Abstract
Purpose
This review summarizes the recommendations for the prophylaxis of acute and delayed nausea and vomiting induced by multiple-day chemotherapy, high-dose chemotherapy, and breakthrough nausea and vomiting as agreed at the MASCC/ESMO Antiemetic Guidelines update meeting in Copenhagen in June 2015.
Methods
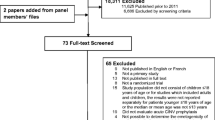
A systematic literature search using PubMed from January 01, 2009 through January 06, 2015 with a restriction to papers in English was conducted.
Results
There were three phase III randomized trials in patients undergoing high-dose chemotherapy and stem cell transplant and eight single arm non-randomized clinical studies (single in patients undergoing transplantation and one in patients receiving multiple-day chemotherapy treatment). We used a total of two randomized clinical trials in this guideline update. For patients receiving treatment for breakthrough chemotherapy-induced nausea and vomiting, a phase III randomized trial investigating the use of olanzapine versus metoclopramide in patients receiving highly emetogenic chemotherapy and a second single arm study looking at the effectiveness of olanzapine were identified.
Conclusions
It was concluded that for patients receiving high-dose chemotherapy with stem cell transplant, a combination of a 5-HT3 receptor antagonist with dexamethasone and aprepitant (125 mg orally on day 1 and 80 mg orally on days 2 to 4) is recommended before chemotherapy.
For patients undergoing multiple-day chemotherapy-induced nausea and vomiting, a 5-HT3 receptor antagonist, dexamethasone, and aprepitant, are recommended before chemotherapy for the prophylaxis of acute emesis and delayed emesis.
For patients experiencing breakthrough nausea and vomiting, the available evidence suggests the use of 10 mg oral olanzapine, daily for 3 days. Mild to moderate sedation in this patient population (especially elderly patients) is a potential problem with this agent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An international expert committee was convened during the 2015 Multinational Association of Supportive Care in Cancer (MASCC) meeting to develop consensus statements on various issues involving chemotherapy-induced nausea and vomiting (CINV). This paper is an update of the recommendations published after the last MASCC/ESMO conference in 2009 [1] and will describe the deliberations concerning multi-day chemotherapy, high-dose chemotherapy, and breakthrough CINV.
Methods
A PubMed systematic literature search was carried out for papers published between January 1, 2009 and January 06, 2015. A number of searches were made for high-dose chemotherapy and stem cell transplantation, multiple-day chemotherapy, and breakthrough nausea and vomiting. The first search consisted of (“high-dose chemotherapy” or “multiple-day chemotherapy” or “stem cell transplantation”) and (emesis or CINV or “chemotherapy-induced nausea and vomiting” or nausea) and prophylaxis. The keywords included were (high dose chemotherapy or multiple-day chemotherapy) and (emesis or CINV or chemotherapy-induced nausea and vomiting or nausea). A second search was done using the key words: (ondansetron OR granisetron OR dolasetron OR tropisetron, OR palonosetron OR ramosetron OR azasetron or metoclopramide OR domperidone OR metopimazine OR prochlorperazine OR olanzapine OR aprepitant OR fosaprepitant OR netupitant OR rolapitant OR casopitant) and (“high dose chemotherapy” or “multiple-day chemotherapy”). A third search was done using the keywords prophylaxis and nausea and vomiting and stem cell transplant. The first search resulted in 52 “hits”, the second in 25 hits, and the third in 34 hits with a total of 111 references. The search was filtered to “clinical trials”. A total of 40 references was identified. We used a total of 12 Clinical Trials in this guideline update. There are three phase III randomized trials in patients undergoing high-dose chemotherapy and stem cell transplant and eight single arm non-randomized clinical studies (seven in patients undergoing transplantation and one in patients receiving multiple-day chemotherapy treatment) [1–13].
A separate search was conducted to identify studies looking at chemotherapy-induced nausea and vomiting for germ cell tumor patients undergoing treatment with multiple-day cisplatin-based chemotherapy. In this search, three studies were identified (one phase III study and two single arm studies) [14–16].
A separate search was conducted for breakthrough nausea and vomiting using the following keywords: (ondansetron OR granisetron OR dolasetron OR tropisetron, OR palonosetron OR ramosetron OR azasetron or metoclopramide OR domperidone OR metopimazine OR prochlorperazine OR olanzapine OR aprepitant OR fosaprepitant OR netupitant OR rolapitant OR casopitant) and “breakthrough nausea” or “breakthrough vomiting”. The first search resulted in seven hits. The search was filtered to clinical trials. A total of three references were identified [17–19]. We used a total of two clinical trials and one systematic review in this guideline update. There was a phase III randomized trial investigating the use of olanzapine versus metoclopramide for the treatment of breakthrough chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy and a single arm looking at the effectiveness of olanzapine for the treatment of breakthrough chemotherapy-induced nausea and vomiting. A recent systematic review was also included [20].
Results
High-dose chemotherapy
The cause of CINV in patients treated with high-dose chemotherapy with stem cell support is multifactorial. Contributing causes include the use of prophylactic antibiotics and narcotic analgesics prescribed for concurrent mucositis management. An additional confounding factor is the use of total-body irradiation. The natural history of CINV in patients undergoing high-dose chemotherapy and stem cell transplantation is unknown. Most patients undergoing high-dose chemotherapy with stem cell support have experienced emesis with prior chemotherapy or irradiation.
Until recently, only phase II studies of a 5-HT3 receptor antagonist alone or combined with dexamethasone were published in the antiemetic literature for patients undergoing high-dose chemotherapy with stem cell support. Interpretation of phase II studies is problematic due to the multifactorial nature of CINV in this patient population. A cross comparison of phase II trials is challenging due to the various chemotherapy regimens, duration of high-dose chemotherapy, different patient populations, and tumor types included in these studies. These trials are also underpowered with a small number of patients, and clinical end points are different compared to the standard phase III antiemetic trials, making study comparison as well as interpretation very difficult. In recent years, phase III studies have been published regarding the use of modern three-drug antiemetic prophylaxis for patients undergoing high-dose chemotherapy and stem cell support. A double-blind phase III study randomized 181 patients (179 eligible) to ondansetron and dexamethasone with or without aprepitant given on each day of the high-dose preparative regimen. The study showed a significant reduction in emesis without increasing toxicity or use of rescue medication in patients receiving aprepitant. The CR rate was 82 % with the aprepitant arm versus 66 % (p < 0.001). However, there was no effect in the overall visual analog scale (VAS) for nausea [7]. Another study assessing aprepitant, palonosetron, and dexamethasone demonstrated that the combination was safe and efficacious for the prophylaxis of nausea and emesis in patients receiving high-dose BEAM (carmustine, etoposide, cytarabine, melphalan) prior to hematopoietic SCT [9]. In a study, aprepitant did not modify the pharmacokinetics of high-dose melphalan used as conditioning therapy before stem cell transplantation in patients with multiple myeloma [21]).
The efficacy of aprepitant in patients with multiple myeloma undergoing high-dose chemotherapy with autologous stem cell transplant was investigated in phase II and phase III clinical studies [3, 4]. In the phase III study, patients with multiple myeloma were randomized to receive either aprepitant administered at a dose of 125 mg orally on day 1 and 80 mg orally on days 2 to 4, granisetron (given at a dose of 2 mg orally on days 1 to 4), and dexamethasone (given at a dose of 4 mg orally on day 1 and 2 mg orally on days 2 to 3) or matching placebo, granisetron at the same dose as in the investigational arm and dexamethasone at a dose of 8 mg orally on day 1 and 4 mg orally on days 2 to 3. The high-dose chemotherapy regimen consisted of melphalan at a dose of 100 mg/m2 administered intravenously on days 1 to 2. The autologous stem cell transplant was performed on day 4. The primary end point was a complete response, defined as no emesis and no rescue therapy within 120 h of melphalan administration. A total of 362 patients were available for the efficacy analysis, with 181 in each treatment arm. The CR rate was significantly higher in the aprepitant arm compared to the control group (58 vs. 41 %; 95 % CI, 1.23 to 3.00; p = .0042). Absence of major nausea (94 vs. 88 %; 95 % CI, 1.09 to 5.15; p = .026) and emesis (78 vs. 65 %; 95 % CI, 1.25 to 3.18; p = .0036) within 120 h was significantly improved by aprepitant. The total mean Functional Living Index-Emesis (FLIE) score (±standard deviation) was 114 ± 18 for aprepitant and 106 ± 26 for placebo (p < .001) [3]. Svanberg and Birgegård randomized 96 patients to the 5-HT3 receptor antagonist, tropisetron, and dexamethasone with or without aprepitant for 7 days following HDCT and autologous SCT [2]. Thirty-eight patients in the triple therapy regimen had no vomiting compared to 16 patients in the control group, and this difference was statistically significant (p = 0.001). The authors found no significant differences with regard to nausea or use of antiemetic rescue medication between the two groups. The investigators concluded that the use of aprepitant for 7 days following HDCT and autologous SCT improved control of vomiting in these patients [2].
In summary, the control of nausea and vomiting with high-dose chemotherapy and stem cell transplantation remains a challenge. However, new phase III data supports the addition of aprepitant to a 5-HT3 receptor antagonist and dexamethasone in the management of these patients.
CINV for high-dose chemotherapy and stem cell transplantation new guideline
The addition of aprepitant to a 5-HT3 receptor antagonist and dexamethasone in the management of these patients is recommended (see Table 1).
Multiple-day chemotherapy
Multiple-day chemotherapy studies, in the present and the past, have included drugs such as dactinomycin, dacarbazine, and ifosfamide. However, as with prior consensus statements [1–20, 22], guidelines are possible only with multiple-day cisplatin in patients with germ cell tumors. Guideline updates that provide no new evidence from previous publications do not require any substantive change [23]. Previous multiple-day chemotherapy studies were incorporated in this review as well as newly published data, including a phase III study [14].
Ondansetron, the first 5-HT3 receptor antagonist, dramatically improved results preventing CINV induced by multiple-day cisplatin, etoposide, and bleomycin (PEB) for testicular cancer [24]. An older study utilizing prochlorperazine demonstrated that on day 1 of a 5-day course of cisplatin, patients experienced a median of 10 emetic episodes [25]. The most severe CINV is seen on days 3–5 as well as delayed CINV days 6–8. The first phase II study with single-agent ondansetron in 35 patients demonstrated that 77 % had no emesis on day 1, and 51 % had two or fewer episodes during the duration of chemotherapy [24]. Subsequent phase III studies documented the value of adding dexamethasone [26] or metopimazine [27]. Thus, the previous MASCC guidelines stated that “patients receiving multiple-day cisplatin should be given a 5-HT3 receptor antagonist plus dexamethasone for acute nausea and vomiting and dexamethasone for delayed nausea and vomiting “[1]. The optimal duration of dexamethasone is unknown. Some prefer to use 20 mg on days 1 and 2, no dexamethasone days 3–5, and then 4 mg orally twice daily, days 6–8 (for delayed CINV), whereas others have incorporated dexamethasone for eight consecutive days. Acute and chronic toxicity with dexamethasone includes hiccups, insomnia, hyperglycemia, gastroesophageal reflux disease, agitation, and acne [28]. A greater concern is the potential for late toxicity. Four of 47 patients (9 %) receiving multiple-day cisplatin for metastatic testicular cancer developed avascular necrosis of the hip [29].
The optimal 5-HT3 receptor antagonist is also unknown, due to a lack of randomized comparative studies. One option is to use palonosetron 0.25 mg IV on days 1, 3, and 5 [30].
Aprepitant is the first neurokinin (NK)1 receptor antagonist to be utilized for CINV. In the Hoosier Oncology Group, a phase III study was conducted with a 5-HT3 receptor antagonist plus dexamethasone plus either aprepitant (125 mg on day 3 and 80 mg days 4–7) or placebo in a randomized, double-blind placebo-controlled study in 69 patients. The CR rate was 42 versus 13 % (p < 0.001) favoring aprepitant. Forty-seven percent had at least one emetic episode with the placebo arm versus 16 % with aprepitant (p < 0.001). Patients served as their own control in this double-blinded cross-over study. Thirty-eight patients preferred the aprepitant cycle and 11 placebo (p < 0.001). The VAS for nausea was better, but not significantly superior with the aprepitant arm [14]. Confirmatory supportive evidence with aprepitant was seen in phase II trials conducted in Australia [15] and Japan [16].
Multiple-day cisplatin chemotherapy new guidelines
Patients receiving multiple-day cisplatin should receive a 5-HT3 receptor antagonist, dexamethasone, and aprepitant for acute nausea and vomiting and dexamethasone for delayed nausea and vomiting. Some prefer to use aprepitant in both acute and delayed nausea and vomiting (aprepitant days 3–7 during a day 1–5 chemotherapy regimen) (see Table 1).
Breakthrough nausea and vomiting
Drugs used to treat CINV should be administered prior to starting chemotherapy to attempt to prevent or mitigate nausea and emesis. Breakthrough nausea and vomiting is defined as nausea and vomiting during chemotherapy in spite of prophylaxis with guideline-directed antiemetics. Several decades ago, chemotherapy-induced emesis was the major concern for patients, family members, and practitioners. The definition of complete remission, in most older and recent studies, is defined as no emetic episodes and no use of rescue medication. Some studies separately incorporate a VAS with ratings of zero (no nausea) to 100-mm worse possible nausea) in an attempt to assess nausea. Today, nausea, during chemotherapy and for several subsequent days, rather than emesis, is the most prevalent problem. Furthermore, VAS merely provides a qualitative assessment of nausea and fails to take into account the duration of nausea.
Clinicians should be aware that persistent nausea and vomiting might be due to causes other than chemotherapy. CNS metastases, azotemia, hepatic metastases, hypercalcemia, gastrointestinal outlet obstruction, or narcotic analgesics can be confounding factors.
Treatment of breakthrough CINV
Olanzapine is one of the few agents evaluated in randomized studies. Navari et al. published data on 276 patients treated with highly emetogenic chemotherapy [17]. All patients received prophylaxis with palonosetron 0.25 mg intravenously (IV) plus fosaprepitant 150 mg IV and dexamethasone 12 mg IV day 1 and 8 mg orally days 2–4. Breakthrough nausea and vomiting were observed in 108 evaluable patients who were then randomized to either olanzapine 10 mg orally for 3 days versus a low dose of metoclopramide, 10 mg orally three times daily for 3 days. This reduced dosage has not been demonstrated to be effective. However, the European Medicine Agency mandated this lowered dosage to lessen neurotoxicity. Patients were monitored for 72 h after randomization to assess effectiveness in the treatment of breakthrough CINV. Thirty-nine of 56 (70 %) on olanzapine versus 16 of 52 (31 %) on metoclopramide experienced no further emesis during the 72-h observation period (p < 0.01). Furthermore, 68 % had no nausea with olanzapine compared with 23 % with metoclopramide (p < 0.01). Olanzapine was associated with mild to moderate sedation [17]. Supportive phase II data was published by Chanthawong et al. [18] as well as a systematic review by Hocking et al. [20].
Breakthrough CINV new guideline
A different class of antiemetic agent from the agents used for prophylaxis is recommended. The available evidence for breakthrough nausea and vomiting suggests the use of 10 mg oral olanzapine daily for 3 days. The mild to moderate sedation in this patient population, especially elderly patients, is a potential problem with olanzapine (see Table 1).
Conclusions
Only a few studies have been published on the prophylaxis of acute and delayed nausea and vomiting induced by high-dose chemotherapy, multiple-day chemotherapy, and breakthrough nausea and vomiting since the 2009 consensus conference. Major advances occurred in the last 5 years regarding the management of these patients. Aprepitant is now recommended for the prophylaxis of acute and delayed nausea and vomiting in patients undergoing both high-dose chemotherapy with stem cell transplant and multiple-day chemotherapy. Olanzapine is now incorporated in the treatment of breakthrough nausea and vomiting. While prophylaxis of vomiting is fairly well managed; nausea remains an unmet medical need. Future studies should concentrate on improving nausea control in these three patient subsets. Randomized trials incorporating olanzapine are indicated looking at nausea as the primary end point.
References
Einhorn LH, Grunberg SM, Rapoport B et al (2011) Antiemetic therapy for multiple-day chemotherapy and additional topics consisting of rescue antiemetics and high-dose chemotherapy with stem cell transplant: review and consensus statement. Support Care Cancer 19(Suppl 1):S1–S4
Svanberg A, Birgegård G (2015) Addition of aprepitant (Emend®) to standard antiemetic regimen continued for 7 days after chemotherapy for stem cell transplantation provides significant reduction of vomiting. Oncology 89:31–36
Schmitt T, Goldschmidt H, Neben K et al (2014) Aprepitant, granisetron, and dexamethasone for prevention of chemotherapy-induced nausea and vomiting after high-dose melphalan in autologous transplantation for multiple myeloma: results of a randomized, placebo-controlled phase III trial. J Clin Oncol 32:3413–3420
Bechtel T, McBride A, Crawford B et al (2014) Aprepitant for the control of delayed nausea and vomiting associated with the use of high-dose melphalan for autologous peripheral blood stem cell transplants in patients with multiple myeloma: a phase II study. Support Care Cancer 22:2911–2916
Sakurai M, Mori T, Kato J et al (2014) Efficacy of aprepitant in preventing nausea and vomiting due to high-dose melphalan-based conditioning for allogeneic hematopoietic stem cell transplantation. Int J Hematol 99:457–462
Uchida M, Ikesue H, Miyamoto T et al (2013) Effectiveness and safety of antiemetic aprepitant in Japanese patients receiving high-dose chemotherapy prior to autologous hematopoietic stem cell transplantation. Biol Pharm Bull 36:819–824
Stiff PJ, Fox-Geiman MP, Kiley K et al (2013) Prevention of nausea and vomiting associated with stem cell transplant: results of a prospective, randomized trial of aprepitant used with highly emetogenic preparative regimens. Biol Blood Marrow Transplant 19:49–55
Pielichowski W, Gawronski K, Mlot B et al (2011) Triple drug combination in the prevention of nausea and vomiting following busulfan plus cyclophosphamide chemotherapy before allogeneic hematopoietic stem cell transplantation. J Buon 3:541–546
Pielichowski W, Barzal J, Gawronski K et al (2011) A triple-drug combination to prevent nausea and vomiting following BEAM chemotherapy before autologous hematopoietic stem cell transplantation. Transplant Proc 43:3107–3110
Giralt SA, Mangan KF, Maziarz RT et al (2011) Three palonosetron regimens to prevent CINV in myeloma patients receiving multiple-day high-dose melphalan and hematopoietic stem cell transplantation. Ann Oncol 22:939–946
Rzepecki P, Pielichowski W, Oborska S et al (2009) Palonosetron in prevention of nausea and vomiting after highly emetogenic chemotherapy before haematopoietic stem cell transplantation-single center experience. Transplant Proc 41:3247–3249
Paul B, Trovato JA, Thompson J et al (2010) Efficacy of aprepitant in patients receiving high-dose chemotherapy with hematopoietic stem cell support. J Oncol Pharm Pract 16:45–51
Musso M, Scalone R, Crescimanno A et al (2010) Palonosetron and dexamethasone for prevention of nausea and vomiting in patients receiving high-dose chemotherapy with auto-SCT. Bone Marrow Transplant 45:123–127
Albany C, Brames MJ, Fausel C et al (2012) Randomized, double-blind, placebo-controlled, phase III cross-over study evaluating the oral neurokinin-1 antagonist aprepitant in combination with a 5HT3 receptor antagonist and dexamethasone in patients with germ cell tumors receiving 5-day cisplatin combination chemotherapy regimens: a Hoosier Oncology Group Study. J Clin Oncol 30:3998–4003
Olver I, Grimson P, Chatfield M et al (2013) Results of a 7-day aprepitant schedule for the prevention of nausea and vomiting in a 5-day cisplatin-based germ cell tumor chemotherapy. Support Care Cancer 21:1561–1568
Hamada S, Hinotsu S, Kawaj K et al (2014) Antiemetic efficacy and safety of a combination of palonosetron, aprepitant and dexamethasone in patients with testicular germ cell tumor receiving 5-day cisplatin-based combination chemotherapy. Support Care Cancer 22:2161–2166
Navari RM, Nagy CK, Gray SE (2013) The use of olanzapine versus metoclopramide for the treatment of breakthrough chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy. Support Care Cancer 21:1655–1663
Chanthawong S, Subongkot S, Sookprasert A (2014) Effective of olanzapine for the treatment of breakthrough chemotherapy-induced nausea and vomiting. J Med Assoc Thail 97:349–355
Vig S, Seibert L, Green MR (2014) Olanzapine is effective for refractory chemotherapy-induced nausea and vomiting irrespective of chemotherapy emetogenicity. J Cancer Res Clin Oncol 140:77–82
Hocking CM, Kichenadasse G (2014) Olanzapine for chemotherapy-induced nausea and vomiting: a systematic review. Support Care Cancer 2014(22):1143–1151
Egerer G, Eisenlohr K, Gronkowski M et al (2010) The NK(1) receptor antagonist aprepitant does not alter the pharmacokinetics of high-dose melphalan chemotherapy in patients with multiple myeloma. Br J Clin Pharmacol 70:903–907
Einhorn LH, Rapoport B, Koeller J et al (2005) Antiemetic therapy for multiple-day chemotherapy and high dose chemotherapy with stem cell transplant: review and consensus statement. Support Care Cancer 13:112–116
Somerfield MR, Einhaus K, Hagerty KL et al (2008) ASCO clinical practice guidelines: opportunities and challenges. J Clin Oncol 26:4022–4026
Einhorn LH, Nagy C, Werner K et al (1990) Ondansetron: a new antiemetic for patients receiving cisplatin chemotherapy. J Clin Oncol 8:731–735
Herman TS, Einhorn LH, Jones SE et al (1979) Superiority of nabilone over prochlorperazine as antiemetics in patients receiving chemotherapy. N Engl J Med 300:1295–1297
Fox SM, Einhorn LH, Cox E et al (1993) Ondansetron versus ondansetron, dexamethasone and chlorpromazine in the prevention of nausea and vomiting associated with multiple-day cisplatin chemotherapy. J Clin Oncol 11:2391–2395
Herrstedt J, Sigsgaard TC, Nielsen HA et al (2007) Randomized, double-blind trial comparing the antiemetic effect of tropisetron plus metopimazine with tropisetron plus placebo in patients receiving multiple cycles of multiple-day cisplatin-based chemotherapy. Support Care Cancer 15:417–426
Vardy J, Chiew KS, Galica J et al (2006) Side effects associated with the use of dexamethasone for prophylaxis of delayed emesis after moderately emetogenic chemotherapy. Br J Cancer 94:1011–1015
Cook AM, Dzik-Jurasz ASK, Padhami AR et al (2001) The prevalence of avascular necrosis in patients treated with chemotherapy for testicular tumors. Br J Cancer 85:1624–1626
Einhorn LH, Brames MJ, Dreicer R et al (2007) Palonosetron plus dexamethasone for prevention of chemotherapy-induced nausea and vomiting in patients receiving multiple-day cisplatin chemotherapy for germ cell cancer. Support Care Cancer 15:1293–1300
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Lawrence H. Einhorn
Amgen: Stock Options
Biogenidec: Stock Options
Bernardo L. Rapoport
Merck and Co: Receipt of grants/research supports, receipt of honoraria or consultation fees and participation in a company sponsored speaker’s bureau
Tesaro Inc.: Receipt of grants/research supports, receipt of honoraria or consultation fees and participation in a company sponsored speaker’s bureau
Herron Therapeutics: Receipt of honoraria or consultation fees
Rudolph M. Navari
The author declares that he has no competing interests.
Jørn Herrstedt
Tesaro Inc.: Consultant Tesaro and remuneration SOBI
Mary J. Brames
The author declares that she has no competing interests.
Rights and permissions
About this article
Cite this article
Einhorn, L.H., Rapoport, B., Navari, R.M. et al. 2016 updated MASCC/ESMO consensus recommendations: prevention of nausea and vomiting following multiple-day chemotherapy, high-dose chemotherapy, and breakthrough nausea and vomiting. Support Care Cancer 25, 303–308 (2017). https://doi.org/10.1007/s00520-016-3449-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3449-y