Abstract
Background/aim
The appearance of anti-adalimumab antibodies (AAAs) is associated with low serum adalimumab (ADA) trough levels and a decrease of clinical response. The goal of this study was to assess the accuracy and clinical utility of new immunoassays for serum ADA and AAA levels.
Patients and methods
Serum ADA trough levels and AAA levels were measured using new immunoassays in 40 patients with Crohn’s disease (CD) receiving ADA maintenance therapy.
Results
Serum ADA trough levels were 12.3 ± 9.6 μg/ml (n = 40) in CD patients, and 14 of 40 patients (35 %) were positive for AAAs. A negative correlation was observed between serum AAA levels and ADA trough levels (y = −6.02x + 18.7, r = −0.54, P < 0.001, n = 40). The ROC (receiver-operator curve) analyses indicated that an ADA trough of 5.9 μg/ml was optimal to maintain negative CRP (C-reactive protein) levels (≤0.3 mg/dl). The ADA trough levels were significantly lower in patients positive for AAAs (5.5 ± 5.4 μg/ml, n = 14) than in patients negative for AAAs (16.0 ± 9.5 μg/ml, n = 26). The CRP and ESR levels were significantly higher in AAA-positive patients than in AAA-negative patients. Serum albumin levels were significantly lower in AAA-positive patients. The positive rate for AAAs in patients who lost a response to infliximab (50 %) was significantly higher than that of anti-TNF-α drug naïve patients (12.5 %).
Conclusions
These new assays for serum AAA trough and AAA levels are useful for routine clinical use and may help guide selection of optimal management strategies for IBD patients with a loss of response to ADA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumor necrosis factor (TNF)-α plays a pivotal role in the pathogenesis of inflammatory bowel disease (IBD), which includes both Crohn’s disease (CD) and ulcerative colitis (UC) [1–4]. The TNF-α is regarded as the major target molecule of monoclonal antibody therapy for IBD [5], and landmark trials and clinical studies have demonstrated that monoclonal antibodies against TNF-α, such as infliximab (IFX) and adalimumab (ADA), are effective for inducing and maintaining remission in patients with CD [1–3, 5–8].
The IFX is a chimeric monoclonal antibody composed of human constant and murine variable regions that specifically binds to TNF-α and neutralizes its biological activity [5, 9]. However, because of the immunogenicity of the murine protein composition, treatment with IFX sometimes causes the formation of antibodies to IFX (ATIs) that leads to infusion reactions, loss of clinical response and lower serum IFX concentrations [10–14]. Approximately 30 % of CD patients who respond to IFX require dose and interval adjustments to maintain their clinical response over the long term [6, 15–19], and the discontinuation of therapy due to a loss of response occurs in approximately 10 % of patients per year [6, 15–17]. Recent studies emphasize the importance of measuring serum IFX and ATI concentrations to predict the clinical efficacy of IFX [10, 13, 14, 20].
The ADA is a human monoclonal anti-TNF-α antibody and is effective in a broad population of CD patients who are naive to IFX or who show intolerance or a loss of response to IFX [21]. Since ADA is a fully human IgG, appearance rate of anti-ADA antibodies (AAAs) was initially considered to be less frequent than that of IFX [19, 20, 22, 23]. However, recent studies reported that AAAs developed in 2.6–38 % of patients treated for CD or rheumatoid arthritis [20, 24, 25], and that the appearance of AAAs is associated with low serum ADA trough concentrations and decreased clinical response [20, 24, 25]. Billioud et al. [26] showed that the mean percentage of loss of response to ADA was approximately 20 % per year, and that the annual risk of requirement for dose intensification was estimated to be 24.8 % per patient-year [26]. Karmiris et al. [20] demonstrated that the serum ADA trough concentration was lower in CD patients who discontinued therapy and that the concentration was affected by the presence of AAAs. Thus, measurement of serum ADA and AAA concentrations is required to understand the clinical status of a loss of response to ADA.
In previous studies, serum ADA concentrations were measured by the enzyme-linked immunosorbent assay (ELISA) based on the principle that ADA is captured via its ability to bind TNF-α [24, 25]. In order to distinguish specific ADA binding from non-specific binding of serum immunoglobulin (Ig)-G, ADA binding was detected by incubation with enzyme-labeled anti-ADA idiotype antibodies [24, 25]. The use of anti-ADA idiotype antibodies is ideal for specific detection of ADA, but they are not generally available and not suitable for routine clinical use. Therefore, the development of a more convenient method to assess serum ADA concentrations that does not require special materials is desired.
Most studies of anti-drug antibody formation use assays that are sensitive to drug interference, leading to false negative results for anti-drug antibody in the presence of a drug and an underestimation of the amount of anti-drug antibody formation [13, 27]. We have recently described an immunoassay for ATIs that can be used in the presence of free IFX [13]. The assay is based on acid dissociation of IFX-ATI complexes and allows for the measurement not only of ‘free’ or excess ATI, but also of so-called ‘complexed’ ATI in the presence of IFX. This approach was introduced to the measurement of AAAs in this study.
The present report describes a new ELISA system for measurement of serum ADA concentrations. In this system, non-specific binding of serum IgG was markedly blocked and did not require specific materials, such as anti-ADA idiotype antibodies. In addition, this study describes a novel immunoassay for AAAs that can measure AAAs in the presence of free ADA. These methods improved the diagnostic accuracy for measurement of serum ADA and AAA concentrations and might be useful for determination of the therapeutic approach for patients with a loss of response to ADA.
Materials and methods
Patients
This study enrolled 40 patients with CD who were receiving ADA maintenance therapy (regular 40 mg ADA injections every other week) at the Gastroenterology outpatient clinic at the Shiga University of Medical Science Hospital. Patient demographic/clinical characteristics are shown in Table 1. Blood samples from healthy volunteers (n = 50) were used as controls. The clinical activity was evaluated according to the Crohn’s disease activity index (CDAI) [28]. A CDAI < 150 was regarded as clinically inactive, and a CDAI ≥ 150 was regarded as active. In this study, the CDAI score was calculated in 20 patients due to stoma or missing data. The protocol of this study was approved by the Ethics Committee of the Shiga University of Medical Science.
The primary endpoint was determination of serum concentrations of ADA and AAA, and the secondary endpoint was association between serum ADA trough (and AAA) levels and clinical markers.
Labeling of recombinant human TNF-α and ADA
Recombinant human TNF-α (R&D systems, Minneapolis, MN) was biotinylated using a commercially available biotin-labeling kit (Dojindo Molecular Technologies Inc., Kumamoto, Japan). The ADA was labeled with horseradish peroxidase (HRP) using a commercially available HRP-conjugation kit (Solulink, San Diego, CA).
New ELISA for measurement of serum ADA concentrations
Blood samples were drawn at standardized time points just before the injection of ADA (trough serum concentration) with a 2 week interval. Serum ADA concentrations were measured by an ELISA system using avidin ELISA plate® (blocking-less type; Sumitomo Bakelite Co., Ltd, Tokyo, Japan). This plate is ready to use with a proprietary special coating to minimize non-specific protein binding. Phosphate-buffered saline (pH 7.4) containing 0.1 % Tween 20 was used for dilution. One hundred microlitre of biotinylated TNF-α (1.0 μg/ml) was added to the plate and incubated for 30 min. This process results in a tight immobilization of TNF-α to the plate surface via biotin–avidin interaction. After extensive washing, a further blocking procedure for non-specific protein binding was performed with incubation with 300 μl of Block Ace® (DS Pharma Biomedical, Co., Ltd., Suita, Japan). After washing, 100 μl of serum samples (×100 diluted) was added to the plate and incubated for 2 h at 4 °C. Immobilized TNF-α was recognized by ADA, and the reacted ADA was detected by HRP-labeled F(ab′)2 fragments of chicken anti-human IgG (×3,000 diluted; Thermo Fisher Scientific Co., Ltd, Waltham, MA). Color development was performed using 3,3′,5,5′-tetramethylbenzidine (TMB; Nacalai Tesque, Tokyo, Japan).
Measurement of serum AAA concentrations
We recently described a novel immunoassay for ATIs that enables measurement in the presence of IFX [13]. Based on this method, we developed an immunoassay for measuring AAAs that can be used in the presence of ADA. Briefly, immune complexes of ADA and AAA in samples were dissociated by treatment with 0.1 M glycine–HCl buffer (pH 2.7) and then immediately diluted with a carbonate-bicarbonate buffer (pH 9.6) at an IgG concentration of 20 μg/ml. Each well of a 96-well ELISA plate was coated with 200 μl of diluted IgG that contained the ATAs and allowed to incubate overnight. After extensive washing, 200 μl of HRP-conjugated ADA (0.4 μg/ml) was added and incubated for 30 min. Then, color development was performed using 3,3′,5,5′-tetramethylbenzidine. The values are reported in μg/ml-calibrated (μg/ml-c) on the basis of calibration standards made with affinity-purified polyclonal rabbit anti-human IgG (MP Biomedicals, LLC, Solon, OH).
Western blotting
The ADA was subjected to SDS-PAGE on a 4–20 % gradient gel under reducing conditions and then transferred electrophoretically onto a polyvinylidene difluoride (PVDF) membrane. Next, the membrane was incubated with IgG isolated from the patients’ serum that was subsequently labeled with HRP. Detection was performed using the ECL Western blotting system (GE Healthcare, Japan).
Statistical analyses
The association between two independent groups was calculated with the Chi square or Student’s t test when appropriate. A P value <0.05 was considered to be statistically significant. The diagnostic power of ADA levels was investigated by the area under the ROC (receiver-operator curve) analysis giving the AUC (area under the curve) with 95 % CI (confidence interval). The cut-off values for the ADA levels that maintained normal CRP (C-reactive protein) levels (≤0.3 mg/dl) were determined by identifying the point closest to the 1.0 angle. Using this cut-off value the number of patients below and above the cut-off was counted, and the odds ratios (ORs), sensitivity, specificity and likelihood ratios were calculated by Fisher’s exact test.
Results
Validation of newly developed ELISA for ADA
To confirm effective prevention of non-specific serum IgG binding, standard ADA samples adjusted by normal human serum to predetermined concentrations (0, 5, 10, 25 μg/ml) were subjected to the newly developed ELISA system. As shown in Fig. 1a, the measured ADA concentrations were approximately consistent with the predetermined concentrations, indicating that non-specific IgG binding was negligible in this system. If a standard ELISA plate was used instead of an avidin ELISA plate®, HRP-labeled anti-human IgG reacted with non-specifically bound serum IgG, leading to a marked overestimation of ADA levels (Fig. 1b). As shown in Fig. 1c, background levels determined by measurement of healthy individuals were 0.23 ± 0.15 μg/ml (mean ± SD, n = 50), and serum ADA trough levels in CD patients were 12.3 ± 9.6 μg/ml (n = 40).
Validation of the newly developed ELISA system for ADA. a To confirm the influence of non-specific binding of serum IgG, standard ADA samples were prepared using normal human serum (0, 5, 10, 25 μg/ml) and subjected to the newly developed ELISA system. The measured ADA concentrations were consistent with the prepared concentrations. Each point represents the mean of measured values (n = 50). b Blocking effects of the avidin-ELISA plate® used in this study. Use of a standard ELISA plate instead of an avidin-ELISA plate® leads to a marked overestimation of ADA levels due to non-specific IgG binding. Each point represents the mean of measured values (85 samples from 40 patients). c Serum ADA trough levels in CD patients. The assay background levels in healthy individuals were 0.23 ± 0.15 μg/ml (mean ± SD, n = 50), and serum ADA trough levels in CD patients were 12.3 ± 9.6 μg/ml (n = 40)
Fixed dosage of ADA (40 mg/body) suggested an association of serum ADA levels with body weight. However, serum ADA trough levels were not associated with body weight (r = −0.098, n = 40).
Immunoassay for AAAs
Next, serum AAA levels were measured using the novel immunoassay. This assay was constructed according to the recently developed method for ATIs in our laboratory [13], which allows measurement of AAA levels in the presence of free ADA. As shown in Fig. 2a, measured values of healthy controls (n = 50) were 0.44 ± 0.23 μg/ml-c, and the cutoff value was determined as 1.12 μg/ml-c (mean + 3SD). Therefore, the AAAs were reported as positive when the concentration was more than 1.12 μg/ml-c. Fourteen of 40 CD patients (35 %) receiving ADA maintenance therapy were positive for AAAs.
Serum AAA levels in CD patients. a Serum AAA levels were measured by the newly developed immunoassay. The measured values of healthy controls (n = 50) were 0.44 ± 0.23 μg/ml-c, and the cutoff value for a positive result was determined as 1.12 μg/ml-c (mean + 3SD of healthy controls). Fourteen of 40 CD patients (35 %) were positive for AAAs. b Western blotting analysis to confirm the presence of AAAs. The IgG fraction of the patients who were positive for AAA by immunoassay was isolated by a protein G column, eluted by an acidic buffer and neutralized. The eluted IgG was labeled with HRP, and then used for the detection of ADA transferred onto a PVDF membrane
Western blotting analysis was performed to confirm the presence of AAAs in the samples that were diagnosed as positive for AAA by the current immunoassay (Fig. 2b). Since the binding sites of the AAAs to ADA were occupied by coexisting free ADA, the ADA–AAA immune complexes were dissociated by treatment with acidic buffer. Sample IgGs were isolated by a protein G column, eluted by an acidic buffer and neutralized. The eluted IgG was labeled with HRP and then used for the detection of ADA transferred onto a nitrocellulose membrane. As shown in Fig. 2b, ADA was clearly detected by IgG isolated from the patients’ serum that was subsequently labeled with HRP, and this was completely blocked by the presence of ADA, indicating that the AAAs were actually present in the AAA-positive sample determined using the current method.
Negative correlation between serum AAA levels and ADA trough levels
The AAA levels and ADA trough levels were plotted with CRP levels (CRP cutoff, 0.3 mg/dl) (Fig. 3a). A negative and significant correlation was observed between serum AAA levels and ADA trough levels (y = −6.02x + 18.7, r = −0.54, P < 0.001, n = 40). Ten (71 %) of the 14 patients who were positive for AAAs also had positive CRP levels (≥0.3 mg/dl), whereas five (19 %) of the 26 patients who were negative for AAAs had positive CRP levels. As shown in Fig. 3b, ADA trough levels were significantly lower in patients positive for AAAs (5.5 ± 5.4 μg/ml, n = 14) than in patients negative for AAAs (16.0 ± 9.5 μg/ml, n = 26).
Relationship between serum AAA levels and ADA trough levels. a Association of serum AAA levels with ADA trough levels. A negative correlation was observed between serum AAA and ADA trough levels (y = −6.02x + 18.7, r = −0.54, P < 0.001, n = 40). b Serum ADA trough levels in AAA positive and negative patients. ADA trough levels were significantly lower in the patients positive for AAAs (5.5 ± 5.4 μg/ml, n = 14) than in the patients negative for AAAs (16.0 ± 9.5 μg/ml, n = 26)
The ROC and AUC analyses showed that the clinical utility of ADA trough levels for identifying CRP ≤ 0.3 mg/dl was 83 %, and the odds ratio (OR) was 23.0 (95 % CI (confidence interval) 3.4–28.1) (Table 2). The cutoff value for identifying CRP ≤ 0.3 mg/dl was determined as an ADA of 5.9 μg/ml using the ROC curve.
Relationship between clinical markers and ADA trough levels
As shown in Fig. 4a and b, CRP and ESR (erythrocyte sedimentation rate) levels significantly elevated in CD patients with ADA trough levels <5.9 μg/ml when compared with patients with ADA trough levels ≥5.9 μg/ml. In contrast, serum albumin levels were significantly lower in patients with ADA trough levels <5.9 μg/ml than in patients with ADA trough levels ≥5.9 μg/ml (Fig. 4c). A negative, but significant, correlation was found between ADA trough levels and CRP levels and between ADA trough levels and ESR levels (Fig. 4d, e). A weak and positive correlation was observed between ADA trough levels and serum albumin levels (Fig. 4f).
Serum ADA trough levels and clinical markers. a, b Serum CRP and ESR were significantly lower in patients with ADA trough levels ≥5.9 μg/ml than in patients with ADA trough levels <5.9 μg/ml. c Serum albumin levels were significantly higher in patients with ADA trough levels ≥5.9 μg/ml than in patients with ADA trough levels <5.9 μg/ml. d–f Serum CRP and ESR negatively correlated with ADA trough levels, but serum albumin levels tended to correlate positively with ADA trough levels
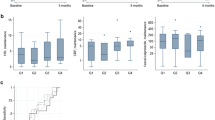
Serum trough ADA levels were significantly elevated in patients with inactive disease (CDAI < 150) compared to those with active disease (CDAI ≥ 150) (supplement Fig. 1A). However, concomitant thiopurine treatment did not affect serum ADA levels [thiopurine group 11.1 ± 8.0 μg/ml (mean ± SD, n = 17) vs. non-thiopurine group 13.1 ± 10.8 μg/ml (n = 23); not significant] (supplement Fig. 2A).
Relationship between clinical markers and AAA levels
As shown in Fig. 5a and b, CRP and ESR levels were significantly higher in AAA-positive patients than in AAA-negative patients. Serum albumin levels were significantly lower in AAA-positive patients than in AAA-negative patients (Fig. 5c). A negative correlation was observed between AAA levels and CRP levels and between AAA levels and ESR levels (Fig. 5d, e). A weak and negative correlation was seen between AAA levels and serum albumin levels (Fig. 5f).
Serum AAA levels and clinical markers. a, b Serum CRP and ESR were significantly higher in patients positive for AAA than in patients negative for AAA. c Serum albumin levels were significantly lower in patients positive for AAA than in patients negative for AAA. d–f Serum CRP and ESR correlated positively with AAA levels, but serum albumin levels tended to correlate negatively with AAA levels
Serum AAA levels were significantly elevated in patients with active disease (CDAI ≥ 150) compared to those with inactive disease (CDAI < 150) (supplement Fig. 1B). However, concomitant thiopurine treatment did not affect serum AAA levels [thiopurine group 1.3 ± 0.9 μg/ml-c (mean ± SD, n = 17) vs. non-thiopurine group 0.91 ± 0.8 μg/ml-c (n = 23); not significant] (supplement Fig. 2B).
Effects of pretreatment with IFX on serum AAA and ADA trough levels
This study included two types of CD patients: the first was anti-TNF-α drug naïve patients (n = 16) and the second was patients who experienced loss of response to IFX and had their drug switched to ADA (n = 24). All patients who lost their response to IFX were positive for ATIs, as determined by the method developed in our laboratory [13]. Serum AAA levels were significantly higher in patients who lost their response to IFX than in the anti-TNF-α drug naïve patients (Fig. 6a). The positive rate for AAAs (levels ≥1.12 μg/ml-c) in patients who lost their response to IFX (12 out of 24, 50 %) was significantly higher than that of anti-TNF-α drug naïve patients (2 out of 16, 12.5 %). In contrast, serum ADA trough levels were significantly higher in anti-TNF-α drug naïve patients than in patients who lost their response to IFX (Fig. 6b). The CRP levels were significantly higher in patients who lost their response to IFX (Fig. 6c). These results indicate a high risk of development of AAAs in patients who experienced a loss of response to IFX.
Preceding IFX treatment affects serum AAA and ADA trough levels. a Serum AAA levels were significantly higher in patients who experienced IFX therapy than in anti-TNF-α drug naïve patients. Twelve out of 24 patients who experienced IFX therapy (50 %) and 2 out of 16 anti-TNF-α drug naïve patients (12.5 %) were positive for AAA. b ADA trough levels were significantly higher in anti-TNF-α drug naïve patients than in patients who experienced IFX therapy. c CRP levels were significantly higher in patients who received IFX therapy than in anti-TNF-α drug naïve patients
Discussion
This study investigated whether newly developed methods for measurement of serum ADA and AAA concentrations are suitable for routine clinical use. The benefits of current methods are high throughput, relatively low cost, and no need for special materials, such as radioisotopes or anti-ADA idiotype antibodies.
Adalimumab is a powerful therapeutic tool for patients with CD. The initial response rate to ADA has been reported to be 70–80 % in CD [29–31], but a substantial proportion of patients (up to 40 %) will subsequently lose their response [26, 32]. Management strategies for patients with a loss of response to ADA include dose escalation or a shortening of the injection interval [26, 32]. In such cases, routine measurements for serum trough ADA and AAA levels would be helpful to optimize management of the disease.
Standard ELISAs are useful for measurement of serum concentrations of anti-TNF-α drugs. For example, IFXs in samples are captured by TNF-α that is immobilized on the surface of plastic ELISA plates, and trapped IFXs are detected by the enzyme-labeled anti-mouse IgG that recognizes the murine variable region of IFX. On the other hand, ELISA for ADA is more complicated, since non-specific binding of serum IgG interferes with selective detection of ADA. In previous studies, enzyme-labeled anti-ADA idiotype antibodies were used as a detection antibody to discriminate captured ADA from non-specific binding of serum IgG [24, 25]. The use of anti-ADA idiotype antibodies is ideal for the specific detection of ADA, but they are not available in most laboratories. Our method is based on a concept of thorough blocking of non-specific binding of serum IgG using a commercially available special ELISA plate, and this enables the use of enzyme-labeled anti-human IgG antibodies as a detection antibody. As shown in Fig. 1, the presence of serum IgG did not interfere with ADA measurement, and the background values in control serum from healthy individuals were negligible. The measured values of serum ADA trough levels were approximately consistent with those measured by the ELISA using anti-ADA idiotype antibodies [20, 25].
Commercially available kits for measurement of anti-TNF-α drug antibodies levels are based on a two-site ELISA in which the drug is used for both capture and detection [13, 33]. The two-site ELISA consists of binding the anti-TNF-α drug to a plastic ELISA plate, adding patient serum and then detection using an enzyme-labeled form of the anti-TNF-α drug. However, the detection of the anti-drug antibodies is affected by the presence of the drug itself. Indeed, the presence of the drug in a sample that contains anti-drug antibodies can result in immune complex formation that interferes with in vitro detection [13]. Therefore, it is likely that the levels of anti-drug antibodies are underestimated as they may be detected only if the concentration of antibody exceeds that of the drug in the serum [13]. The current immunoassay for AAAs includes a critical step of acidic buffer treatment of the ADA–AAA immune complexes trapped by the protein G-beads [13]. This process dissociates ADA and AAA complexes and effectively recovers the binding capacity of ADA to TNF-α [13]. The cutoff value of AAAs was determined as 1.12 μg/ml-c based on the results for healthy individuals, and 35 % (14 of 40 patients) of CD patients on ADA maintenance therapy were positive for AAAs.
Recent studies have investigated the clinical utility of CRP levels as a predictor of endoscopic and disease activities of CD. Normalized CRP levels were associated with endoscopic improvement and healing [31], and normalized CRP levels after initiation of IFX predicted better long-term outcome [16]. Based on these observations, we evaluated the relationship between serum ADA trough levels and AAA levels using normal CRP values (≤0.3 mg/dl). In accordance with previous studies [20, 25], CD patients who were positive for AAAs (≥1.12 μg/ml-c) had significantly lower serum ADA trough levels when compared with patients who were negative for AAAs. Similarly, inflammatory markers (e.g., CRP, ESR) were significantly higher and serum albumin levels were significantly lower in patients who were positive for AAAs. The ROC and AUC analyses revealed that an ADA trough cutoff level of 5.9 μg/ml was optimal for reflection of normalized CRP levels. Significant improvements of ESR and serum albumin levels were also observed in patients with high ADA trough levels (≥5.9 μg/ml). Thus, an ADA trough cutoff level of 5.9 μg/ml may be optimal as an indicator of preserved response to ADA.
As shown in Fig. 3, the majority of patients (19 of 22) who were negative for AAAs (<1.12 μg/ml-c) and who had high ADA trough levels (≥5.9 μg/ml) revealed normal CRP levels (≤0.3 mg/dl), indicating a well-controlled condition in response to ADA treatment. The patients who were negative for AAAs, but who had low ADA trough levels (<5.9 μg/ml) and positive CRP levels, may need more intensive ADA strategies (e.g., dose-escalation, shortening of the injection interval). In these patients, rapid turnover of ADA due to increased consumption could be suspected. All patients who were positive for AAAs and had low ADA trough levels (n = 8) were positive for CRP (levels >0.3 mg/dl), suggesting that active neutralization of ADA by AAAs caused the loss of response to ADA. For these patients, a shift to other biologics as well as intensification of ADA therapy was recommended. Some patients (four of six) who were positive for AAAs, but maintained high ADA trough levels (≥5.9 μg/ml), were negative for CRP. In these patients, AAAs may possess only binding capacity against ADA without neutralizing activity. Alternatively, TNF-α may not play a role in the pathophysiology of these patients.
A previous study on rheumatoid arthritis reported that ADA is more effective for anti-TNF-α drug naïve patients compared to anti-TNF-α experienced patients [34]. However, it is unclear how previous IFX therapy affects immunologic and clinical responses subsequent to ADA therapy in CD patients. We compared serum AAA and ADA trough levels between patients who experienced IFX therapy and patients who were naïve to anti-TNF-α drugs. As shown in Fig. 6, serum AAA levels were significantly higher in patients who experienced IFX therapy than in anti-TNF-α drug naïve patients, and the rate of AAA-positivity was 50 % in IFX-experienced patients and 12.5 % in anti-TNF-α drug naïve patients. These data suggest a high risk of development of AAAs in patients who experienced IFX therapy. This notion is supported by the findings of lower ADA trough levels and higher CRP levels in patients who experienced IFX therapy. The molecular mechanisms underlying easy development of AAAs in IFX-experienced patients are unclear, but the possibility of immunologic cross reaction of antibodies against IFX and ADA should be investigated in the future.
In conclusion, this study is the first to develop an improved immunoassay for the accurate measurement of ADA trough and AAA levels without special materials. The methods described here will help facilitate decision-making in terms of optimal use of ADA therapy for CD patients. Further investigation of the clinical utility of these methods in a large number of IBD patients would be of benefit.
References
Danese S, Colombel JF, Reinisch W, et al. Review article: infliximab for Crohn’s disease treatment—shifting therapeutic strategies after 10 years of clinical experience. Aliment Pharmacol Ther. 2011;33:857–69.
Mayer L. Evolving paradigms in the pathogenesis of IBD. J Gastroenterol. 2010;45:9–16.
Hanauer SB, Kornbluth AA, Messick J, et al. Clinical scenarios in IBD: optimizing the use of conventional and biologic agents. Inflamm Bowel Dis. 2010;16(Suppl 1):S1–11.
Andoh A, Kuzuoka H, Tsujikawa T, et al. Multicenter analysis of fecal microbiota profiles in Japanese patients with Crohn’s disease. J Gastroenterol. 2012;47:1298–307.
Allez M, Vermeire S, Mozziconacci N, et al. The efficacy and safety of a third anti-TNF monoclonal antibody in Crohn’s disease after failure of two other anti-TNF antibodies. Aliment Pharmacol Ther. 2010;31:92–101.
Hanauer SB, Feagan BG, Lichtenstein GR, et al. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. Lancet. 2002;359:1541–9.
Colombel JF, Sandborn WJ, Rutgeerts P, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn’s disease: the CHARM trial. Gastroenterology. 2007;132:52–65.
Ueno F, Matsui T, Matsumoto T, et al. Evidence-based clinical practice guidelines for Crohn’s disease, integrated with formal consensus of experts in Japan. J Gastroenterol. 2013;48:31–72.
D’Haens GR, Panaccione R, Higgins PD, et al. The London Position Statement of the World Congress of Gastroenterology on Biological Therapy for IBD with the European Crohn’s and Colitis Organization: when to start, when to stop, which drug to choose, and how to predict response? Am J Gastroenterol. 2011;106:199–212. quiz 213.
Cassinotti A, Travis S. Incidence and clinical significance of immunogenicity to infliximab in Crohn’s disease: a critical systematic review. Inflamm Bowel Dis. 2009;15:1264–75.
Hanauer SB, Wagner CL, Bala M, et al. Incidence and importance of antibody responses to infliximab after maintenance or episodic treatment in Crohn’s disease. Clin Gastroenterol Hepatol. 2004;2:542–53.
Vermeire S, Noman M, Van Assche G, et al. Effectiveness of concomitant immunosuppressive therapy in suppressing the formation of antibodies to infliximab in Crohn’s disease. Gut. 2007;56:1226–31.
Imaeda H, Andoh A, Fujiyama Y. Development of a new immunoassay for the accurate determination of anti-infliximab antibodies in inflammatory bowel disease. J Gastroenterol. 2012;47:136–43.
Nanda KS, Cheifetz AS, Moss AC. Impact of antibodies to infliximab on clinical outcomes and serum infliximab levels in patients with inflammatory bowel disease (IBD): a meta-analysis. Am J Gastroenterol. 2012;108(1):40–7.
Sands BE, Anderson FH, Bernstein CN, et al. Infliximab maintenance therapy for fistulizing Crohn’s disease. N Engl J Med. 2004;350:876–85.
Schnitzler F, Fidder H, Ferrante M, et al. Long-term outcome of treatment with infliximab in 614 patients with Crohn’s disease: results from a single-centre cohort. Gut. 2009;58:492–500.
Van Assche G, Magdelaine-Beuzelin C, D’Haens G, et al. Withdrawal of immunosuppression in Crohn’s disease treated with scheduled infliximab maintenance: a randomized trial. Gastroenterology. 2008;134:1861–8.
Gisbert JP, Panes J. Loss of response and requirement of infliximab dose intensification in Crohn’s disease: a review. Am J Gastroenterol. 2009;104:760–7.
Yanai H, Hanauer SB. Assessing response and loss of response to biological therapies in IBD. Am J Gastroenterol. 2011;106:685–98.
Karmiris K, Paintaud G, Noman M, et al. Influence of trough serum levels and immunogenicity on long-term outcome of adalimumab therapy in Crohn’s disease. Gastroenterology. 2009;137:1628–40.
Sandborn WJ, Rutgeerts P, Enns R, et al. Adalimumab induction therapy for Crohn disease previously treated with infliximab: a randomized trial. Ann Intern Med. 2007;146:829–38.
West RL, Zelinkova Z, Wolbink GJ, et al. Immunogenicity negatively influences the outcome of adalimumab treatment in Crohn’s disease. Aliment Pharmacol Ther. 2008;28:1122–6.
Chaparro M, Guerra I, Munoz-Linares P, et al. Systematic review: antibodies and anti-TNF-alpha levels in inflammatory bowel disease. Aliment Pharmacol Ther. 2012. doi:10.1111/j.1365-2036.2012.05057.x.
Bartelds GM, Wijbrandts CA, Nurmohamed MT, et al. Clinical response to adalimumab: relationship to anti-adalimumab antibodies and serum adalimumab concentrations in rheumatoid arthritis. Ann Rheum Dis. 2007;66:921–6.
Bartelds GM, Krieckaert CL, Nurmohamed MT, et al. Development of antidrug antibodies against adalimumab and association with disease activity and treatment failure during long-term follow-up. JAMA. 2011;305:1460–8.
Billioud V, Sandborn WJ, Peyrin-Biroulet L. Loss of response and need for adalimumab dose intensification in Crohn’s disease: a systematic review. Am J Gastroenterol. 2011;106:674–84.
van Schouwenburg PA, Krieckaert CL, Rispens T, et al. Long-term measurement of anti-adalimumab using pH-shift-anti-idiotype antigen binding test shows predictive value and transient antibody formation. Ann Rheum Dis. 2013 [Epub ahead of print].
Best WR, Becktel JM, Singleton JW, et al. Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology. 1976;70:439–44.
Sprakes MB, Hamlin PJ, Warren L, et al. Adalimumab as second line anti-tumour necrosis factor alpha therapy for Crohn’s disease: a single centre experience. J Crohns Colitis. 2011;5:324–31.
Orlando A, Renna S, Mocciaro F, et al. Adalimumab in steroid-dependent Crohn’s disease patients: prognostic factors for clinical benefit. Inflamm Bowel Dis. 2012;18:826–31.
Kiss LS, Szamosi T, Molnar T, et al. Early clinical remission and normalisation of CRP are the strongest predictors of efficacy, mucosal healing and dose escalation during the first year of adalimumab therapy in Crohn’s disease. Aliment Pharmacol Ther. 2011;34:911–22.
Sandborn WJ, Colombel JF, Schreiber S, et al. Dosage adjustment during long-term adalimumab treatment for Crohn’s disease: clinical efficacy and pharmacoeconomics. Inflamm Bowel Dis. 2011;17:141–51.
Afif W, Loftus EV Jr, Faubion WA, et al. Clinical utility of measuring infliximab and human anti-chimeric antibody concentrations in patients with inflammatory bowel disease. Am J Gastroenterol. 2010;105:1133–9.
Bartelds GM, Wijbrandts CA, Nurmohamed MT, et al. Anti-adalimumab antibodies in rheumatoid arthritis patients are associated with interleukin-10 gene polymorphisms. Arthritis Rheum. 2009;60:2541–2.
Acknowledgments
This study was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (21590809) and by the Health and Labour Sciences Research Grants for Research on Intractable Diseases from the Ministry of Health, Labour and Welfare of Japan.
Conflict of interest
The authors have declared that no conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Imaeda, H., Takahashi, K., Fujimoto, T. et al. Clinical utility of newly developed immunoassays for serum concentrations of adalimumab and anti-adalimumab antibodies in patients with Crohn’s disease. J Gastroenterol 49, 100–109 (2014). https://doi.org/10.1007/s00535-013-0803-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-013-0803-4