Abstract
Introduction
African-American women are more likely than white women to have functional impairments after breast cancer (BC) surgery; however, no differences were found in self-reported health status surveys at 12+ months postsurgery.
Purpose
This analysis compared white and African-American BC survivors’ (BCS) health status, health-related quality of life, and the occurrence of physical impairments after BC treatment.
Methods
One hundred sixty-six women (130 white, 28 African-American, 8 other) were assessed for impairments preoperatively and at 1, 3, 6, 9, and 12+ months postsurgery. Health status was assessed at 12+ months using the Short Form Health Survey (SF36v2™). Analysis of variance estimated differences between groups for health status and impairment occurrence.
Results
No differences were found between groups for BC type, stage, grade, or tumor size; surgery type; or number of lymph nodes sampled. African-American BCS had more estrogen/progesterone receptor-negative tumors (p < 0.001; p = 0.036) and received radiation more frequently (p = 0.03). More African-American BCS were employed (p = 0.022) and reported higher rates of social activities (p = 0.011) but less recreational activities (p = 0.020) than white BCS. African-American BCS had higher rates of cording (p = 0.013) and lymphedema (p = 0.011) postoperatively. No differences were found in self-reported health status.
Conclusion
In a military healthcare system, where access to care is ubiquitous, there were no significant differences in many BC characteristics commonly attributed to race. African-American women had more ER/PR-negative tumors; however, no other BC characteristics differed between racial groups. African-American women exhibited more physical impairments, although their BC treatment only differed regarding radiation therapy. This suggests that African-American BCS may be at higher risk for physical impairments and should be monitored prospectively for early identification and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
There are approximately 2.5 million breast cancer survivors in the USA [1]. Although the incidence is greater among white women, the mortality rate is higher for African-Americans [1, 2]. African-American women are more likely to have aggressive (high-grade and hormone–receptor-negative) tumors [3–7] and higher mortality rates [1, 2]. However, health-related quality of life (HRQOL) studies regarding levels of physical functioning [8–10], general health [8], mental health [9], and emotional well-being [11] have yielded conflicting results in racial comparisons. The small number of studies conducted within populations with equal access to care has had conflicting results as well, with some reporting that health differences exist despite equal access [12, 13], and others reporting that equal healthcare access eliminates racial disparities [14]. Nevertheless, many health outcomes, including health status and certain physical impairments, have been under-evaluated in these populations.
Health status measures relative burden of disease and benefit of treatments on a patient [15, 16], while HRQOL measures the effect of a condition on a patient’s physical, psychological, emotional, and social well-being [17]. The early and late adverse effects of breast cancer treatment can impact both health status and HRQOL outcomes among breast cancer survivors and may do so differently based on race [8].
The purpose of this analysis is to compare health status, HRQOL, and the occurrence of physical impairments between white and African-American breast cancer survivors participating in a physical therapy study within an equal-access military healthcare system.
Methods
Subject selection
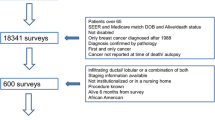
A prospective, observational studyFootnote 1 was conducted from 2001 to 2005 at the National Naval Medical Center Breast Care Center. All newly diagnosed breast cancer patients were screened preoperatively to determine eligibility for the trial. Patients were excluded if they were male, under 18 years old, diagnosed with bilateral breast cancer, or if they had a prior history of breast cancer, prior severe trauma, or surgery of the affected upper limb. All women who met the inclusion criteria and agreed to participate provided informed consent. The study used a physical therapy-based prospective surveillance model (Fig. 1) which included a baseline, preoperative evaluation, and interval postoperative assessment at 1, 3, 6, 9, and 12–24 months.
One hundred and ninety-six (196) women met eligibility requirements and enrolled preoperatively. One hundred and sixty-six (n = 166) participants who completed the preoperative assessment and at least one postoperative visit after 12–24 months were included in this subset analysis. The study population included 130 white women, aged 28 to 82 years (mean ± standard deviation [SD], 54.4 ± 12.5 years) and 28 African-American women, aged 34 to 66 years (mean ± SD, 51.0 ± 8.5 years). Eight participants with other racial designations were included in the group characteristic analysis but were not analyzed by race because of the small sample sizes. Subject characteristics for the entire group and for white and African-American participants are shown in Table 1. All participants had equivalent access to breast cancer screening and treatment in a military healthcare system.
Data collection and measurement
All patients were seen preoperatively for a physical therapy evaluation that included bilateral upper limb strength and range of motion (ROM) testing, and bilateral limb volume assessment. Baseline self-reported employment status, participation in physical activity, social activity, and recreational activity were also documented (Table 1). Physical activity examples included walking, running, and aerobics; social activity examples included involvement in church, volunteer groups, and social clubs; recreational activity examples included gardening, knitting, and other personal hobbies.
Subjects were assessed using a prospective surveillance model according to an algorithm previously described by these authors [18, 19] at 1, 3, 6, 9, and 12–24 months postoperatively to repeat baseline tests and measures, reassess self-reported activity levels and provide early intervention for any identified physical impairments.
Postoperative examinations documented physical impairments according to severity and location. Subject reports of musculoskeletal chest pain, shoulder pain, numbness, and fatigue were assessed using a numerical rating scale (NRS) from 0 (no symptoms) to 10 (worst possible sensation) [20]. Symptoms reported as >1 on NRS were identified as a complaint. Severity scales for axillary web syndrome (cording) and seroma were ranked as none, present and asymptomatic, or present and symptomatic. Cording is described as a ropelike structure, usually found in the axilla extending into the upper extremity, which may cause pain and restrict arm ROM after breast cancer-related axillary surgery [21]. Seroma is an above normal collection of serous fluid which can develop in the breast, axilla, or skin flaps formed during a mastectomy [22].
Bilateral upper limb measurements were taken in a standard position as described by Stout Gergich et al. [18] with the Perometer® [23].Footnote 2 The Perometer® calculates total limb volume (milliliter) for each extremity and allows interlimb comparison as well as comparison of change over time. Diagnostic criterion for lymphedema [18] was a limb volume increase of ≥3% in the affected limb from baseline as compared to the unaffected limb volume change. Body weight was taken at each visit with a standard scale [19].Footnote 3
Examination findings at 12–24 months (mean ± SD, 14.38 ± 4.31 months) postsurgery were analyzed for endpoint data. These examinations included provision of the SF36v2™. The analysis used the total SF36v2™ scores and the standardized scores of each subscale: physical functioning, role-physical, body pain, general health (which complete the Physical Health Summary Scale), mental health, vitality, social functioning, and role-emotional (which complete the Mental Health Summary Scale). Each scale score has been accepted as a valid calculation of the burden of disease [15, 24]. The Social Functioning Scale was used as a correlate of HRQOL. Participants also completed the Harvard Alumni Health Study Physical Activity Questionnaire (HPAQ) [25] to assess physical activity levels, in addition to the shortened Disabilities of Arm, Shoulder and Hand Questionnaire (QuickDASH) [26].
Statistical analyses
Statistical analyses for baseline and endpoint data were performed by SPSS software (Version 15.0; SPSS, Inc., Chicago, IL, USA). Descriptive statistics were calculated for all variables. Scores for each subscale of the SF36v2™ were analyzed with one-way repeated analysis of variance to test whether scores were significantly different (p ≤ 0.05) between white and African-American groups. Presence of lymphedema, cording, fatigue, musculoskeletal chest pain, shoulder pain, and numbness were tested by the Pearson chi-square test or Fisher’s exact test to identify significant differences (p ≤ 0.05) between the two groups. Trends were defined as 10% or greater differences between the two groups’ nominal or ordinal data tested by the chi-squared test or Fisher’s exact test.
Results
Table 1 shows baseline characteristics of all subjects and of African-American and white participants. At baseline, African-American women were significantly more likely to be employed full-time (p = 0.022). Whites engaged in more recreational activity (p = 0.020), while African-American participants engaged in more social activity (p = 0.011). Table 2 shows activity examples. No baseline differences in social or functional history between groups were identified, nor were there differences in the incidence of comorbid conditions (Table 1).
Table 2 outlines the endpoint comparisons in health status, HRQOL, and physical impairments in African-American and whites. Ninety-seven (74.6%) whites and 15 (53.6%) African-Americans completed the SF36v2™ survey at endpoint. No significant differences were found between the two groups on average subscale scores, average summary scores, and average total score of the SF36v2™. No significant differences were found between whites and African-Americans in average QuickDASH scores although the survey response rate was less than the full cohort for both groups (71.5% and 42.9%, respectively). Ninety-seven (74.6%) whites and 11 (39.3%) African-American subjects completed the HPAQ with no significant differences found. Furthermore, due to the considerably lower response rate to the questionnaires in the African-American subjects, a t test was used to compare the characteristics of the African-American nonresponders to the responders. No significant difference was noted between these groups, verifying that the questionnaire responders were a representative sample of the African-American study subjects.
Table 3 highlights differences in breast cancer-related characteristics between groups. African-American women were more likely to have estrogen receptor (ER)-negative (p < 0.001) and progesterone receptor (PR)-negative (p = 0.036) tumors.
African-American women were more likely to have symptomatic cording (p = 0.0130) and lymphedema (p = 0.011) compared to white women. White women trended towards having fewer complaints of musculoskeletal chest pain and arm numbness as compared to African-American women but significance was not reached.
African-American participants were more likely than whites to receive radiation therapy (p = 0.030). The rates of chemotherapy or hormone therapy delivery between the two groups were not significant (Fig. 2).
Discussion
It is widely reported that African-American women are diagnosed with larger tumors of a more aggressive pathology, and at later disease stages [3–6], suggesting that African-American women have biologically different breast cancers compared to white women [27–29]. Historical evidence attributes this to differences in access to screening [4, 27, 30, 31], genetic predisposition [27, 28], and differences in cultural norms that may impact a patient’s willingness to seek screening and early treatment [32]. This analysis examined racial differences in the physical impairment rates and health status of breast cancer survivors treated within a military healthcare system where insurance coverage and access to care were ubiquitous before, during, and after diagnosis and treatment. African-American patients did demonstrate pathologically different tumors from their white counterparts regarding ER and PR status; however, contrary to other reports there were no significant differences in grade, stage, type, or size of tumor between white and African-American women. These important findings may speak to the ability for earlier diagnosis of breast cancer in a health care delivery system that enables open access to all patients regardless of socioeconomic status.
Historical research suggests that racial minorities are more likely than whites to be categorized as having lower socioeconomic status (SES) [33] and that lower SES is associated with poorer health status in cancer [34, 35]. The provision of health care in the military system essentially controls for SES, diminishing its impact as a significant factor in the outcomes presented here. The demographic similarities seen between groups (Table 1) may have influenced endpoint health status, which suggests that controlling for SES may eliminate some disparities between white and African-American breast cancer survivors.
Other baseline characteristics, such as weight, Body Mass Index (BMI), and self-reported activity levels, may have also influenced subjects’ physical impairment occurrences at endpoint. Although no statistical significance was noted in weight or BMI differences between the groups, a trend showed that the African-American women tended to be more overweight than their white counterparts (Table 1). Overweight and obese BMI classifications also correlate with a higher risk of lymphedema [36–39]. These factors may help explain why African-American participants were more likely than white participants to develop lymphedema. There was also a trend showing that African-American participants were less engaged in physical activity prior to treatment, which may have affected their postsurgery physical impairment level.
The impact of physical activity on BC survivors’ posttreatment HRQOL and physical impairment occurrence is uncertain [36, 39]. Considering the differences in physical activity levels between the African-American and white participants, along with the subsequent differences in the two groups’ occurrence of physical impairments, results suggest a relationship between physical activity and postsurgery physical impairment.
The treatment differences between the two groups reflect the differences in their breast cancer characteristics, especially hormone receptor status. With significantly more ER- and PR-negative tumors, African-American women were more likely to receive radiation therapy and showed a trend to be less likely than white women to receive hormonal therapy. Radiation therapy can also increase risk for lymphedema [40–42] and may have been a factor in the significance of lymphedema as a more prevalent impairment in African-American women.
There was no significant difference in rate of axillary lymph node dissection or sentinel lymph node biopsy between white and African-American participants. The analysis did, however, demonstrate that African-American women were significantly more likely than white women to have symptomatic impairments, including lymphedema and cording, at endpoint suggesting a difference in the physical response of African-American women to breast cancer surgery and lymph node dissection.
Lymphedema presents as tissue swelling in the limb affected by breast cancer surgery and lymph node dissection [18]. Risk factors associated with the onset of lymphedema include high BMI [36–39], low physical activity levels [43], and radiation therapy [40–42]. The trends in this analysis showed that African-American women had higher BMI classifications and lower levels of physical activity than white women, in addition to being significantly more likely to receive radiation therapy. These factors may have contributed to African-American participants’ higher tendency to suffer from lymphedema over time. Evidence supports the findings that African-American breast cancer survivors are more likely than white breast cancer survivors to suffer from postsurgery physical impairments, including lymphedema [9, 10] and a decrease in physical functioning [8, 10, 11, 44, 45]. Nevertheless, the two groups had no differences in other factors attributable to the onset of lymphedema including age [36], history of hypertension [36], type of breast cancer surgery [37, 39], lymph node dissection [37], and number of lymph nodes taken [36, 37].
African-American participants were significantly more likely to experience cording at endpoint, but there were no differences between whites and African-Americans in incidence of seroma. Risk factors for cording include type of axillary surgery (showing a higher risk with axillary dissection than with sentinel node biopsy), radiation therapy, and lower BMI [21, 46, 47]. African-American participants in the study had higher rates of radiation therapy, but there was no difference between patients in type of axillary surgery, and African-Americans did not have lower BMI than white participants suggesting vulnerability for African-American breast cancer survivors to posttreatment cording. The two groups did not differ in the frequency of seroma formation, which has been attributed to surgery type, drainage flow rate, and increased body weight [22].
Although African-American participants in the cohort were more likely to suffer from specific physical impairments at endpoint, contrary to other studies [8–11, 44], there were no differences in self-reported health status or HRQOL found. In addition, both groups’ mean Physical Health and Mental Health Summary Scales were well above the USA average SF36v2™ score of 50.0 [15], indicating that participants perceived themselves to have excellent health status.
The cohort had no difference in each SF36v2™ subscale score, summary score, or total score. There were also no differences in scores for QuickDASH or HPAQ suggesting that the study population maintained functional capacity throughout treatment. This may be attributable to physical therapy intervention and education provided pre- and postoperatively, in addition to participants’ vocational status and active lifestyle requirements. Although impairments were more evident in the African-American women, they were not deterred in returning to functional activities; however, their activities tended to be of a more social nature rather than physical.
Having a social support system correlates with better emotional well-being [44], mental health [9], and HRQOL [11]. African-American survivors are more likely to depend on social networks (including church and extended family) to help cope with their illness than their white counterparts [9, 11, 44, 48]. Our analysis supports this finding; African-American subjects were more likely to participate in social activity, while whites were more likely to participate in recreational activity. However, despite this distinction, there were no differences between African-American and white breast cancer survivors in health status, determined by SF36v2™ or HRQOL, determined by the SF36v2™ Social Functioning Subscale. The lack of differences between the two groups in overall mental and physical health shows that social activity, recreational activity, and equal access to care may be factors in eliminating disparities between African-American and white breast cancer survivors’ postsurgery health status and HRQOL. More research is needed to discover the correlations between recreational activity and postsurgery mental and emotional health in breast cancer survivors.
Clinical relevance
The results suggest that in a health care system where care is equally delivered regardless of socioeconomic status or population demographics, differences in functional and health status still exist. The related clinical implications may be broad reaching with regard to breast cancer diagnosis and treatment and should be further examined.
Recognizing that the African-American subjects in the cohort suffered from more postoperative impairments confirms the need for ongoing prospective surveillance by a rehabilitation specialist. African-American women appear to be a high-risk group that should be monitored in the absence of impairment to enable early detection and early intervention for breast cancer-related impairments. When impairments such as lymphedema and axillary web syndrome are identified early the intervention is less intense and promotes quicker return to function. Further, there may be a preventive effect from the physical therapy-based prospective surveillance model’s ongoing care and educational components.
Limitations
This study was conducted in a military health care system, which may not be reflective of the general US population. The cohort is comprised of active duty women, spouses of active duty military members, retirees, and their spouses. The substantial difference in overall participation in the study must be considered in light of the results. A greater percentage of white participants completed the surveys compared to African-American participants, which may have been due to the mailing process used. However, all subjects completed the assessments that measured physical impairments. A larger African-American cohort would perhaps provide better insight to the significance levels of the study variables that trended towards but did not reach significance.
Conclusion
Racial disparities are known to exist and impact breast cancer diagnosis and treatment and may impact a patient’s physical and functional capacity. In a cohort of patients who have equal access to care and participate in a surveillance model of care, an increased prevalence of lymphedema and cording is present in African-American participants compared with white participants. The health status measures demonstrate no differences. The combination of increased lymphedema, higher rate of radiation therapy, and a trend towards a lower level of physical activity put the African-American group at risk for physical impairments and possible functional loss with time. Close observation of African-American breast cancer survivors should be implemented to monitor and reduce these racially disparate risks in breast cancer survivors.
Notes
National Institutes of Health (NIH) Protocol 02-CC-0044; National Naval Medical Center (NNMC) Protocol B01-052
Pero-System Messgerate, Am Tescher Busch 9, D-42327, Wuppertal, Germany
Detecto Model CN20, Webb City, MO, USA
References
American Cancer Society (2009) Breast cancer facts and figures 2009–2010. American Cancer Society, Atlanta
Field TS, Buist DS, Doubeni C et al (2005) Disparities and survival among breast cancer patients. J Natl Cancer Inst Monogr 35:88–95
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V (2007) Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor. Cancer 109(9):1721–1728
Shavers VL, Harlan LC, Stevens JL (2003) Racial/ethnic variation in clinical presentation, treatment, and survival among. Cancer 97(1):134–147
Bigby J, Holmes MD (2005) Disparities across the breast cancer continuum. Cancer Causes Control 16(1):35–44
Bradley CJ, Given CW, Roberts C (2002) Race, socioeconomic status, and breast cancer treatment and survival. J Natl Cancer Inst 94(7):490–496
Simon MS, Severson RK (1997) Racial differences in breast cancer survival: the interaction of socioeconomic status and tumor biology. Am J Obstet Gynecol 176(6):S233–S239
Paskett ED, Alfano CM, Davidson MA et al (2008) Breast cancer survivors' health-related quality of life: racial differences and comparisons with noncancer controls. Cancer 113(11):3222–3230
Bowen DJ, Alfano CM, McGregor BA et al (2007) Possible socioeconomic and ethnic disparities in quality of life in a cohort of breast cancer survivors. Breast Cancer Res Treat 106(1):85–95
Eversley R, Estrin D, Dibble S, Wardlaw L, Pedrosa M, Favila-Penney W (2005) Post-treatment symptoms among ethnic minority breast cancer survivors. Oncol Nurs Forum 32(2):250–256
Janz NK, Mujahid MS, Hawley ST et al (2009) Race/ethnicity, physical activity, and quality of life in breast cancer. J Cancer Surviv 3(4):212–222
Jatoi I, Becher H, Leake CR (2003) Widening disparity in survival between white and African-American patients with breast carcinoma treated in the U.S. Department of Defense Healthcare system. Cancer 98(5):894–899
Halmin M, Bellocco R, Lagerlund M, Karlsson P, Tejler G, Lambe M (2008) Long-term inequalities in breast cancer survival—a ten year follow-up study of patients managed within a National Health Care System (Sweden). Acta Oncol 47(2):216–224
Du W, Simon MS (2005) Racial disparities in treatment and survival of women with stage I-III breast cancer at a large academic medical center in metropolitan Detroit. Breast Cancer Res Treat 91(3):243–248
Ware JE Jr, Gandek B (1998) Overview of the SF-36 Health Survey and the International Quality of Life. J Clin Epidemiol 51(11):903–912
Hawthorne G, Osborne RH, Taylor A, Sansoni J (2007) The SF36 version 2: critical analyses of population weights, scoring algorithms and population norms. Qual Life Res 16(4):661–673
Cella DF (1994) Quality of life: concepts and definition. J Pain Symptom Manage 9(3):186–192
Stout Gergich NL, Pfalzer LA, McGarvey C, Springer B, Gerber LH, Soballe P (2008) Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer 112(12):2809–2819
Springer B, Levy E, McGarvey C et al (2010) Pre-operative assessment enables early diagnosis and recovery of shoulder function in patients with breast cancer. Breast Cancer Res Treat 120(1):135–147
Brunelli C, Zecca E, Martini C et al (2010) Comparison of numerical and verbal rating scales to measure pain exacerbations in patients with chronic cancer pain. Health Qual Life Outcomes 8:42
Leduc O, Sichere M, Moreau A et al (2009) Axillary web syndrome: nature and localization. Lymphology 42(4):176–181
Agrawal A, Ayantunde AA, Cheung KL (2006) Concepts of seroma formation and prevention in breast cancer surgery. ANZ J Surg 76(12):1088–1095
Stanton AW, Northfield JW, Holroyd B, Mortimer PS, Levick JR (1997) Validation of an optoelectronic limb volumeter (Perometer). Lymphology 30(2):77–97
Ware JE Jr (1976) SF-36 health survey update. Spine (Phila Pa 1976) 25(24):3130–3139
Albanes D, Conway JM, Taylor PR, Moe PW, Judd J (1990) Validation and comparison of eight physical activity questionnaires. Epidemiology 1(1):65–71
Gummesson C, Ward MM, Atroshi I (2006) The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord 7:44
Elmore JG, Moceri VM, Carter D, Larson EB (1998) Breast carcinoma tumor characteristics in black and white women. Cancer 83(12):2509–2515
Wojcik BE, Spinks MK, Optenberg SA (1998) Breast carcinoma survival analysis for African American and white women in an equal-access health care system. Cancer 82(7):1310–1318
Shiao YH, Chen VW, Scheer WD, Wu XC, Correa P (1995) Racial disparity in the association of p53 gene alterations with breast cancer survival. Cancer Res 55(7):1485–1490
Weiss HA, Brinton LA, Brogan D et al (1996) Epidemiology of in situ and invasive breast cancer in women aged under 45. Br J Cancer 73(10):1298–1305
Weinick RM, Zuvekas SH (2000) Experience of primary care by racial and ethnic groups. Med Care 38(4):447–448
Phillips JM, Cohen MZ, Moses G (1999) Breast cancer screening and African American women: fear, fatalism, and silence. Oncol Nurs Forum 26(3):561–571
Williams DR (1996) Race/ethnicity and socioeconomic status: measurement and methodological issues. Int J Health Serv 26(3):483–505
Fiscella K, Franks P, Gold MR, Clancy CM (2000) Inequality in quality: addressing socioeconomic, racial, and ethnic disparities. Jama 283(19):2579–2584
Ward E, Jemal A, Cokkinides V et al (2004) Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin 54(2):78–93
Meeske KA, Sullivan-Halley J, Smith AW et al (2009) Risk factors for arm lymphedema following breast cancer diagnosis in Black women. Breast Cancer Res Treat 113(2):383–391
Hack TF, Kwan WB, Thomas-Maclean RL (2010) et al. Predictors of arm morbidity following breast cancer surgery. Psychooncology 22
Helyer LK, Varnic M, Le LW, Leong W, McCready D (2009) Obesity is a risk factor for developing postoperative lymphedema in breast cancer. Breast J 16(1):48–54
Sagen A, Karesen R, Risberg MA (2009) Physical activity for the affected limb and arm lymphedema after breast cancer. Acta Oncol 48(8):1102–1110
Cormier JN, Askew RL, Mungovan KS, Xing Y, Ross MI, Armer JM. Lymphedema beyond breast cancer: a systematic review and meta-analysis of cancer-related secondary lymphedema. Cancer. doi:10.1002/cncr.25458
Tsai RJ, Dennis LK, Lynch CF, Snetselaar LG, Zamba GK, Scott-Conner C (2009) The risk of developing arm lymphedema among breast cancer survivors: a meta-analysis of treatment factors. Ann Surg Oncol 16(7):1959–1972
Swenson KK, Nissen MJ, Leach JW, Post-White J (2009) Case-control study to evaluate predictors of lymphedema after breast cancer surgery. Oncol Nurs Forum 36(2):185–193
Smith AW, Alfano CM, Reeve BB et al (2009) Race/ethnicity, physical activity, and quality of life in breast cancer. Cancer Epidemiol Biomarkers Prev 18(2):656–663
Rao D, Debb S, Blitz D, Choi SW, Cella D (2008) Racial/Ethnic differences in the health-related quality of life of cancer. J Pain Symptom Manage 36(5):488–496
Giedzinska AS, Meyerowitz BE, Ganz PA, Rowland JH (2004) Health-related quality of life in a multiethnic sample of breast cancer survivors. Ann Behav Med 28(1):39–51
Torres Lacomba M, Mayoral Del Moral O, Coperias Zazo JL, Yuste Sanchez MJ, Ferrandez JC, Zapico Goni A (2009) Axillary web syndrome after axillary dissection in breast cancer: a prospective study. Breast Cancer Res Treat 117(3):625–630
Leidenius M, Leppanen E, Krogerus L, von Smitten K (2003) Motion restriction and axillary web syndrome after sentinel node biopsy and axillary clearance in breast cancer. Am J Surg 185(2):127–130
Ashing-Giwa KT, Padilla G, Tejero J et al (2004) Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina, and Caucasian cancer survivors. Psychooncology 13(6):408–428
Acknowledgments
This study was supported by the National Naval Medical Center (National Naval Medical Center [NNMC] Protocol NNMC 2001–052) and by the National Institutes of Health (NIH), Clinical Center, Rehabilitation Medicine Department, Physical Therapy Section (Protocol NIH 02-CC-0044).
Author information
Authors and Affiliations
Corresponding author
Additional information
All authors have read and approved this manuscript.
The views expressed in this article are those of the author(s) and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. Government.
Rights and permissions
About this article
Cite this article
Morehead-Gee, A.J., Pfalzer, L., Levy, E. et al. Racial disparities in physical and functional domains in women with breast cancer. Support Care Cancer 20, 1839–1847 (2012). https://doi.org/10.1007/s00520-011-1285-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-011-1285-7