Abstract
Purpose
To examine the feasibility of a breast cancer-related lymphoedema (BCRL) screening programme. Additionally, to investigate the efficacy of bioimpedance analysis (BIA) compared to circumferential measurements (CM) in detecting BCRL.
Methods
This was a 12-month prospective feasibility study. Participants were recruited from two diagnostic breast clinics and consented to be screened for BCRL. Pre-surgical assessments were conducted, and participants were followed up at quarterly intervals. BIA and CM measurements were conducted at all time points. An L-Dex score of >10 or a 10-U increase from baseline or a ≥5 % increase in proximal, distal or total percentage volume difference (PVD) from baseline was indicative of BCRL. Information was collected on subjective symptoms, potential risk factors, demographics and medical data. Feasibility was based on uptake and retention.
Results
One hundred twenty-six participants were recruited with an attrition rate of 16.2 %. Participants’ mean age was 59 years with the majority having stage I (63.9 %), infiltrating ductal carcinoma (87.4 %). 31.6 % were identified as having BCRL, 90.3 % detected by CM and 35.5 % by BIA (p = ≤0.0001). We found no significant correlation between BIA and CM. Participants identified as having BCRL had a higher BMI, a recent injury to their ‘at-risk’ arm and more lymph nodes excised (p = <0.05). These findings were not evident across all time points. A large percentage of participants had transient BCRL when assessed by a lymphoedema physiotherapist.
Conclusions
BCRL screening is acceptable and valued by breast cancer survivors. Work needs to continue to establish the most effective screening tool and the natural behaviour of BCRL within the first-year post-surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common female cancer worldwide [1] with approximately 48,988 new cases diagnosed annually within the UK [2] and 1.38 million worldwide [1]. Survival rates are steadily increasing; thus, issues surrounding cancer survivorship are much the focus of current research [3] and clinical practice. Breast cancer-related lymphoedema (BCRL) is one of the most common and dreaded complications of breast cancer treatment. It is an accumulation of protein-rich fluid in the interstitial spaces of the arm, due to a reduction in lymph transport capacity, secondary to cancer and its treatment [4]. BCRL is a chronic condition which impacts negatively on quality of life [5, 6], developing any time post-surgery, although the majority (70–80 %) present within the first year [7, 8]. The true incidence of lymphoedema is notoriously difficult to quantify due to the lack of standardised diagnostic criteria, assessment methodology [9] and associated risk factors. Incidence rates of 21.4 % have been reported [10], extrapolating to 10,483 breast cancer survivors in the UK and 295,320 worldwide who will develop BCRL.
Early detection and treatment are vital in reversing or slowing the progression of BCRL [11], proving to be cost-effective by reducing complications and the need for intensive treatment [12]. Despite this and the promotion of surveillance programmes [11], BCRL screening is not commonplace. This notwithstanding, before BCRL screening, can be widely implemented, we need to establish its feasibility, appropriate screening tools and the cohort that should be targeted.
Upper limb circumferential measurement (CM) has commonly been used as a diagnostic tool and outcome measure [10]. CM can be used to compute relative limb volume difference, comparing the surgically ipsilateral arm with the contralateral arm. This method is ideal as it is not reliant on physique [13] and has minimal associated cost. While Taylor et al. [14] state that CM is a reliable and valid measurement of BCRL, others question its sensitivity [15]. This debate, in part, may be due to the lack of a standardised approach. Studies have measured at one fixed point on the upper arm only [16]; others have used a fixed point on both the upper and forearm [17–19]. Few have taken multiple anatomical measurements of the whole arm [20], which is likely to give a more accurate calculation of limb volume [14]. Diagnostic criteria is also inconsistent, with some studies using CM differences of >1 to ≥5 cm as an indication of BCRL, while others use volume differences ranging from >150 ml to >200 ml and percentage volume differences (PVD) between 3 and 20 % [21–23, 10].
Bioimpedance analysis (BIA) has been developed for the assessment of lymphoedema, comparing the surgically ipsilateral arm with the contralateral arm, generating an L-Dex™ score (normal range −10 to +10). It is proposed that BIA can differentiate between extracellular fluid and total limb volume [21]. BIA has been reported as a reliable measure of BCRL [22, 23] with excellent sensitivity and specificity [24]. Studies claim BIA to be four times more sensitive than CM [25]; others report no advantage [26].
Little research exists in relation to BCRL screening programmes and those that do have varied aims. Specht et al. [27] utilised a screening programme to explore interventional thresholds for patients with BCRL, while others focused on treatment outcomes/surveillance models [28]. To our knowledge, this is the first to report on the feasibility of a clinical BCRL screening programme. Additionally, the efficacy of advocating one screening tool over another has yet to be established, and the evidence-base is limited, inconclusive and perhaps marred by the issues outlined earlier. We also aim to investigate the efficacy of single frequency BIA compared to upper limb CM in identifying early BCRL and factors which may influence its development.
Methods
Design, setting and participants
This was a 12-month prospective feasibility study which was approved by the Office for Research Ethics Committee, Northern Ireland, and Research Governance within both the Belfast and South Eastern Health and Social Care Trusts. The research was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Women, aged 18–99 years, newly diagnosed with stages I–III unilateral breast cancer, were eligible. Exclusions are listed in Table 1. Participants were recruited between April and December 2012 from specialist diagnostic breast clinics at the Belfast City Hospital and Ulster Hospital, Dundonald. Patients were screened for eligibility by their breast care team, and those suitable were informed of the study and given a participant information sheet. Interested individuals were followed up by the principle investigator (JB). Those agreeable to take part provided written informed consent, and participants’ GPs were informed of their involvement. Figure 1 outlines participants’ flow through the study.
Data collection and outcome measures
Baseline assessments were conducted prior to surgery and repeated 3, 6, 9 and 12 months later. All assessments were carried out by the same individual (JB) and included upper limb CM and BIA. BMI, subjective BCRL symptoms and risk factors were also assessed (including, BP/venipuncture taken on ipsilateral arm, cording, decreased range of movement). Demographic, medical and treatment information was collected using an investigator-developed questionnaire and participants’ medical records. Assessments lasted approximately 25–30 min.
CM of the ipsilateral (surgical) and contralateral arms were measured using a retractable, flexible tape measure (cm). Distance from the nail bed of the middle finger to the mid-position of the radial and ulnar bones was measured in zero degrees flexion. This was the starting position of the first arm measurement and then sequentially every 4 cm to the approximate level of the axilla. Proximal, distal and total volume differences (ml and %) were computed (ipsilateral arm vs. contralateral) using LymCalc™ (Haddenham Healthcare Ltd, UK). A ≥5 % increase in participants’ proximal, distal or total percentage volume difference (PVD) from baseline was indicative of lymphoedema [29]. This ≥5 % PVD relates to absolute volume difference as a percentage of the ipsilateral arm (at-risk arm) versus the contralateral arm (not at-risk arm).
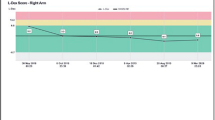
BIA was conducted using ImpediMed XCA® (ImpediMed, Brisbane, Australia) single frequency (<30 kHz) bioimpedance analyser. An L-Dex score of >10 or a 10 U increase from baseline was indicative of lymphoedema [30]. Manufacturer guidelines were adhered to for patient preparation and positioning of single-tab electrodes. Two electrodes were placed on each arm, one on the dorsum of the wrist at the level of the radial and ulnar bones and a second 5 cm distally (midline to midline of electrode tabs). The final electrode placement was on the dorsum of the right foot, 1 cm from the base of the third metatarsal.
Any participants identified by PVD or BIA cut-offs were referred to their local physiotherapy lymphoedema service for assessment and management.
Statistical analysis
Feasibility was measured by recruitment, uptake and retention. McNemar’s test examined the percentage of participants identified as having lymphoedema by CM and BIA. Partial correlation was used to explore the relationship between BIA and PVD, controlling for BMI and age. Independent samples t tests (or non-parametric equivalent) examined continuous data differences between participants identified as having lymphoedema and those who were not. Categorical data was analysed using chi-square. Statistical significance was set at p = ≤0.05 level. Data was analysed using SPSS, version 18 (Chicago, IL, USA).
Results
Recruitment, attrition and participants
One hundred ninety-three patients were screened for eligibility (Table 1). One hundred forty-seven (76.2 %) met the criteria and 126 (85.7 %) patients consented. Nine (7.1 %) participants’ data were excluded from analysis as it emerged post-baseline assessment that n = 4 had stage IV disease, n = 2 had ductal carcinoma in situ, n = 1 reported pre-operative upper limb swelling and n = 2 were identified as having lymphoedema external to the screening programme. Attrition was 16.2 % (n = 19; Table 1): 10.5 % withdrew prior to undertaking baseline assessment, 36.8 % before 3-month follow-up (MFU), 31.6 % before 6 MFU, 5.3 % before 9 MFU and 15.8 % prior to 12 MFU. No significant differences existed between those who were retained and withdrew in relation to age, BMI, cancer stage, socioeconomic status or distance from home to hospital.
Table 2 describes participant characteristics and treatment received. Mean age at baseline was 59.2 years (±12.8, range 30–89) and 33 % were classed as overweight and 30.7 % obese (World Health Organisation Classification). 87.4 % had infiltrating ductal carcinoma, 34.8 % had a mastectomy and 58.8 % sentinel lymph node dissection (SLND). The median number of lymph nodes dissected within the total cohort was 5 (interquartile range (IQR) 13; range 1–38). 78.2 % had radiotherapy, 39.1 % had chemotherapy and 33.3 % were treated with both chemotherapy and radiotherapy.
Baseline percentage volume difference and L-Dex scores
The mean total PVD was 0.24 % (±4.3 %), distal PVD was −0.13 % (±4.7 %) and proximal PVD was 0.52 % (±5.0 %). Categorically, 11.3 % of participants had a total PVD ranging between −9.9 and −5.0 % and 40.9 % between −4.9 and 0 %; 31.3 % that fell in to the category of 0.1 to 4.9 % and 16.5 % were between 5.0 and 9.9 % at baseline. The mean baseline L-Dex score was 0.1 (±4.0). 7.8 % of participants’ L-Dex scores were between −9.9 and −5.0 U, 44.3 % between −4.9 and 0 U, 34.2 % between 0.1 and 4.9 U and 13.7 % between 5.0 and 9.9 U.
Lymphoedema
During the study, 31.6 % (n = 31/98) of participants who were screened over a 12-month period were identified as having lymphoedema based on CM or BIA (Table 3). Incidence rates based on CM were 28.6 and 11.2 % based on BIA. Median time from surgery to BCRL identification was 22 weeks (IQR 24; range 10–55 weeks), with the majority being identified at 3 MFU (41.9 %) and 6 MFU (29.0 %). 90.3 % of participants were identified by CM, 35.5 % by BIA (p = ≤0.0001). There was agreement between the two measures in 25.8 % of cases.
In 50.0 %, only the proximal segment of the ipsilateral arm was affected and for 28.5 %, only the distal segment (Table 3). A ≥5 % difference in both distal and proximal segments only affected 21.4 % of participants. Table 3 also details the average L-Dex difference from baseline (DFB) score and distal, proximal and total PVDs from baseline across all time points. As before and with the exception of 9 MFU, there is a general trend towards proximal PVD being greater than distal.
Just over one third (n = 11) of the participants identified as having lymphoedema reported subjective symptoms. There were no significant differences in distal (4.4, 4.4; p = 0.97), proximal (6.8, 5.0; p = 0.31) or total (5.8, 4.8; p = 0.39) PVD in those who reported subjective symptoms and those who did not. This was similar of L-Dex DFB scores (12.7, 16.1; p = 0.29).
Table 4 details the partial correlation analysis between distal, proximal, total PVD and L-Dex DFB scores across time points and for the total cohort. Analysis demonstrates that there is a lack of consistency regarding the relationship between BIA and PVD, with a mixture of positive and negative r-values. These were not statistically significant.
At 3 MFU (Table 5), those identified as having lymphoedema had a significantly higher BMI (32.7, 25.9; p = 0.004), and a significantly higher proportion reported an injury to their surgical arm (15.4 %, 1.1 %; p = 0.04). These findings however were not apparent across time; in fact, there were no significant differences found between groups at 6 MFU or at 9 MFU. At 12 MFU, a significantly higher percentage of participants in the BCRL group had either axillary lymph node dissection (ALND; 50.0 % vs. 22.4 %) or both SLND followed by ALND (50.0 vs. 11.9 %; p = 0.02) and had significantly more lymph nodes removed (n = 18 vs. n = 4; p = 0.02).
PICC line
Coincidentally during follow-up assessments, we noted that on average, participants who had a peripherally inserted central catheter (PICC) line in situ had significantly lower BIA DFB scores than those who did not. That is, their ‘at-risk’ arm had decreased in terms of extracellular fluid compared to the contralateral/PICC arm. At 3 MFU, median BIA DFB scores for those with a PICC (n = 27) were −1.40 (IQR 3.6) compared with 1.00 (IQR 4.2) for those without (p = <0.0001). These findings were not significant at 6, 9 or 12 MFU; however, sample sizes were very small (n = 7, n = 3, n = 3, respectively) as most PICC lines were redundant post-chemotherapy. There were no significant differences in PVD between these groups.
Follow-up
Any of the participants that reached the CM or BIA cut-offs at any of the assessment time points (3, 6, 9 or 12 months) were referred to the specialist lymphoedema team for further assessment and management. Over the course of the study, a total of 31 participants were identified by either CM or BIA and referred on. Several of these lymphoedema therapists brought it to the research teams’ attention that some patients, when re-assessed, were below cut-offs or near baseline measurements. As a result, we were able to obtain follow-up information for 27 of the 31 participants that were referred. The mean time from referral to being assessed by a lymphoedema specialist was 4.8 weeks (±20.1). At their first lymphoedema assessment, 14/27 (51.8 %) patients’ measurements had returned to approximate baseline/below cut-off. These patients were monitored by the lymphoedema team. We were able to further follow up on 10/14 patients and at their 6-month review with the lymphoedema team. Six of these patients continued to have no evidence of lymphoedema, three had been treated for lymphoedema and one patient declined follow-up assessment.
Discussion
To our knowledge, this was the first prospective BCRL screening programme to examine feasibility within a clinical setting. We also investigated the efficacy of single frequency BIA (10-U increase from baseline values or outside the normal range of +10 U) compared to CM (≥5 % volume increase from baseline) in identifying early BCRL and factors associated with lymphoedema development.
High recruitment (85.7 %) and retention (83.8 %) rates indicate that breast cancer survivors are interested and value such a programme. Common reasons for declining or withdrawing from the study were related to time and travel. We aimed to accommodate participants with convenient follow-up assessments, and this is perhaps one reason that a high retention rate was achieved. It further highlights that screening programmes could be incorporated within patient pathways. Programmes introduced as part of routine care can increase acceptance among breast cancer survivors [31].
It is difficult to evaluate our uptake and attrition as similar studies have often failed to report these [27, 28]. However, Kilbreath and colleagues [32] utilised BCRL screening as part of the design of their intervention RCT and reported retention rates of 88 %. A prospective observational study [7] reported recruitment and retention rates of 85.1 and 74.9 %, respectively. Based on these figures, our study compares favourably. In terms of eligibility, 23.8 % of those screened were excluded. These exclusions may not all be valid in clinical practice, and thus, more patients could benefit from screening. This notwithstanding, due to safety issues, BIA cannot be used in patients with a cardiac device or metal implant and, due to fluid fluctuations, may not be reliable in patients with renal or heart failure and pregnant women.
Participants’ baseline volume measurements (total PVD −0.3 %, IQR 5.4 %, range −9.7 % to 9.9 %) and L-Dex scores (0, IQR 5.1, range −9.7 to 9.9) were diverse and reiterate the importance of pre-surgical quantification of inter-limb variance in achieving an accurate and early diagnosis of BCRL [28, 32]. Few participants in our study had zero PVD between arms or indeed BIA score at baseline. Thus, using our PVD and BIA cut-offs without baseline comparisons would risk a large percentage of participants being undiagnosed or misdiagnosed, both of which could have significant implications on quality of life and psychological well-being. However, it is uncertain as to whether or not it is possible to obtain true baseline values. Physiologically, it is conceivable that metastatic spread to the axillary lymph nodes could disrupt lymphatic drainage prior to surgery. Our findings suggest that this is feasible as 16.5 % of participants had a total PVD of between 5 and 10 % at baseline and 13.7 % had L-Dex scores between 5 and 10 U. While further exploration is warranted, two recent studies indicate that pre-surgical inter-limb differences are mainly related to limb dominance and not that of cancer side or level of nodal involvement [32, 33].
Overall, BCRL incidence was 31.6 %, with just over one third reporting subjective symptoms. Based on PVD, incidence rates were 28.6 and 11 % for BIA. Studies using similar PVD cut-offs have reported incidence rates of 20.7–67.7 % [7, 34]. In terms of BIA, rates have ranged from 33 to 40 % [8, 26]. A systematic review and meta-analysis detailed the huge variation by study design, measurement method, surgery and study location [10]. The authors report an incidence rate of 21.4 % from prospective cohort studies and incidence rates of 15.9 % for those diagnosed by BIA and 14.8 % for those identified by CM.
We considered both segmental and total PVD in assessing lymphoedema which may explain our higher incidence rate. Our findings demonstrate that BCRL can be present in isolation in distal or proximal segments which may not be identified if only calculating total PVD. Stout et al. [35] echo our findings and acknowledge that using total PVD may not be sufficiently sensitive for screening purposes. Likewise, lymphoscintigraphy has demonstrated that drainage pathways do not run in a direct, progressive manner and that segmental variations exist [36]. Future studies and clinicians should consider these findings.
In our study, of the 28 participants that were identified with PVD, 8 (28.6 %) of these patients were also identified by BIA. Similarly, other studies report varying degrees of detection. Hayes et al. [37] found that of the cases identified by BIA, only 35 % were detected using CM. Similar findings were reported in a later study [8]. These studies however did not obtain baseline measures, which, as previously outlined, is imperative for an accurate diagnosis [9, 28]. Box et al. [26] found BIA to have a 67 % detection rate compared to limb volume difference. In terms of advocating one measurement technique over another, our findings should be considered with care, as our study did not take into account upper limb dominance. We recognise this as a limitation of our study when comparing the two measurement techniques for BCRL screening, especially as BIA does account for dominance.
Our findings further show that distal, proximal and total PVD are not significantly correlated with BIA. Fu and colleagues [38] did find that BIA and CM were correlated, but the authors did not control for BMI or age, even though they report that L-Dex scores showed positive trends with BMI. Within their study, the authors acknowledge that there is no existing data to support the sensitivity and specificity of BIA using an L-Dex score of greater than +10 as a diagnostic cut-off point, and this criterion misses 34 % of true BCRL cases [38]. However, while lowering the L-Dex cut-off to greater than +7.1 (approx impedance ratio of 1.108 or a cut-off point approximately equivalent to the mean +2 SD), BIA was able to identify 80 % of true lymphoedema cases but still produced false negatives for 20 %. It should however be highlighted that this cross-sectional study compared healthy females, cancer survivors at risk of BCRL and those diagnosed with BCRL; thus, no baseline data was available for each group which is a major limitation of their findings. Additionally, the BCRL cohort was only eligible if treated for lymphoedema at least 6 months prior to enrolment. It is recognised that BIA may not be suitable for assessing established lymphoedema due to the changes that can occur within the tissues [38]. Furthermore, the authors compare BIA with CM as the reference/gold standard. As with our study, it should be highlighted that a gold standard approach for BCRL identification and screening has yet to reach consensus. Additional research is highly warranted to explore the discrepancies outlined in our study and those by Fu et al. [38] to establish the best screening tool, measurement protocol and CM and BIA cut-offs that are reliable for early-stage detection and screening. Future studies should also explore the impact PICC line insertions in the contra-lateral arm may have on the BIA results and thus establish if our findings are noteworthy. PICC line insertions can cause phlebitis and inflammation within the tissues [39] and could explain the high percentage of cases that went undetected by BIA.
Our sample size was not large enough across time points to enable a regression analysis of BCRL risk factors. However, patients with lymphoedema had significantly higher BMI; higher proportions had a recent injury to the ipsilateral arm and more lymph nodes excised. Although these findings were not consistent across time points, they have been reported elsewhere. A meta-analysis of treatment-related risk factors found that ALND significantly increases patients’ risk of developing BCRL [40]. Like us, many studies have reported high BMI/obesity as a BCRL risk factor [6, 10, 38, 41–43].
We were able to follow-up on 27 participants who were identified as having BRCL and referred on from our study to a specialist lymphoedema service. Just over half (n = 14) of these patients had returned to approximate baseline measurements or below cut-offs when assessed by a lymphoedema therapist. Information was available for ten of these patients at their 6-month specialist review, and six continued to have no evidence of lymphoedema. It is reported that the majority of BCRL cases present within the first year [7, 8]; however, our findings suggest that a large proportion of these may be transient. Kilbreath and colleagues [32] conducted a secondary analysis of an intervention RCT whereby patients at risk of lymphoedema were randomised into an exercise programme or a control. They found that 15 participants had elevated extracellular fluid at 3 MFU, but only 8 remained elevated at 9 MFU and only 4 at 15 MFU. Similarly, a longitudinal study by Hayes et al. [8] found that 58 % had transitory lymphoedema, while other research found 23 % to experience mild lymphoedema that was transient in nature [44]. In all three studies, percentages of participants had received an intervention, and in two, participants did not have pre-surgical measurements [8, 44]. Considering the methodological issues in the aforementioned studies and as we were not able to follow up on all participants and over a longer period of time, further research is warranted to investigate the nature of lymphoedema in the first-year post-surgery and establish the incidence of true lymphoedema cases.
Although BCRL is defined as a chronic, progressive condition, our results and that of existing evidence [8, 32, 44] demonstrate that for some, oedema within the first-year post-surgery may be temporary and fluctuate as part of the natural treatment process. Taxane-based chemotherapy has been documented to cause generalised swelling [28]. These findings thus contest our thinking and further complicate BCRL screening, diagnosis and treatment. Giving a patient a diagnosis of BCRL is not to be taken without due consideration as the diagnosis itself and the subsequent management can impact greatly on quality of life and cause psychological distress [5, 6, 45]. Nonetheless, a delayed diagnosis could have a more significant bearing on overall quality of life, and treatment outcome as lymphoedema that has progressed beyond an early stage can often require more intensive management. Again, the best approach has yet to be established.
Conclusion
A screening programme is acceptable by breast cancer patients within the first-year post-surgery. However, we are still some way from fully understanding the natural behaviour of BCRL within this timeframe and how this should be managed as well as definitive risk factors. As it stands, we are yet to agree a definition of what constitutes early-stage lymphoedema as well as the best screening tool. Ours was a feasibility study with relatively small numbers, and dominance was not accounted for using CM. Larger well-designed research methodologies are required to explore this further. Addressing these issues will significantly progress our knowledge, clinical diagnosis and treatment of BCRL.
References
Ferlay J, Shin H, Bray F, Forma D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127:2893–2917
Office for National Statistics (2012) Cancer incidence and mortality in the United Kingdom, 2008–2010. Available at: http://www.ons.gov.uk/ons/dcp171778_289890.pdf [Accessed 17.01.2014]
McLaughlin SA, Van Zee KJ (2010) The prevalence of lymphoedema and changes in practice to reduce its occurrence in women with breast cancer. Eur J Clin Med Oncol 2:23–29
Miaskowski C, Dodd M, Paul SM, West C, Hamolsky D, Abrams G, Cooper BA, Elboim C, Neuhaus J, Schmidt BL, Smoot B, Aouizerat BE (2013) Lymphatic and angiogenic candidate genes predict the development of secondary lymphoedema following breast cancer surgery. PLoS One 8:e60164. doi:10.1371/journal.pone.0060164
Ahmed RL, Prizment A, Lazovich D, Schmitz KH, Folsom AR (2008) Lymphoedema and quality of life in breast cancer survivors: the Iowa Women’s health study. J Clin Oncol 26:5689–5696
Paskett ED, Dean JA, Oliveri JM, Harrop JP (2012) Cancer-related lymphoedema risk factors, diagnosis, treatment and impact. J Clin Oncol 30:3726–3733
Clark B, Sitzia J, Harlow W (2005) Incidence and risk of arm oedema following treatment for breast cancer: a three-year follow-up study. QJM 98:343–348
Hayes SC, Janda M, Cornish B, Battistutta D, Newman B (2008) Lymphoedema following breast cancer: incidence, risk factors and effect on upper body function. J Clin Oncol 26:3536–3542
Penha TRL, Slangen JJG, Heuts EM, Voogd AC, Von Meyenfeldt MF (2011) Prevalence of lymphoedema more than five years after breast cancer treatment. Eur J Surg Oncol 37:1059–1063
DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14:500–515
National Lymphedema Network (2013) Position paper: screening and measurement for early detection of breast cancer related lymphedema. Available at: http://www.lymphnet.org/resources/position-paper-screening-and-measurement-for-early-detection-of-breast-cancer-related
Stout NL, Pfalzer LA, Springer B, Levy E, McGarvey CL, Danoff JV, Gerber LH, Soballe PW (2012) Breast cancer-related lymphedema: comparing direct costs of a prospective surveillance model and a traditional model of care. Phy Ther 92:152–163
Ancukiewicz M, Miller CL, Skolny MN, O’Toole J, Warren LE, Jammallo LS, Specht MC, Taghian (2012) Comparison of relative versus absolute arm size changes as criteria for quantifying breast cancer-related lymphoedema. Breast Cancer Res Treat 135:145–152
Taylor R, Jayasinghe UW, Koelmeyer L, Ung O, Boyages (2006) Reliability and validity of arm volume measurements for assessment of lymphoedema. Phy Ther 86:205–214
Ridner SH, Dietrich MS, Deng J, Bonner CM, Kidd N (2009) Bioelectrical Impedance for detecting upper limb lymphoedema in non-laboratory settings. Lymphat Res Biol. doi:10.1089/lrb.2008.1003
Lucci A, Mackie McCall L, Beitsch PD, Whitworth PW, Reintgen DS, Blumencranz PW, Leitch AM, Saha S, Hunt KK, Giuliano AE (2007) Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection (ALND) compared with SLND alone in the American college of surgeons oncology group trial Z0011. J Clin Oncol 25:3657–3663
Schrenk P, Rieger R, Shamiyeh A, Wayand W (2000) Morbidity following sentinel node biopsy versus axillary lymph node dissection for patients with breast carcinoma. Cancer 88:608–614
Langer I, Guller U, Berclaz G, Koechli OR, Schaer G, Fehr MK, Hess T, Oertli D, Bronz L, Schnarwyler B, Wight E, Uehlinger U, Infanger E, Burger D, Zuber M (2007) Morbidity of sentinel lymph node biopsy (SLN) alone versus SLN and completion axillary lymph node dissection after breast cancer surgery: a prospective Swiss multicenter study on 659 patients. Ann Surg 245:452–461
McLaughlin SA, Wright MJ, Morris KT, Giron GL, Sampson MR, Brockway JP, Hurley KE, Riedel ER, Van Zee KJ (2008) Prevalence of lymphoedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. J Clin Oncol 26:5213–5219
Mansel RE, Fallowfield L, Kissin M, Goyal A, Newcombe RG, Dixon JM, Yiangou C, Horgan K, Bundred N, Moneypenny I, England D, Sibbering M, Abdullah TI, Barr L, Chetty U, Sinnett DH, Fleissig A, Clarke D, Ell PJ (2006) Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC Trial. J Natl Cancer Inst 98:599–609
Cornish B (2006) Bioimpedance analysis: scientific background. Lymphat Res Biol 4:47–50
Moseley A, Piller N (2008) Reliability of bioimpedance spectroscopy and tonometry after breast conserving treatment. Lymphat Res Biol 6:85–87
Czerniec SA, Ward LC, Refshauge KM, Beith J, Lee MJ, York S, Kilbreath SL (2010) Assessment of breast cancer-related arm lymphoedema-comparison of physical measurement methods and self-report. Cancer Invest 28:54–62
Cornish BH, Chapman M, Hirst C, Mirolo B, Bunce IH, Ward LC, Thomas BJ (2001) Early diagnosis of lymphedema using multiple frequency bioimpedance. Lymphology 34:2–11
Ward LC (2006) Bioelectrical impedance analysis: proven utility in lymphoedema risk assessment and therapeutic monitoring. Lymph Res Biol 4:51–56
Box RC, Reul-Hirche HM, Bullock-Saxton JE, Furnival CM (2002) Physiotherapy after breast cancer surgery: results of a randomised controlled study to minimise lymphoedema. Breast Cancer Res Treat 75:51–64
Specht MC, Miller CL, Russell TA, Horick N, Skolny MN, O’Toole JA, Jammallo LS, Niemierko A, Sadek BT, Shenouda MN, Finkelstein DM, Smith BL, Taghian AG (2013) Defining a threshold for intervention in breast cancer-related lymphedema: what level of arm volume increase predicts progression? Breast Cancer Res Treat 140:485–494
Stout NL, Pfalzer LA, McGarvey C, Springer B, Gerber LH, Soballe P (2008) Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer 112:2809–2819
National Lymphedema Network (2011) Position Statement of the National Lymphedema Network. Screening and measurement for early detection of breast cancer-related lymphedema. Availabel at: http://www.massgeneral.org/cancer/assets/pdfs/ScreeningandMeasurement%20.pdf
Australasian Lymphology Association (2012) Monitoring for the early detection of breast cancer related lymphoedema. Available at: http://www.lymphoedema.org.au/ALA/Lymphoedema/Position_Statements/ALA/Lymphodema/Position_Statements.aspx?hkey=c2afe208-5f01-49c0-8fc9-21f7fff87d5b
Stout NL, Binkley JM, Schmitz KH, Andrews K, Hayes SC, Campbell KL, McNeely ML, Soballe PW, Berger AM, Cheville AL, Fabian C, Gerber LH, Harris SR, Johansson K, Pusic AL, Prosnitz RG, Cancer SRA (2012) A prospective surveillance model for rehabilitation for women with breast cancer. Cancer 118:2191–2200
Kilbreath SL, Refshauge KM, Ward LC, Kastanias K, Yee J, Koelmeyer LA, Beith JM, French JR, Ung OA, Black D (2013) Factors affecting the preoperative and postoperative extracellular fluid in the arm on the side of breast cancer: a cohort study. Lymph Res Biol 11:66–71
Smoot B, Paul SM, Aouizerat BE, Elboim C, Levine JD, Abrams G, Hamolsky D, Neuhaus J, Schmidt B, West C, Topp K, Miaskowski C (2014) Side of cancer does not influence limb volumes in women prior to breast cancer surgery. Lymph Res Biol 12:189–193
Francis WP, Abghari P, Du W, Rymal C, Suna M, Kosir MA (2006) Improving surgical outcomes: standardising the reporting of incidence and severity of acute lymphoedema after sentinel lymph node biopsy and axillary lymph node dissection. Am J Surg 192:636–639
Stout NL, Pfalzer LA, Levy E, McGarvey C, Springer B, Gerber LH, Soballe P (2011) Segmental limb volume change as a predictor of the onset of lymphedema in women with early breast cancer. PM&R 3:1098–1105
Stanton AW, Modi S, Mellor RH, Levick JR, Mortimer PS (2009) Recent advances in breast cancer-related lymphedema of the arm: lymphatic pump failure and predisposing factors. Lymph Res Biol 7:29–45
Hayes S, Cornish B, Newman B (2005) Comparison of methods to diagnose lymphoedema among breast cancer survivors: 6 month follow-up. Breast Cancer Res Treat 89:221–226
Fu MR, Cleland CM, Guth AA, Kayal M, Haber J, Cartwright F, Kleinman R, Kang Y, Scagliola J, Axelrod D (2013) L-Dex ratio in detecting breast cancer-related lymphedema: reliability, sensitivity, and specificity. Lymphology 46:85–96
Wu Z, Zhao J (2013) The problem with peripherally inserted catheters in China. Pak J Med Sci 29:896
Tsai RJ, Dennis LK, Lynch CF, Snetselaar LG, Zambe GKD, Scott-Conner C (2009) The risk of developing arm lymphoedema among breast cancer survivors: a meta-analysis of treatment factors. Ann Surg Oncol 16:1959–1972
Kwan ML, Darbinian J, Schmitz KH, Citron R, Partee P, Kutner SE, Kushi LH (2010) Risk factors for lymphedema in a prospective breast cancer survivorship study: the Pathways Study. Arch Surg 145:1055–1063
Ugur S, Arici C, Yaprak M, Mesci A, Arici GA, Dolay K, Ozmen V (2013) Risk factors of breast cancer-related lymphedema. Lymphat Res Biol 11:72–75
Morcos B, Ahmad FA, Anabtawi I, Sba’ AM, Shabani H, Yaseen R (2014) Development of breast cancer-related lymphedema: is it dependent on the patient, the tumor or the treating physicians? Surg Today 44:100–106
Norman SA, Localio AR, Potashnik SL, Simoes Torpey HA, Kallan MJ, Weber AL, Miller LT, Demichele A, Solin LJ (2009) Lymphedema in breast cancer survivors: incidence, degree, time course, treatment, and symptoms. J Clin Oncol 27:390–397
Fu MR, Ridner SH, Hu SH, Stewart BR, Cormier JN, Armer JM (2013) Psychosocial impact of lymphedema: a systematic review of literature from 2004 to 2011. Psychooncology 22:1466–1484
Acknowledgments
This work was funded by Friends of the Cancer Centre, Northern Ireland Cancer Centre, Belfast City Hospital, Belfast.
Conflict of interest
The authors declare that they have no conflict of interest and confirm that they have control of all primary data and agree to allow the journal to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Blaney, J.M., McCollum, G., Lorimer, J. et al. Prospective surveillance of breast cancer-related lymphoedema in the first-year post-surgery: feasibility and comparison of screening measures. Support Care Cancer 23, 1549–1559 (2015). https://doi.org/10.1007/s00520-014-2504-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2504-9