions as underweight (< 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥ 30 kg/m2). Because there are only a small number of obese patients with BMI > 30 kg/m2 in the Japanese population, overweight was defined as a BMI ≥ 25 kg/m2 in the analysis, in this study. Preoperative oral medication was investigated for the presence of benzodiazepines, statins, and beta-blockers, which may affect delirium [23]. The type of surgery was classified into three categories: cardiac surgery, endovascular surgery, and aortic aneurysm repair, in accordance with the Japanese Intensive PAtient Database (JIPAD) surgery codes (Online Resource 1) [24]. The following variables were described as intra- and postoperative factors: actual surgery time, actual anesthesia time, anesthesia induction drugs, primary maintenance anesthetics, concomitant maintenance anesthetics, the total amount of anesthetics and opioids, infusion volume, transfusion volume, urine volume, blood loss volume, intubated patients under sedation at ICU admission, the duration between ICU admission and extubation, and the lengths of ICU stay and hospital stay.
General anesthesia and patient management in the intensive care unit
All patients underwent general anesthesia with tracheal intubation in accordance with routine practice. Anesthetic induction and maintenance drugs were determined at the discretion of the attending anesthesiologist. The muscle relaxant was rocuronium, and continuous remifentanil was administered during surgery. All patients were monitored with electrocardiography, partial pressure of end-expiratory carbon dioxide, and arterial pressure by radial artery cannulation. Central venous catheters or Swan–Ganz catheters were inserted according to the case. Vasopressors (ephedrine, phenylephrine, and noradrenaline) were administered at the discretion of the anesthesiologist in charge. After surgery, whether the patient was extubated in the operating room or admitted to the ICU while intubated under sedation depended primarily on the type of surgery. Intraoperative events were also considered, and the final decision was based on the discussions between the cardiac surgeon and the anesthesiologist.
Standardized perioperative care, including preoperative and intraoperative care and postoperative pain control, was provided to all patients. In addition to delirium assessment using the CAM-ICU and ICDSC, pain assessment using a numerical rating scale and the Richmond agitation−sedation scale were performed in the ICU. Patients intubated under sedation at ICU admission were also assessed for delirium during intubation by maintaining light sedation. The intensivist determined the timing of extubation and ICU discharge. Pain management in the general ward was performed at the discretion of the cardiac surgeon.
Sample size calculation
The incidence of postoperative delirium after cardiac surgery has been reported to range from 11 to 46% [6], and we assumed a baseline incidence of 25% for postoperative delirium within 5 days, in this study. We considered a 15% difference in the incidence of postoperative delirium (primary outcome) to be a clinically significant increase and assumed a 40% incidence of delirium with remimazolam. Therefore, the number of patients with 80% power required to detect that difference at a level of p = 0.05 was calculated to be 152. We planned to prospectively enroll 200 patients, considering that some patients may meet the exclusion criteria after inclusion.
Statistical analysis
Categorical variables were reported as number and percentage, and continuous variables were reported as the mean and standard deviation. Chi-squared tests were used to compare the categorical variables, and continuous variables were analyzed using Student’s t test.
We used a propensity score method to adjust the baseline covariates between the remimazolam and control groups because numerous confounders collected prospectively would be difficult to adjust using a multivariate regression model owing to the number of outcomes. A logistic regression model was created to calculate the propensity scores for patients receiving remimazolam. The following variables were used to calculate the propensity score: age, sex, BMI category, ASA class, comorbidities, preoperative oral medication, preoperative MMSE score, living alone, type of surgery, cardiopulmonary bypass, and scheduled surgery time. For each variable, balances in baseline variables using absolute standardized differences were examined, and values ≥ 10% were considered unbalanced [25].
To maintain a predetermined sample size, stabilized inverse probability treatment weighting (IPTW) via the propensity score was used as the primary analysis. Stabilized IPTW is a propensity score-based method to adjust for measured potential confounding factors, and the method creates a pseudo-dataset by preserving the sample size [26]. Stabilized IPTW estimates the average treatment effects over a marginal distribution of measured covariates in the matched cohort [25]. Regarding the outcomes, we used a generalized linear model after stabilized IPTW and calculated the risk differences, 95% confidence intervals (CI), and p values. Two subgroup analyses were performed, one with three categories in accordance with the JIPAD surgery codes and the other with or without intraoperative cardiopulmonary bypass as the primary outcome. Two-sided p values of < 0.05 were considered significant.
Propensity score matching was used as a sensitivity analysis. In the sensitivity analysis, we performed one-to-one nearest-neighbor matching without replacement for estimated propensity scores using a caliper width set at 20% of the standard deviation of the propensity scores on the logit scale [27, 28]. All analyses were performed using Stata/BE 17 (StataCorp, College Station, TX, U.S.A.).
Results
Patient selection and characteristics
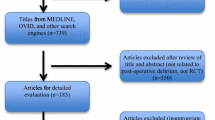
During the study period, 292 consecutive patients aged ≥ 65 years were assessed for eligibility, and 222 patients were included in the study. After excluding patients who met the exclusion criteria, 200 patients were included in the final analysis (Fig. 1). The patients were divided into the remimazolam group (n = 78) and the control group (n = 122). The primary maintenance anesthetics in the control group comprised propofol (n = 83), desflurane (n = 16), and sevoflurane (n = 23). In surgeries involving cardiopulmonary bypass (n = 114), the maintenance anesthetic during cardiopulmonary bypass was remimazolam in all cases in the remimazolam group (n = 37) and propofol in all cases in the control group (n = 77). No patients died in-hospital and none were censored during the study period.
Table 1 shows the patients’ baseline characteristics. Before adjusting using stabilized IPTW, the remimazolam group comprised higher percentages of underweight patients; patients with higher ASA class and undergoing endovascular surgery; and lower percentages of patients with hypertension, chronic kidney disease, cerebral infarction, smoking, alcohol use, β-blocker medication, cardiac and aortic aneurysm surgery, cardiopulmonary bypass, and shorter scheduled surgery time when comparing these data categories with those in the control group. After using stabilized IPTW, a pseudo-dataset comprising 200 patients (76 in the remimazolam group and 124 in the control group) was created, and all baseline characteristics were well balanced between the two groups. The C statistic was 0.72. The intra- and postoperative variables between the groups are shown in Online Resource 2.
Primary analysis (stabilized IPTW)
The proportions of patients who developed delirium within 5 days of surgery were 18/78 (23.1%) in the remimazolam group and 34/122 (27.9%) in the control group (Table 2). Table 3 shows the outcomes after adjustment by stabilized IPTW; the remimazolam group was not associated with increased delirium within 5 days of surgery when comparing the rate in the control group (remimazolam vs. control: 30.3% vs. 26.6%; risk difference, 3.8%; 95% CI −11.5 to 19.1; p = 0.63). Figure 2 shows that there were no significant differences in the results of the subgroup analyses. The development of delirium in the ICU and during the hospital stay, and the differences in MMSE scores from the preoperative measurement to the measurements on postoperative days 2 and 5 did not differ between the groups. In addition, the total duration of delirium and the rate of development of subsyndromal delirium did not differ significantly between the groups. Online Resource 3 shows the preoperative MMSE score and the scores on postoperative days 2 and 5 before and after stabilized IPTW.
Sensitivity analysis (propensity score matching)
In the sensitivity analysis using propensity score matching, both groups’ baseline characteristics were almost balanced (Online Resource 4). After one-to-one propensity score matching, delirium developed within 5 days of surgery in 16/61 (26.2%) patients in the remimazolam group and 17/61 (27.9%) patients in the control group, with no significant difference between the groups (risk difference −1.6%; 95% CI −17.4 to 14.1; p = 0.84). For all other secondary outcomes, the remimazolam group and control group did not differ significantly, similar to the primary analysis results (Online Resource 5).
Discussion
We showed that the use of remimazolam for general anesthesia in cardiovascular surgery was not associated with an increase in the rate of development of postoperative delirium with 5 days of surgery or in the ICU and during hospitalization when compared with the rates with general anesthesia with other anesthetics. Furthermore, the duration of delirium, the rate of development of subsyndromal delirium and the difference in pre- vs. postoperative days 2 and 5 MMSE scores did not differ between the groups. All results were robust in the sensitivity analysis.
To our knowledge, this is the first study to show that remimazolam is not associated with the development of postoperative delirium up to 5 days postoperatively, which is a novel finding that contradicts the conventional notion that benzodiazepines are associated with delirium [7,8,9]. The chemical structure of remimazolam is like that of midazolam, and its affinity for the significant subtypes of benzodiazepine receptors and its potentiation of chloride ion intracellular transfer are almost identical to those of midazolam [13, 14]. However, remimazolam has a side chain with an ester bond attached to the diazepine ring, which allows this drug to be rapidly hydrolyzed by carboxylesterases in the liver. The major metabolite of midazolam, α-hydroxymidazolam, is approximately one-eighth as potent as midazolam, and the affinity of remimazolam metabolites for the benzodiazepine receptor is only one four-hundredth that of remimazolam [13]. Therefore, remimazolam may act differently from classical benzodiazepines and may not be associated with long-term adverse effects, such as PICS, including postoperative delirium.
The most common basis for the diagnosis of delirium in the present study was physician interviews, followed by the ICDSC, and least commonly, the CAM-ICU. The CAM-ICU and ICDSC cannot fully diagnose patients with delirium in the ICU because these scoring systems were designed as screening tools [29]. Therefore, we attempted to compensate to improve the diagnostic performance for detecting delirium in the ICU by simultaneously assessing the CAM-ICU and ICDSC, and using CAM-based interviews and reviewing the electronic record systems in the general wards [19, 22]. The reason for the high proportion of a diagnosis of delirium on the basis of physician interviews may be because the ICDSC and CAM-ICU were evaluated during the ICU stay (average of approximately 40 h; Online Resource 2), whereas the physician interviews were conducted daily over 5 days.
With the increasing demand for sedation in critically ill patients and limited intravenous sedatives available to anesthesiologists, remimazolam deserves attention. Remimazolam has been adopted as a general anesthetic in some countries and as a sedative during other procedures [30]. Hypotension is considered a determinant of perioperative morbidity and mortality, and high-dose propofol sedation may be harmful [31]. Remimazolam has the advantages over propofol of having a more negligible hypotensive effect and an antagonist (flumazenil) [12, 30, 32]. Remimazolam can also be administered safely in patients with renal and hepatic impairment without the need for volume adjustment [33]. The finding in this study that remimazolam is not associated with increased delirium suggests that remimazolam may be a promising agent for sedation and general anesthesia in critically ill patients.
We acknowledge that this study has some limitations, although it has the strength of including dialysis patients and those who underwent endovascular surgery, which are patients who would be excluded in a randomized controlled trial, and the generalizability of the results is high. First, despite the study’s prospective enrollment, randomly assigning anesthetics as an interventional study was impossible. We initially planned a randomized controlled trial comparing remimazolam vs. propofol for cardiac surgery. However, most anesthesiologists disagreed with the study design, which was planned as an observational study. We also considered the European phase III randomized trial of remimazolam vs. propofol in cardiac surgery, which was terminated early owing to anesthesiologist opposition (28 of 530 planned patients were enrolled, and the trial was terminated) [34]. Second, over half of all patients received other concomitant anesthetics. Although intraoperative electroencephalographic monitoring was performed in this study, the optimal anesthetic depth for remimazolam is still unknown, and other anesthetic agents were combined with remimazolam for short periods to prevent intraoperative awakening. In addition, among the other benzodiazepines known to be associated with the risk of delirium, only midazolam was administered as the anesthetic induction drug. The number (%) of patients who received a single dose of midazolam differed significantly between the remimazolam and control groups (Online Resource 2). However, the administration of midazolam in this study was intermittent in all patients, and a large observational study reported that benzodiazepines were associated with an increased risk of delirium with continuous administration but not with intermittent administration [35]. Finally, we could not evaluate the outcomes in the present study at a fixed time of day. Human circadian rhythms influence delirium; therefore, ideally, the patients’ delirium and MMSE scores should be assessed at the same time of day [36].
Conclusions
This prospective observational study showed that continuous administration of remimazolam as a general anesthetic in patients aged ≥ 65 years undergoing elective cardiovascular surgery was not associated with an increased risk of postoperative delirium.
References
Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, Jones RN. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367:30–9.
Wolters AE, van Dijk D, Pasma W, Cremer OL, Looije MF, de Lange DW, Veldhuijzen DS, Slooter AJC. Long-term outcome of delirium during intensive care unit stay in survivors of critical illness: a prospective cohort study. Crit Care. 2014;18:R125.
van den Boogaard M, Schoonhoven L, Evers AWM, van der Hoeven JG, van Achterberg T, Pickkers P. Delirium in critically ill patients: impact on long-term health-related quality of life and cognitive functioning. Crit Care Med. 2012;40:112–8.
Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, Zawistowski C, Bemis-Dougherty A, Berney SC, Bienvenu OJ, Brady SL, Brodsky MB, Denehy L, Elliott D, Flatley C, Harabin AL, Jones C, Louis D, Meltzer W, Muldoon SR, Palmer JB, Perme C, Robinson M, Schmidt DM, Scruth E, Spill GR, Storey CP, Render M, Votto J, Harvey MA. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40:502–9.
Schenning KJ, Deiner SG. Postoperative delirium in the geriatric patient. Anesthesiol Clin. 2015;33:505–16.
Inouye SK, Westendorp RGJ, Saczynski JS. Delirium in elderly people. Lancet. 2014;383:911–22.
Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, Pandharipande PP, Watson PL, Weinhouse GL, Nunnally ME, Rochwerg B, Balas MC, van den Boogaard M, Bosma KJ, Brummel NE, Chanques G, Denehy L, Drouot X, Fraser GL, Harris JE, Joffe AM, Kho ME, Kress JP, Lanphere JA, McKinley S, Neufeld KJ, Pisani MA, Payen J-F, Pun BT, Puntillo KA, Riker RR, Robinson BRH, Shehabi Y, Szumita PM, Winkelman C, Centofanti JE, Price C, Nikayin S, Misak CJ, Flood PD, Kiedrowski K, Alhazzani W. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46:e825–73.
American Geriatrics Society Expert Panel on Postoperative Delirium in Older Adults. Postoperative delirium in older adults: best practice statement from the American Geriatrics Society. J Am Coll Surg. 2015;220:136-148.e1.
Burry LD, Cheng W, Williamson DR, Adhikari NK, Egerod I, Kanji S, Martin CM, Hutton B, Rose L. Pharmacological and non-pharmacological interventions to prevent delirium in critically ill patients: a systematic review and network meta-analysis. Intensive Care Med. 2021;47:943–60.
Rajaei M, Tabari M, Soltani G, Alizadeh K, Nazari A, Noroozian M, Morovatdar N. Comparison between the effects of dexmedetomidine and midazolam on postoperative cognitive impairment after coronary artery bypasses graft surgery: a randomized clinical trial. J Tehran Heart Cent. 2019;14:67–73.
Doi M, Hirata N, Suzuki T, Morisaki H, Morimatsu H, Sakamoto A. Safety and efficacy of remimazolam in induction and maintenance of general anesthesia in high-risk surgical patients (ASA Class III): results of a multicenter, randomized, double-blind, parallel-group comparative trial. J Anesth. 2020;34:491–501.
Doi M, Morita K, Takeda J, Sakamoto A, Yamakage M, Suzuki T. Efficacy and safety of remimazolam versus propofol for general anesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J Anesth. 2020;34:543–53.
Kilpatrick GJ, McIntyre MS, Cox RF, Stafford JA, Pacofsky GJ, Lovell GG, Wiard RP, Feldman PL, Collins H, Waszczak BL, Tilbrook GS. CNS 7056: a novel ultra-short-acting benzodiazepine. Anesthesiology. 2007;107:60–6.
Kilpatrick GJ. Remimazolam: non-clinical and clinical profile of a new sedative/anesthetic agent. Front Pharmacol. 2021;12: 690875.
Morimoto Y. Efficacy and safety profile of remimazolam for sedation in adults undergoing short surgical procedures. Ther Clin Risk Manag. 2022;18:95–100.
Yang M, Liu X, Yang D, Bai Y, Qin B, Tian S, Dong R, Song X. Effect of remimazolam besylate compared with propofol on the incidence of delirium after cardiac surgery: study protocol for a randomized trial. Trials. 2021;22:717.
Liu S, Su L, Zhang B, He H, Li Z, Li Q, Wang Q, Smith F, Long Y. The availability and safety study of remimazolam besylate for injection on sedation of ERAS patients under mechanical ventilation in ICU: protocol for a randomized, open-label, controlled trial. Front Med (Lausanne). 2021;8:
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Kuhn E, Du X, McGrath K, Coveney S, O’Regan N, Richardson S, Teodorczuk A, Allan L, Wilson D, Inouye SK, MacLullich AMJ, Meagher D, Brayne C, Timmons S, Davis D. Validation of a consensus method for identifying delirium from hospital records. PLoS ONE. 2014;9:e111823.
Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318:1161–74.
Saczynski JS, Kosar CM, Xu G, Puelle MR, Schmitt E, Jones RN, Marcantonio ER, Wong B, Isaza I, Inouye SK. A tale of two methods: chart and interview methods for identifying delirium. J Am Geriatr Soc. 2014;62:518–24.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–8.
Kassie GM, Nguyen TA, Kalisch Ellett LM, Pratt NL, Roughead EE. Preoperative medication use and postoperative delirium: a systematic review. BMC Geriatr. 2017;17:298.
Irie H, Okamoto H, Uchino S, Endo H, Uchida M, Kawasaki T, Kumasawa J, Tagami T, Shigemitsu H, Hashiba E, Aoki Y, Kurosawa H, Hatakeyama J, Ichihara N, Hashimoto S, Nishimura M, JIPAD Working Group in the Japanese Society of Intensive Care Medicine. The Japanese Intensive care PAtient Database (JIPAD): a national intensive care unit registry in Japan. J Crit Care. 2020;55:86–94.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46:399–424.
Xu S, Ross C, Raebel MA, Shetterly S, Blanchette C, Smith D. Use of stabilized inverse propensity scores as weights to directly estimate relative risk and its confidence intervals. Value Health. 2010;13:273–7.
Griswold ME, Localio AR, Mulrow C. Propensity score adjustment with multilevel data: setting your sites on decreasing selection bias. Ann Intern Med. 2010;152:393–5.
Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39:33–8.
Chen T-J, Chung Y-W, Chang H-CR, Chen P-Y, Wu C-R, Hsieh S-H, Chiu H-Y. Diagnostic accuracy of the CAM-ICU and ICDSC in detecting intensive care unit delirium: a bivariate meta-analysis. Int J Nurs Stud. 2021;113:103782.
Sneyd JR, Gambus PL, Rigby-Jones AE. Current status of perioperative hypnotics, role of benzodiazepines, and the case for remimazolam: a narrative review. Br J Anaesth. 2021;127:41–55.
Sneyd JR, Absalom AR, Barends CRM, Jones JB. Hypotension during propofol sedation for colonoscopy: an exploratory analysis. Br J Anaesth. 2021;S0007–0912(21):00731–5.
Dai G, Pei L, Duan F, Liao M, Zhang Y, Zhu M, Zhao Z, Zhang X. Safety and efficacy of remimazolam compared with propofol in induction of general anesthesia. Minerva Anestesiol. 2021;87:1073–9.
Stöhr T, Colin PJ, Ossig J, Pesic M, Borkett K, Winkle P, Struys MMRF, Schippers F. Pharmacokinetic properties of remimazolam in subjects with hepatic or renal impairment. Br J Anaesth. 2021;127:415–23.
Paion UK Ltd. A randomized, single-blind, propofol-controlled phase III study evaluating the efficacy and safety of remimazolam in general anesthesia in adult patients undergoing cardiac surgery, including follow-up sedation in the post-anesthesia care unit/intensive care unit [Internet]. clinicaltrials.gov; 2017 Aug. Report No.: NCT02523859. Available from: https://clinicaltrials.gov/ct2/show/NCT02523859
Zaal IJ, Devlin JW, Hazelbag M, Klein Klouwenberg PMC, van der Kooi AW, Ong DSY, Cremer OL, Groenwold RH, Slooter AJC. Benzodiazepine-associated delirium in critically ill adults. Intensive Care Med. 2015;41:2130–7.
Fitzgerald JM, Adamis D, Trzepacz PT, O’Regan N, Timmons S, Dunne C, Meagher DJ. Delirium: a disturbance of circadian integrity? Med Hypotheses. 2013;81:568–76.
Author information
Authors and Affiliations
Contributions
YA, TK, and MN provided substantial contributions to the study design, and RI, YS, and HM provided substantial contributions to patient recruitment and data acquisition. Statistical analysis was supported by MN, HK, MD, and YN. YA, TK, and MN contributed to manuscript writing, and RI, YS, HM, HK, MD, and YN contributed to manuscript revision. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Aoki, Y., Kurita, T., Nakajima, M. et al. Association between remimazolam and postoperative delirium in older adults undergoing elective cardiovascular surgery: a prospective cohort study. J Anesth 37, 13–22 (2023). https://doi.org/10.1007/s00540-022-03119-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-022-03119-7