Abstract
The purpose of this study is to evaluate arm volume measurements and clinico-pathologic characteristics of breast cancer patients to define a threshold for intervention in breast cancer-related lymphedema. We prospectively performed arm volume measurements on breast cancer patients using a Perometer. Arm measurements were performed pre- and post-operatively, and change in arm volume was quantified using a relative volume change (RVC) equation. Patient and treatment risk factors were evaluated. Cox proportional hazards models with time-dependent covariates for RVC were used to evaluate whether RVC elevations of ≥3 to <5 % or ≥5 to <10 % occurring ≤3 months or >3 months after surgery were associated with progression to ≥10 % RVC. 1,173 patients met eligibility criteria with a median of 27 months post-operative follow-up. The cumulative incidence of ≥10 % RVC at 24 months was 5.26 % (95 % CI 4.01–6.88 %). By multivariable analysis, a measurement of ≥5 to <10 % RVC occurring >3 months after surgery was significantly associated with an increased risk of progression to ≥10 % RVC (HR 2.97, p < 0.0001), but a measurement of ≥3 to <5 % RVC during the same time period was not statistically significantly associated (HR 1.55, p = 0.10). Other significant risk factors included a measurement ≤3 months after surgery with RVC of ≥3 to <5 % (p = 0.007), ≥5 to <10 % (p < 0.0001), or ≥10 % (p = 0.023), axillary lymph node dissection (ALND) (p < 0.0001), and higher BMI at diagnosis (p = 0.0028). Type of breast surgery, age, number of positive or number of lymph nodes removed, nodal radiation, chemotherapy, and hormonal therapy were not significant (p > 0.05). Breast cancer patients who experience a relative arm volume increase of ≥3 to <5 % occurring >3 months after surgery do not have a statistically significant increase in risk of progression to ≥10 %, a common lymphedema criterion. Our data support utilization of a ≥5 to <10 % threshold for close monitoring or intervention, warranting further assessment. Additional risk factors for progression to ≥10 % include ALND, higher BMI, and post-operative arm volume elevation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Survival rates after treatment for breast cancer are high, making attention to quality of life and long-term effects of treatment increasingly important [1–3]. Lymphedema is a chronic condition characterized by swelling of the arm, hand, breast, or trunk, which may develop as a result of breast cancer treatment from an accumulation of lymphatic fluid in the interstitial tissues. It is known to have detrimental effects on quality of life due to body image changes, alterations in arm function, and increased complications such as infection and cellulitis [2, 4–6].
Although reported incidence rates vary, a recent meta-analysis indicated that more than one in five breast cancer patients will develop lymphedema [7]. The most commonly cited risk factors for breast cancer-related lymphedema include axillary lymph node dissection (ALND) [7–16], and high body mass index (BMI) or obesity [7, 10, 13, 15–25]. A number of other risk factors have been suggested, including mastectomy [5, 7, 13, 14, 21], extent of axillary surgery [7, 15, 22, 23, 26–28], number of pathologically involved lymph nodes [14, 15, 21, 24, 29], chemotherapy [8, 10, 15, 22, 29], nodal radiation [13, 14, 22, 24, 25, 28, 30–34], age [5, 12, 17, 27, 31, 33], and physical activity levels [5, 7, 13].
In an effort to decrease the physical and psychosocial complications of lymphedema, it is increasingly recommended that patients should be screened for low-level arm volume changes to enable early intervention [4, 35–37]. The National Lymphedema Network recommends preoperative assessment and ongoing surveillance for lymphedema as “imperative” and “best practice” [38]. However, the appropriate threshold for intervention when volume changes occur has not been adequately defined.
Varying definitions and methods of measurement for lymphedema have been utilized [37, 39, 40]. An absolute difference between arms or increase from pre-operative baseline in the at-risk arm of >2 cm circumference by tape measurement or >200 ml volume by water displacement or perometry is often considered indicative of lymphedema [7, 14, 41]. In addition, a relative volume difference between arms or increase in at-risk arm volume from pre-operative baseline of 5–10 % by perometry, water displacement, or circumferential tape measurement may be used to define lymphedema [7, 14, 39, 41, 42]. Bioimpedance spectroscopy (BIS) is a technique which measures extracellular fluid of the upper extremity, with a corresponding lymphedema criterion based on the impedance ratio between arms or change from a pre-operative baseline outside of a normal range [43].
The quantification of lymphedema by the Perometer has been rigorously validated, demonstrating high accuracy and overall reliability across repeated measurements [44, 45]. We previously reported that accurate evaluation for breast cancer-related lymphedema must include a pre-operative measurement and account for changes in the at-risk and contralateral arm, and developed the relative volume change (RVC) equation [46]. Although prior studies have defined lymphedema as a volume increase of >3–15 % [7, 14], the majority have utilized >10 % as a lymphedema criterion [21, 33, 41, 47–55]. In addition, a 2009 study by Cormier et al. [42] found that >10 % volume change was an independent risk factor for decreased quality of life. Therefore in the clinical setting at our institution and for the purpose of this study, we chose to utilize ≥10 % RVC as an endpoint for progression.
In a 2008 report, Stout-Gergich et al. [36] proposed four stages for evaluating early lymphedema based on volume change measured via perometry: 0–3 %—at risk for lymphedema, 3–5 %—pre-clinical lymphedema, 5–8 %—mild lymphedema, and >8 %—moderate–severe lymphedema. Based on their findings, the authors advocated that an arm volume increase of >3 % is an appropriate threshold for intervention with compression therapy.
We sought to determine whether utilization of ≥3 to <5 % or ≥5 to <10 % RVC thresholds prognosticate progression to ≥10 % RVC by analyzing arm volume measurements from patients prospectively screened for lymphedema at our institution. Arm volume measurements, patient demographics, and treatment characteristics were analyzed to identify risk factors for progression to ≥10 % RVC.
Materials and methods
Beginning in 2005, with Institutional Review Board approval, we prospectively obtained bilateral arm volume measurements on women diagnosed with breast cancer using a Perometer. Measurements were obtained pre- and post-operatively, during treatment for breast cancer, and at follow-up oncology visits after completion of breast cancer treatment. The protocol for lymphedema screening and the equation for RVC have previously been published [46]. Briefly, RVC = [(A 2 U 1)/(U 2 A 1)] − 1 where A 1, A 2 are arm volumes on the side treated for breast cancer at pre-operative baseline and a post-operative follow-up; and U 1, U 2 are arm volumes on the contralateral side at the corresponding time points. The RVC equation accounts for pre-operative asymmetry between arms, and incorporates contralateral arm volume to account for changes in arm size caused by factors unrelated to lymphedema, such as weight gain. Any measurements obtained after a patient was diagnosed with distant metastasis or recurrence were excluded to avoid potential confounding. Patients who underwent bilateral breast or axillary surgery were excluded entirely from the analysis, since the RVC formula cannot be used for patients at risk for bilateral lymphedema.
For this analysis, patients underwent a pre-operative measurement between 08/2005 and 08/2012, and received surgery and follow-up care at our institution for primary breast cancer. All patients had a pre-operative measurement and at least one follow-up measurement occurring >3 months after surgery. A measurement with ≥10 % RVC occurring >3 months after surgery was utilized as the endpoint for analysis of arm volume progression. Once a patient underwent a measurement with ≥10 % RVC (occurring at an assessment >3 months post-operative), all further measurements for that patient were excluded from the analysis.
To determine whether low-level RVC elevation is associated with progression to ≥10 % RVC, patients were categorized according to whether they had an RVC in the ≥3 to <5 % and/or ≥5 to <10 % range at a measurement >3 months after surgery. Measurements occurring ≤3 months post-operative were categorized similarly (with an additional category of ≥10 % RVC) and considered as independent risk factors in the analysis. Any measurements occurring after a patient initiated lymphedema treatment with compression therapy were excluded from analysis in order to analyze the natural history of arm volume progression without the influence of treatment intervention. Medical record review was used to determine which patients received treatment and defined by prescription for a compression sleeve.
Patient demographics, surgical, radiation, and medical oncology treatments were collected via medical record review to analyze as risk factors. Nodal radiation was defined as radiation to the breast/chest wall with supraclavicular and/or axillary radiation.
We used Cox proportional hazards regression to evaluate whether an RVC of ≥3 to <5 % and/or ≥5 to <10 % occurring >3 months after surgery was associated with progression to ≥10 % RVC. The time from surgery to ≥10 % RVC (“event”) or most recent follow-up RVC measurement (“censored”) was used as the time-to-event variable in the Cox models. Thus, estimates are adjusted for the amount of follow-up time, as only patients with comparable follow-up are included in each risk set. Separate time-dependent covariates for RVC measurements in the range of ≥3 to <5 % and ≥5 to <10 % were used such that patients were included in the non-elevated category until their first RVC in the ≥3 to <5 % or ≥5 to <10 % category occurred. Therefore a patient categorized in the ≥3 to <5 % RVC group, who progressed to ≥5 to <10 % RVC before crossing RVC ≥10 %, was considered in both groups when analyzing for progression.
Separate covariates were included for RVC categories of ≥3 to <5 %, ≥5 to <10 %, and ≥10 % occurring ≤3 months after surgery. A small fraction of patients did not have a measurement within 3 months of surgery, and were included in the <3 % reference category. Models were also run with these patients excluded to assess the impact on results. Patient and treatment risk factors were evaluated, and the number of measurements per year was included in the multivariable regression to account for variation in the frequency of measurements among patients. The Kaplan–Meier method was used to obtain estimates of cumulative incidence of ≥10 % RVC occurring >3 months after surgery [56]. The cumulative incidence of progression to ≥10 % RVC was calculated among patients who had a measurement in the ≥3 to <5 % RVC category, where the starting point for assessment of progression was the patient’s initial measurement in the ≥3 to <5 % category after 3 months post-operative. Similarly, the cumulative incidence of progression to ≥10 % RVC was calculated among those with a measurement in the ≥5 to <10 % RVC category occurring >3 months after surgery.
Results
Patient population
1,173 patients met eligibility. The median post-operative follow-up was 26.9 months (range 3.3–82.6, 25th percentile 15.2, 75th percentile 43.9). Median number of measurements per patient was 6 (range 2–21, 25th percentile 4, 75th percentile 8). Clinical and pathologic characteristics of the study population are presented in Table 1. The cumulative incidence of ≥10 % RVC occurring >3 months after surgery was 5.26 % (95 % CI 4.01–6.88 %) at 24 months and 9.75 % (95 % CI 7.62–12.4 %) at 48 months post-operative (Fig. 1). The median time to crossing ≥10 % RVC (at an assessment >3 months post-operative) was 14.4 months (range 3.5–57.1). 5 % (57/1,173) of patients received treatment for lymphedema with compression therapy. Of these patients, five had a maximum RVC of <5 %, 25 had a maximum RVC of ≥5 to <10 %, and 27 patients had a maximum RVC of ≥10 % prior to treatment initiation.
Risk of progression to ≥10 % RVC by patient/treatment factors
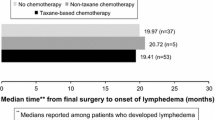
Patients who underwent ALND with nodal radiation had the highest 2-year cumulative incidence at 18.1 %, compared to 6.1 % for sentinel lymph node biopsy (SLNB) with nodal radiation. The cumulative incidence of ≥10 % RVC was 2.0 % for patients who underwent SLNB without nodal radiation, and 2.4 % for no axillary surgery (Table 2). Factors significant for increased risk of progression to ≥10 % RVC at >3 months after surgery by univariate analysis are included in Table 3. By multivariable analysis, ALND (p < 0.0001) and higher BMI at diagnosis (p = 0.0028) were the only patient/treatment factors significantly associated with an increased risk of progression to ≥10 % RVC at >3 months after surgery (Table 4).
Risk of progression to ≥10 % RVC by levels of arm volume increase occurring >3 months post-operative
Among patients who had an RVC measurement in the ≥3 to <5 % category occurring >3 months after surgery, the cumulative incidence of progression to ≥10 % RVC was 10.8 % (95 % CI 7.1–16.1 %) at 24 months after the first measurement in the ≥3 to <5 % range. Among those who had an RVC of ≥5 to <10 %, the comparable estimate of cumulative incidence of progression was 18.7 % (95 % CI 12.6–27.4 %) (Fig. 2). By multivariable analysis, a measurement of ≥5 to <10 % RVC occurring >3 months after surgery was statistically significantly associated with an increased risk of progression to ≥10 % RVC (p = <0.0001), but a measurement of ≥3 to <5 % RVC during this time period was not statistically significant (p = 0.10) (Table 4). The number of measurements per year was also significantly associated with increased risk of progression to ≥10 % RVC by multivariable analysis (p < 0.0001).
Risk of progression to ≥10 % RVC by levels of arm volume increase occurring ≤3 months post-operative
95 % (1,120/1,173) of patients had a measurement ≤3 months after surgery. Of these patients, 8.4 % (94/1,120) had an RVC of ≥3 to <5 %, 7.1 % (79/1,120) had an RVC of ≥5 to <10 % and 1.3 % (14/1,120) had an RVC of ≥10 % within 3 months of surgery. The remaining 933 patients (83.3 %) had an RVC of <3 % during this time period. By multivariable analysis, all three categories of RVC elevation occurring ≤3 months after surgery were significantly associated with an increased risk of progression to ≥10 % RVC (Table 4). A multivariable model excluding the 53 patients without a measurement within 3 months of surgery demonstrated similar results (data not shown).
Discussion
To our knowledge, the current study represents the largest cohort of breast cancer patients prospectively screened for lymphedema using the Perometer, a tool with demonstrated validity in quantifying arm volume. In our analysis of 1,173 patients, a measurement of ≥5 to <10 % RVC, higher BMI at diagnosis, and ALND were associated with a statistically significant increase in risk of progression to ≥10 % RVC by multivariable analysis. A measurement of ≥3 to <5 % RVC was significant for progression to ≥10 % RVC when it occurred within 3 months of surgery, but did not reach statistical significance at a time >3 months post-operative. Interestingly, any range of RVC elevation occurring ≤3 months after surgery was significantly associated with increased risk of progression to ≥10 % RVC. Our findings support utilization of a ≥5 to <10 % threshold for close monitoring or intervention. Further assessment of this strategy is warranted.
Screening programs for early detection and intervention in breast cancer-related lymphedema have been recommended [35, 36, 38], but an appropriate threshold for intervention has not yet been determined. The emotional and financial burden of lymphedema treatment is well-documented [8, 57], as is the importance of early intervention aimed at preventing progression of this condition [40, 58, 59]. It is therefore critical that an effective threshold for intervention be established.
A prior study by Stout-Gergich et al. [36] utilized compression therapy at >3 % increase in arm volume to assess the effectiveness of early intervention. In this single arm, Phase II study, 43 breast cancer patients who developed an arm volume increase of >3 % received intervention with compression therapy. In the follow-up period after intervention (mean 4.8 months), a greater decrease in absolute arm volume was reported in patients who received intervention compared to an age-matched control group. The study did not have a randomized-controlled design. Based on their results, the authors proposed that >3 % arm volume increase is a diagnostic criterion for subclinical lymphedema and recommended intervention at that threshold.
Our data suggest that a measurement of ≥3 to <5 % RVC is statistically significant for progression to ≥10 % RVC only when it occurs within 3 months of surgery, and not at later time points. While Stout-Gergich et al. [36] reported reduced arm volume in patients who initiated compression therapy after reaching >3 %, it is unclear that such intervention was warranted. The median time to development of >3 % in their trial was 6.9 months post-operative, and based on our data it is likely that some patients would not otherwise have progressed to ≥10 %, a common lymphedema criterion, had they not received intervention.
In contrast, our data suggest that a ≥5 to <10 % RVC criterion may be a better threshold for early intervention, as crossing this threshold at any time following surgery was a significant predictor of progression to ≥10 % RVC. The cumulative incidence of progression to ≥10 % for patients with an RVC of ≥5 to <10 % occurring >3 months after surgery was 18.7 %, compared with 10.8 % for ≥3 to <5 % during this period. Furthermore, recent reports have suggested that arm volume increases in the range of 5–10 % may represent low-level edema based on lymphedema symptoms reported by patients with volume changes in this range [42, 60]. It should be noted that the confidence intervals for cumulative incidence of progression for patients with a measurement of ≥3 to <5 % and ≥5 to <10 % in our series overlap, warranting further investigation. We are currently conducting a prospective, randomized-controlled trial of compression therapy versus observation in patients with a measurement of ≥5 to <10 % RVC to evaluate the efficacy of intervention at this threshold (Clinical Trials.gov Identification number NCT00959985) [61].
In our series, a measurement of ≥3 to <5 % RVC occurring within 3 months of surgery was significant for increased risk of progression to ≥10 % RVC, but was not statistically significant when it occurred later in follow-up (>3 months post-operative). We did find that patients with a measurement of ≥3 to <5 % occurring >3 months after surgery had a 10.8 % risk of progression to ≥10 % RVC. Given these findings, we suggest that patients with a measurement of ≥3 to <5 % RVC any time after surgery undergo close monitoring with a re-measurement at 1–2 months to assess for progression.
Consistent with prior reports, independent clinico-pathologic risk factors for progression to ≥10 % RVC in our series included ALND and higher BMI at diagnosis [7–16]. We did not find type of breast surgery, extent of axillary surgery, number of pathologically involved lymph nodes, chemotherapy, or nodal radiation to be significant for progression to ≥10 % RVC by multivariable analysis. These have less commonly been cited as risk factors for lymphedema, with the majority lacking strong evidence from prospective studies utilizing accurate measurement techniques. Interestingly, we found that the rate of ≥10 % RVC in patients with no axillary surgery was 2.4 %, which was similar to the 2.0 % incidence for SLNB without nodal radiation. These findings suggest that while patients who undergo SLNB are at risk for developing lymphedema (albeit low), this risk may not be significantly greater than for patients without axillary surgery.
We also found that a measurement of ≥3 to <5 %, ≥5 to <10 %, or ≥10 % RVC within 3 months of surgery was significantly associated with an increased risk of progression to ≥10 % RVC. Furthermore, increasingly higher categories of RVC elevation during this period represented a more significant risk of progression. Mahamaneerat et al. [62] also demonstrated the importance of post-operative arm volume elevation as a risk factor for lymphedema, reporting that a ≥5 % increase in arm volume ≤1 month after surgery was associated with a 1.4-fold increased risk of lymphedema. These findings demonstrate the importance of screening within 3 months of surgery, such that patients with elevated arm volume during this period can be closely monitored for future progression.
The 2-year cumulative incidence of ≥10 % RVC in our series was 6.1 % for patients who underwent SLNB with nodal radiation and 2.0 % for SLNB without, compared to 18.1 % for ALND with and 10.2 % for ALND without nodal radiation. McLaughlin et al. [16] similarly reported a 5 % incidence for patients with SLNB and 16 % for those with ALND. Other studies have reported significantly higher rates of lymphedema compared to our series, ranging as high as 30–80 % [5, 63–66]. The incidence of ≥10 % RVC in our cohort may be lower than lymphedema rates reported in previous studies due to differences in length of follow-up, method of measurement and definition of lymphedema. We chose to report cumulative incidence at 2 years (rather than 4 or 5 years) based on our median follow-up of 26.9 months. In addition, we excluded measurements occurring after initiation of compression therapy, which may underestimate the incidence of ≥10 % RVC in our cohort. However, the exclusion of measurements obtained after initiation of compression therapy uniquely enabled us to analyze the natural history of arm volume progression as it occurs without the influence of treatment intervention.
New cases of lymphedema continued to appear up to 4 years after surgery in our series, with cumulative incidence increasing from 5.3 to 9.8 % at 2–4 years. Although some have reported that lymphedema most commonly occurs within 2 years of diagnosis [7], others have shown that incidence continues to increase throughout follow-up [63, 67]. Petrek et al. [67] demonstrated that lymphedema developed at >3 years in 25 % of patients, with an ongoing risk of approximately 1 % per year for at least 20 years. In another study, Norman et al. [63] reported that 20 % of lymphedema cases occurred between 2 and 5 years. These findings support screening for lymphedema both during and after completion of breast cancer treatment.
Our study is limited by the variable time intervals at which patients underwent arm volume measurements. Patients were measured at their routine oncology follow-up visits, raising the possibility that transient episodes of arm volume elevation may have been missed between measurements. This may underestimate the number of patients who developed ≥10 % RVC, and the number who met an RVC threshold and subsequently underwent regression of arm volume. There may also have been a bias of greater frequency of screening for patients with lymphedema symptoms or those perceived to be at high risk for lymphedema, as reflected by the association of number of measurements per year with progression to ≥10 % RVC in the multivariable model. A prospective study with pre-specified time intervals for follow-up measurements is underway to address this issue (Clinical Trials.gov Identification number NCT00959985) [61]. Finally, our study is limited by variable use of lymphedema treatments, as the decision to treat using compression therapy was left to the patient and clinician. As a result, we may be under- or over-estimating the risk of arm volume progression since measurements occurring after initiation of compression therapy were excluded from analysis.
Lymphedema continues to be one of the most-feared complications of breast cancer treatment. Our study provides new insights into the natural history of arm volume progression in breast cancer patients, and suggests use of specific thresholds for intervention. In addition, we identify independent risk factors for arm volume progression which can be utilized to target high-risk patients for close monitoring. Based on our results, we propose a revised approach for classification of, and intervention for, arm volume elevation which may occur in breast cancer patients.
-
≥3 to <5 % RVC—close monitoring with repeat arm volume measurement within 1–2 months.
-
≥5 to <10 % RVC—randomization into a prospective trial of observation versus treatment with compression therapy. For patients not participating in a clinical trial, close monitoring with a repeated arm volume measurement within 1–2 months.
-
≥10 % RVC—treatment with compression therapy or other methods at the discretion of the healthcare provider.
In conclusion, our data suggest that an increase in arm volume of ≥5 to <10 % may represent an appropriate threshold for intervention to prevent progression to ≥10 %, a common criterion for lymphedema. An arm volume increase of ≥3 to <5 % occurring >3 months after surgery is not statistically significant for increased risk of progression to ≥10 %, and therefore may be insufficient to warrant intervention. We found that patients who undergo ALND, have a high BMI at diagnosis, or experience elevated arm volume within 3 months of surgery had an increased risk of progression to ≥10 %, suggesting the importance of close monitoring for these patients. Further research is warranted to determine the efficacy of early intervention with compression therapy for patients with an arm volume increase of ≥5 to <10 %. In addition, future studies should address the impact of such interventions on quality of life compared with the benefit of preventing lymphedema development.
References
Khan F, Amatya B, Pallant JF, Rajapaksa I (2012) Factors associated with long-term functional outcomes and psychological sequelae in women after breast cancer. Breast 3:314–320. doi:10.1016/j.breast.2012.01.013
Ahmed RL, Prizment A, Lazovich D, Schmitz KH, Folsom AR (2008) Lymphedema and quality of life in breast cancer survivors: the Iowa Women’s health study. J Clin Oncol 26(35):5689–5696. doi:10.1200/JCO.2008.16.4731
Rief W, Bardwell WA, Dimsdale JE, Natarajan L, Flatt SW, Pierce JP (2011) Long-term course of pain in breast cancer survivors: a 4-year longitudinal study. Breast Cancer Res Treat 130(2):579–586. doi:10.1007/s10549-011-1614-z
Sakorafas GH, Peros G, Cataliotti L, Vlastos G (2006) Lymphedema following axillary lymph node dissection for breast cancer. Surg Oncol 15(3):153–165. doi:10.1016/j.suronc.2006.11.003
Hayes SC, Janda M, Cornish B, Battistutta D, Newman B (2008) Lymphedema after breast cancer: incidence, risk factors, and effect on upper body function. J Clin Oncol 26(21):3536–3542. doi:10.1200/JCO.2007.14.4899
Jager G, Doller W, Roth R (2006) Quality-of-life and body image impairments in patients with lymphedema. Lymphology 39(4):193–200
Disipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14(6):500–515. doi:10.1016/S1470-2045(13)70076-7
Shih YC, Xu Y, Cormier JN, Giordano S, Ridner SH, Buchholz TA, Perkins GH, Elting LS (2009) Incidence, treatment costs, and complications of lymphedema after breast cancer among women of working age: a 2-year follow-up study. J Clin Oncol 27(12):2007–2014. doi:10.1200/JCO.2008.18.3517
Mansel RE, Fallowfield L, Kissin M, Goyal A, Newcombe RG, Dixon JM, Yiangou C, Horgan K, Bundred N, Monypenny I, England D, Sibbering M, Abdullah TI, Barr L, Chetty U, Sinnett DH, Fleissig A, Clarke D, Ell PJ (2006) Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC trial. J Natl Cancer Inst 98(9):599–609. doi:10.1093/jnci/djj158
Norman SA, Localio AR, Kallan MJ, Weber AL, Torpey HA, Potashnik SL, Miller LT, Fox KR, DeMichele A, Solin LJ (2010) Risk factors for lymphedema after breast cancer treatment. Cancer Epidemiol Biomarkers Prev 19(11):2734–2746. doi:10.1158/1055-9965.EPI-09-1245
Yang EJ, Park WB, Seo KS, Kim SW, Heo CY, Lim JY (2010) Longitudinal change of treatment-related upper limb dysfunction and its impact on late dysfunction in breast cancer survivors: a prospective cohort study. J Surg Oncol 101(1):84–91
Lucci A, McCall LM, Beitsch PD, Whitworth PW, Reintgen DS, Blumencranz PW, Leitch AM, Saha S, Hunt KK, Giuliano AE (2007) Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol 25(24):3657–3663. doi:10.1200/JCO.2006.07.4062
Park JH, Lee WH, Chung HS (2008) Incidence and risk factors of breast cancer lymphoedema. J Clin Nurs 17(11):1450–1459. doi:10.1111/j.1365-2702.2007.02187.x
Tsai RJ, Dennis LK, Lynch CF, Snetselaar LG, Zamba GK, Scott-Conner C (2009) The risk of developing arm lymphedema among breast cancer survivors: a meta-analysis of treatment factors. Ann Surg Oncol 16(7):1959–1972. doi:10.1245/s10434-009-0452-2
Ahmed RL, Schmitz KH, Prizment AE, Folsom AR (2011) Risk factors for lymphedema in breast cancer survivors, the Iowa women’s health study. Breast Cancer Res Treat 130(3):981–991. doi:10.1007/s10549-011-1667-z
McLaughlin SA, Wright MJ, Morris KT, Giron GL, Sampson MR, Brockway JP, Hurley KE, Riedel ER, Van Zee KJ (2008) Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. J Clin Oncol 26(32):5213–5219. doi:10.1200/JCO.2008.16.3725
Wilke LG, McCall LM, Posther KE, Whitworth PW, Reintgen DS, Leitch AM, Gabram SG, Lucci A, Cox CE, Hunt KK, Herndon JE 2nd, Giuliano AE (2006) Surgical complications associated with sentinel lymph node biopsy: results from a prospective international cooperative group trial. Ann Surg Oncol 13(4):491–500. doi:10.1245/ASO.2006.05.013
Soran A, Wu WC, Dirican A, Johnson R, Andacoglu O, Wilson J (2011) Estimating the probability of lymphedema after breast cancer surgery. Am J Clin Oncol 34(5):506–510. doi:10.1097/COC.0b013e3181f47955
Swenson KK, Nissen MJ, Leach JW, Post-White J (2009) Case-control study to evaluate predictors of lymphedema after breast cancer surgery. Oncol Nurs Forum 36(2):185–193. doi:10.1188/09.ONF.185-193
Box RC, Reul-Hirche HM, Bullock-Saxton JE, Furnival CM (2002) Physiotherapy after breast cancer surgery: results of a randomised controlled study to minimise lymphoedema. Breast Cancer Res Treat 75(1):51–64
Nesvold IL, Dahl AA, Lokkevik E, Marit Mengshoel A, Fossa SD (2008) Arm and shoulder morbidity in breast cancer patients after breast-conserving therapy versus mastectomy. Acta Oncol 47(5):835–842. doi:10.1080/02841860801961257
Hayes SB, Freedman GM, Li T, Anderson PR, Ross E (2008) Does axillary boost increase lymphedema compared with supraclavicular radiation alone after breast conservation? Int J Radiat Oncol Biol Phys 72(5):1449–1455. doi:10.1016/j.ijrobp.2008.02.080
Paskett ED, Naughton MJ, McCoy TP, Case LD, Abbott JM (2007) The epidemiology of arm and hand swelling in premenopausal breast cancer survivors. Cancer Epidemiol Biomarkers Prev 16(4):775–782. doi:10.1158/1055-9965.EPI-06-0168
Crosby MA, Card A, Liu J, Lindstrom WA, Chang DW (2012) Immediate breast reconstruction and lymphedema incidence. Plast Reconstr Surg 129(5):789e–795e. doi:10.1097/PRS.0b013e31824a2ab1
Ozaslan C, Kuru B (2004) Lymphedema after treatment of breast cancer. Am J Surg 187(1):69–72. doi:10.1200/JCO.2007.14.4899JCO
Goldberg JI, Wiechmann LI, Riedel ER, Morrow M, Van Zee KJ (2010) Morbidity of sentinel node biopsy in breast cancer: the relationship between the number of excised lymph nodes and lymphedema. Ann Surg Oncol 17(12):3278–3286. doi:10.1245/s10434-010-1155-4
Meeske KA, Sullivan-Halley J, Smith AW, McTiernan A, Baumgartner KB, Harlan LC, Bernstein L (2008) Risk factors for arm lymphedema following breast cancer diagnosis in Black women and White women. Breast Cancer Res Treat 113(2):383–391. doi:10.1007/s10549-008-9940-5
Herd-Smith A, Russo A, Muraca MG, Del Turco MR, Cardona G (2001) Prognostic factors for lymphedema after primary treatment of breast carcinoma. Cancer 92(7):1783–1787. doi:10.1002/1097-0142(20011001)92:7<1783
Querci della Rovere G, Ahmad I, Singh P, Ashley S, Daniels IR, Mortimer P (2003) An audit of the incidence of arm lymphoedema after prophylactic level I/II axillary dissection without division of the pectoralis minor muscle. Ann R Coll Surg Engl 85(3):158–161
Deo SV, Ray S, Rath GK, Shukla NK, Kar M, Asthana S, Raina V (2004) Prevalence and risk factors for development of lymphedema following breast cancer treatment. Indian J Cancer 41(1):8–12
Graham P, Jagavkar R, Browne L, Millar E (2006) Supraclavicular radiotherapy must be limited laterally by the coracoid to avoid significant adjuvant breast nodal radiotherapy lymphoedema risk. Australas Radiol 50(6):578–582. doi:10.1111/j.1440-1673.2006.01658.x
Hayes S, Janda M, Cornish B, Battistutta D, Newman B (2008) Lymphedema secondary to breast cancer: how choice of measure influences diagnosis, prevalence, and identifiable risk factors. Lymphology 41(1):18–28
Asim M, Cham A, Banerjee S, Nancekivell R, Dutu G, McBride C, Cavanagh S, Lawrenson R, Campbell I (2012) Difficulties with defining lymphoedema after axillary dissection for breast cancer. N Z Med J 125(1351):29–39
Coen JJ, Taghian AG, Kachnic LA, Assaad SI, Powell SN (2003) Risk of lymphedema after regional nodal irradiation with breast conservation therapy. Int J Radiat Oncol Biol Phys 55(5):1209–1215
Boccardo FM, Ansaldi F, Bellini C, Accogli S, Taddei G, Murdaca G, Campisi CC, Villa G, Icardi G, Durando P, Puppo F, Campisi C (2009) Prospective evaluation of a prevention protocol for lymphedema following surgery for breast cancer. Lymphology 42(1):1–9
Stout Gergich NL, Pfalzer LA, McGarvey C, Springer B, Gerber LH, Soballe P (2008) Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer 112(12):2809–2819. doi:10.1002/cncr.23494
Armer JM (2005) The problem of post-breast cancer lymphedema: impact and measurement issues. Cancer Invest 23(1):76–83
National Lymphedema Network Medical Advisory Committee (2012) Supplement to NLN position breast cancer screening: Screening and early detection of breast cancer-related lymphedema: The imperative. National Lymphedema Network
Cheville AL, McGarvey CL, Petrek JA, Russo SA, Thiadens SR, Taylor ME (2003) The grading of lymphedema in oncology clinical trials. Semin Radiat Oncol 13(3):214–225. doi:10.1016/S1053-4296(03)00038-9
Petrek JA, Pressman PI, Smith RA (2000) Lymphedema: current issues in research and management. CA Cancer J Clin 50(5):292–307
Armer JM, Stewart BR (2005) A comparison of four diagnostic criteria for lymphedema in a post-breast cancer population. Lymphat Res Biol 3(4):208–217. doi:10.1089/lrb.2005.3.208
Cormier JN, Xing Y, Zaniletti I, Askew RL, Stewart BR, Armer JM (2009) Minimal limb volume change has a significant impact on breast cancer survivors. Lymphology 42(4):161–175
Cornish BH, Chapman M, Hirst C, Mirolo B, Bunce IH, Ward LC, Thomas BJ (2001) Early diagnosis of lymphedema using multiple frequency bioimpedance. Lymphology 34(1):2–11
Stanton AW, Northfield JW, Holroyd B, Mortimer PS, Levick JR (1997) Validation of an optoelectronic limb volumeter (Perometer). Lymphology 30(2):77–97
Tierney S, Aslam M, Rennie K, Grace P (1996) Infrared optoelectronic volumetry, the ideal way to measure limb volume. Eur J Vasc Endovasc Surg 12(4):412–417
Ancukiewicz M, Russell TA, Otoole J, Specht M, Singer M, Kelada A, Murphy CD, Pogachar J, Gioioso V, Patel M, Skolny M, Smith BL, Taghian AG (2011) Standardized method for quantification of developing lymphedema in patients treated for breast cancer. Int J Radiat Oncol Biol Phys 79(5):1436–1443. doi:10.1016/j.ijrobp.2010.01.001
Celebioglu F, Perbeck L, Frisell J, Grondal E, Svensson L, Danielsson R (2007) Lymph drainage studied by lymphoscintigraphy in the arms after sentinel node biopsy compared with axillary lymph node dissection following conservative breast cancer surgery. Acta Radiol 48(5):488–495. doi:10.1080/02841850701305440
Johansson K, Ingvar C, Albertsson M, Ekdahl C (2001) Arm lymphoedema, shoulder mobility and muscle strength after breast cancer treatment—a prospective 2-year study. Adv Physiother 3:55–66
Bennett Britton TM, Buczacki SJ, Turner CL, Vowler SL, Pain SJ, Purushotham AD (2007) Venous changes and lymphoedema 4 years after axillary surgery for breast cancer. Br J Surg 94(7):833–834. doi:10.1002/bjs.5711
Kosir MA, Rymal C, Koppolu P, Hryniuk L, Darga L, Du W, Rice V, Mood D, Shakoor S, Wang W, Bedoyan J, Aref A, Biernat L, Northouse L (2001) Surgical outcomes after breast cancer surgery: measuring acute lymphedema. J Surg Res 95(2):147–151. doi:10.1006/jsre.2000.6021
Pain SJ, Vowler S, Purushotham AD (2005) Axillary vein abnormalities contribute to development of lymphoedema after surgery for breast cancer. Br J Surg 92(3):311–315. doi:10.1002/bjs.4835
Quinlan E, Thomas-MacLean R, Hack T, Kwan W, Miedema B, Tatemichi S, Towers A, Tilley A (2009) The impact of breast cancer among Canadian women: disability and productivity. Work 34(3):285–296. doi:10.3233/WOR-2009-0926
Edwards TL (2000) Prevalence and aetiology of lymphoedema after breast cancer treatment in southern Tasmania. Aust N Z J Surg 70(6):412–418
Tengrup I, Tennvall-Nittby L, Christiansson I, Laurin M (2000) Arm morbidity after breast-conserving therapy for breast cancer. Acta Oncol 39(3):393–397
Armer JM, Stewart BR (2010) Post-breast cancer lymphedema: incidence increases from 12 to 30 to 60 months. Lymphology 43(3):118–127
Satagopan JM, Ben-Porat L, Berwick M, Robson M, Kutler D, Auerbach AD (2004) A note on competing risks in survival data analysis. Br J Cancer 91(7):1229–1235. doi:10.1038/sj.bjc.6602102
Stout NL, Pfalzer LA, Springer B, Levy E, McGarvey CL, Danoff JV, Gerber LH, Soballe PW (2011) Breast cancer-related lymphedema: comparing direct costs of a prospective surveillance model and a traditional model of care. Phys Ther 92(1):152–163. doi:10.2522/ptj.20100167
Torres Lacomba M, Yuste Sanchez MJ, Zapico Goni A, Prieto Merino D, Mayoral del Moral O, Cerezo Téllez E, Minayo Mogollón E (2010) Effectiveness of early physiotherapy to prevent lymphoedema after surgery for breast cancer: randomised, single blinded, clinical trial. BMJ 340:b5396. doi:10.1136/bmj.b5396
Rockson SG (1998) Precipitating factors in lymphedema: myths and realities. Cancer 83 (12 Suppl American):2814–2816. doi 10.1002/(SICI)1097-0142(19981215)83:12B+<2814
Hayes S, Cornish B, Newman B (2005) Comparison of methods to diagnose lymphoedema among breast cancer survivors: 6-month follow-up. Breast Cancer Res Treat 89(3):221–226. doi:10.1007/s10549-004-2045-x
O’Toole J, Jammallo LS, Miller CL, Skolny MN, Specht MC, Taghian AG (2013) Screening for breast cancer-related lymphedema: the need for standardization. Oncologist. doi:10.1634/theoncologist.2012-0387
Mahamaneerat WK, Shyu CR, Stewart BR, Armer JM (2008) Breast cancer treatment, BMI, post-op swelling/lymphoedema. J Lymphoedema 3(2):38–44
Norman SA, Localio AR, Potashnik SL, Simoes Torpey HA, Kallan MJ, Weber AL, Miller LT, Demichele A, Solin LJ (2009) Lymphedema in breast cancer survivors: incidence, degree, time course, treatment, and symptoms. J Clin Oncol 27(3):390–397. doi:10.1200/JCO.2008.17.9291
Clark B, Sitzia J, Harlow W (2005) Incidence and risk of arm oedema following treatment for breast cancer: a three-year follow-up study. Q J Med 98:343–348
Petrek JA, Heelan MC (1998) Incidence of breast carcinoma-related lymphedema. Cancer 83 (12 Suppl American):2776–2781. doi: 10.1002/(SICI)1097-0142(19981215)83:12B+<2776
Erickson VS, Pearson ML, Ganz PA, Adams J, Kahn KL (2001) Arm edema in breast cancer patients. J Natl Cancer Inst 93(2):96–111
Petrek JA, Senie RT, Peters M, Rosen PP (2001) Lymphedema in a cohort of breast carcinoma survivors 20 years after diagnosis. Cancer 92(6):1368–1377. doi:10.1002/1097-0142(20010915)92:6<1368
Acknowledgments
This project was supported by Award R01CA139118 (AGT), and Award P50CA089393 (AGT) from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the views of the National Cancer Institute or the National Institutes of Health. In addition, we would like to acknowledge Nadine R. Taghian, whose dedication helped expedite completion of this project. The authors are greatly appreciative of her efforts.
Disclosure
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Specht, M.C., Miller, C.L., Russell, T.A. et al. Defining a threshold for intervention in breast cancer-related lymphedema: what level of arm volume increase predicts progression?. Breast Cancer Res Treat 140, 485–494 (2013). https://doi.org/10.1007/s10549-013-2655-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-013-2655-2