Abstract
Purpose
Newer drugs incorporated in prophylactic regimens for chemotherapy-induced nausea and vomiting (CINV) have resulted in significantly reduced rates of this feared complication of cytotoxic chemotherapy. However, both delayed chemotherapy-induced nausea and breakthrough CINV remain difficult areas of management and require novel treatment strategies. Recent randomized trial evidence has suggested that olanzapine, an atypical antipsychotic, may have a role in both the prevention and treatment of CINV. A systematic review was conducted to assess the efficacy of olanzapine in (a) preventing CINV in highly emetogenic chemotherapy (HEC) and moderately emetogenic chemotherapy (MEC) and (b) the treatment of breakthrough CINV. The toxicity of olanzapine in this setting was also reviewed.
Methods
MEDLINE, Embase and Cochrane Database of Systematic Reviews databases were searched to identify all randomized clinical trials (RCTs) investigating olanzapine in patients receiving chemotherapy.
Results
A total of 488 patients from three trials of CINV prophylaxis and 323 patients from three trials of breakthrough CINV were included. Regimens including olanzapine were associated with significant improvements in CINV prevention with both HEC and MEC. Single agent olanzapine for breakthrough nausea was superior to standard alternative options.
Conclusion
Data from RCTs support the use of an olanzapine containing combination regimen as an option for CINV prophylaxis and single agent olanzapine for the treatment of breakthrough CINV. In the included trials, the short duration of olanzapine appears safe and well tolerated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Despite significant advances over the past two decades, chemotherapy-induced nausea and vomiting (CINV) is still perceived by patients as a major adverse effect of cytotoxic therapy [1]. New classes of drugs like serotonin (5-HT3) and neurokinin 1 (NK1) receptor antagonists have demonstrated improved rates of CINV control in randomized control trials (RCTs) and significant improvements in the quality of life of patients receiving chemotherapy [2, 3]. Further, understanding and clear categorization of cytotoxics by their emetogenic potential, improved trial design and establishment of widely accepted guidelines for CINV prevention have all contributed to improved outcomes for patients [4].
Trials evaluating the prevention of CINV have reported the occurrence of nausea and vomiting in three different phases post-chemotherapy: acute (0–24 h), delayed (24–120 h) and overall period (0–120 h). The two symptoms, vomiting (emesis) and nausea, have often been considered together. However, it has become apparent from recent trial results that improvement in vomiting prevention has not always reflected improved control of nausea. A common primary end point in clinical trials is “complete response” defined as no vomiting and no use of breakthrough antiemetic medications. Complete response (CR) provides an important and objectively measured outcome but does not provide reliable information on nausea control. The reporting of nausea relies on subjective assessment through standardized visual analogue scales. The subjective nature of data collection leads to considerable variation over how nausea is categorized and reported [5].
The combination of aprepitant, a NK1 receptor antagonist, and palonosetron, a second-generation 5-HT3 antagonist, along with steroids has demonstrated a significant improvement in complete response rates in patients receiving highly emetogenic chemotherapy (HEC). This triple combination is recommended as routine prophylaxis in this group of patients receiving HEC [4]. The addition of aprepitant achieved complete response in over 80 % of patients in the acute phase and 70 % of patients in the delayed phase, a major improvement compared to non-aprepitant-containing prophylaxis [3, 6, 7]. In non-aprepitant-containing prophylactic regimen, palonosetron achieved complete responses in 75 and 57 % in the acute and delayed phases, respectively [8]. The combination of netupitant, a novel NK1 antagonist, and palonosetron (termed NEPA) has recently shown superiority to palonosetron (both with dexamethasone) in achieving CR in the overall time period (74 vs 67 %; p = 0.01) [9]. This large phase III randomized double-blind trial consisted of, almost exclusively, female patients receiving anthracycline chemotherapy for breast cancer. Rates of “no significant nausea” were also improved with NEPA (75 vs 69 %; p = 0.20). Despite these newer developments, control of nausea remains a significant challenge. The reported rates of nausea exceeded 50 % in all the major RCTs exploring CINV prophylaxis in HEC [3, 6, 8].
The other area of significant unmet need is the effective treatment of CINV that occurs despite standard prophylaxis, termed breakthrough CINV. This scenario represents a very difficult clinical problem. No clinical trial data exists to support a particular antiemetic agent in this setting, and as such clinical practice guidelines lack specific recommendations for optimal treatment [4, 10].
Olanzapine, an atypical antipsychotic agent, antagonizes multiple neuronal receptors including dopamine (D1, D2, D4), serotonin (5HT2A, 5HT2C, 5HT3), alpha-1 adrenergic, histamine (H1) and multiple muscarinic receptors [11]. Olanzapine is FDA-approved for the treatment of schizophrenia and bipolar disorder since 1996 with well-documented long-term safety data [12]. Common toxicities include dizziness, sedation and extrapyramidal symptoms such as akathisia [12]. Long-term use of olanzapine is associated with metabolic effects including weight gain, dyslipidemia and onset of diabetes mellitus [5]. Dopamine and serotonin are well-recognized mediators of CINV, with the 5HT2 receptor a key factor in cisplatin-induced emesis in pre-clinical studies [13]. The demonstration that olanzapine is an effective antagonist of the serotonin-mediated 5-HT receptors provides biological rationale for its efficacy in the CINV setting [11]. Case reports and retrospective trials have demonstrated the efficacy of olanzapine in treating nausea and vomiting in various cancer settings [14–16] and led to several early-phase single-arm trials evaluating olanzapine in preventing CINV [17–19]. In this systematic review, we aimed to provide a comprehensive overview of the current evidence regarding the efficacy of olanzapine as an antiemetic option for both the prevention and treatment of CINV.
Objectives
The two primary objectives of this review are to investigate the clinical efficacy of olanzapine in the primary prevention of CINV and treating breakthrough CINV in patients receiving moderate or highly emetogenic chemotherapy.
The secondary objective is to examine information on adverse effects with olanzapine when used for the prevention and treatment of CINV.
Methods
A study protocol was prospectively developed outlining the objectives and methods of our systematic review. We defined the types of studies for inclusion into the review, the methods for searching, and data extraction and analysis.
Studies for inclusion
Studies were assessed against predefined eligibility criteria. Eligible studies were trials of adult patients receiving moderate or highly emetogenic chemotherapy for any indication where olanzapine was used as an intervention. Only randomized controlled trials were included.
Search methods and trial selection
Electronic databases MEDLINE® (PubMed), Embase and Cochrane Central Register of Controlled Trials were searched. A literature search was conducted using the following terms: “nausea AND chemotherapy”, “vomiting AND chemotherapy” with these results then searched against “AND olanzapine”. The search included all references up until 9 April 2013. Bibliographies and references listed in primary sources were also reviewed for additional trials.
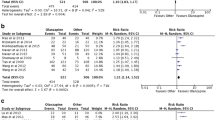
The two authors (CH and GK) undertook a first screening of all results (title and abstracts) independently against the inclusion criteria. A second independent screening occurred with full-text articles to identify the final trials for inclusion into this systematic review. Unpublished trials were included if adequate information on study design, intervention and outcomes were available. A total of six RCTs were included in the final analyses, three assessing olanzapine for prophylaxis against CINV and three for the treatment of breakthrough CINV (Fig. 1).
Assessment of methodological quality
Methodological qualities of the six trials included in this review were assessed using the Jadad scale, the most widely used assessment scale of methodologic quality in a clinical trial [20]. A higher score (range 0–5) indicates greater methodological rigor in areas of randomization, blinding and accountability of participants.
Of the three trials assessing olanzapine for the prevention of CINV, two scored 4 out of 5 on the Jadad scale [21, 22], while one of the reports scored 3 out of 5 [23]. Of the three trials assessing the use of olanzapine for breakthrough CINV, one trial scored 5 on the Jadad scale [24], while the other two [25, 26] (both unpublished reports) scored 2 out of 5, indicating significant deficiency of methodology and reporting.
Analysis
Data extraction from the included RCTs was undertaken and recorded on separate data extraction forms. Results from the trials of olanzapine as prophylaxis and treatment of breakthrough CINV were tabulated in separate tables. Data was not considered adequate to attempt meta-analysis.
Results
Prophylaxis of CINV
Patient characteristics
A total of 488 patients were included from three RCTs [21–23] (see Table 1). The age range was 18 to 81 years and included 267 females and 221 males. Primary sites of cancer and specific chemotherapy regimens were not able to be accurately identified in one of the included trials contributing 18 patients [22]. The remaining 470 patients had cancer diagnoses including breast cancer (38 %), non-small cell lung cancer (29 %) and lymphoma (9 %). HEC consisted of cisplatin (>70 mg/m2) in 56.5 %, doxorubicin and cyclophosphamide (AC regimen) in 42.9 % and dacarbazine in less than 1 %.
Study design
All three studies were randomized controlled trials. Only one was a double-blind trial [22]. However, this trial randomized a small cohort of 18 patients and was available in abstract form as a conference presentation.
Efficacy
All three trials reported CR as the primary end point. CR was evaluated in the acute and delayed phases in all trials. Two trials reported CR in the overall time period [21, 23], while one did not report this outcome measure [22]. In the large trial by Navari et al. comparing olanzapine to aprepitant (the current standard of care) in patients receiving HEC, the numerically improved rates of CR with olanzapine were not statistically significant in any time period including the primary end point: CR in the overall period (77 vs 73 %; p > 0.05) [21]. Statistically significant improvements in olanzapine-treated patients were seen in secondary end points: no delayed nausea (69 vs 38 %; p < 0.01) and no nausea in the overall period (69 vs 38 %; p < 0.01). No nausea was defined as a score of 0 out of 10 in the nausea domain of the MD Anderson Symptom Inventory (MDASI).
In the other large trial evaluating CINV for both HEC and moderately emetogenic chemotherapy (MEC) regimens [23], a NK1 antagonist was not used. The investigational arm involved the addition of olanzapine to the control arm (5-HT3 antagonist, dexamethasone). CR rates were not significantly different in the acute period for either chemotherapy regimen. There was a statistically significant difference in delayed and overall CR rates in both HEC-treated (overall CR; 79 vs 57 %; p < 0.05) and MEC-treated (overall CR; 89 vs 76 %; p < 0.05) patients. Nausea control was also significantly improved in the delayed and overall periods in both HEC- and MEC-treated patients. The definition of nausea control in this trial involved a quality of life (QoL) questionnaire and the absence of breakthrough antiemetics.
In the trial by Shumway et al., 18 patients receiving HEC, olanzapine was compared to aprepitant [22]. While there was a numerical trend to improved CR with olanzapine, no statistical analysis was reported. Interestingly in this report, the rates of nausea control were not improved with olanzapine.
Toxicity
The Navari et al. study used items (beyond nausea and vomiting) on the MDASI to evaluate for any treatment-related toxicities [21]. The MDASI uses 13 core symptom items and 6 items reflecting interference with daily life. This inventory is patient-reported and includes the most common symptoms found in patients with various cancers and treatment types. Symptoms are scored from 0 (not present) to 10 (most severe) on a visual analogue scale. MDASI scores were recorded on day 1 (commencing chemotherapy) and day 5. There was no significant difference between the olanzapine and aprepitant groups in any of the MDASI items. Specifically, no differences were observed in drowsiness or fatigue.
In the study by Tan et al., patients completed a quality of life questionnaire (EORTC QLQ-C30) on days 0 and 6 of chemotherapy [23]. Seventy-three percent of patients receiving olanzapine described sleepiness during chemotherapy. Severity was not described nor was the rate of sleepiness in the control group. There were no differences in patient’s weight, blood lipid nor blood glucose levels. No grade III or IV toxicities were seen. In the group receiving olanzapine, significant improvements were seen across many QoL items including global health status, emotional functioning, social functioning, fatigue, nausea and vomiting, insomnia and appetite loss when compared to the control group (p < 0.01).
In the Shumway trial, toxicity was not reported in detail [22]. Here the absence of grade III or IV toxicities is the extent of toxicity reporting.
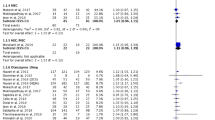
Treatment of breakthrough CINV
Patient characteristics
A total of 323 patients were included from three RCTs, all conducted by one investigator group [24–26] (see Table 2). The age range was 37 to 85 years and included 154 females and 169 males. Specific cancer diagnosis and chemotherapy regimens were not described in two trials contributing 215 patients [25, 26]. In the remaining trial of 108 patients, diagnoses included cancer of the breast (50 %), non-small cell lung (34 %), lymphoma (9 %) and bladder (6 %) [24]. Patients in this trial received HEC consisting of cisplatin (>70 mg/m2) in 41 % and AC in 59 %. In the other two trials in which patients received MEC, the specific regimens were not described.
Study design
All three trials were randomized controlled trials; however, only one trial involved double blinding [24]. The two other trials did not involve any blinding, contained three treatment arms and were only available in abstract form as conference presentations [25, 26].
Efficacy
The large double-blind trial (Navari et al. 2013) compared olanzapine with metoclopramide, one of the common drugs used for the treatment of breakthrough CINV in patients who had received HEC [24]. The primary end point for this trial was the proportion of patients with no episodes of emesis in the 72 h following initiation of study treatment. This was the only trial of the three to use single agent olanzapine (the other two trials used olanzapine in combination with dexamethasone) and was the only trial to use these end points. The other two non-blinded trials used CR (no emesis and no use of additional antiemetics) as the end point [25, 26]. Across these three trials, all end points were superior in the olanzapine-treated patients compared to control groups.
The largest double-blind study compared 10 mg daily of olanzapine with 10 mg three times daily of metoclopramide in those patients experiencing breakthrough CINV (defined as any emesis or moderate to severe nausea as indicated by >3 on the MDASI for nausea) [24]. There was a statistically significant improvement in the rate of no further emesis in the olanzapine-treated patients compared to metoclopramide (70 vs 31 %; p < 0.01) and a significantly improved rate of no nausea (68 vs 23 %; p < 0.01).
The two other studies were three-arm randomized trials in which olanzapine was given in combination with a single dose of IV dexamethasone [25, 26]. In the trial comparing olanzapine with metoclopramide and dexamethasone, the CR rates were 66, 36 and 37 %, respectively [25]. In the trial comparing olanzapine (plus single dose of dexamethasone) with metoclopramide and prochlorperazine, the complete response rate for each arm was 66, 36 and 20 %, respectively [26].
Toxicity
The large double-blind trial also used the MDASI to evaluate for any treatment-related toxicities [24]. MDASI scores were recorded on day 1 (commencing breakthrough treatment) and day 3. There were no significant differences in average MDASI scores in any item between the two treatment arms or between days 1 and 3. Specifically, scores of fatigue and drowsiness were not different between groups or days. In the two three-arm trials available as abstracts, toxicity was not reported beyond stating there were no grade III or IV treatment-related toxicities [25, 26].
Discussion
In this systematic review, we have presented the randomized clinical trial data evaluating the effect of olanzapine in the prevention and treatment of CINV. Despite the described limitations in terms of methodological rigor in the included trials, the overall weight of evidence clearly demonstrates the efficacy of olanzapine for the prevention and treatment of CINV. The results of these trials could direct optimal clinical use of olanzepine for CINV.
In all, we have included six randomized clinical trials evaluating olanzapine for CINV (three for prophylaxis and three for treating breakthrough CINV). Each of these trials demonstrated numerical superiority for the olanzapine-containing treatment compared to the non-olanzapine-containing treatment, with many of the end points reaching statistical significance. In the trials addressing CINV prophylaxis, two were well conducted and relatively large RCTs although neither involved blinding [21, 23]. The Navari et al. trial [21] is most noteworthy and generalizable to clinical practice as the control group received the current optimal prophylaxis including the potent second-generation 5-HT3 antagonist palonosetron and the NK1 receptor antagonist aprepitant. All patients received HEC, and in the investigational group, aprepitant was replaced with olanzapine. An additional benefit of the investigational protocol was that dexamethasone was not given beyond day 1 in contrast to the control group where dexamethasone was administered from days 1 to 4. The finding of a statistically significant improvement in delayed and overall nausea control in the olanzapine arm provides the strongest support for olanzapine in the prophylaxis setting. The significantly improved nausea control is particularly clinically relevant as nausea is a common and well-recognized unmet need in oncology practice.
In the treatment of breakthrough CINV, only one of the three included trials was available as a final publication [24]. In over 100 patients experiencing breakthrough CINV after HEC and optimal prophylactic antiemetic regimen, the rates of vomiting and nausea control were significantly higher in the olanzapine group compared to the metoclopramide control group. The magnitude of the difference with olanzapine treatment is noteworthy (no emesis, 70 vs 31 %; no nausea, 68 vs 23 %). Most importantly, this trial is the only double-blind RCT evaluating treatment in the breakthrough CINV setting and therefore represents the best available evidence for any specific therapeutic approach. As stated previously, international guidelines do not recommend a specific therapeutic strategy for breakthrough CINV due to the lack of high-quality evidence. Recently published National Comprehensive Cancer Network (NCCN) 2014 guidelines now include olanzapine as an option for breakthrough CINV and olanzapine, palonosetron and dexamethasone (OPD) regimen as an alternate prophylactic regimen in both HEC and MEC [27]. Given the overall paucity of trial data, ongoing clinical trials in the breakthrough CINV setting are urgently needed to define optimal current therapeutic strategies and identify novel therapies.
A further objective of this review was to evaluate the role of olanzapine in patients receiving HEC and MEC. All included trials specified whether patients received HEC or MEC, but only the three trials with complete publications detailed the specific chemotherapy regimens used (see below). The two trials with the most robust methodological quality [21, 24], and hence the strongest evidence for the efficacy of olanzapine in the prophylaxis and treatment of CINV, respectively, are in HEC-treated patients. Tan et al. was the only trial to include both HEC and MEC chemotherapy and demonstrated benefit in both groups, though the magnitude of difference was higher in the HEC-treated patients [23]. This greater absolute benefit is likely due to the higher incidence of CINV with HEC compared to MEC rather than any difference in the relative efficacy of olanzapine between the groups.
The major limitation of this current review is due to three of the included trials being available only as conference abstracts and lacking full details of methodology, patient population and toxicity [22, 25, 26]. Lack of blinding in two published trials of CINV prophylaxis [21, 23] creates a possible bias in the interpretation of the results. The paper by Tan et al. did not provide detailed numerical data on the toxicity of each treatment group, instead providing a descriptive analysis of the toxicities experienced and concluding that no higher rate of toxicity was seen in the control group compared to the investigational group and that no grade 3 or higher toxicities were reported.
In reviewing the toxicity data from the included trials, there does not appear to be any significant safety concerns of olanzapine in either setting. The daily dose of olanzapine was equivalent across all trials (10 mg daily) and ranged from 3 to 5 days in duration. Side effects of olanzapine are already well documented from use in the mental health setting for many years. Patients with psychiatric illness are treated with olanzapine at an optimal dosing of 10 mg daily indefinitely. Sedation, weight gain, increased blood glucose and cholesterol are common toxicities. Fatigue and rarely extrapyramidal side effects such as akathisia may occur [12]. With short-term use in patients receiving chemotherapy, it appears that the metabolic effects of olanzepine will be uncommon and is supported by the trials of this review. The co-administration of benzodiazepines (CNS depression) or anticholinergic medications (delirium) may cause clinically significant interactions with olanzapine and would require caution.
The intervention of olanzapine for CINV is an example of a commonly used drug with proven efficacy for an alternative indication being evaluated in a novel setting. This has the significant advantages of a well-established toxicity profile and is relatively inexpensive. Despite well-conducted clinical trials, the use of olanzapine in oncology practice has not picked up due to lack of clinician familiarity, non-inclusion in international consensus guidelines and possibly poor pharmaceutical industry support. In Australia, the cost of the OPD regimen (Australian $72) is significantly lower than the standard aprepitant, palonosetron and dexamethasone (APD) (Australian $169) when calculated using the Australian Government Pharmaceutical Benefits Scheme (PBS) dispensing price [28]. The reduced cost of this regimen has also been identified in the Japanese setting [29]. Any cost benefits to the use of olanzapine for CINV, however, should be interpreted with caution given the variability throughout geographic regions based on differing government reimbursement practices and use of generic pharmaceuticals. A cost analysis incorporated into future CINV trials would provide a more robust estimate of these differences.
Future studies in the area of CINV prophylaxis are ongoing with novel NK1 antagonists, casopitant, rolapitant and netupitant. Alternative methods of delivery of prophylactic CINV agents (transdermal patch and intranasal spray) are also being investigated. Despite the significant progress made in the past 20 years in CINV prophylaxis, the current areas of unmet need appear to be in the prevention of nausea (particularly delayed) and in treatment options of breakthrough CINV. While olanzapine appears to have a role in both of these areas, future studies in CINV are needed to focus on these outcomes with better therapeutics.
In summary, we recommend that olanzapine-containing triplet antiemetic regimen (OPD) should be added as an alternative option for the prophylaxis of CINV following moderately or highly emetogenic chemotherapy. Similarly, olanzapine is probably the drug of choice for breakthrough CINV, especially for delayed nausea (Table 3).
References
Cohen L, de Moor CA, Eisenberg P, Ming EE, Hu H (2007) Chemotherapy-induced nausea and vomiting: incidence and impact on patient quality of life at community oncology settings. Support Care Cancer 15(5):497–503. doi:10.1007/s00520-006-0173-z
Billio A, Morello E, Clarke MJ (2010) Serotonin receptor antagonists for highly emetogenic chemotherapy in adults. Cochrane Database Syst Rev 1, CD006272. doi:10.1002/14651858.CD006272.pub2
Hesketh PJ, Grunberg SM, Gralla RJ, Warr DG, Roila F, de Wit R, Chawla SP, Carides AD, Ianus J, Elmer ME, Evans JK, Beck K, Reines S, Horgan KJ, Aprepitant Protocol 052 Study G (2003) The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin—the Aprepitant Protocol 052 Study Group. J Clin Oncol 21(22):4112–4119. doi:10.1200/JCO.2003.01.095
Roila F, Herrstedt J, Aapro M, Gralla RJ, Einhorn LH, Ballatori E, Bria E, Clark-Snow RA, Espersen BT, Feyer P, Grunberg SM, Hesketh PJ, Jordan K, Kris MG, Maranzano E, Molassiotis A, Morrow G, Olver I, Rapoport BL, Rittenberg C, Saito M, Tonato M, Warr D, Group EMGW (2010) Guideline update for MASCC and ESMO in the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting: results of the Perugia consensus conference. Ann Oncol 21(Suppl 5):v232–v243. doi:10.1093/annonc/mdq194
Navari RM (2013) Management of chemotherapy-induced nausea and vomiting: focus on newer agents and new uses for older agents. Drugs 73(3):249–262. doi:10.1007/s40265-013-0019-1
Poli-Bigelli S, Rodrigues-Pereira J, Carides AD, Julie Ma G, Eldridge K, Hipple A, Evans JK, Horgan KJ, Lawson F, Aprepitant Protocol 054 Study G (2003) Addition of the neurokinin 1 receptor antagonist aprepitant to standard antiemetic therapy improves control of chemotherapy-induced nausea and vomiting. Results from a randomized, double-blind, placebo-controlled trial in Latin America. Cancer 97(12):3090–3098. doi:10.1002/cncr.11433
Schmoll HJ, Aapro MS, Poli-Bigelli S, Kim HK, Park K, Jordan K, von Pawel J, Giezek H, Ahmed T, Chan CY (2006) Comparison of an aprepitant regimen with a multiple-day ondansetron regimen, both with dexamethasone, for antiemetic efficacy in high-dose cisplatin treatment. Ann Oncol 17(6):1000–1006. doi:10.1093/annonc/mdl019
Saito M, Aogi K, Sekine I, Yoshizawa H, Yanagita Y, Sakai H, Inoue K, Kitagawa C, Ogura T, Mitsuhashi S (2009) Palonosetron plus dexamethasone versus granisetron plus dexamethasone for prevention of nausea and vomiting during chemotherapy: a double-blind, double-dummy, randomised, comparative phase III trial. Lancet Oncol 10(2):115–124. doi:10.1016/S1470-2045(08)70313-9
Aapro M, Rossi G, Rizzi G, Palmas M, Grunberg S (2013) Phase III study of NEPA, a fixed-dose combination of netupitant (NETU) and palonosetron (PALO), versus PALO for prevention of chemotherapy-induced nausea and vomiting (CINV) following moderately emetic chemotherapy (MEC). 2013 ASCO Annual Meeting Abstract LBA9514. Presented June 1st 2013
National Comprehensive Cancer Network (2013) Antiemesis Version 1.2013. www.nccn.org. Accessed 30 Apr 2013
Bymaster FP, Calligaro DO, Falcone JF, Marsh RD, Moore NA, Tye NC, Seeman P, Wong DT (1996) Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology 14(2):87–96. doi:10.1016/0893-133X(94)00129-N
Food and Drug Administration (2011) Zyprexa prescribing information. www.fda.gov. Accessed 30 Apr 2013
Rudd JA, Ngan MP, Wai MK, King AG, Witherington J, Andrews PL, Sanger GJ (2006) Anti-emetic activity of ghrelin in ferrets exposed to the cytotoxic anti-cancer agent cisplatin. Neurosci Lett 392(1–2):79–83. doi:10.1016/j.neulet.2005.08.062
Kaneishi K, Kawabata M, Morita T (2012) Olanzapine for the relief of nausea in patients with advanced cancer and incomplete bowel obstruction. J Pain Symptom Manag 44(4):604–607. doi:10.1016/j.jpainsymman.2011.10.023
Shinjo T, Okada M (2006) Olanzapine use in cancer patients for refractory vomiting. Gan To Kagaku Ryoho 33(3):349–352
Srivastava M, Brito-Dellan N, Davis MP, Leach M, Lagman R (2003) Olanzapine as an antiemetic in refractory nausea and vomiting in advanced cancer. J Pain Symptom Manag 25(6):578–582
Navari RM, Einhorn LH, Loehrer PJ Sr, Passik SD, Vinson J, McClean J, Chowhan N, Hanna NH, Johnson CS (2007) A phase II trial of olanzapine, dexamethasone, and palonosetron for the prevention of chemotherapy-induced nausea and vomiting: a Hoosier Oncology Group study. Support Care Cancer 15(11):1285–1291. doi:10.1007/s00520-007-0248-5
Navari RM, Einhorn LH, Passik SD, Loehrer PJ Sr, Johnson C, Mayer ML, McClean J, Vinson J, Pletcher W (2005) A phase II trial of olanzapine for the prevention of chemotherapy-induced nausea and vomiting: a Hoosier Oncology Group study. Support Care Cancer 13(7):529–534. doi:10.1007/s00520-004-0755-6
Passik SD, Navari RM, Jung SH, Nagy C, Vinson J, Kirsh KL, Loehrer P (2004) A phase I trial of olanzapine (Zyprexa) for the prevention of delayed emesis in cancer patients: a Hoosier Oncology Group study. Cancer Investig 22(3):383–388
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17(1):1–12
Navari RM, Gray SE, Kerr AC (2011) Olanzapine versus aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a randomized phase III trial. J Support Oncol 9(5):188–195. doi:10.1016/j.suponc.2011.05.002
Shumway NM, Terrazzino SE, Jones CB (2009) A randomized pilot study comparing aprepitant to olanzapine for treatment of chemotherapy-induced nausea and vomiting. Journal of Clinical Oncology: Annual ASCO meeting 27(15)
Tan L, Liu J, Liu X, Chen J, Yan Z, Yang H, Zhang D (2009) Clinical research of olanzapine for prevention of chemotherapy-induced nausea and vomiting. J Exp Clin Cancer Res 28:131. doi:10.1186/1756-9966-28-131
Navari RM, Nagy CK, Gray SE (2013) The use of olanzapine versus metoclopramide for the treatment of breakthrough chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy. Support Care Cancer 21(6):1655–1663. doi:10.1007/s00520-012-1710-6
Navari RM, Gray S (2010) Treatment of chemotherapy-induced breakthrough nausea and vomiting. Conference publication: 7th annual conference of the American Psychosocial Oncology Society
Navari RM, Gray SE (2009) Treatment of chemotherapy-induced breakthrough nausea and vomiting. Conference publication: 2009 annual meeting of the American Society of Clinical Oncology
National Comprehensive Cancer Network (2013) Antiemesis Version 1.2014. www.nccn.org. Accessed 12 Dec 2013
Australian Pharmaceutical Benefits Scheme (2013) Schedule of pharmaceutical benefits. www.pbs.gov.au. Accessed 12 Dec 2013
Ishiguro H, Kawaguchi K, Nishimura T, Toi M (2013) Antipsychotics-containing regimen as an alternative to standard antiemetics for delayed nausea induced by highly emetogenic chemotherapy. J Clin Oncol 31(10):1377–1378. doi:10.1200/JCO.2012.47.2951
Conflict of interest
None to declare. No funding was received for the preparation of this manuscript. We have full control of all primary data and agree to allow the journal to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hocking, C.M., Kichenadasse, G. Olanzapine for chemotherapy-induced nausea and vomiting: a systematic review. Support Care Cancer 22, 1143–1151 (2014). https://doi.org/10.1007/s00520-014-2138-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2138-y