Abstract
Background
The renin-angiotensin system plays an important role in hepatic fibrosis and portal hypertension. We evaluated the long-term effects of olmesartan, an angiotensin type 1 (AT1) receptor blocker, on hemodynamics and liver fibrosis.
Methods
Forty-eight selected patients with cirrhosis were randomly divided into two groups of 24 patients each, those who received and those who did not receive olmesartan treatment for 1 year. Hepatic hemodynamic studies, and measurements of transforming growth factor-beta1 (TGF-beta1) and blood markers of hepatic fibrosis, including serum hyaluronic acid (HA), type IV collagen, and procollagen III N-terminal propeptide levels, were also performed at the beginning and end of the study.
Results
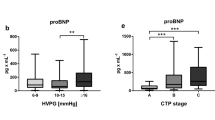
The median dose of the final drug administration was 20 mg (range 10–40 mg). Olmesartan reduced the hepatic venous pressure gradient (HVPG) by −12.9 ± 9.1% (p = 0.035) after 1 year. No significant changes were seen in controls. Six of the 24 patients (25%) in the olmesartan group showed a >20% reduction of HVPG from baseline values. TGF-beta1 was significantly decreased in patients who received olmesartan (7.0 ± 8.2 vs. 3.1 ± 1.6 ng/mL, p = 0.046) but there was no decrease in the controls. A significant trend was shown by correlating HA and TGF-beta1 variations in cirrhosis patients (p = 0.018, r = 0.377). Fibrosis markers were unchanged at the end of the study in both groups.
Conclusions
Olmesartan induced a mild reduction of portal pressure and TGF-beta1 for 1 year, but did not suppress hepatic fibrosis markers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Angiotensin II (Ang II), the main peptide of the renin–angiotensin system (RAS) regulates cell growth, inflammation, and fibrosis, and contributes to the progression of injury of various organs through angiotensin type 1 (AT1) receptors [1]. The profibrogenic effect of Ang II is associated with an increased concentration of transforming growth factor-beta1 (TGF-beta1) [2]. Induction of TGF-beta1 by Ang II stimulates the synthesis of matrix proteins, inhibits matrix degradation, and enhances the expression of integration that facilitates matrix assembly [3].
In the liver, the RAS is also involved in chronic inflammation and fibrosis. TGF-beta1 produced from Kupffer cells and infiltrating inflammatory cells activates hepatic stellate cells (HSCs) [4]. AT1 receptors are expressed on activated HSCs, and Ang II enhances hepatic fibrosis through the production of TGF-beta1 in animal models [1]. Previous studies have suggested that RAS inhibitors might diminish the progression of fibrosis in patients with noncirrhotic hepatitis C and nonalcoholic steatohepatitis (NASH) [5, 6].
Recently, Debernardi-Venon et al. [7] reported that, in selected cirrhotic patients, the AT1 receptor antagonist candesartan cilexetil (candesartan) was effective in reducing portal pressure and liver fibrosis markers after 1 year. In their study, the hepatic venous pressure gradient (HVPG) decreased significantly in patients treated with a different AT1 receptor antagonist, olmesartan (−8.4 ± 2.4%), with a reduction of >20% in 25% of the treated patients vs. 5.6 ± 2.9% in the untreated patients. Of note, in candesartan-treated patients, hyaluronic acid (HA) levels were decreased significantly, but only in those in whom HVPG was reduced. However, in other studies of candesartan, TGF-beta1, which is a key cytokine for liver fibrosis, was not significantly decreased, although angiotensin receptor blockers (ARBs) significantly attenuate tissue fibrosis by suppressing TGF-beta1 mRNA [8–11].
Olmesartan medoxomil (olmesartan) is a comparatively new ARB [12], and the active metabolite olmesartan has been demonstrated to be a potent, selective ARB [13]. Oparil et al. [13] reported that olmesartan was more effective than the other ARBs tested in reducing cuff diastolic blood pressure in patients with essential hypertension in a multicenter, randomized, double-blind trial. Therefore, this agent may possibly elicit a better outcome for portal hypertension and antifibrosis than the other ARBs. The aim of the present study was to investigate the effect of olmesartan on portal pressure and liver fibrosis in patients with cirrhosis.
Patients, materials, and methods
Patients
A prospective randomized study was conducted in patients with either biopsy-proven liver cirrhosis, or clinically evident liver cirrhosis, who were recruited from the Kitasato University East Hospital, Sagamihara, Japan. Forty-eight selected patients with cirrhosis were randomly divided into two groups of 24 patients each, those who received and those who did not receive olmesartan treatment for 1 year. The final protocol was approved by the Ethics Committee of the Kitasato University of Sagamihara, Japan (C-Ethics Committee, ID 07-365). The study was conducted following the principles of the Declaration of Helsinki. After providing written informed consent, patients with the following inclusion criteria, and none of the exclusion criteria, agreed to participate in the study, from May 2007 to October 2008.
The inclusion criteria were: (1) age between 18 and 75 years; (2) proven liver cirrhosis with a diagnosis based on histology or unequivocal clinical, sonographic, and laboratory findings; (3) if the etiology of the cirrhosis was alcoholic , the patient had to have abstained from alcohol for ≥3 months prior to the start of the study; (4) Child-Pugh score ≤9; and (5) absent or small esophageal varices. The exclusion criteria were: (1) mean arterial pressure (MAP) <60 mmHg; (2) ARB intolerance; (3) current treatment with an ARB, angiotensin-converting enzyme inhibitors, or beta-blockers; (4) hypertrophic cardiomyopathy or renal arterial stenosis; (5) serum creatinine >1.6 mg/dL; (6) hyperkalemia, defined as plasma potassium >5.5 meq/L; (7) hepatocellular carcinoma; and (8) portal venous thrombosis. Treatment with furosemide was allowed in order to check for ascites throughout the study period if necessary.
Study protocol
Patients were randomized to receive either olmesartan (Olmetec; Daiichi-Sankyo, Tokyo, Japan) or not. The starting dose of olmesartan was 10 mg daily, in the morning, and the dose was increased in a stepwise fashion according to the manufacturer’s recommendations (e.g., from 10 to 20 then to 40 mg) at 2-week intervals up to the maximum dose of 40 mg daily, if tolerated, as long as the systolic blood pressure did not decrease below 90 mmHg, because 40 mg daily is recommended as the maximum daily dose in the general patient population [12]. Once the maintenance dose was reached, treatment was maintained for 48 weeks.
All patients underwent bi-weekly clinical check-ups until the end of the study. Serum biochemistry and blood pressure were monitored at the beginning of the study regimen and every 4 weeks thereafter. Hepatic hemodynamic studies, endoscopic examinations, and measurements of the levels of TGF-beta1, and blood markers for hepatic fibrosis, including serum HA, type IV collagen, and procollagen III N-terminal propeptide (PIIINP), were also performed at the beginning and at the end of the study. The occurrence of severe orthostatic symptoms together with severe arterial hypotension, defined as MAP <60 mmHg during the treatment, was considered a severe side effect that required withdrawal of the medication.
TGF-beta1 and blood markers of hepatic fibrosis
Platelet-poor plasma was prepared using collecting tubes for platelet factor 4 (SRL, Tokyo, Japan). Venous blood from the subjects was immediately transferred to a siliconized centrifuge tube containing 0.275 mL of a mixture of the following reagents: 2.7 g/L theophylline, 1.0 g/L adenosine, 0.1 g/L dipyridamole, 24 g/L trisodium citrate dehydrate, and 5.8 g/L citric acid monohydrate. The tubes were centrifuged (2000g for 30 min at 4°C) and the top 0.6 mL of the platelet-poor plasma was carefully removed and stored at −33°C until analysis. After the acid–ethanol extraction of TGF-beta1 from platelet-poor plasma, the TGF-beta1 concentration was measured with an enzyme-linked immunosorbent assay (ELISA) kit that uses chicken anti-human TGF-beta1 antibody as a solid-phase primary antibody and rabbit anti-human TGF-beta1 antibody as a second antibody (TGF-beta1 ELISA system; Amersham, Tokyo, Japan) [14, 15].
Serum HA concentration was determined by an enzyme-linked binding protein assay. The assay uses microwells coated with a highly specific HA binding protein (HABP) from bovine cartilage to capture HA, and an enzyme-conjugated version of HABP; the assay is carried out with a commercially available ELISA-type test kit (LPIA Ace HA; Fujirebo., Tokyo, Japan). The serum PIIINP concentration was measured with a commercial radioimmunoassay (RIA) kit (RIA-gnost PIIINP kit; Hoechst, Tokyo, Japan). The concentrations of the 7S fragment (7S collagen) and of the central triple-helix (IV collagen) of type IV collagen in serum were measured with a type IV collagen 7S domain RIA kit (Nippon DPC, Chiba, Japan) and a type IV collagen enzyme immunoassay (EIA) kit (Panassay IV-C; Fuji Chemical Industries, Takaoka, Japan), respectively.
Hepatic hemodynamic study
Portal venous pressure was assessed by hepatic vein catheterization. Under fluoroscopic control, a balloon catheter (5F, 8.5 mm, Meditech; Boston Scientific, Watertown, MA, USA) was inserted into a branch of the hepatic vein for manometry. HVPG was calculated as the occluded, wedged hepatic venous pressure (WHVP) minus the unoccluded free hepatic vein pressure (FHVP). The final value of HVPG measurements was the mean of at least two determinations [16]. The hemodynamic study and tracings analysis were performed by two different radiologists who were blinded to the clinical features of the patients and to the type of treatment.
Endoscopic findings
Endoscopic findings of esophageal varices were evaluated according to the grading system outlined in “The general rules for recording endoscopic findings of esophageal varices (2nd edition)” prepared by the Japanese Research Committee on Portal Hypertension [17]. The form (F) of the varices was classified as small, straight (F1), enlarged tortuous (F2), and large, coiled-shaped (F3).
Sample size calculation and randomization
We set up the primary endpoint as a reduction rate of HVPG of more than 20% of baseline values after 1 year because, in a previous study, we had estimated a reduction rate of 33% in the olmesartan group and a rate of 10% in the control group [18]. At least a 10% failure rate in both groups was estimated previously. On the basis of this 23% difference in 1 year, a minimum sample size of 22 per group would provide 80% power with a 2-sided type 1 error of 0.05 for significance. Randomization was done by computer and the results were kept in consecutively numbered see-through envelopes, and the sequence was concealed until treatment was assigned.
Statistical analysis
All data are presented as means ± SD. A paired or nonpaired Student’s t-test was used to assess the significance of comparisons of normally distributed data, and the Mann–Whitney U-test or the Wilcoxon test was used for non-normally distributed data. Correlation among variables was analyzed by Pearson correlation. All p values were two-tailed. A value of p < 0.05 was considered to indicate a statistically significant difference. Statistical analysis was performed with the statistical package SPSS Base 17.0 J for Windows (Microsoft).
Results
Between May 2007 and October 2008, a total of 57 patients with early liver cirrhosis were referred for possible randomization after screening (Fig. 1). In all, 9 patients were excluded from randomization. Four patients were treated with nonselective beta-blockers (NSBBs). Three patients were confirmed to have hepatocellular carcinoma. Furthermore, 2 patients were confirmed to have had portal venous thrombosis.
A total of 48 patients were randomized: 24 patients in the olmesartan arm and 24 patients in the control arm. The main characteristics of these patients are summarized in Table 1. There were no significant differences between patients randomized to the olmesartan group or the control in any parameter.
The therapy was well accepted and tolerated. However, 1 patient in the olmesartan group did not complete the study because of hypotension, and 1 patient from each group withdrew after we had received written informed consent. Thus, the final analysis included 22 patients receiving olmesartan and 23 controls. The median maximum administration dose of olmesartan was 20 mg; therefore, 5 patients were treated with a maintenance dose of 40 mg, 8 patients with 20 mg, and 9 patients with 10 mg.
Systemic and hepatic hemodynamics
Olmesartan reduced MAP by −9.8 ± 13.7% (p = 0.008) and HVPG by −12.9 ± 9.1% (p = 0.035) after 1 year. However, no significant changes were seen in these parameters in the controls (Table 2; Fig. 2). On intention-to-treat analysis, 6 of the 24 patients (25%) in the olmesartan group showed >20% reduction of HVPG from baseline values. Furthermore, 10 of the 24 (42%) patients showed between 10 and 20% reduction, while 8 of the 24 (33%) remained unchanged. There were no significant correlations between the reduction of HVPG and the doses of olmesartan. Furthermore, there were no significant differences between responders and non-responders in the patients’ baseline characteristics . However, we found a significant difference in baseline renin activity between the patients who achieved even a mild reduction of HVPG (>10% from baseline) and those who remained unchanged (1.1 ± 0.8 vs. 2.1 ± 1.6 ng/mL/h, p = 0.046).
Individual hepatic venous pressure gradient (HVPG) values at the baseline and after 1 year of treatment with olmesartan, and the control. Olmesartan significantly reduced HVPG by −12.9 ± 9.1% after 1 year, whereas no significant changes were seen in the controls. On intention-to-treat analysis, 6 of 24 patients (25%) in the olmesartan group showed >20% reduction of HVPG from baseline values. Mean values are indicated by the horizontal bar. *Significant differences (p = 0.035) by Wilcoxon test are shown
Endoscopic examinations
In the patients who had no varices before randomization, varices were observed in 2 of 11 patients (18%) in the control group but in 0 of 9 patients in the olmesartan group. Moreover, in the patients who had small varices (F1), the varices worsened in 6 of 13 patients (46%) in the control group and in 3 of 15 patients (20%) in the olmesartan group. There were no patients in either group who bled from esophageal varices, and there were no significant differences in baseline characteristics between the two groups.
TGF-beta1 and blood markers of hepatic fibrosis
Transforming growth factor-beta1 was significantly decreased in the olmesartan group (7.0 ± 8.2 vs. 3.1 ± 1.6 ng/mL, p = 0.046) at the end of the present study, compared with the level in the controls (6.3 ± 9.0 vs. 4.5 ± 4.5 ng/mL, p = 0.24). There was a significant negative correlation between the reduction of TGF-beta1 and the dose of olmesartan in the treated patients after 1 year (Fig. 3). Furthermore, a significant trend was shown by correlating HA and TGF-beta1 variations in cirrhosis patients at the end of the study. HA was significantly decreased in olmesartan-treated patients whose TGF-beta1 level was reduced and remained at the same level as that in the untreated patients (in whom the TGF-beta1 level remained the same as at baseline) (Fig. 4). A similar trend was observed in type IV collagen levels, but it did not reach statistical significance. On the other hand, the serum concentrations of the fibrosis markers, PIIINP, type IV collagen, and HA, were unchanged at the end of the study in both groups (Table 2). Furthermore, there were no significant differences in the alterations of HA and TGF-beta between the HVPG responders and non-responders.
Correlation between the variation of transforming growth factor-beta1 (TGF-beta1) and the maximum dose of olmesartan in the treated patients after 1 year. TGF-beta1 variation was defined as baseline TGF-beta1 value minus value after 1 year. A significant negative correlation between the above two variables was shown by Pearson correlation test (r = −0.48, p = 0.044)
Correlation between serum hyaluronic acid (HA) variation and TGF-beta1 variation in the treated patients (dark squares) and in the untreated patients (open triangles) after 1 year. The serum hyaluronic acid variation was defined as baseline serum hyaluronic acid value minus value after 1 year. A significant correlation between the above two variables was shown by Pearson correlation test (r = 0.377, p = 0.018)
Renal function
Serum creatinine was significantly increased in the olmesartan group (0.70 ± 0.15 vs. 0.76 ± 0.19 mg/dL, p = 0.004) but not in the control group (0.66 ± 0.16 vs. 0.68 ± 0.18 mg/dL, p = 0.17). There was no significant correlation between the variation in serum creatinine after 1 year and the maximum administration dose of olmesartan in the treated patients. On the other hand, there was a significant difference between patients treated with 40 mg and controls (0.12 ± 0.07 vs. 0.02 ± 0.02 mg/dL, p = 0.016) (Fig. 5).
Mean variation of serum creatinine in patients receiving olmesartan at the manufacturer’s recommended 10-, 20-, or 40-mg daily dose and in the control. Serum creatinine variation was defined as the baseline serum creatinine value minus that value after 1 year. There was no significant correlation between the variation in serum creatinine after 1 year and the maximum administration dose of olmesartan in the treated patients after 1 year. There was a significant difference between patients treated with 40 mg and controls (0.12 ± 0.07 vs. 0.02 ± 0.02 mg/dL). *Significant differences (p = 0.016) by Mann–Whitney U-test are shown
Tolerability to and side effects of olmesartan treatment
Twenty-two of the 24 patients (92%) who were randomized successfully completed the entire protocol. Three patients in the treatment group underwent diuretic treatment with 20 mg furosemide for ascites, and 1 patient in the control group underwent diuretic treatment with the same dose of furosemide.
One patient who had a Child-Pugh score of 9, and was undergoing diuretic treatment with 20 mg of furosemide for ascites, complained about dizziness after the first 10 mg of olmesartan was administered. She had hypotension with an arterial pressure of 79/60 mmHg, and discontinuation of treatment was mandatory. One week later, her arterial pressure had completely recovered. At her request, the medication was continued, at a one-quarter dose of olmesartan (5 mg). Neither subjective complaints nor hypotension recurred. Her TGF-beta1 level and serum concentrations of the fibrosis markers, type IV collagen and HA, had decreased after 1 year. A hepatic hemodynamic study was not done.
Discussion
In the present study, we demonstrated that long-term administration of an AT1 receptor blocker, olmesartan, significantly reduced HVPG as well as TGF-beta1 production. Overall, olmesartan achieved a more than 20% reduction of HVPG from the basal value in 25% of the patients. Furthermore, a mild HVPG reduction (>10%), generally observed in patients who had a significantly lower development of varices, was seen in 67% of the treated patients [19]. These results suggested that this AT1 receptor antagonist, olmesartan, would be effective for the early treatment of portal hypertension.
Nonselective beta-blockers (NSBBs) are widely used for variceal bleeding in patients with portal hypertension. However, a substantial proportion of the patients cannot be treated effectively because of side effects or an insufficient reduction in HVPG [19]. However, in a randomized, placebo-controlled study of NSBBs in patients with early cirrhosis with portal hypertension, the development of gastroesophageal varices and variceal hemorrhage did not differ significantly between the NSBB and placebo groups [20], although serious adverse events were more common in the NSBB group than in the placebo group. In light of these findings, patients with cirrhosis without clinical complications of portal hypertension do not receive treatment [19]. For this reason, a new active agent with the ability to reduce portal pressure safely is required in patients with early-stage cirrhosis.
Recently, ARBs have been proposed as new drugs for portal hypertension. In patients with cirrhosis, the action of Ang II is of major importance in regulating peripheral vascular tone [21]. It has clearly been shown that AT1 receptors induce contraction and proliferation of HSCs, which play a key role in intrahepatic resistance in cirrhosis [22]. Thus, the mechanism of olmesartan for the treatment of portal hypertension is probably a combination of systemic and local effects. In addition to the systemic effect we found in significantly reducing MAP (−9.8 ± 13.7%), which might reduce the splanchnic inflow and, thereby, portal pressure, the blockade of AT1 receptors on HSCs might induce sinusoidal vasodilatation and, thus, a reduction of intrahepatic resistance.
In the present study, we started to administer olmesartan at a daily dose of 10 mg. Generally, olmesartan has been approved for the treatment of arterial hypertension and it is usually prescribed at a dose of 20 mg/day. Von Bergmann et al. reported that after once-daily oral doses of 10 mg olmesartan were given to patients with mild and moderate hepatic impairment (Child-Pugh scores of ≤6 and 7–9, respectively), the daily maximum concentration of the drug in the body was generally similar to that in healthy matched subjects, but the area under the curve increased by 30 and 48%, respectively, and was reflected in increases of absolute bioavailability values compared with those in healthy subjects [23]. De et al. [24] showed that low-dose losartan was as effective as propranolol in reducing portal pressure in cirrhotic patients. On the other hand, Schepke et al. [25] showed that another ARB, irbesartan, moderately reduced portal pressure but induced marked arterial hypotension and renal impairment in patients with advanced cirrhosis. However, patients with advanced cirrhosis generally have relatively low systemic vascular resistance and arterial blood pressure [26], and may develop hypotension when taking irbesartan when given at 150 mg/day, the standard recommended dose for the treatment of hypertension. In the present study, olmesartan at 10 mg/day significantly reduced MAP, and only 1 patient, who had a Child-Pugh score of 9, had a hypotensive reaction during the study. Moreover, olmesartan significantly reduced serum creatinine after 1 year, especially in patients treated with a 40-mg daily dose. Therefore, we recommend that an ARB should be administered to patients with early-stage cirrhosis, starting with a low dose.
In the present study, we first observed that the ARB significantly attenuated the increase of TGF-beta1, which is a key cytokine for liver fibrosis. We found that there were significant negative correlations between the reduction of TGF-beta1 and the maximum administration dose of olmesartan. Furthermore, HA was significantly decreased in the olmesartan-treated patients who manifested a reduced TGF-beta1 level that remained at the same level as that in the untreated patients (in whom TGF-beta1 remained constant). This observation could therefore indicate that reduction of TGF-beta1 might mediate the modification of fibrogenetic activity. However, this hypothesis warrants further study, because it is based on the change of only 1 of 3 serum markers of liver fibrosis and is not supported by histological data.
There are two limitations of the present study. First, the study defined the primary endpoint as a reduction rate of HVPG of more than 20% of baseline values after 1 year. This based on a 1-year administration effect of olmesartan for HVPG. However, we were not able to assess whether there was a significant difference in the patients’ baseline characteristics in relation to their olmesartan responses. We included 20 of 24 Child-Pugh Class A patients (83%) in the present study because we had found, in our previous study, that responders to olmesartan had a significant tendency toward better hepatic function [18]. In the present study, the mean HVPG reduction rate in the treated patients was −12.9% after 1 year. On the other hand, in the candesartan study done by Debernardi-Venon et al., the mean HVPG reduction rate in the treated patients was −8.4% [7]. In their study, Child-Pugh A patients accounted for 71% of their cohort (17/24). The difference in the mean HVPG reduction rate between their study and ours is likely related to the higher proportion of Child-Pugh A patients (83%) in the present study. Second, we compared the effects of treatment with olmesartan with no treatment, but not with treatment with NSBBs. When we planned this study, at the end of 2006, to our knowledge, there were no randomized studies that had investigated the long-term effects of ARBs in patients with cirrhosis. Therefore, we conducted this randomized study which compared olmesartan with no treatment. Recently, Tandon et al. [27] reported, in their systematic review and meta-analysis, the efficacy of ARB for patients with cirrhosis. They concluded that ARB reduced portal pressure in patients with Child-Pugh A cirrhosis without adverse events; moreover, the effect of the ARB was similar to that of an NSBB. Also, there were no significant differences between their groups in adverse events or withdrawals. However, in their review, the effect of ARB on hepatic fibrosis in patients with cirrhosis remained unclear. Therefore, we are planning a future study of olmesartan which compares its long-term efficacy with that of an NSBB for the treatment of patients with hepatic fibrosis.
In conclusion, 1 year of administration of olmesartan significantly reduced portal pressure and TGF-beta1, which is the key cytokine for liver fibrosis, in patients with cirrhosis. Further examinations are warranted to confirm the efficacy of this AT1 receptor blocker.
Abbreviations
- TGF-beta1:
-
Transforming growth factor-beta1
- AT1:
-
Angiotensin type 1
- HA:
-
Hyaluronic acid
- HVPG:
-
Hepatic venous pressure gradient
- Ang II:
-
Angiotensin II
- RAS:
-
Renin–angiotensin system
- HSC:
-
Hepatic stellate cell
- NASH:
-
Nonalcoholic steatohepatitis
- ARB:
-
Angiotensin receptor blocker
- PIIINP:
-
Procollagen III N-terminal propeptide
- MAP:
-
Mean arterial pressure
- ELISA:
-
Enzyme-linked immunosorbent assay
- HABP:
-
Hyaluronic acid binding protein
- RIA:
-
Radioimmunoassay
- EIA:
-
Enzyme immunoassay
- WHVP:
-
Wedged hepatic venous pressure
- FHVP:
-
Free hepatic vein pressure
- NSBB:
-
Nonselective beta-blocker
References
Yoshiji H, Kuriyama S, Yoshii J, Ikenaka Y, Noguchi R, Nakatani T, et al. Angiotensin-II type 1 receptor interaction is a major regulator for liver fibrosis development in rats. Hepatology. 2001;34:745–50.
Gaedeke J, Peters H, Noble NA, Border WA. Angiotensin II, TGF-beta and renal fibrosis. Contrib Nephrol. 2001;135:153–60.
Nagy P, Scaff Z, Lapis K. Immunohistochemical detection of transforming growth factor-beta 1 in fibrotic liver diseases. Hepatology. 1991;14:269–73.
Matsuoka M, Tsukamoto H. Stimulation of hepatic lipocyte collagen production by Kupffer cell-derived transforming growth factor beta: implication for a pathogenetic role in alcoholic liver fibrogenesis. Hepatology. 1990;11:599–605.
Terui Y, Saito T, Watanabe H, Togashi H, Kawata S, Kamada Y, et al. Effect of angiotensin receptor antagonist on liver fibrosis in early stages of chronic hepatitis C. Hepatology. 2002;36:1022.
Yokohama S, Yoneda M, Haneda M, Okamoto S, Okada M, Aso K, et al. Therapeutic efficacy of an angiotensin II receptor antagonist in patients with nonalcoholic steatohepatitis. Hepatology. 2004;40:1222–5.
Debernardi-Venon W, Martini S, Biasi F, Vizio B, Termine A, Poli G, et al. AT1 receptor antagonist candesartan in selected cirrhotic patients: effect on portal pressure and liver fibrosis markers. J Hepatol. 2007;46:1026–33.
Kim S, Iwao H. Involvement of angiotensin II in cardiovascular and renal injury: effects of an AT1-receptor antagonist on gene expression and the cellular phenotype. J Hypertens Suppl. 1997;15:S3–7.
Otsuka M, Takahashi H, Shiratori M, Chiba H, Abe S. Reduction of bleomycin induced lung fibrosis by candesartan cilexetil, an angiotensin II type 1 receptor antagonist. Thorax. 2004;59:31–8.
Boffa JJ, Lu Y, Placier S, Stefanski A, Dussaule JC, Chatziantoniou C. Regression of renal vascular and glomerular fibrosis: role of angiotensin II receptor antagonism and matrix metalloproteinases. J Am Soc Nephrol. 2003;14:1132–44.
Yamada T, Kuno A, Masuda K, Ogawa K, Sogawa M, Nakamura S, et al. Candesartan, an angiotensin II receptor antagonist, suppresses pancreatic inflammation and fibrosis in rats. J Pharmacol Exp Ther. 2003;307:17–23.
Mizuno M, Sada T, Ikeda M, Fukuda N, Miyamoto M, Yanagisawa H, et al. Pharmacology of CS-866, a novel nonpeptide angiotensin II receptor antagonist. Eur J Pharmacol. 1995;285:181–8.
Oparil S, Williams D, Chrysant SG, Marbury TC, Neutel J. Comparative efficacy of olmesartan, losartan, valsartan, and irbesartan in the control of essential hypertension. J Clin Hypertens (Greenwich). 2001;3:283–91 (318).
Murawaki Y, Ikuta Y, Nishimura Y, Koda M, Kawasaki H. Serum markers for fibrosis and plasma transforming growth factor-beta 1 in patients with hepatocellular carcinoma in comparison with patients with liver cirrhosis. J Gastroenterol Hepatol. 1996;11:443–50.
Shirai Y, Kawata S, Tamura S, Ito N, Tsushima H, Takaishi K, et al. Plasma transforming growth factor-beta 1 in patients with hepatocellular carcinoma. Comparison with chronic liver diseases. Cancer. 1994;73:2275–9.
Bosch J, Mastai R, Kravetz D, Navasa M, Rodes J. Hemodynamic evaluation of the patient with portal hypertension. Semin Liver Dis. 1986;6:309–17.
Tajiri G, Yoshida H, Obara K, Onji M, Kage M, Kitano S, et al. General rules for recording endoscopic findings of esophagogastric varices (2nd edn). Dig Endosc. 2010;22:1–9.
Hidaka H, Kokubu S, Nakazawa T, Okuwaki Y, Ono K, Watanabe M, et al. New angiotensin II type 1 receptor blocker olmesartan improves portal hypertension in patients with cirrhosis. Hepatol Res. 2007;37:1011–7.
Garcia-Tsao G, Bosch J, Groszmann RJ. Portal hypertension and variceal bleeding—unresolved issues. Summary of an American Association for the Study of Liver Diseases and European Association for the Study of the Liver single-topic conference. Hepatology. 2008;47:1764–72.
Groszmann RJ, Garcia-Tsao G, Bosch J, Grace ND, Burroughs AK, Planas R, et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005;353:2254–61.
Bataller R, Gines P, Nicolas JM, Gorbig MN, Garcia-Ramallo E, Gasull X, et al. Angiotensin II induces contraction and proliferation of human hepatic stellate cells. Gastroenterology. 2000;118:1149–56.
Rockey D. The cellular pathogenesis of portal hypertension: stellate cell contractility, endothelin, and nitric oxide. Hepatology. 1997;25:2–5.
Von Bergmann K, Laeis P, Puchler K, Sudhop T, Schwocho LR, Gonzalez L. Olmesartan medoxomil: influence of age, renal and hepatic function on the pharmacokinetics of olmesartan medoxomil. J Hypertens Suppl. 2001;19:S33–40.
De BK, Bandyopadhyay K, Das TK, Das D, Biswas BK, Majumdar D, et al. Portal pressure response to losartan compared with propranolol in patients with cirrhosis. Am J Gastroenterol. 2003;98:1371–6.
Schepke M, Werner E, Biecker E, Schiedermaier P, Heller J, Neef M, et al. Hemodynamic effects of the angiotensin II receptor antagonist irbesartan in patients with cirrhosis and portal hypertension. Gastroenterology. 2001;121:389–95.
Henriksen JH, Fuglsang S, Bendtsen F, Moller S. Arterial hypertension in cirrhosis: arterial compliance, volume distribution, and central haemodynamics. Gut. 2006;55:380–7.
Tandon P, Abraldes JG, Berzigotti A, Garcia-Pagan JC, Bosch J. Renin-angiotensin-aldosterone inhibitors in the reduction of portal pressure: a systematic review and meta-analysis. J Hepatol. 2010;53:273–82.
Acknowledgments
The authors thank the radiologists of Kitasato University East Hospital for their technical assistance. We also thank Robert E. Brandt (Founder and CEO, MedEd Japan) for editing the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
The trial described in this work has been registered under the following trial number UMIN000003975.
Rights and permissions
About this article
Cite this article
Hidaka, H., Nakazawa, T., Shibuya, A. et al. Effects of 1-year administration of olmesartan on portal pressure and TGF-beta1 in selected patients with cirrhosis: a randomized controlled trial. J Gastroenterol 46, 1316–1323 (2011). https://doi.org/10.1007/s00535-011-0449-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-011-0449-z