Abstract
Goals of work
Patients with low-risk neutropenic fever as defined by the Multinational Association of Supportive Care in Cancer (MASCC) score might benefit from ambulatory treatment. Optimal management remains to be clearly defined, and new oral antibiotics need to be evaluated in this setting.
Materials and methods
Cancer patients with febrile neutropenia and a favorable MASCC score were randomized between oral moxifloxacin and intravenous ceftriaxone. All were fit for early hospital discharge. The global success rate was related to the efficacy of monotherapy, as well as to the success of ambulatory monitoring.
Main results
The trial was closed prematurely because of low accrual. Ninety-six patients were included (47 in the ceftriaxone arm and 49 in the moxifloxacin arm). A total of 65% were women, 30.2% had lymphoma, 34.4% had metastatic, and 35.4% had non-metastatic solid tumors. The success rates of home antibiotics were 73.9% and 79.2% for ceftriaxone and moxifloxacin, respectively. Seven patients were not discharged, and 14 required re-hospitalization. There were 17% of microbiologically documented infections that were, in most cases, susceptible to oral monotherapy.
Conclusions
These results suggest that MASCC is a valid and useful tool to select patients for ambulatory treatments and that oral moxifloxacin monotherapy is safe and effective for the outpatient treatment of cancer patients with low-risk neutropenic fever.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Febrile neutropenia is a potentially life-threatening complication of chemotherapy requiring hospitalization and empirical broad-spectrum intravenous antibiotics [11, 13, 22]. However, only a small proportion of patients develop serious morbidity. Some cooperative groups have identified predictive clinical criteria at fever onset to select patients at low risk for complications [16, 17, 27, 30]. Two main risk-prediction rules have been proposed and validated with a positive predictive value from 91% to 95%. The most recent one (Multinational Association for Supportive Care in Cancer, MASCC, score ), developed from a database of 1,139 episodes of neutropenia, defined a weighted scoring system of clinical factors [17]. A low-risk score was associated with absence of mortality and reduced morbidity (4.5%).
This MASCC score is considered a reliable tool for the selection of patients who might benefit from early hospital discharge and oral antibiotics.
Oral antibiotics have been evaluated in an inpatient setting, and two controlled trials comparing oral and parenteral administration have reported equivalence in terms of safety and efficacy [9, 15]. Both oral or parenteral antibiotics have been largely used in the outpatient setting with similar low readmission rates and high efficacy [7, 8, 10, 12, 18, 19, 21, 24, 29].
After our study of cefepime monotherapy, which demonstrated the safety and efficacy of cefepime in monotherapy in an inpatient setting [4], we have reported the feasibility and efficacy results of home intravenous cefepime antibiotics in a selected subset of low-risk patients [26].
Based on our previous experience, we initiated a multicentric randomized controlled trial, comparing oral versus parenteral antibiotics in cancer patients with low-risk febrile neutropenia defined by a MASCC score ≥21. Early hospital discharge on the day or within 2 days of therapy was organized for all patients.
Ceftriaxone, a third-generation parenteral cephalosporin, has been largely evaluated in this setting, with good efficacy and tolerance, and has the advantage of once-daily dosing [6, 14].
Moxifloxacin, a new broad-spectrum methoxyquinolone, has been reported to have higher activity against Gram-positive pathogens and anaerobes than older fluroquinolones while retaining good activity against Gram-negative pathogens [2, 3]. Furthermore, it is administered once daily and has favorable pharmacokinetic and pharmacodynamic profiles. The oral form is currently approved in France for the treatment of community-acquired respiratory tract infections. At the time the study was set up, no published data were available about its use in cancer patients with febrile neutropenia.
Materials and methods
Eligibility criteria
To be eligible, patients were to have received chemotherapy for a solid tumor, lymphoma, or myeloma in the previous month (patients with acute leukemia or undergoing autologous stem cell transplantation were excluded) and be aged 18 years or more.
Patients were required to have had an oral temperature ≥38.5°C once or ≥38°C twice in a period of 12 h, an absolute neutrophil count (ANC) <0.5 or <1 G/l with a predicted decrease to <0.5 G/l within 48 h of entry, no symptoms of septic shock, a MASCC score ≥21, no contraindication to the two tested antibiotics, and no mucositis preventing oral administration. In addition, they were to be willing to go home as soon as possible and to have signed the written consent form.
Patients were excluded from participation if they had received previous antibiotics within 4 days of entry, if they had severe clinical infection, serum transaminase levels more than five times the upper limit of normal, serum creatinine level >265 μmol/l, and were not willing to go home or had no relatives. Psychological status and social environment were evaluated by the physician before obtaining patient consent. Patients could not have been included in the same study within the previous 4 weeks or be hospitalized on occurrence of febrile neutropenia.
Study design and treatment strategy
This was a prospective, randomized, multicenter, controlled study. Randomization was centralized and was stratified according to the participating center.
The protocol was approved by an ethics committee and a written consent was obtained from all patients before enrolment.
Eligible patient evaluation included detailed medical history and complete physical examination, allowing accurate determination of the MASCC score.
Patients were evaluated for expected compliance, willingness to go home, home environment, and social status.
Biological examination consisted of a complete blood cell count and differential, determination of creatinine, serum electrolyte, and C reactive protein levels, and liver function tests. Blood cultures (one sample drawn from a peripheral vein and one from central venous access if available) were performed in duplicate (one sample for aerobes and one for anaerobes). Infecting pathogens were identified by genus and species, and susceptibility to antibiotics was determined.
Patients who fulfilled the entry criteria were randomly assigned to receive either moxifloxacin administered orally as 400 mg once daily or ceftriaxone 2 g administered intravenously as a single daily dose.
For all patients, the first antibiotic dose (oral or intravenous) was administered at the hospital before discharge.
The minimum duration of treatment was 4 days. Treatment was discontinued when patients reached an ANC >0.5 G/l and had no fever for 24 h.
Patients were to be discharged to home on the same day or within 24 h in case of logistical problems. An interval of 48 h between hospitalization and home discharge was allowed if febrile neutropenia occurred early in the weekend.
The monitoring of all included patients was performed by a coordination team with recording of temperature every 12 h and daily blood cell count until neutropenia recovery, daily phone calls, medical visits when necessary, and repeated blood cultures if needed.
In case of persistent fever after 72 h with no clinical sign of severity, the addition of a glycopeptide was recommended.
Blood transfusions in the ambulatory care unit were permitted and not considered a re-hospitalization.
Quality of life was evaluated at the end of the episode using the Quality of Life Questionnaire C30 (QLQ-C30) developed by the European Organization for Research and Treatment of Cancer [1].
Primary endpoint
The primary endpoint of the study was the global success of the at-home antibiotic therapy. The overall strategy (antibiotics and early hospital discharge) was considered a success not only when the effectiveness of the antibiotic therapy was achieved (as defined by the resolution of fever and of the possible clinical or microbiological manifestations of the infection) but also in the presence of the following criteria: early hospital discharge (within 24 or 48 h), no death from any cause, no sign or symptom of clinical deterioration requiring hospital readmission, no initial infection by a pathogen resistant in vitro to the antibiotics tested, no modification of initial anti-biotherapy, no relapse or new infection during antibiotic treatment, no toxic reaction to the antibiotic requiring discontinuation of treatment, and no re-hospitalization of the patient for any cause.
Evaluation of these criteria was performed at resolution of the episode.
Secondary endpoints
Secondary endpoints were the effectiveness of the antibiotic monotherapy (as evidenced by the lack of need for any additional antibiotics besides ceftriaxone or moxifloxacin), the toxicity of the two treatments, the frequency of re-admissions, and patient quality of life.
Statistical considerations
The study was initially designed as a non-inferiority trial. The sample size was calculated assuming a success rate of 80% in the standard intravenous arm, based on our previous experience, and that oral therapy would not be 10% worse. With a statistical power of 90% and a significance level of 5% in a one-sided test, the trial required 275 episodes of febrile neutropenia in each arm. Patients could be included twice, as long as an interval of more than 28 days was achieved between two inclusions; the episodes were then regarded as independent. Assuming a rate of 5% of non-evaluable patients, 580 episodes were needed.
Comparison between groups was carried out by a descriptive statistical analysis, and differences were tested using common tests.
Success rates were calculated for each group. The difference between the rates achieved with moxifloxacin and with ceftriaxone was calculated with a 95% confidence interval. If the upper limit of this confidence interval was lower than 10%, the moxifloxacine arm would be regarded as non-inferior to the ceftriaxone arm.
The analysis was made on an intention-to-treat basis and performed using the SAS software (version 8.2).
Results
Between September 2003 and December 2005, 90 patients representing 96 episodes of febrile neutropenia (47 in the ceftriaxone arm and 49 in the moxifloxacin arm) consented to participate in the study. Six patients were included twice.
This trial had to be closed prematurely because of recruitment problems. While six centers had been activated, only four included patients, and 91% of the patients were finally included by only one center.
In two cases, no data were available for follow-up. Of the 96 episodes of febrile neutropenia, 94 were, thus, evaluable for efficacy and toxicity.
Baseline characteristics
Baseline characteristics were well balanced between the two treatment arms (Table 1): 64.6% of patients were women, 30.2% of the patients had lymphoma, 34.4% had metastatic tumors, and 35.4% had non-metastatic solid tumors. Of the 67 patients with solid tumors, 28 (41.8%) had breast cancer (14 patients in each arm) and 22 (32.8%) had sarcoma (seven in the ceftriaxone arm and 15 in the moxifloxacin arm).
In 47 cases (49%), patients received only the first course of chemotherapy; nine of these (19.1%) received concomitant granulocyte-colony stimulating factor (GCSF). Of the remaining 49 patients undergoing the second course of chemotherapy or more, 17 received GCSF (34.7%).
At admission, 68 patients (70.8%) had a fever of unknown origin (FUO), 16 patients (16.7%) had microbiologically documented infection and 12 (12.5%) had clinically documented infection: eight cases of nasopharyngitis or bronchitis, one cellulitis, one ocular infection, one urinary infection, and one infection of the central venous access.
The overall mean MASCC score at admission was 24.31 (SD = 1.67); it was similar in the two treatment groups.
The median duration of treatments was 4 days (range, 1 to 10 days) in the moxifloxacin arm and 5 days (range, 1 to 10 days) in the ceftriaxone arm.
Efficacy
Primary outcomes
Table 2 lists the main outcome variables in each treatment group.
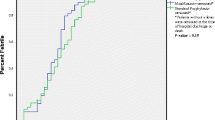
Success of the at-home antibiotic strategy was observed for 34 (73.9%) of the 46 patients included in the ceftriaxone arm and 38 (79.2%) of the 48 patients included in the moxifloxacin arm. The calculated risk difference between the moxifloxacin arm and the ceftriaxone arm was 5.3% (95% CI, 11.9 to 22.4%). The upper limit exceeded the 10% initially anticipated, and the non-inferiority of moxifloxacin was not demonstrated.
Secondary outcomes
No statistical difference was found for any component of the primary endpoint. As seen from Table 2, no toxic death was observed in the study population. Furthermore, no severe complication or significant morbidity were reported.
Seven patients (7.4%) were not discharged within 24 to 48 h, and 14 patients (14.9%) required re-hospitalization. These cases were regarded as failures of the strategy. Among the seven patients not discharged on time, five were in the moxifloxacin arm and two in the ceftriaxone arm; five had no other criteria of failure, but two patients in the moxifloxacin arm had a modification of the initial antibiotic regimen. Among the 14 patients who had to be re-hospitalized, nine had persistence of temperature, two chose to be re-hospitalized, one had a severe dental infection, one had positive initial blood cultures, and one had an allergic reaction to ceftriaxone.
Initial anti-biotherapy had to be modified in four cases (8.9%) in the ceftriaxone arm and in seven cases (15%) in the moxifloxacin arm. This modification was because of the persistence of temperature in six cases, mucositis requiring intravenous antibiotics in two cases, toxicity of initial antibiotics in two cases, and severe dental infection in one case.
In 82.6% of cases in the ceftriaxone arm and in 83.3% in the moxifloxacin arm, no antibiotic was added.
Quality-of-life data at 24 h after the end of the treatment were available for 42 patients (16 in the ceftriaxone arm and 26 in the moxifloxacin arm). In terms of global QOL, scores were not significantly different between the two arms (p = 0.78), with a mean global score of 46.3 in the ceftriaxone arm and 44.9 in the moxifloxacin arm.
Table 3 summarizes the initial microbiological data, the susceptibility of clinical isolates to the tested antibiotics, and patient clinical outcome. An initial microbiologically documented infection was reported in 16 cases (16.7%). One patient in the ceftriaxone arm had initial urinary tract infection because of Pseudomonas aeroginosa and resistant to ceftriaxone, justifying the immediate replacement of the antibiotic. In all other cases, antibiotic changes were decided after clinical failure. Six of the 16 (37.5%) documented infections failed to respond to the global strategy.
Safety
All patients had a favorable evolution after re-hospitalization and no death was observed. The toxicity profile was good in the two treatment groups. Three moderate gastrointestinal toxicities were reported in the moxifloxacin arm. In the ceftriaxone arm, five adverse events were reported: two cases of cutaneous allergy, one of moderate cutaneous modification, and two of moderate gastrointestinal toxicity. Treatment was stopped only in two cases in the ceftriaxone arm for cutaneous allergy. No statistical differences were found between the two arms for toxicity.
Discussion
Rapid hospitalization and broad-spectrum intravenous antibiotics have become the standard care for febrile neutropenia in cancer patients, resulting in a dramatic reduction of mortality and morbidity. However, when the expected duration of neutropenia is short, the vast majority of the episodes are benign in nature. Useful and convenient tools have been developed to select low-risk populations in whom other approaches could be used, such as early discharge from hospital and oral antibiotics.
This study included only low-risk patients defined by the MASCC score system, and early discharge and monotherapy with intravenous or oral antibiotics were successful in almost 80% of the cases. The MASCC score has been validated in at least three recent prospective studies with demonstration of the feasibility and safety of a less intensive approach in the defined low-risk population [5, 18, 28].
A meta-analysis including 15 trials comparing oral versus intravenous antibiotics has reported similar outcomes for the two strategies [29]. Four studies have been performed in the outpatient setting [20, 21, 23], and three have compared oral outpatient versus intravenous inpatient strategies [10, 12, 25]. The sample size of each separate study seems insufficient to provide certainty of equivalence. Similarly, the present study failed to demonstrate equivalence between oral and intravenous antibiotics because of insufficient recruitment. To be convincing, the demonstration of an equivalence between the two strategies would have necessitated at least 500 patients. However, consistent with published data, we observed no differences in terms of efficacy of the antibiotics, re-hospitalization rate, and toxicity. The patient selection was appropriate, as we observed no mortality and no significant morbidity.
Many reasons might explain this unexpected poor recruitment. We observed in our institution a significant decrease of febrile neutropenia episodes, probably caused by the routine use of GCSF. Furthermore, the monitoring of included patients required the participation of an ambulatory coordination team, which was difficult to organize in some centers. Early hospital discharge (within the first 24 h) was also a cause of non-inclusion. Many centers used this approach for their selected patients but without a careful evaluation.
If oral antibiotic therapy is an accepted alternative, there is no evidence in support of any specific regimen. Because of the preponderance of Gram-positive bacteria, most studies have tested quinolones frequently combined to another drug active against Gram-positive bacteria.
In the present study, we tested moxifloxacin, a new-generation quinolone that is more potent in vitro against Gram-positive bacteria than older quinolones and has a broad spectrum of activity against Gram-negative bacteria. A recent uncontrolled study has reported the outcome of 54 patients with febrile neutropenia receiving a single daily dose of moxifloxacin, with 91% overall success rate and no significant toxicity [5]. Organisms that we identified in this study from blood cultures were mostly coagulase-negative staphylococci; five of the eight isolates were susceptible to moxifloxacin in vitro. Similarly, the Gram-negative bacteria isolated from blood cultures and potentially dangerous for neutropenic patients were all susceptible to moxifloxacin. Monotherapy with oral moxifloxacin seems to be efficacious and safe in the setting of low-risk febrile neutropenia. The oral and once-daily administration of the drug is convenient, allows for outpatient treatment, and, thus, reduces the occurrence of nosocomial infections and the cost of patient monitoring.
Our study failed to enrol the number of patients that was originally planned, and our primary objective of demonstrating the non-inferiority of moxifloxacin could not be reached. However, even if definitive conclusions cannot be drawn, we believe that moxifloxacin is effective and safe for the outpatient management of low-risk neutropenic fever.
The MASCC score is now considered a useful tool to predict the outcome of febrile neutropenia and to identify candidates for oral antibiotics and immediate or early hospital discharge. Careful inpatient clinical and biological evaluation remains a standard procedure for the selection of patients for safe home care. Oral antibiotics such as new-generation fluoroquinolones, in conjunction with early hospital discharge, offer a feasible and cost-effective alternative to conventional management of low-risk neutropenic fever. However, other aspects, such as psychosocial conditions, evidence of good compliance, and evaluation of mucositis, remain to be addressed. The results of this exploratory study should provide the basis for a larger, well-powered, controlled study permitting to further evaluate the use of oral antibiotics and early discharge in a multicenter setting.
References
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376
Aktas Z, Gonullu N, Salcioglu M, Bal C, Ang O (2002) Moxifloxacin activity against clinical isolates compared with the activity of ciprofloxacin. Int J Antimicrob Agents 20:196–200
Balfour JA, Wiseman LR (1999) Moxifloxacin. Drugs 57:363–373
Biron P, Fuhrmann C, Cure H, Viens P, Lefebvre D, Thyss A, Viot M, Soler-Michel P, Rollin C, Gres JJ (1998) Cefepime versus imipenem-cilastatin as empirical monotherapy in 400 febrile patients with short duration neutropenia. CEMIC (Study Group of Infectious Diseases in Cancer). J Antimicrob Chemother 42:511–518
Chamilos G, Bamias A, Efstathiou E, Zorzou PM, Kastritis E, Kostis E, Papadimitriou C, Dimopoulos MA (2005) Outpatient treatment of low-risk neutropenic fever in cancer patients using oral moxifloxacin. Cancer 103:2629–2635
Chamorey E, Magne N, Foa C, Otto J, Largillier R, Viot M, Benard-Thiery I, Thyss A (2004) Ceftriaxone monotherapy for the treatment of febrile neutropenia in patients with solid tumors: a prospective study of 100 episodes. Med Sci Monit 10:I119–I125
Escalante CP, Rubenstein EB, Rolston KV (1997) Outpatient antibiotic therapy for febrile episodes in low-risk neutropenic patients with cancer. Cancer Invest 15:237–242
Escalante CP, Weiser MA, Manzullo E, Benjamin R, Rivera E, Lam T, Ho V, Valdres R, Lee EL, Badrina N, Fernandez S, DeJesus Y, Rolston K (2004) Outcomes of treatment pathways in outpatient treatment of low risk febrile neutropenic cancer patients. Support Care Cancer 12:657–662
Freifeld A, Marchigiani D, Walsh T, Chanock S, Lewis L, Hiemenz J, Hiemenz S, Hicks JE, Gill V, Steinberg SM, Pizzo PA (1999) A double-blind comparison of empirical oral and intravenous antibiotic therapy for low-risk febrile patients with neutropenia during cancer chemotherapy. N Engl J Med 341:305–311
Hidalgo M, Hornedo J, Lumbreras C, Trigo JM, Colomer R, Perea S, Gomez C, Ruiz A, Garcia-Carbonero R, Cortes-Funes H (1999) Outpatient therapy with oral ofloxacin for patients with low risk neutropenia and fever: a prospective, randomized clinical trial. Cancer 85:213–219
Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, Feld R, Pizzo PA, Rolston KV, Shenep JL, Young LS (2002) 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 34:730–751
Innes HE, Smith DB, O'Reilly SM, Clark PI, Kelly V, Marshall E (2003) Oral antibiotics with early hospital discharge compared with in-patient intravenous antibiotics for low-risk febrile neutropenia in patients with cancer: a prospective randomised controlled single centre study. Br J Cancer 89:43–49
Jun HX, Zhixiang S, Chun W, Reksodiputro AH, Ranuhardy D, Tamura K, Matsumoto T, Lee DG, Purushotaman SV, Lim V, Ahmed A, Hussain Y, Chua M, Ong A, Liu CY, Hsueh PR, Lin SF, Liu YC, Suwangool P, Jootar S, Picazo JJ (2005) Clinical guidelines for the management of cancer patients with neutropenia and unexplained fever. Int J Antimicrob Agents 26:S128–S132
Karthaus M, Egerer G, Kullmann KH, Ritter J, Jurgens H (1998) Ceftriaxone in the outpatient treatment of cancer patients with fever and neutropenia. Eur J Clin Microbiol Infect Dis 17:501–504
Kern WV, Cometta A, De Bock R, Langenaeken J, Paesmans M, Gaya H (1999) Oral versus intravenous empirical antimicrobial therapy for fever in patients with granulocytopenia who are receiving cancer chemotherapy. International Antimicrobial Therapy Cooperative Group of the European Organization for Research and Treatment of Cancer. N Engl J Med 341:312–318
Klaassen RJ, Goodman TR, Pham B, Doyle JJ (2000) “Low-risk” prediction rule for pediatric oncology patients presenting with fever and neutropenia. J Clin Oncol 18:1012–1019
Klastersky J, Paesmans M, Rubenstein EB, Boyer M, Elting L, Feld R, Gallagher J, Herrstedt J, Rapoport B, Rolston K, Talcott J (2000) The Multinational Association for Supportive Care in Cancer risk index: a multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol 18:3038–3051
Klastersky J, Paesmans M, Georgala A, Muanza F, Plehiers B, Dubreucq L, Lalami Y, Aoun M, Barette M (2006) Outpatient oral antibiotics for febrile neutropenic cancer patients using a score predictive for complications. J Clin Oncol 24:4129–4134
Malik IA, Khan WA, Karim M, Aziz Z, Khan MA (1995) Feasibility of outpatient management of fever in cancer patients with low-risk neutropenia: results of a prospective randomized trial. Am J Med 98:224–231
Mullen CA, Petropoulos D, Roberts WM, Rytting M, Zipf T, Chan KW, Culbert SJ, Danielson M, Jeha SS, Kuttesch JF, Rolston KV (1999) Outpatient treatment of fever and neutropenia for low risk pediatric cancer patients. Cancer 86:126–134
Petrilli AS, Dantas LS, Campos MC, Tanaka C, Ginani VC, Seber A (2000) Oral ciprofloxacin vs. intravenous ceftriaxone administered in an outpatient setting for fever and neutropenia in low-risk pediatric oncology patients: randomized prospective trial. Med Pediatr Oncol 34:87–91
Rolston KV (2004) The Infectious Diseases Society of America 2002 guidelines for the use of antimicrobial agents in patients with cancer and neutropenia: salient features and comments. Clin Infect Dis 39:S44–S48
Rolston K, Rubenstein E, Elting L, Escalante E, Manzullo E, Bodey GP (1995) Ambulatory management of febrile episodes in low-risk neutropenic patients. In: Programs and abstracts of the 35th interscience conference on antimicrobial agents and chemotherapy, San Francisco. Abstract LM81. American Society for Microbiology, Washington, DC, USA
Rubenstein EB, Rolston KV (1995) Outpatient treatment of febrile neutropenic patients with cancer. Eur J Cancer 31A:2–4
Samonis G, Anaissie E, Kalbakis K, Georgoulias V (1997) Therapy for low risk cancer patients with fever and neutropenia:results of a prospective randomized trial with cost analysis. Programs and abstracts of the 37th interscience conference on antimicrobial agents and chemotherapy, Toronto, Canada. Abstract LM51. American Society for Microbiology, Washington, DC, USA
Sebban C, Fuhrmann C, Perol D, Devaux Y, Ghesquiere H, Galand-Desme S, Leveque N, Claude L, Biron P (2006) Prise en charge à domicile des neutropénies fébriles courtes après chimiothérapie: résultats et leçons d’une étude pilote menée sur deux ans dans un centre de lutte contre le cancer. Oncologie 8:HS29–HS33
Talcott JA, Siegel RD, Finberg R, Goldman L (1992) Risk assessment in cancer patients with fever and neutropenia: a prospective, two-center validation of a prediction rule. J Clin Oncol 10:316–322
Uys A, Rapoport BL, Anderson R (2004) Febrile neutropenia: a prospective study to validate the Multinational Association of Supportive Care of Cancer (MASCC) risk-index score. Support Care Cancer 12:555–560
Vidal L, Paul M, Ben Dor I, Soares-Weiser K, Leibovici L (2004) Oral versus intravenous antibiotic treatment for febrile neutropenia in cancer patients: a systematic review and meta-analysis of randomized trials. J Antimicrob Chemother 54:29–37
Viscoli C, Bruzzi P, Castagnola E, Boni L, Calandra T, Gaya H, Meunier F, Feld R, Zinner S, Klastersky J, Glauser M (1994) Factors associated with bacteraemia in febrile, granulocytopenic cancer patients. The International Antimicrobial Therapy Cooperative Group (IATCG) of the European Organization for Research and Treatment of Cancer (EORTC). Eur J Cancer 30:430–437
Acknowledgement
This study was supported by a grant from Bayer Pharma France. We thank Dr. Pierre Arvise for the logistical and technical assistance; Giovanna Gonnon, Séverine Guillemaut, and Mathieu Cassin for the help in the study design, study monitoring, and data analysis; Carlos Poncelas for the help in the management of outpatient treatment; and Marie-Dominique Reynaud for the editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sebban, C., Dussart, S., Fuhrmann, C. et al. Oral moxifloxacin or intravenous ceftriaxone for the treatment of low-risk neutropenic fever in cancer patients suitable for early hospital discharge. Support Care Cancer 16, 1017–1023 (2008). https://doi.org/10.1007/s00520-007-0383-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-007-0383-z