Abstract
Purpose
Bacteremia is an important clinical condition in febrile neutropenia that can cause clinical failure of antimicrobial therapy. The purpose of this study was to investigate the clinical factors predictive of bacteremia in low-risk febrile neutropenia at initial patient evaluation.
Methods
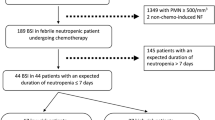
We performed a retrospective cohort study in a university hospital in Seoul, Korea, between May 1995 and May 2007. Patients who met the criteria of low-risk febrile neutropenia at the time of visit to emergency department after anti-cancer chemotherapy were included in the analysis.
Results
During the study period, 102 episodes of bacteremia were documented among the 993 episodes of low-risk febrile neutropenia. Single gram-negative bacteremia was most frequent. In multivariate regression analysis, initial body temperature ≥39°C, initial hypotension, presence of clinical sites of infection, presence of central venous catheter, initial absolute neutrophil count <50/mm3, and the CRP ≥10 mg/dL were statistically significant predictors for bacteremia. A scoring system using these variables was derived and the likelihood of bacteremia was well correlated with the score points with AUC under ROC curve of 0.785. Patients with low score points had low rate of bacteremia, thus, would be candidates for outpatient-based or oral antibiotic therapy.
Conclusions
We identified major clinical factors that can predict bacteremia in low-risk febrile neutropenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Febrile neutropenia is a potentially life-threatening condition in patients undergoing chemotherapy for cancer [1]. Although febrile neutropenia is frequently associated with high medical risk to varying degrees [2–5], it can occur in patients with low risk for serious clinical outcome. It is important to identify the patients with low risk for serious medical complications or death who can be treated with outpatient-based oral antibiotic therapy [3, 6–8]. Currently, the clinical risk prediction model proposed by the Multinational Association for Supportive Care in Cancer (MASCC) is widely used in the clinical practice to define low-risk febrile neutropenia [6, 9, 10].
Febrile neutropenia can be caused by various primary diseases, among which bacteremia is the most critical condition. Clinicians who are treating febrile neutropenic patients at the outpatient clinic or emergency department (ED) should consider the possibility of bacteremia because it can cause the clinical failure of oral antibiotic therapy [11–14]. Early prediction and treatment of bacteremia is clinically important for ultimate clinical outcome of febrile neutropenia. However, the current clinical prediction model may not be accurate in predicting the possibility of bacteremia, especially in low-risk febrile neutropenic patients. In the present study, we analyzed the clinical factors predictive of bacteremia in low-risk febrile neutropenia at initial patient evaluation.
Methods
Study design
A retrospective cohort study was conducted to evaluate the clinical features and outcome of bacteremia and neutropenia in cancer patients. Patients who visited the ED of the Samsung Medical Center due to febrile neutropenia after anti-cancer chemotherapy between May 1995 and May 2007 were included in this study. Samsung Medical Center is a tertiary care university hospital with 1,950 beds located in Seoul, South Korea. Demographic data, clinical features, and outcome data were collected retrospectively based on the review of the medical records.
Study population and definition
All patients with neutropenia at the time of visiting ED were screened using the electronic medical record system. Neutropenia was defined as an absolute neutrophil count <0.5 × 109 cells/L or <1.0 × 109 cells/L and expected to fall below 0.5 × 109 cells/L within 24–48 h because of antecedent anti-cancer chemotherapy [10]. Fever was defined as a single temperature of ≥38.3°C or a temperature of 38.0°C for ≥1 h. For each episode, the MASCC score was assessed retrospectively. The low-risk group was defined as patients with MASCC score ≥21 [6]. Episodes that met the criteria of low-risk febrile neutropenia were enrolled in the study group. Each febrile episode was categorized as an unexplained fever (UF), clinically documented infection (CDI), or microbiologically documented infection (MDI) according to the guidelines of the Infectious Diseases Society of America (IDSA) [10, 15]. Diagnosis of febrile neutropenia and treatment decision were up to the physicians in charge, who followed the updated guidelines of IDSA at the time [10, 16]. Bacteremia was defined as the isolation of bacterial pathogens from blood cultures with the presence of clinical signs and symptoms of infection. A single isolation of coagulase-negative staphylococci, Corynebacterium species, Bacillus species other than Bacillus anthracis, or Micrococcus species in blood was considered contamination [17, 18]. To look at the changes in microbiology and therapy over time, we divided the study period into two stages; the duration between May 1995 and May 2001 was assigned to the first period and the duration between June 2001 and May 2007 to the second period.
Exclusion criteria were as follows: (1) patients who were <18 years of age at the time of visiting ED, (2) patients who had no history of anti-cancer chemotherapy before the development of neutropenia, and (3) patients who had no documented fever during the hospital stay.
Statistical analysis
The Student’s t test and Mann–Whitney U test were used to compare continuous variables, and the χ2 or Fisher’s exact test was used to compare categorical variables. All reported P values were two-tailed, and a P < 0.05 was considered statistically significant. Variables that were associated with bacteremia in the univariate analyses (P < 0.05) were entered into a multivariate logistic regression analysis using stepwise selection. Continuous variables were re-categorized into binary factors using the most discriminant cutoff point. The goodness of fit of the model was tested with the Hosmer-Lemeshow test, which revealed adequate model fit (P = 0.662).
We assigned score points to each risk factor according to the regression coefficients. Then, the whole score was obtained by summing the individual points for each patient and probability of bacteremia for each score was calculated. Finally, we performed a receiver-operating characteristic (ROC) curve analysis and computed the area under the ROC curve and its corresponding 95% confidence interval (CI).
Results
Patient characteristics and clinical features
During the study period, a total of 993 episodes of low-risk febrile neutropenia in 802 patients were collected. The median age of the patients was 50 years and the male-to-female ratio was 0.86. Solid tumors were the most common underlying malignancy (73%), followed by lymphoma (24%) and hematologic diseases (3%). Among the solid tumors, the most common malignancy was breast cancer (25%), followed by lung cancer (14%) and gastrointestinal tract malignancy (12%; Table 1). The majority of febrile episodes were UF (589 cases, 59.3%) followed by CDI (266 cases, 26.8%) and MDI (138 cases, 13.9%). Twelve (1.2%) were admitted to intensive care unit, and ten (1.0%) needed mechanical ventilation. Anti-pseudomonal beta-lactam-based antibiotic regimens were used in 950 (95.6%) cases. Granulocyte colony stimulating factor was administered at least once in 956 (96.3%) cases. The all-cause 30-day mortality rate was 1.1% (11 cases) with no differences between the groups, but all-cause in hospital mortality rate was higher in the bacteremia group (4.9% vs. 1.2% P = 0.018).
Of the total 993 cases, blood cultures were done in 989 (99.6%) cases and were not done in four cases (0.4%). Among these 989 episodes, 102 episodes of bacteremia and one episode of fungemia (invasive cryptococcal disease) were found. Monomicrobial gram-negative bacteremia accounted for 48% (49 episodes), monomicrobial gram-positive bacteremia 37% (38 episodes), and polymicrobial bacteremia 15% (15 episodes). Of the 102 episodes of bacteremia, Escherichia coli was the most frequent pathogen isolated (21 episodes, 20.6%) followed by coagulase-negative staphylococci (19 episodes, 18.6%), Klebsiella species and Staphylococcus aureus (16 episodes, 15.7% for each) and Pseudomonas aeruginosa (15 episodes, 14.7%). The changes in microbiology, antibiotic treatment and 30-day mortality over time were not statistically significant except that commonly used antibiotic regimen was switched from ceftazidime based in the first period to cefepime based in the second period (Table 2).
Clinical parameters associated with bacteremia and derivation of scoring system
Clinical characteristics and outcome according to the documentation of bacteremia are summarized in Table 3. Lymphoma or hematologic disease were significantly more frequent underlying malignancies in bacteremic patients (P = 0.02). The patients with bacteremia were more likely to have defined clinical sites of infection than non-bacteremic patients (70% vs. 34%, respectively; P < 0.001). Serum levels of initial C-reactive protein (CRP) were available in 789 (80%) cases with similar proportion of missed data in the two groups (21.6% in “Bacteremia” group vs. 20.0% in “No bacteremia” group, P = 0.704). In univariate analysis, clinical factors associated with bacteremia were lymphoma or hematologic disease as the underlying malignancy, presence of central venous catheter, presence of clinical sites of infection, initial absolute neutrophil count <50/mm3, initial body temperature ≥39°C, presence of initial hypotension, and higher levels of CRP. When we performed a multivariate logistic regression analysis on the 789 episodes with available initial CRP level, presence of clinical sites of infection, initial hypotension, presence of central venous catheter, body temperature ≥39°C, initial absolute neutrophil count <50/mm3, and CRP ≥10 mg/dL were statistically significant predictors for bacteremia. We then assigned score points to each risk factor according to the weight of regression coefficient for simple and easy use at bedside as shown in Table 4. An 8-point scale (0–7) scoring model was derived and the 789 subjects were categorized into eight groups according to their score (Table 5). No one in the study population scored 8 points. The rate of bacteremia increased in concordance with the increasing score, it ranged from 1.1% with 0 point to 66.7% with 7 points. For the subjects who had no risk factors (in other words, subjects with 0 point), the negative predictive value for bacteremia was 98.9%. The accuracy of scoring model to predict bacteremia, measured by the area under the ROC curve, was 0.785 (95% CI, 0.733–0.837).
Discussion
In the present study, we found the clinical factors to predict bacteremia in low-risk febrile neutropenia. A simple scoring system based on six clinical and laboratory data were derived and was well correlated with the rate of bacteremia. If a patient scores 0 or 1 point, this patient could be a candidate for outpatient or oral antibiotic therapy because the probability of bacteremia is very low. If the patient scores more points, the probability of bacteremia would increase higher and the patient would need inpatient-based intravenous antibiotic therapy while awaiting the blood culture results.
Although bacteremia is not considered as a serious medical complication or a high-risk factor in the current risk scoring system such as the MASCC index score, it is related to poor outcome in febrile neutropenia in both high-risk and low-risk patients [11–14, 19–25]. Therefore, early prediction of bacteremia in patients with febrile neutropenia might be important to decide empirical therapy at the initial assessment and management. In a previous study, shock, very high fever, presence and location of signs of infection, long-lasting granulocytopenia, thrombocytopenia, and administration of antifungal prophylaxis were predictive for bacteremia [26]. However, most of the patients in this study had hematologic malignancies and the authors failed to show predictability when tested in the validation set. In our study, shock, very high fever, and presence of local infectious signs were also confirmed to be predictive of bacteremia. In addition, our data revealed that severe neutropenia (absolute neutrophil count <50/mm3), increased level of CRP, and the presence of central venous catheter were other predictors of bacteremia. In another study, variables such as absolute neutrophil count, absolute phagocyte count, temperature, or platelet count were analyzed in pediatric patients who had hematologic malignancies or solid tumors and an absolute monocyte count ≥155/mm3 was the only factor for the lowest risk of bacteremia [27]. This could not be a good guide in caring adult patients considering different clinical situations and management principles between pediatric and adult patients. The risk of bacteremia during febrile neutropenia has been studied mostly in patients with hematological malignancies undergoing hematopoietic stem cell transplantations [26, 28, 29]. Data from patients with solid tumors have been lacking, while the prevalence of febrile neutropenia in this group has been increasing. But, majority of patients enrolled in our study had solid tumors (73%) and the data would be useful in managing low risk febrile neutropenia with solid tumors.
The majority of causative microorganisms in this study were gram-negative bacteria. Previous studies have shown that infections caused by gram-positive bacteria have increased during the past few decades and now accounts for 60–70% of MDI [10, 30, 31]. It may be due to increasing use of long-term indwelling catheters, use of more cytotoxic chemotherapeutic drugs which can lead to increased infection with Enterococcus or Viridans streptococcus and fluoroquinolone prophylaxis [32, 33]. In contrast, the current study showed a higher prevalence of gram-negative organisms than gram-positive organisms (56.3% vs. 43.7%) in our institution. The increasing trend in the rate of gram-positive bacteremia over time was seen in our study but not prominent. One of the possible reasons for this finding is that we do not do antibacterial prophylaxis (e.g., fluoroquinolones) in cancer patients undergoing anti-cancer chemotherapy. In addition, because our patient population is outpatient-based and low-risk group with majority of the patients having solid tumors, the microbiologic features of bacteremia in the whole group including high-risk group, patients with hematologic malignancies, or inpatient setting might be different from our data. Nevertheless, the distribution of major pathogens such as E. coli, S. aureus, and coagulase-negative staphylococci in this study was consistent with other data [34, 35].
There are several limitations in this study. First, since this is a retrospective study, some of the clinical data were not available. Blood cultures were not done in four cases and CRP level was not checked in 199 cases, thus we had to do statistical analyses on 789 out of 993 cases. However, other clinical factors were not missed because our hospital has an electronic medical record system that can preserve vital sign records, doctors’ notes, orders, and lab results in the computer-based system. Secondly, our scoring systems could not be validated in a separate patient population, which should be validated before it is routinely used.
In conclusion, we found simple clinical predictors for bacteremia in low-risk febrile neutropenia; the presence of clinical sites of infection, high body temperature, hypotension, absolute neutrophil count <50/mm3, and CRP ≥10 mg/dL. Data from this study could be useful in managing patients at initial evaluation by providing relevant clinical criteria for selecting candidates for outpatient-based oral antibiotic therapy in low-risk febrile neutropenic patients.
References
Bodey GP, Buckley M, Sathe YS, Freireich EJ (1966) Quantitative relationships between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med 64:328–340
Feld R (2008) Bloodstream infections in cancer patients with febrile neutropenia. Int J Antimicrob Agents 32:S30–S33
Talcott JA, Finberg R, Mayer RJ, Goldman L (1988) The medical course of cancer patients with fever and neutropenia. Clinical identification of a low-risk subgroup at presentation. Arch Intern Med 148:2561–2568
Schimpff SC, Gaya H, Klastersky J, Tattersall MH, Zinner SH (1978) Three antibiotic regimens in the treatment of infection in febrile granulocytopenic patients with cancer. The EORTC international antimicrobial therapy project group. J Infect Dis 137:14–29
Pizzo PA, Hathorn JW, Hiemenz J, Browne M, Commers J, Cotton D, Gress J, Longo D, Marshall D, McKnight J et al (1986) A randomized trial comparing ceftazidime alone with combination antibiotic therapy in cancer patients with fever and neutropenia. N Engl J Med 315:552–558
Klastersky J, Paesmans M, Rubenstein EB, Boyer M, Elting L, Feld R, Gallagher J, Herrstedt J, Rapoport B, Rolston K, Talcott J (2000) The Multinational Association for Supportive Care in Cancer risk index: a multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol 18:3038–3051
Cameron D (2009) Management of chemotherapy-associated febrile neutropenia. Br J Cancer 101(Suppl 1):S18–S22
Chamilos G, Bamias A, Efstathiou E, Zorzou PM, Kastritis E, Kostis E, Papadimitriou C, Dimopoulos MA (2005) Outpatient treatment of low-risk neutropenic fever in cancer patients using oral moxifloxacin. Cancer 103:2629–2635
Uys A, Rapoport BL, Anderson R (2004) Febrile neutropenia: a prospective study to validate the Multinational Association of Supportive Care of Cancer (MASCC) risk-index score. Support Care Cancer 12:555–560
Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, Feld R, Pizzo PA, Rolston KV, Shenep JL, Young LS (2002) 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 34:730–751
Kern WV, Cometta A, De Bock R, Langenaeken J, Paesmans M, Gaya H (1999) Oral versus intravenous empirical antimicrobial therapy for fever in patients with granulocytopenia who are receiving cancer chemotherapy. International Antimicrobial Therapy Cooperative Group of the European Organization for Research and Treatment of Cancer. N Engl J Med 341:312–318
Klastersky J, Paesmans M, Georgala A, Muanza F, Plehiers B, Dubreucq L, Lalami Y, Aoun M, Barette M (2006) Outpatient oral antibiotics for febrile neutropenic cancer patients using a score predictive for complications. J Clin Oncol 24:4129–4134
Freifeld A, Marchigiani D, Walsh T, Chanock S, Lewis L, Hiemenz J, Hiemenz S, Hicks JE, Gill V, Steinberg SM, Pizzo PA (1999) A double-blind comparison of empirical oral and intravenous antibiotic therapy for low-risk febrile patients with neutropenia during cancer chemotherapy. N Engl J Med 341:305–311
Sebban C, Dussart S, Fuhrmann C, Ghesquieres H, Rodrigues I, Geoffrois L, Devaux Y, Lancry L, Chvetzoff G, Bachelot T, Chelghoum M, Biron P (2008) Oral moxifloxacin or intravenous ceftriaxone for the treatment of low-risk neutropenic fever in cancer patients suitable for early hospital discharge. Support Care Cancer 16:1017–1023
Buchheidt D, Bohme A, Cornely OA, Fatkenheuer G, Fuhr HG, Heussel G, Junghanss C, Karthaus M, Kellner O, Kern WV, Schiel X, Sezer O, Sudhoff T, Szelenyi H (2003) Diagnosis and treatment of documented infections in neutropenic patients—recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 82(Suppl 2):S127–S132
Hughes WT, Armstrong D, Bodey GP, Brown AE, Edwards JE, Feld R, Pizzo P, Rolston KV, Shenep JL, Young LS (1997) 1997 guidelines for the use of antimicrobial agents in neutropenic patients with unexplained fever. Infectious Diseases Society of America. Clin Infect Dis 25:551–573
Link H, Bohme A, Cornely OA, Hoffken K, Kellner O, Kern WV, Mahlberg R, Maschmeyer G, Nowrousian MR, Ostermann H, Ruhnke M, Sezer O, Schiel X, Wilhelm M, Auner HW (2003) Antimicrobial therapy of unexplained fever in neutropenic patients—guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO), Study Group Interventional Therapy of Unexplained Fever, Arbeitsgemeinschaft Supportivmassnahmen in der Onkologie (ASO) of the Deutsche Krebsgesellschaft (DKG-German Cancer Society). Ann Hematol 82(Suppl 2):S105–S117
Hall KK, Lyman JA (2006) Updated review of blood culture contamination. Clin Microbiol Rev 19:788–802
Klastersky J, Ameye L, Maertens J, Georgala A, Muanza F, Aoun M, Ferrant A, Rapoport B, Rolston K, Paesmans M (2007) Bacteraemia in febrile neutropenic cancer patients. Int J Antimicrob Agents 30(Suppl 1):S51–S59
Elting LS, Rubenstein EB, Rolston KV, Bodey GP (1997) Outcomes of bacteremia in patients with cancer and neutropenia: observations from two decades of epidemiological and clinical trials. Clin Infect Dis 25:247–259
Karp JE, Merz WG, Hendricksen C, Laughon B, Redden T, Bamberger BJ, Bartlett JG, Saral R, Burke PJ (1987) Oral norfloxacin for prevention of gram-negative bacterial infections in patients with acute leukemia and granulocytopenia. A randomized, double-blind, placebo-controlled trial. Ann Intern Med 106:1–7
Love LJ, Schimpff SC, Schiffer CA, Wiernik PH (1980) Improved prognosis for granulocytopenic patients with gram-negative bacteremia. Am J Med 68:643–648
Pizzo PA (1981) Infectious complications in the child with cancer. I. Pathophysiology of the compromised host and the initial evaluation and management of the febrile cancer patient. J Pediatr 98:341–354
Klastersky J (1998) Science and pragmatism in the treatment and prevention of neutropenic infection. J Antimicrob Chemother 41(Suppl D):13–24
Viscoli C, Cometta A, Kern WV, Bock R, Paesmans M, Crokaert F, Glauser MP, Calandra T (2006) Piperacillin-tazobactam monotherapy in high-risk febrile and neutropenic cancer patients. Clin Microbiol Infect 12:212–216
Viscoli C, Bruzzi P, Castagnola E, Boni L, Calandra T, Gaya H, Meunier F, Feld R, Zinner S, Klastersky J et al (1994) Factors associated with bacteraemia in febrile, granulocytopenic cancer patients. The International Antimicrobial Therapy Cooperative Group (IATCG) of the European Organization for Research and Treatment of Cancer (EORTC). Eur J Cancer 30A:430–437
Baorto EP, Aquino VM, Mullen CA, Buchanan GR, DeBaun MR (2001) Clinical parameters associated with low bacteremia risk in 1100 pediatric oncology patients with fever and neutropenia. Cancer 92:909–913
Frere P, Baron F, Bonnet C, Hafraoui K, Pereira M, Willems E, Fillet G, Beguin Y (2006) Infections after allogeneic hematopoietic stem cell transplantation with a nonmyeloablative conditioning regimen. Bone Marrow Transplant 37:411–418
Norgaard M, Larsson H, Pedersen G, Schonheyder HC, Sorensen HT (2006) Risk of bacteraemia and mortality in patients with haematological malignancies. Clin Microbiol Infect 12:217–223
Ramphal R (2004) Changes in the etiology of bacteremia in febrile neutropenic patients and the susceptibilities of the currently isolated pathogens. Clin Infect Dis 39(Suppl 1):S25–S31
Zinner SH (1999) Changing epidemiology of infections in patients with neutropenia and cancer: emphasis on gram-positive and resistant bacteria. Clin Infect Dis 29:490–494
Del Favero A, Menichetti F, Martino P, Bucaneve G, Micozzi A, Gentile G, Furno P, Russo D, D’Antonio D, Ricci P, Martino B, Mandelli F (2001) A multicenter, double-blind, placebo-controlled trial comparing piperacillin-tazobactam with and without amikacin as empiric therapy for febrile neutropenia. Clin Infect Dis 33:1295–1301
Cordonnier C, Buzyn A, Leverger G, Herbrecht R, Hunault M, Leclercq R, Bastuji-Garin S (2003) Epidemiology and risk factors for gram-positive coccal infections in neutropenia: toward a more targeted antibiotic strategy. Clin Infect Dis 36:149–158
Link H, Maschmeyer G, Meyer P, Hiddemann W, Stille W, Helmerking M, Adam D (1994) Interventional antimicrobial therapy in febrile neutropenic patients. Study Group of the Paul Ehrlich Society for Chemotherapy. Ann Hematol 69:231–243
Kamana M, Escalante C, Mullen CA, Frisbee-Hume S, Rolston KV (2005) Bacterial infections in low-risk, febrile neutropenic patients. Cancer 104:422–426
Acknowledgments
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A090764).
Conflict of interest statement
There is no financial conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Ha, Y.E., Song, JH., Kang, W.K. et al. Clinical factors predicting bacteremia in low-risk febrile neutropenia after anti-cancer chemotherapy. Support Care Cancer 19, 1761–1767 (2011). https://doi.org/10.1007/s00520-010-1017-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-010-1017-4