Abstract
Introduction
The aim of this study is to rigorously review the efficacy and safety of olanzapine in defined hematology oncology settings including (1) the setting of highly emetogenic chemotherapy (HEC) and moderately emetogenic chemotherapy (MEC) settings (2) at 5 mg and 10 mg doses, and (3) for response rates for use in the acute, delayed, and overall settings post-MEC and HEC.
Methods
Ovid MEDLINE, Embase, and Cochrane Central Register of Controlled Trials were searched through April 23, 2020. The primary efficacy endpoints were the rate of complete response, in the acute (0–24 h post-chemotherapy), delayed (24–120 h post-chemotherapy), and overall (0–120 h post-chemotherapy) phases. The secondary efficacy endpoints were the rates of no nausea and no emesis, for each phase. Safety endpoints were the rate of no serious adverse events (i.e., no grade 3 or 4 toxicities), as assessed by Common Terminology Criteria for Adverse Events (CTCAE) criteria. The Mantel-Haenszel, random-effects analysis model was used to compute risk ratios and accompanying 95% confidence intervals for each endpoint. For endpoints that statistically favored one arm, absolute risk differences were computed to assess whether there is a 10% or greater difference, used as the threshold for clinical significance by MASCC/ESMO. Fragility indices were also calculated for each statistically significant endpoint, to quantitatively assess the robustness of the summary estimate. A cumulative meta-analysis was conducted for each efficacy meta-analysis with more than 5 studies, also using the Mantel-Haenszel random-effects analysis model.
Results
Three studies reported on olanzapine for the rescue of breakthrough chemotherapy-induced nausea and vomiting (CINV); 22 studies reported on olanzapine in the prophylactic setting. For studies reporting on HEC patients, olanzapine-containing regimens were statistically and clinically superior in seven of nine efficacy endpoints in the prophylaxis setting. When olanzapine is administered at a 10-mg dose, it is statistically and clinically superior to control patients in eight of nine endpoints among adults. Olanzapine may be effective in the MEC setting and when administered at 5-mg doses, but the paucity of data leads to notable uncertainty.
Conclusion
Further RCTs are needed in the setting of MEC patients and administration of olanzapine at a lower 5-mg dose, which may be given to reduce the sedative effect of olanzapine at 10 mg.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For cancer patients undergoing chemotherapy, chemotherapy-induced nausea and vomiting (CINV) are two prevalent and potentially treatment-limiting side effects [1]. Female patients and younger patients have been reported to be at greater risk [2,3,4]. Patients who have experienced vomiting during previous chemotherapy and those with high expectations of severe nausea prior to chemotherapy are at greater risk as well [5].
CINV is classified according to its time of incidence as either acute (0–24 h post-chemotherapy) or delayed (24–120 h post-chemotherapy). CINV that occurs during the course of chemotherapy despite a prophylactic regimen is termed as breakthrough CINV [6, 7].
Only two groups of antiemetics have been developed to target specific biochemical CINV pathways. These include neurokinin (NK)1-receptor antagonists (e.g., aprepitant, rolapitant, and netupitant), and serotonergic (5-HT)3-receptor antagonists (e.g., ondansetron, palonosetron), whereas dopamine (D)2-receptor antagonists (e.g., prochlorperazine, metoclopramide) initially were developed for different indications [8,9,10,11]. Olanzapine was approved by the US Food and Drug Administration as an antipsychotic [12], but has been used off-label as an antiemetic due to its potential to bind to multiple receptors in the CINV pathway, specifically serotonergic 5-HT2a, 5-HT2c, 5-HT3, 5-HT6, and dopamine D1, D2, D3, and D4 receptors [13].
Several phase I–II trials first investigated the efficacy and safety of olanzapine [14,15,16,17,18,19]. A systematic review and meta-analysis of early phase trials reported that 97.2% and 83.1% of patients achieved complete response (defined as no emesis and no use of rescue antiemetics) in the acute and delayed phase, respectively [20].
A number of phase III randomized controlled trials were subsequently undertaken and published, and multiple systematic reviews and meta-analyses have been conducted [21,22,23,24,25,26,27]. However, no review has separately analyzed antiemetics for highly emetogenic chemotherapy (HEC) and moderately emetogenic chemotherapy (MEC) patients, an important distinction that leads to different clinical guideline recommendations. Notably, the American Society of Clinical Oncology (ASCO) [28] currently recommends olanzapine as part of a four-drug regimen for HEC patients, while the National Comprehensive Cancer Network (NCCN) [29] and the Multinational Association of Supportive Care in Cancer (MASCC)/the European Society for Medical Oncology (ESMO) [30] recommend the four-drug regimen as an option in HEC patients. None of these guidelines, however, recommend olanzapine for MEC patients [28, 30]. Furthermore, each of the published reviews has methodological limitations when appraised using AMSTAR-2, a critical appraisal tool for systematic reviews [31] (Appendix 1 Electronic Supplementary Material).
Given the growing interest in olanzapine and the need for a more rigorous review, the aim of this study is to review the efficacy and safety of olanzapine for the prophylaxis and rescue of CINV through a systematic review and meta-analysis. Furthermore, given the large body of existing data, the aim of this review will be to determine the shortfalls of existing literature to provide future direction for olanzapine research in the CINV setting through a cumulative meta-analysis and fragility assessment.
Methods
The protocol for this review has been included in Appendix 2 Electronic Supplementary Material. The reporting of this review is conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA) checklist [32].
Search strategy
In the interest of conducting a rigorous and comprehensive review, a de novo search strategy was developed to search databases from their beginnings. Ovid MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials were searched from their beginning to April 24, 2020. Search restrictions were placed, so only English-language clinical trials were identified (Appendix 3 Electronic Supplementary Material).
Study selection
Two independent in-duplicate screenings were conducted. Where disagreements occurred, discussion of discrepancies occurred and consensus achieved, with the input of a senior author if required. Cohen’s kappa coefficient was calculated, to report the concordance.
Studies were first screened by title and abstract (level 1 screening). Studies were included after level 1 if they reported on olanzapine in a clinical trial for the setting of CINV. These abstracts then underwent full-text screening (level 2 screening) and were eligible for assessment of quantitative synthesis if they compared an olanzapine-containing regimen in one trial arm to a non-olanzapine-containing regimen in the other trial arm(s). Reference lists of included articles after level 2 screening were also assessed, to identify other potentially relevant randomized controlled trials. Studies with less than 5 patients per arm and non-randomized trials were excluded.
Data extraction
As with study selection, data extraction was conducted in duplicate and independently. Disagreements were resolved via discussion, to achieve consensus.
Study demographics of age range, percentage male, chemotherapy emetogenicity, and the difference between the olanzapine regimen and the comparative regimen were noted. The primary efficacy endpoints were the rate of complete response, in the acute (0–24 h post-chemotherapy), delayed (24–120 h post-chemotherapy), and overall (0–120 h post-chemotherapy) phases. The secondary efficacy endpoints were the rates of no nausea and no emesis, for each phase. Safety endpoints were the rate of no serious adverse events (i.e., no grade 3 or 4 toxicities, as assessed by Common Terminology Criteria for Adverse Events (CTCAE) criteria), as reported by authors. Grades 1 and 2 toxicities were not extracted for analysis, due to the paucity of data.
When a trial had two olanzapine-containing arms, the data across the two olanzapine arms were summed for analysis and compared to the non-olanzapine-containing arm.
Meta-analysis
The Mantel-Haenszel, random-effects analysis model was used to compute risk ratios (RRs) and accompanying 95% confidence intervals for each endpoint. A p value of less than 0.05 was considered statistically significant in the test for overall effect.
Studies were first separately meta-analyzed by regimen intent—whether olanzapine was administered for prophylaxis or for management of breakthrough nausea. It was then analyzed by age, separating studies reporting on adult and children. Adult studies were further meta-analyzed according to chemotherapy emetogenicity, olanzapine dosage, comparative regimens, and study quality; meta-analyses were conducted for the following subgroups of adult studies:
-
1.
HEC studies, as determined by the MASCC/ESMO classification [33]
-
2.
MEC studies, as determined by the MASCC/ESMO classification [33]
-
3.
Olanzapine, administered as 10 mg daily PO
-
4.
Olanzapine, administered as 5 mg daily PO
-
5.
Studies with a double-blind, placebo-controlled design, where the control arm includes a placebo and all antiemetics of the olanzapine-containing arm except for olanzapine itself
-
6.
Studies with an open-controlled design, where the control arm includes all the antiemetics of the olanzapine-containing arm except for olanzapine itself
-
7.
Studies with an open-controlled design, where the control arm includes antiemetics not included in the olanzapine-containing arm
For endpoints that statistically favored one arm and had more than 3 included trials, absolute risk differences (RD) were computed to assess whether there is a 10% or greater difference, deemed to be the threshold for clinical significance by MASCC/ESMO [34]. These analyses were performed using Review Manager (RevMan 5.4) by Cochrane IMS.
Fragility assessment
Fragility indices were calculated for each statistically significant endpoint by subgroup, to quantitatively assess the robustness of the summary estimate. Determination of the index involves a series of iterative calculations, until the simulated study results change from statistically significant to statistically insignificant according to the Fisher’s exact test. Essentially, the index is the number of control patients that would need to change from a nonevent to an event outcome, to change the statistical conclusion of a trial [35]. These analyses were conducted using Stata 16.
Cumulative meta-analysis
A cumulative meta-analysis was conducted for each efficacy meta-analysis with more than 5 studies, also using the Mantel-Haenszel random-effects analysis model. These analyses will allow for the assessment of the impact of each trial on the meta-analysis summary effect size and 95% CI. These analyses were conducted using Comprehensive Meta-Analysis (Version 3) by Biostat.
Assessment of bias
The Cochrane Risk of Bias tool was used to assess the quality of included randomized controlled trials. Four reviewers (RC, LC, ML, CD) independently assessed bias, after which discussion and consensus was used to resolve any discrepancies. Funnel plots were generated to visually assess for publication bias, for each phase of the three efficacy endpoints where there are 5 or more trials; these were generated using Comprehensive Meta-Analysis (Version 3) by Biostat.
Results
Included studies
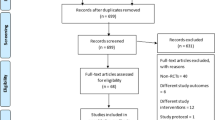
From the search strategies, 312 records were identified. After removing duplicate records and adding records identified from included trials, 178 records underwent level 1 screening. A total of 34 full-text articles were assessed for eligibility through level 2 screening, at which points 6 were excluded with reason—three were not a randomized controlled trial [36,37,38], one did not investigate olanzapine in the CINV setting [39], and two did not have an appropriate treatment regimen for inclusion in our review [40, 41]. Of the remaining 28 articles, 25 randomized controlled trials had extractable data and were included in this systematic review and meta-analysis(Appendix 4 Electronic Supplementary Material). Concordance, as measured by Cohen’s Kappa, for level 1 screening was 0.86, and 0.84 for level 2 (Appendix 5 Electronic Supplementary Material).
Three studies reported on olanzapine for the rescue of breakthrough CINV [42,43,44]; 22 studies reported on olanzapine in the prophylactic setting [45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66]. Only seven studies (one reporting on rescue of breakthrough CINV, and six reporting on prophylactic CINV) had no corresponding full-text articles [42, 48, 53, 55, 56, 60, 61]. One study reported on olanzapine for children [48]. Among the adult prophylactic studies, 15 reported exclusively on HEC patients [46, 49,50,51,52, 55, 56, 58, 60,61,62,63,64,65,66], three exclusively on MEC patients [53, 57, 59], and three on a patient population that consists of both HEC and MEC patients [45, 47, 54]. Eight studies compared olanzapine to a double-blind placebo-controlled regimen [47, 52, 59, 62,63,64,65,66] and thirteen used an opened controlled study design—nine studies used a control arm with antiemetics different from the antiemetics in the investigational (olanzapine-containing) arm [46, 49, 51, 53, 55, 56, 58, 60, 61] and four used a control arm with the same antiemetics as in the investigational (olanzapine-containing) arm except for olanzapine [45, 50, 54, 57]. 17 adult prophylactic studies used 10 mg doses of olanzapine [45, 46, 49,50,51,52,53,54,55,56,57,58,59, 61, 62, 65, 66], and 3 studies used 5 mg [47, 60, 63]; 1 used a mix of 5 mg and 10 mg [64] (Table 1).
Quality of included studies
The risk of bias assessment for each included study is reported in Appendix 6 Electronic Supplementary Material. Over half of all included studies had high risk of bias, due to concerns around lack of blinding.
Assessment for publication bias of olanzapine for the prophylaxis of CINV
Funnel plots are presented in Appendix 7, 8 Electronic Supplementary Material. There are no obvious asymmetries, suggesting no obvious concerns of publication bias in this body of literature.
Efficacy of olanzapine for the prophylaxis of CINV in children
In children, olanzapine was not statistically superior in the acute and overall phases, according to the one study by Long et al.
Efficacy of olanzapine for the prophylaxis of CINV in adults
Complete response
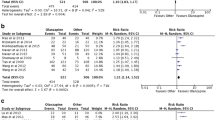
Acute phase
Olanzapine was statistically better than comparative regimens in the acute phase. Among HEC studies, studies using 10 mg olanzapine dosages, studies using a double-blind placebo-controlled design, and open-design studies comparing olanzapine to control regimens of antiemetics not included in the investigational arm, olanzapine was still statistically superior (Fig. 1.1). Olanzapine was clinically superior (risk difference greater than 10%) overall, in HEC studies, studies using 10 mg olanzapine doses, and for studies comparing olanzapine in a double-blind placebo-controlled design (Table 2).
Delayed phase
Olanzapine was also statistically and clinically superior in the delayed phase. This statistical and clinical superiority prevails in analyses of HEC studies, studies using 10-mg olanzapine doses, studies administering 5-mg of olanzapine, and studies assessing olanzapine in double-blind placebo control studies (Fig. 1.2; Table 2).
Overall phase
Olanzapine was statistically and clinically superior in the overall phase among all studies, HEC studies, 10-mg olanzapine studies, 5-mg olanzapine studies, and double-blind placebo-controlled studies (Fig. 1.3; Table 2).
Nausea control
For the acute, delayed, and overall phases, olanzapine was statistically superior to comparative regimens. This observation was similarly noted among HEC studies, studies where 10 mg of olanzapine was administered, and double-blind placebo-controlled trials. Olanzapine was also statistically and clinically superior to open-design studies using a control arm with different antiemetics than used in the investigational (olanzapine-containing) arm in the delayed and overall phases (Fig. 2; Table 2).
Emesis control
Neither olanzapine nor control arms were statistically superior to the comparator arm in the acute phase. Olanzapine was both statistically and clinically superior in the delayed and overall phases. Olanzapine was statistically and clinically better in the delayed phase among HEC trials and 10-mg olanzapine trials (Fig. 3; Table 2).
Cumulative meta-analysis and fragility assessment of olanzapine for the prophylaxis of CINV
Across all three time phases, the meta-analysis results for complete response are the most robust; results reporting on emetic control are the least robust of the three efficacy endpoints (Appendix 9 Electronic Supplementary Material). The most recent trials did not lead to a noticeable effect on the meta-analysis’ summary estimate for the endpoints of complete response and nausea control (Appendix 10, 11 Electronic Supplementary Material).
Olanzapine for the rescue of breakthrough CINV
Olanzapine was statistically superior to comparative regimens with respect to complete control, nausea control, and emetic control, according to the one study reporting on each outcome (Fig. 4). Olanzapine was also clinically superior in all these aforementioned endpoints—RD = 0.33 (95% CI: 0.10–0.56) for complete response in the acute phase, RD = 0.38 (95% CI: 0.18–0.57) for complete response in the overall phase, RD = 0.45 (95% CI: 0.28–0.62) for nausea control in the overall phase, and RD = 0.39 (95% CI: 0.21–0.56) for emetic control in the overall phase.
Safety of olanzapine for the prophylaxis of CINV
Olanzapine is as safe as comparative regimens; the risk of serious adverse events is not statistically significant for olanzapine relative to other regimens (Appendix 12, 13 Electronic Supplementary Material).
Discussion
This review is the most rigorous systematic review to date investigating olanzapine in the CINV setting. A protocol was developed prior to the commencement, risk of bias for studies were assessed, and publication bias was assessed; some or all of these three methodological elements were omitted in prior reviews [21,22,23,24,25,26,27].
This review also has the highest statistical power and appraises all the clinically important endpoints. The most recent reviews by Zhou et al. in 2020 included 11 studies with 1107 patients [21]; other reviews by Bahbah et al. in 2019 and Sutherland et al. in 2018 included 9 RCTs with 1572 patients, and 14 trials with 1917 participants, respectively [22, 23]. This review summarizes the results across 25 studies, which reported on 4275 patients. One study reported the effect of olanzapine on children, and three studies reported on olanzapine for the rescue of breakthrough CINV; the remaining 23 studies reported on olanzapine for the prophylaxis of CINV in adults, across 4217 patients. Zhou et al. reported on acute and delayed emetic control with or without nausea control, Bahbah et al. meta-analyzed complete response and nausea control rates, and Sutherland et al. summarized instances where patients successfully experienced no nausea and no emesis; our review reports on complete response, nausea control, and emetic control.
For studies reporting on HEC patients, olanzapine is statistically and clinically superior in seven of nine efficacy endpoints in the prophylaxis setting; only complete emetic control in the acute and overall phases were not statistically different from comparative regimens. Meta-analysis results among studies employing 10-mg doses and among studies comparing olanzapine to placebo-controlled regimens indicated olanzapine as statistically and clinically superior in eight of nine efficacy endpoints for prophylaxis of CINV, with the exception of complete emetic control in the acute phase. These results support the international clinical guidelines [28,29,30] in their recommendation of 10-mg olanzapine in addition to standard antiemetic regimens for the prophylaxis of CINV among HEC patients.
Furthermore, this review includes important subgroup analyses not previously conducted among prophylactic studies, namely meta-analyzing studies reporting on MEC patients and 5-mg olanzapine dosing. Olanzapine is both statistically and clinically superior in only three of six efficacy endpoints where a 5-mg dosage is employed—complete response in the acute, delayed, and overall phases. However, it is important to note that over 800 patients across 4 studies were meta-analyzed for the efficacy endpoints of complete response; there was much less statistical power relative to meta-analyses looking at HEC patients alone. Furthermore, even for the efficacy endpoints of complete response, these meta-analysis results are much more fragile and less certain than those pertaining to olanzapine administered at 10-mg dose studies. Olanzapine may potentially be superior to comparative regimens when administered in 5-mg doses as indicated by point estimates, but the paucity of data results in low statistical power to find these differences statistically significant. Olanzapine has also recently been reported to be effective at 5-mg doses in controlling nausea and vomiting, unrelated to chemotherapy, for patients with advanced cancer [67]. More RCTs are needed in the CINV setting, to evaluate the efficacy of 5-mg olanzapine doses compared to non-olanzapine-containing regimens. Studies comparing 5-mg doses to 10-mg doses are also encouraged; an abstract recently presented by Mukhopadhyay et al. suggests that 5-mg and 10-mg doses may have similar efficacy, although it has no description of drop out patients or chemotherapy regimens in either arm, and no statistical calculations were published [39].
In the MEC setting, olanzapine is reported to be statistically and clinically superior in two of nine efficacy endpoints only—no nausea in the delayed phase, and no emesis in the overall phase. However, as with the results from the meta-analysis of 5-mg doses, there is a paucity of data in this setting. The results are less robust compared to those in the HEC setting, with the recent clinical trials having noticeable impacts on the summary effect size. More RCTs in this setting would allow for a better understanding of olanzapine’s true efficacy for MEC patients.
Olanzapine is reported to be clinically and statistically superior than other regimens for the rescue of breakthrough CINV. However, this review’s results are only supported by one included study for each efficacy endpoint. Results should be interpreted with caution. In both the prophylactic and rescue setting, olanzapine is reported to be equally as safe as other regimens. However, this too should be interpreted with caution, as the key adverse event of sedation is not routinely reported—many studies commonly reported only on serious (i.e., grade 3 or greater toxicity) adverse events, an observation also noted by our group several years ago [26]. It has been well-documented that olanzapine is a strong sedative, and patients commonly experience fatigue, drowsiness, and reduced general activity [20]. In the interest of reducing adverse events, further exploring the reduction of the dosage of olanzapine (i.e. more RCTs reporting on 5-mg olanzapine doses) is encouraged.
This review was not without limitations. Ideally, the protocol would have been registered on PROSPERO; given the COVID 19 pandemic, this was not a feasible option—protocol registration would have required several months, while in hindsight our review was already completed. There were numerous instances where there were high levels of heterogeneity; a random-effects model was applied in all circumstances to try to appropriately account for this. As well, as is the nature of meta-analyses, the results suffer from any intrinsic biases from included RCTs; over half of the studies have notable concerns of bias due to lack of blinding.
In conclusion, olanzapine is effective and safe for the prophylaxis and rescue of CINV. It has been well-documented in the HEC setting and when administered at 10-mg doses; it is statistically and clinically superior to comparative regimens, but its sedative properties can make it difficult to use in outpatient settings. It is unclear if olanzapine is effective in the MEC setting and when administered at a lower 5-mg dose, and further RCTs are needed for a more definitive conclusion. The sedative effect associated with 10 mg of olanzapine further corroborates the need for more investigations into using olanzapine at lower doses.
Data availability
N/A
References
Cohen L, de Moor CA, Eisenberg P et al (2007)Chemotherapy-induced nausea and vomiting: incidence and impact on patient quality of life at community oncology settings. Support Care Cancer 15:491–503
Pollera CF, Giannarelli D (1989) Prognostic factors influencing cisplatin-induced emesis: definition and validation of a predictive logistic model. Cancer 64:1117–1122
du Bois A, Meerpohl HG, Vach W et al (1992) Course, patterns and risk-factors for chemotherapy-induced emesis in cisplatin-pretreated patients: a study with ondansetron. Eur J Cancer 28:450–457
Osoba D, Zee B, Pater J, Warr D, Latreille J, Kaizer L (1997) Determinants of postchemotherapy nausea and vomiting in patients with cancer. J Clin Oncol 15:116–123
Molassiotis A, Aapro M, Dicato M, Gascon P, Novoa SA, Isambert N, Burke TA, Gu A, Roila F (2014) Evaluation of risk factors predicting chemotherapy-related nausea and vomiting: results from a European prospective observational study. J Pain Symptom Manag 47:839–848
Chow R, Warr DG, Navari RM, Tsao M, Milakovic M, Popovic M, Chiu L, Lam H, DeAngelis C (2018) Efficacy and safety of 1-day versus 3-day dexamethasone for the prophylaxis of chemotherapy-induced nausea and vomiting: a systematic review and meta-analysis of randomized controlled trials. J Hosp Manag Health Policy 2:25
Chow R, Valdez C, Chow N, Zhang D, Im J, Sodhi E, Lock M (2020) Oral cannabinoid for the prophylaxis of chemotherapy-induced nausea and vomiting – a systematic review and meta-analysis. Support Care Cancer 28:2095–2103
Gralla RJ, Itri LM, Pisko SE, Squillante AE, Kelsen DP, Braun DW Jr, Bordin LA, Braun TJ, Young CW (1981) Antiemetic efficacy of high-dose metoclopramide: randomized trials with placebo and prochlorperazine in patients with chemotherapy-induced nausea and vomiting. N Engl J Med 305:905–909
Chow R, Tsao M, Chiu L, Popovic M, Milakovic M, Lam H, DeAngelis C (2018) Efficacy of the combination of neurokinin-1 receptor antagonist, palonosetron, and dexamethasone compared to others for the prophylaxis of chemotherapy-induced nauseas and vomiting: a systematic review and meta-analysis of randomized controlled trials. Ann Palliat Med 7:221–223
Jordan K, Blattermann L, Hinke A et al (2018) Is the addition of a neurokinin-1 receptor antagonist beneficial in moderately emetogenic chemotherapy? – A systematic review and meta-analysis. Support Care Cancer 26:21–32
Chow R, Warr DG, Navari RM, Tsao M, Popovic M, Chiu L, Milakovic M, Lam H, DeAngelis C (2018) Should palonosetron be a preferred 5-HT3 receptor antagonist for chemotherapy-induced nausea and vomiting? An updated systematic review and meta-analysis. Support Care Cancer 26:2519–2549
Brymaster FP, Calligaro D, Falcone J et al (1996)Radio-receptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology 14:87–96
Srivastava M, Brito-Dellan N, Davis MP, Leach M, Lagman R (2003) Olanzapine as an antiemetic in refractory nausea and vomiting in advanced cancer. J Pain Symptom Manag 25:578–582
Abe M, Hirashima Y, Kasamatsu Y, Kado N, Komeda S, Kuji S, Tanaka A, Takahashi N, Takekuma M, Hihara H, Ichikawa Y, Itonaga Y, Hirakawa T, Nasu K, Miyagi K, Murakami J, Ito K (2016) Efficacy and safety of olanzapine combined with aprepitant, palonosetron and dexamethasone for preventing nausea and vomiting by cisplatin-based chemotherapy in gynecological cancer: KCOG-G1303 phase II trial. Support Care Cancer 24:675–682
Park S, Choi C, Kwon M et al (2015) A phase II trial of palonosetron and olanzapine without dexamethasone for the prevention of chemotherapy-induced nausea and vomiting. Support Care Cancer 23(Suppl 1):S147
Navari RM, Einhorn L, Passik S et al (2005) A phase II trial of olanzapine for the prevention of chemotherapy-induced nausea and vomiting: a Hoosier Oncology Group study. Support Care Cancer 13:529–534
Navari RM, Einhorn L, Loehrer P et al (2007) A phase II trial of olanzapine for the prevention of chemotherapy-induced nausea and vomiting: a Hoosier Oncology Group study. Support Care Cancer 15:1285–1291
Passik S, Navari RM, Jong S et al (2004) A phase I trial of olanzapine (zyprexa) for the prevention of delayed emesis in cancer patients: a Hoosier Oncology Group Study. Cancer Investig 22:383–388
Passik S, Lundberg J, Kirsh K et al (2002) A pilot exploration of the antiemetic activity of olanzapine for the relief of nausea in patients with advanced cancer and pain. J Pain Symptom Manag 23:526–532
Chow R, Chiu L, Navari R, Passik S, Chiu N, Popovic M, Lam H, Pasetka M, Chow E, DeAngelis C (2016) Efficacy and safety of olanzapine for the prophylaxis of chemotherapy-induced nausea and vomiting (CINV) as reported in phase I and II studies: a systematic review. Support Care Cancer 24:1001–1008
Zhou JG, Huang L, Jin SH et al (2020) Olanzapine combined with 5-hydroxytryptamine type 3 receptor antagonist (5-HT3 RA) plus dexamethasone for prevention and treatment of chemotherapy-induced nausea and vomiting in high and moderate emetogenic chemotherapy: a systematic review and meta-analysis of randomized controlled trials. ESMO Open 6:e000621
Bahbah EI, Abdalla AR, Abdelshafy K, Almohandes AD, Menshawy A, Elalem Aziz MA, Ebada MA, Hegab A, Negida A (2019) Should olanzapine be advocated over conventional anti-emetics for the prevention of chemotherapy-induced nausea and vomiting? An updated meta-analysis of randomized control trials. Curr Enzym Inhib 15:80–90
Sutherland A, Naessens K, Plugge E, Ware L, Head K, Burton MJ, Wee B, Cochrane Pain, Palliative and Supportive Care Group (2018) Olanzapine for the prevention and treatment of cancer-related nausea and vomiting in adults. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD012555.pub2
Chelkeba L, Gidey K, Mamo A, Yohannes B, Matso T, Melaku T (2017) Olanzapine for chemotherapy-induced nausea and vomiting: systematic review and meta-analysis. Pharm Pract 15:877
Yoodee J, Permsuwan U, Nimworapan M (2017) Efficacy and safety of olanzapine for the prevention of chemotherapy-induced nausea and vomiting: a systematic review and meta-analysis. Crit Rev Oncol Hematol 112:113–125
Chiu L, Chow R, Popovic M, Navari RM, Shumway NM, Chiu N, Lam H, Milakovic M, Pasetka M, Vuong S, Chow E, DeAngelis C (2016) Efficacy of olanzapine for the prophylaxis and rescue of chemotherapy-induced nausea and vomiting (CINV): a systematic review and meta-analysis. Support Care Cancer 24:2381–2392
Hocking CM, Kichenadasse G (2014) Olanzapine for chemotherapy-induced nausea and vomiting: a systematic review. Support Care Cancer 22:1142–1151
Hesketh PJ, Kris MG, Basch E et al (2017) Antiemetics: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 28:3240–3261
Berger MJ, Ettinger DS, Aston J, Barbour S, Bergsbaken J, Bierman PJ, Brandt D, Dolan DE, Ellis G, Kim EJ, Kirkegaard S, Kloth DD, Lagman R, Lim D, Loprinzi C, Ma CX, Maurer V, Michaud LB, Nabell LM, Noonan K, Roeland E, Rugo HS, Schwartzberg LS, Scullion B, Timoney J, Todaro B, Urba SG, Shead DA, Hughes M (2017) NCCN guidelines insights: antiemesis, versions 2.2017. J Natl Compr Cancer Netw 15:883–893
Herrstedt J (2018) The latest consensus on antiemetics. Curr Opin Oncol 30:233–239
Shea BJ, Wells G, Hamel C et al (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:j4008
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Jordan K, Chan A, Gralla RJ, Jahn F, Rapoport B, Warr D, Hesketh PJ (2017) 2016 updated MASCC/ESMO consensus recommendations: emetic risk classification and evaluation of the emetogenicity of antineoplastic agents. Support Care Cancer 25:271–275
Roila F, Molassiotis A, Herrstedt J et al (2016) 2016 MASCC and ESMO guideline update for the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting and of nausea and vomiting in advanced cancer patients. Ann Oncol 26:v119–v133
Walsh M, Srinathan SK, McAuley DF et al (2014) The statistical significance of randomized controlled trial results is frequently fragile: a case for a Fragility Index. J Clin Epidemiol 67:622–628
Babu G, Saldanha SG, Chinnaglriyappa LK et al (2016) The efficacy, safety and cost benefit of olanzapine versus aprepitant in highly emetogenic chemotherapy: a pilot study from South India. Chemother Res Pract 2016:1–5. https://doi.org/10.1144/2016/3439707
Flank J, Schechter T, Gibson P, Johnston DL, Orsey AD, Portwine C, Sung L, Dupuis LL (2018) Olanzapine for prevention of chemotherapy-induced nausea and vomiting in children and adolescents: a multi-center, feasibility study. Support Care Cancer 26:549–555
Osman AAM, Elhassan MMA, AbdElrahim BHA et al (2018) Olanzapine for the prevention of chemotherapy-induced nausea and vomiting: a comparative study from Sudan. J Glob Oncol 4:1–9. https://doi.org/10.1200/JGO.17.00216
Navari RM, Brenner MC (2010) Treatment of cancer-related anorexia with olanzapine and megestrol acetate: a randomized trial. Support Care Cancer 18:951–956
Minatogawa H, Izawa N, Kawaguchi T et al (2019) Phase III study of comparing dexamethasone on day 1 with day 1-4 with combined neurokinin-1 receptor antagonist, palonosetron and olanzapine in cisplatin-based chemotherapy. Support Care Cancer 27(Suppl 1):S38–S39
Mukhopadhyay S, Dutta P, Bhattacharya B et al (2018) Low dose olanzapine in chemotherapy induced nausea and vomiting: The ideal 8 pm antiemetic? Support Care Cancer 26(Suppl 1):S79
Navari RM, Gray SE (2009) Treatment of chemotherapy-induced breakthrough nausea and vomiting. J Clin Oncol 27:e20536. https://doi.org/10.1200/jco.2009.27.15_suppl.e20536
Navari RM, Nagy CK, Gray SE (2013) The use of olanzapine versus metoclopramide for the treatment of breakthrough chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy. Support Care Cancer 21:1655–1663
Nakagaki M, Barras M, Curley C, Butler JP, Kennedy GA (2017) A randomized trial of olanzapine versus palonosetron versus infused ondansetron for the treatment of breakthrough chemotherapy-induced nausea and vomiting in patients undergoing hematopoietic stem cell transplantation. Support Care Cancer 25:607–613
Tan L, Liu J, Liu X, Chen J, Yan Z, Yang H, Zhang D (2009) Clinical research of olanzapine for prevention of chemotherapy-induced nausea and vomiting. J Exp Clin Cancer Res 28:131
Navari RM, Gray SE, Kerr AC (2011) Olanzapine versus aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a randomized phase III trial. J Support Oncol 9:188–195
Mizukami N, Yamauchi M, Koike K, Watanabe A, Ichihara K, Masumori N, Yamakage M (2014) Olanzapine for the prevention of chemotherapy-induced nausea and vomiting in patients receiving highly or moderately emetogenic chemotherapy: a randomized, double-blind, placebo-controlled study. J Pain Symptom Manag 47:542–550
Long C, Knoderer H, Mueller E (2015) A pilot study comparing the addition of olanzapine or aprepitant in an antiemetic regimen for highly emetogenic chemotherapy. Pediatr Blood Cancer 62(Suppl 2):S104
Shumway NM, Terrazzino SE, Jones CG (2015) A randomized pilot study comparing olanzapine (Zyprexa) to aprepitant (Emend) for treatment of chemotherapy-induced nausea and vomiting. J Pain Manag 8:233–241
Wang X, Wang L, Wang H, Zhang H (2015) Effectiveness of olanzapine combined with ondansetron in prevention of chemotherapy-induced nausea and vomiting of non-small cell lung cancer. Cell Biochem Biophys 72:471–473
Navari RM, Nagy CK, Le-Rademacher JL et al (2016) Olanzapine versus fosaprepitant for the prevention of concurrent chemotherapy radiotherapy-induced nausea and vomiting. J Community Support Oncol 14:141–147
Navari RM, Qin R, Ruddy KJ, Liu H, Powell SF, Bajaj M, Dietrich L, Biggs D, Lafky JM, Loprinzi CL (2016) Olanzapine for the prevention of chemotherapy-induced nausea and vomiting. N Engl J Med 375:134–142
Mukesh S, Sathya M, Akshay JK (2017) Olanzapine versus aprepitant in the prevention of chemotherapy induced nausea and vomiting (CINV) in breast cancer patients. J Clin Oncol 35:e21670. https://doi.org/10.1200/JCO.2017.35.15_suppl.e21670
Mukhopadhyay S, Gagandeep K, Alice KP et al (2017) Role of olanzapine in chemotherapy-induced nausea and vomiting on platinum-based chemotherapy patients: a randomized controlled study. Support Care Cancer 25:145–154
Sapkota S, Mahaseth R, Jha K (2017) The use of olanzapine compared to aprepitant as antiemetic for prevention of chemotherapy induced nausea and vomiting in highly emetogenic chemotherapy – a randomized trial. Eur J Cancer 72:S168. https://doi.org/10.1016/S0959-8049(17)30623-8
Tran T, Nguyen N, Pham V et al (2017) Olanzapine and omeprazole combination is simple, safe and effective for delayed nausea and vomiting control in adjuvant chemotherapy for early stage breast cancer. Support Care Cancer 25:S72
Celio L, Salbene G, Lepori S et al (2019)Short-course olanzapine to prevent delayed emesis following carboplatin/paclitaxel for gynecologic cancer: a randomised study. Tumori J 105:253–258
Dulal S, Paudel BD, Neupane P, Shah A, Acharya B, Poudyal BS, Shilpakar R, Wood LA (2019) Randomized phase II trial to compare the efficacy of haloperidol and olanzapine in the control of chemotherapy-induced nausea and vomiting in Nepal. J Glob Oncol 5:1–6. https://doi.org/10.1200/JGO.18.00245
Jeon SY, Han HS, Bae WK, Park MR, Shim H, Lee SC, Go SI, Yun HJ, Im YJ, Song EK (2019) A randomized double-blind, placebo-controlled study of the safety and efficacy of olanzapine for the prevention of chemotherapy-induced nausea and vomiting in patients receiving moderately emetogenic chemotherapy: results of the Korean South West Oncology Group (KSWOG) study. Cancer Res Treat 51:90–97
Rumyantsev A, Glazkova E, Nasyrova R, Ignatova E, Chitia L, Popova A, Chekini D, Kochetkova Y, Kit S, Elsnukaeva K, Menshikova S, Sekhina O, Pokataev I, Tyulyandina A, Stenina M, Frolova MA, Bulanov A, Fedyanin M, Tryakin A, Tjulandin S (2019) Olanzapine (OLN) versus aprepitant (APR) in patients receiving high-emetogenic chemotherapy: final results of randomized phase II trial. J Clin Oncol 37:11504. https://doi.org/10.1200/JCO.2019.37.15_suppl.11504
Saldanha SC, Dasappa L, Jacob LA, Babu SM, Lokesh KN, Rudresha AH, Lakkavalli RK, Kumar J (2019) Efficacy of olanzapine combination in prevention of nausea & vomiting in highly emetogenic chemotherapy. Ann Oncol 30:v722
Tienchaiananda P, Nipondhkit W, Maneenil K, Sa-nguansai S, Payapwattanawong S, Laohavinij S, Maneechavakajorn J (2019) A randomized, double-blind, placebo-controlled study evaluating the efficacy of combination olanzapine, ondansetron and dexamethasone for prevention of chemotherapy-induced nausea and vomiting in patients receiving doxorubicin plus cyclophosphamide. Ann Palliat Med 8:372–380
Hashimoto H, Abe M, Tokuyama O, Mizutani H, Uchitomi Y, Yamaguchi T, Hoshina Y, Sakata Y, Takahashi TY, Nakashima K, Nakao M, Takei D, Zenda S, Mizukami K, Iwasa S, Sakurai M, Yamamoto N, Ohe Y (2020) Olanzapine 5 mg plus standard antiemetic therapy for the prevention of chemotherapy-induced nausea and vomiting (J-FORCE): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 21:242–249
Ithimakin S, Theeratrakul P, Laocharoenkiat A, Nimmannit A, Akewanlop C, Soparattanapaisarn N, Techawattanawanna S, Korphaisarn K, Danchaivijitr P (2020) Randomized, double-blind, placebo-controlled study of aprepitant versus two dosages of olanzapine with ondansetron plus dexamethasone for prevention of chemotherapy-induced nausea and vomiting in patients receiving high-emetogenic chemotherapy. Support Care Cancer 28:5335–5342. https://doi.org/10.1007/s00520-020-05380-6
Vimolchalao V, Sakdejayont S, Wongchanapai P, Sukprakun S, Angspatt P, Thawinwisan W, Chenaksara P, Sriuranpong V, Vinayanuwatikun C, Parinyanitikun N, Poovorawan N, Tanasanvimon S (2020) The efficacy and safety of the addition of olanzapine to ondansetron and dexamethasone for prevention of chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy. Int J Clin Oncol 25:396–402
Yeo W, Lau TKH, Li L, Lai KT, Pang E, Cheung M, Chan VTC, Wong A, Soo WMT, Yeung VTY, Tse T, Lam DCM, Yeung EWM, Ng KPK, Tang NLS, Tong M, Suen JJS, Mo FKF (2020) A randomized study of olanzapine-containing versus standard antiemetic regimens for the prevention of chemotherapy-induced nausea and vomiting in Chinese breast cancer patients. Breast 50:30–38
Navari RM, Pywell CM, Le-Rademacher JG et al (2020) Olanzapine for the treatment of advanced cancer-related chronic nausea and/or vomiting. JAMA Oncol 6:895–899. https://doi.org/10.1001/jamaoncol.2020.1052
Author information
Authors and Affiliations
Contributions
All authors contributed substantially to conception and design, or acquisition of data, or analysis and interpretation of data. All authors contributed in drafting the article or revising it critically for important intellectual content. All authors approved the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
Dr Lock reports consulting fees from Ferring, Abbvie, Sanofi, and AstraZeneca in the past 10 years outside the submitted work. Dr Herrstedt reports personal fees from SOBI and GSK outside the submitted work. Dr Aapro reports personal fees and non-financial support from the Multinational Association for Supportive Care in Cancer, personal fees and non-financial support from European Society of Medical Oncology, personal fees and non-financial support from the European Cancer Organisation, grants and personal fees from Helsinn, personal fees from Tesaro, grants and personal fees from Sandoz, personal fees from Merck USA, personal fees from Vifor, personal fees from Pfizer, personal fees from Taiho, and personal fees from Kyowa Kirin, outside the submitted work. The other authors declare that they have no conflict of interest.
Ethics approval
N/A
Consent to participate
N/A
Consent to publication
N/A
Code availability
N/A
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chow, R., Herrstedt, J., Aapro, M. et al. Olanzapine for the prophylaxis and rescue of chemotherapy-induced nausea and vomiting: a systematic review, meta-analysis, cumulative meta-analysis and fragility assessment of the literature. Support Care Cancer 29, 3439–3459 (2021). https://doi.org/10.1007/s00520-020-05935-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05935-7