Abstract
Background
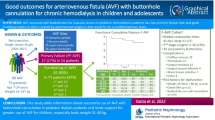
This study aimed to describe the efficiency and longevity of arteriovenous fistula (AVF) for hemodialysis (HD) in children weighing ≤20 kg.
Methods
We collected data of all AVFs created using microsurgery techniques between 1988 and 2015. Success was considered as the ability to use the AVF for HD. Primary and secondary patency rates were measured.
Results
Forty-eight AVFs (35 forearm, 13 upper arm) were created in 41 children with a median weight of 13.5 kg (range 5.5–20). The need for a second AVF was significantly higher in younger and thinner children at the time of AVF creation (p = 0.046 and p = 0.019, respectively). Successful use for HD occurred in 42 AVFs (87.5%), while six (12.5%) resulted in failure for early thrombosis or nonmaturation. Median time to first cannulation was 18.8 weeks (range 2–166.3). Primary and secondary patency rates at 1, 5, and 10-year follow-ups were 54.2%, 29.2%, and 13.7%; and 85.4%, 57.7%, and 33%, respectively. Almost one third of thromboses after first AVF cannulation were observed at kidney transplantation (KT) perioperatively. At the end of the follow-up (median duration 5.07 years, range 0–17.95), one patient was still on HD via AVF, two died of unrelated reason, and 38 were transplanted—one of whom returned to HD with a new AVF.
Conclusions
AVF using microsurgery techniques is feasible in young children, showing an early failure rate of 12.5%. Time to first cannulation may be rather long, but secondary patency is excellent. Thrombosis rate is high during KT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
End-stage renal disease (ESRD) is rare in young children. While pre-emptive kidney transplantation (KT) is the optimal therapy, its application is not always feasible due to either surgical difficulties or lack of suitable kidney donor [1]. Clinical practice guidelines recommend peritoneal dialysis (PD) as the first option for renal replacement therapy (RRT) [2, 3]. However, when PD is inefficient or technically impossible, hemodialysis (HD) is an alternative option [4]. Arteriovenous fistula (AVF) may be preferred to central venous catheter (CVC) due to lower associated infection rate and better preservation of central vein patency [2, 5,6,7,8]. Nevertheless, feasibility of AVF in children weighing ≤20 kg is a surgical challenge, while its efficiency, longevity, and associated morbidity are not widely assessed. Few studies have reported the high rates of immediate success and long-term patency as benefits of microsurgery techniques and preventive hemostasis for AVF creation in children [9,10,11,12,13,14]. The aim of this study was to present our experience with microsurgical AVF created in children weighing ≤20 kg.
Patients and methods
This retrospective study comprised 48 AVFs for HD created in 41 children weighing ≤20 kg from January 1998 to December 2015 at the Robert Debré Hospital, in Paris. As with adults, preoperative vessel mapping was initially performed with venography (n = 16), but it may be intrusive and technically demanding, particularly in young children. Color duplex imaging (CDI) became secondarily the de facto standard for vessel mapping and search for indirect signs of central vein stenosis if any history of CVC.
No minimal diameter of cephalic and basilic veins was required, but assessment of continuity, absence of stenosis, and compliance of the main superficial veins were considered mandatory. Forearm radiocephalic AVF in the nondominant wrist was the preferred localization. All AVFs were created using microsurgery techniques and preventive hemostasis by specialized microvascular surgeons. Microsurgery includes surgical microscope, microinstruments, microclamps, and microsutures. Preventive hemostasis was used routinely with Esmarch bandage and pneumatic tourniquet [15]. Anticoagulation prophylaxis was used routinely with low-molecular-weight heparin for 20 days after surgery [16]. Anti-Xa level (target range 0.5–1 U/ml) was systematically monitored to adjust heparin dose. Pre- and postoperative anti-vitamin-K anticoagulation therapy was used in 13 selected cases when thrombotic risk was substantial. A second-stage lipectomy was necessary in radiocephalic AVFs when the cephalic vein was deep under thick subcutaneous tissues of the forearm (n = 8) and in all brachiobasilic AVFs (n = 9) [17, 18]. Maturation of AVF was evaluated by palpation of the vein, while its depth and volume flow rate were assessed using CDI. It was confirmed by ease of the first cannulation and efficient dialysis. However, as time to first cannulation depends on the need for HD, time to maturation was determined as the time interval between AVF creation and first cannulation in patients already on RRT with PD or HD. All AVFs were cannulated with 17-gauge needles using the rope ladder technique after application of a local anesthetic cream. Follow-up of AVF during HD included monitoring of venous and arterial pressure, and blood flow at each HD session, weekly clinical AVF examination, and monthly assessment of dialysis adequacy. AVF CDI was performed every 6 months until the day of KT and then every 12–24 months. Well-trained nursing staff was responsible for educating parents about the best care for AVF and the early recognition of abnormal signs or symptoms. Of note, we collaborated with specialized pediatric interventional radiologists and anesthesiologists for percutaneous transluminal angioplasty (PTA) and thromboaspiration.
Early failure characterized AVF, which were abandoned (i.e., never for HD) because of occlusion or absent maturation. Success was indicative for AVF, which were used for HD. Primary maturation was defined as spontaneous AVF maturation without radiological or surgical reintervention. Primary patency was defined as the time interval from AVF creation until any intervention designed to maintain or re-establish patency. Secondary patency was defined as the time interval from AVF creation until failure (including intervening manipulations designed to re-establish functionality) [19]. Early and late complications were defined as those observed before and after first AVF cannulation.
All statistical evaluations were performed using SPSS statistics software. The Kaplan–Meier method was used to calculate patency rates. The box-and-whisker plot histogram illustrates the variation (median, quartiles, minimum, and maximum values) of selected nonparametric data. The log-rank and Mann–Whitney tests were used to compare patency curves and distribution of selected parameters in independent groups, respectively [20]. A p value <0.05 was considered statistically significant.
Results
Patient characteristics
Forty-one children (23 boys, 18 girls) were evaluated. The observed primary renal diseases are reported in Table 1. Twenty-one children (51%) had AVF creation before RRT and 20 (49%) while on RRT: 16 on HD via CVC and four on PD (3 graft failures included). In total, HD via CVC was observed in 21 (51.2%): 16 before AVF maturation, two long before AVF creation (transitory HD via CVC discontinued after improvement of kidney function), and in three after AVF failure. Median follow-up was 5.07 years, with variations from 0 to 17.95 years. “0” (zero) indicates one patient who was not followed up because of immediate thrombosis of AVF and continuation of HD via CVC without creation of a new AVF. At the end of the overall follow-up, one patient was still on HD via AVF, two died of unrelated reason, and 38 were transplanted—one of whom recommenced HD with a newly created AVF after graft rejection.
AVF characteristics
Forty-eight AVFs were placed in 41 patients: 38 (79%) in the left upper limb and ten (21%) in the right. Thirty-five (72.9%) were in the forearm and 13 (27.1%) in the upper arm; 33 (68.8%) were radiocephalic, two (4.2%) ulnobasilic, ten (20.8%) brachiobasilic, and three (6.2%) brachiocephalic.
Thirty-four (83%) patients underwent a single AVF placement, whereas a second was required in seven (17%). Reasons for failure of first AVF were four perioperative thromboses, one absent maturation, one thrombosis secondary to a juxta-anastomosis stenosis, and one unsuccessful high-flow reduction. The need for a second AVF was significantly higher in younger and lighter children at AVF creation (p = 0.046 and p = 0.019, respectively) (Table 2). Median age at AVF creation was 3.2 years (range 0.5–8.1); <2 years in eight (16.7%), ≥ 2 years and <4 years in 25 (52%), ≥ 4 years and <6 years in nine (18.8%), and ≥6 years in six (12.5%). Median weight at AVF creation was 13.5 kg (range 5.5–20): <10 kg in eight (16.7%), ≥10 kg and <15 kg in 22 (45.8%), and ≥15 kg in 18 (37.5%). Most patients weighed between 10 and 15 kg.
At the end of follow-up, 28 (58.3%) AVFs were complicated and eventually failed, six (12.5%), were ligated after 1 year of a well-functioning KT for fear of future cardiac issues, two (4.2%) were abandoned because of patient death unrelated to treatment, and 12 (25%) were patent.
Early AVF failure
Success occurred in 42 (87.5%) AVFs, which were used for HD. Early failure was observed in six (12.5%) (4 radiocephalic, 1 brachiobasilic, and 1 brachiocephalic). Causes of early failure were postoperative AVF thromboses in four and absent maturation in two(1 after unsuccessful cephalic vein superficialization). Two postoperative AVF thromboses were observed in the same patient. Among the five patients with early failure, four underwent a new AVF creation, and one was converted to HD via CVC.
Maturation and early complications
Primary maturation was observed in 29 (60.4%) AVFs and early complications in the remaining 19; six were abandoned; 13 achieved secondary maturation after surgical or radiological reintervention (median = 1 per AVF, range 1–2). In total, 16 interventions were performed: four percutaneous transluminal angioplasties, six surgical anastomosis revisions, and six thrombectomies (5 surgically and 1 percutaneously).
Median time to first cannulation was 18.8 weeks (range 2–166.3) (Fig. 1) and to maturation in patients already on RRT 17.2 weeks (range 2–68.7). Localization of AVF did not significantly influence time to maturation (p = 0.139), which was significantly shorter in patients ≥3 years (approximate median age) but did not significantly differ between patients weighing ≥13 or <13 kg (approximate median weight) (p = 0.01 and p = 0.307, respectively) (Table 3).
Patency rates
Primary patency rates [± standard error (SE)] at 1 and 2 years of follow-up were 54.2% (± 7%) and 39.6% (± 7%). Secondary patency rates (± SE) at 1, 2, 3, 4, 5, and 10-year follow-up were 85.4% (± 5%), 83.3% (± 5%), 70.5% (± 7%), 64.1% (± 7%), 57.7% (± 7%), and 33% (± 8%), respectively (Fig. 2).
Primary and secondary patency rates were compared between patients aged ≥3 and <3 years (approximate median age) and ≥13 and <13 kg (approximate median weight). Primary patency rate was not influenced by patient age and weight at AVF creation (p = 0.116 and p = 0.233, respectively). However, secondary patency rate was significantly higher in patients aged ≥3 years or weighing ≥13 kg at AVF creation (p = 0.006 and p = 0.003, respectively) (Fig. 3). Median number of open surgeries or percutaneous reinterventions per AVF after initial success was 0.27 (range 0–2.4) per year. Median duration of HD via AVF was 0.75 years (range 0.05–5.34).
Late complications
After first AVF cannulation, 12 stenoses and 18 thromboses were observed; their evolution and management are described in detail on Table 4. Almost one third of thromboses were observed during KT. Among the stenoses, only one was complicated by cephalic vein aneurysmal degeneration after KT, resulting to AVF ligation.
Evolution of AVF flow rates is illustrated in Fig. 4 showing a progressive increase, which is remarkable after a 3-year-follow-up. High-flow surgical reduction was required in 12 AVFs (4 during HD and 8 after KT), including five in the upper arm (38%) and seven in the forearm (20%). In the upper arm, one AVF causing high-output cardiac failure was ligated; surgical reduction was attempted in four but was successful only in one [21]. AVF ligation in the forearm was performed in three cases, and juxta-anastomosis ligation of the proximal radial artery resulted in 50% flow reduction in three of four AVFs [22].
Coagulation disorders
Coagulation disorders were observed in four patients: homozygous MTHFR mutation in three and Factor V Leiden mutation in one. Primary renal disease associated with a higher thrombotic risk was present in 14 patients: nephrotic syndrome (congenital and idiopathic infantile) in 11, atypical hemolytic uremic syndrome in two, and vasculitis in one. As mentioned, most of these children were under anti-vitamin-K anticoagulation therapy (13). Primary and secondary patency was compared between children with nephrotic syndrome (congenital or infantile idiopathic) and those with congenital abnormalities of kidney and urinary tract (CAKUT). Primary and secondary patency was not statistically different between groups (p = 0.071 and p = 0.281, respectively; data not shown).
Discussion
We present results of 48 AVFs created for HD in children weighing ≤20 kg. In recent published studies evaluating the efficacy of HD in young children, few AVF creations have been reported [23,24,25,26,27,28]. CVC-associated infections (ranging from 0.6/1000 to 7.7/1000 CVC days) and malfunctions were the main complications observed, both leading to a CVC exchange rate of 0.32–3 per patient-years [23,24,25,26,27,28]. History of long-term and repetitive CVC placements increases the risk of central veins stenosis. In our study, CVC was not inserted in 48.8% of patients. No AVF infection was observed, and second AVF placement was required in only 17% of patients. Early failure was observed in approximately one of ten procedures. Additionally, more than 60% of AVFs achieved primary maturation, and more than eight of ten AVFs did not develop secondary patency failure at 1-year follow-up. These data encourage the concept of changing HD strategy in younger children toward a long-lasting, infection-free AVF.
The Kidney Disease Outcome Quality (KDOQI) 2006 recommendations and the International Pediatric Fistula First Initiative in 2004 emphasized the need for considering AVF as the first choice for pediatric HD [29]. Since then, there has been an increase in published articles demonstrating the feasibility of AVF in the pediatric population, proving that patency rates are comparable with those of adults [30,31,32,33,34,35,36,37,38]. They reported early AVF failures in older and heavier children ranging from 10 to 33.3%. The first-year primary and secondary patency rates varied from 50 to 100% and from 73 to 100%, respectively [30,31,32,33,34,35,36,37,38,39]. In our study, early failure and patency rates were similar to these reports, indicating that AVF is suitable in younger and smaller children. Nevertheless, in our cohort, AVF longevity was, as expected, longer in older (≥3 years) and heavier (≥13 kg) children (Fig. 2).
Surgical expertise plays an important role in the success of an AVF creation. Since Bourquelot et al. in 1978, several surgeons have claimed that microsurgery techniques in AVF creation can reduce early failure rate, diminish maturation time, and achieve longer access survival rates [9,10,11,12,13]. Moreover, this technique benefits the successful creation of distal forearm AVF in small children, which is the best location. However, this technique is not yet adopted by all pediatric HD centers mainly because it requires microsurgical training. In our study, all AVFs were created by the same vascular surgeon using microsurgery techniques and the forearm was the first-choice location. The observed early failure and nonmaturation rates were among the lowest published results in the pediatric population, proving that microsurgery should be considered as the technique of choice in AVF placement [40]. Microsurgery with microscope training seminars on rats are valuable for initial formation of young surgeons. Participation in microsurgical AVF creation in adult patients is the next stage. Early detection and prompt treatment of AVF stenosis is highly important to avoid possible secondary thrombosis. Immediate treatment of the latter might minimize the risk of AVF failure [33, 38, 41]. We therefore recommend centralizing AVFs in children with a pediatric AVF multidisciplinary team comprising well-trained nurses, pediatric nephrologist, specialized angiologist, interventional radiologist, and experienced microsurgeon. Such a team would ensure creation of long-lasting distal AVF and early treatment of complications.
In our study, the number of interventions performed after initially successful AVF creation per year were similar to those reported in the literature concerning older patients [30,31,32,33,34,35,36,37,38]. Stenosis and thrombosis were the most frequent late complications. It is remarkable that 30% of late thromboses occurred at perioperative KT, implying that attention should be paid to maintaining the patient in a good volemic state. Moreover, it is worth noting that AVF flow rate was remarkably increased after 3 years of follow-up. Surgical reduction of high-flow proximal AVF remains a challenge, especially in younger children [21, 22].
Despite the proven superiority of AVF in terms of morbidity and life quality when compared with CVC, the latter remains the most common choice for pediatric HD worldwide [42]. The pediatric KT priority allocation policy, which dramatically decreased the waiting time to KT in the pediatric population, is one reason CVC is the preferred vascular access for HD [43, 44]. Nevertheless, AVF can be used even after KT, as it is safe, easily accessible, and durable. This is highly beneficial for younger children with fragile vascular capital. Young transplanted children are more vulnerable to infections or serious dehydration, imperiling kidney function; these conditions necessitate repeated vein cannulation [45]. Furthermore, as children are transplanted at a young age, they are suceptible to higher risk for acute allograft rejection or even loss [46]. Therefore, maintaining their central and superficial vein capital is primordial.
Delayed first AVF cannulation results in some centers preferring CVC as the first vascular access choice for HD. However, the most common primary renal diseases, described in our study, are the CAKUT and congenital nephrotic syndromes, which evolve slowly toward ESRD. In our study, more than half the patients underwent a preemptive arteriovenous AVF procedure. Therefore, we recommend AVF as the optimal option in younger children on HD, even in case of prominent KT.
Time to first AVF cannulation has been reported from 6 to 12 weeks in children [47]. In our study, median maturation time was 17.2 weeks and was not influenced by AVF localization and was shorter in patients aged ≥3 years (median 8.3 weeks). Hence, we propose that AVF, preferably placed in the forearm, should be inserted 4– 5 months before expected manifestation of ESRD in younger children, although 2 months is probably enough for those aged ≥ 3 years. As shown, one reintervention is probably essential to achieve maturation.
In conclusion, AVF is feasible in young children, showing an early failure rate at 12.5%. Time to maturation is longer than in older children, but primary and secondary patency rates are excellent. Therefore, we recommend that pediatric HD centers establish a strategy supporting AVF creation in young children when PD is contraindicated and pre-emptive KT is not feasible.
Abbreviations
- AVF:
-
Arteriovenous fistula
- CAKUT:
-
Congenital abnormalities of kidney and urinary tract
- CDI:
-
Color duplex imaging
- CVC:
-
Central venous catheter
- ESRD:
-
End-stage renal disease
- HD:
-
Hemodialysis
- KT:
-
Kidney transplantation
- PD:
-
Peritoneal dialysis
- RRT:
-
Renal replacement therapy
- PTA:
-
Percutaneous transluminal angioplasty
References
Amaral S, Sayed BA, Kutner N, Patzer RE (2016) Preemptive kidney transplantation is associated with survival benefits among pediatric patients with end-stage renal disease. Kidney Int 90:1100–1108
(2006) Clinical practice recommendation 8: vascular access in pediatric patients. Am J Kidney Dis 48 Suppl 1:S274–276. https://doi.org/10.1053/j.ajkd.2006.04.049
Zurowska AM, Fischbach M, Watson AR, Edefonti A, Stefanidis CJ (2013) Clinical practice recommendations for the care of infants with stage 5 chronic kidney disease (CKD5). Pediatr Nephrol 28:1739–1748
Feinstein S, Rinat C, Becker-Cohen R, Ben-Shalom E, Schwartz SB, Frishberg Y (2008) The outcome of chronic dialysis in infants and toddlers--advantages and drawbacks of haemodialysis. Pediatr Nephrol 23:1336–1345
Ma A, Shroff R, Hothi D, Lopez MM, Veligratli F, Calder F, Rees L (2013) A comparison of arteriovenous fistulas and central venous lines for long-term chronic haemodialysis. Pediatr Nephrol 28:321–326
Zaritsky JJ, Salusky IB, Gales B, Ramos G, Atkinson J, Allsteadt A, Brandt ML, Goldstein SL (2008) Vascular access complications in long-term pediatric hemodialysis patients. Pediatr Nephrol 23:2061–2065
Baracco R, Mattoo T, Jain A, Kapur G, Valentini RP (2014) Reducing central venous catheters in chronic hemodialysis--a commitment to arteriovenous fistula creation in children. Pediatr Nephrol 29:2013–2020
Mak RH, Warady BA (2013) Dialysis: vascular access in children--arteriovenous fistula or CVC? Nat Rev Nephrol 9:9–11
Bourquelot P, Cussenot O, Corbi P, Pillion G, Gagnadoux MF, Bensman A, Loirat C, Broyer M (1990) Microsurgical creation and follow-up of arteriovenous fistulae for chronic haemodialysis in children. Pediatr Nephrol 4:156–159
Gallieni M, Saxena R, Davidson I (2009) Dialysis access in europe and north america: are we on the same path? Semin Intervent Radiol 26:96–105
Yazbeck S, O'Regan S (1984) Microsurgery for Brescia-Cimino fistula construction in pediatric patients. Nephron 38:209–212
Bourquelot P, Wolfeler L, Lamy L (1981) Microsurgery for haemodialysis distal arteriovenous fistulae in children weighing less than 10kg. Proc Eur Dial Transplant Assoc 18:537–541
Sanabia J, Polo JR, Morales MD, Canals MJ, Polo J, Serantes A (1993) Microsurgery in gaining paediatric vascular access for haemodialysis. Microsurgery 14:276–279
Gagnadoux MF, Pascal B, Bronstein M, Bourquelot P, Degoulet P, Broyer M (1978) Arterio-venous fistula in small children. Proc Eur Dial Transplant Assoc 15:573–574
Bourquelot PD (1993) Preventive haemostasis with an inflatable tourniquet for microsurgical distal arteriovenous fistulas for haemodialysis. Microsurgery 14:462–463
Sharathkumar A, Hirschl R, Pipe S, Crandell C, Adams B, Lin JJ (2007) Primary thrombophylaxis with heparins for arteriovenous fistula failure in pediatric patients. J Vasc Access 8:235–244
Bourquelot P, Tawakol JB, Gaudric J, Natario A, Franco G, Turmel-Rodrigues L, Van Laere O, Raynaud A (2009) Lipectomy as a new approach to secondary procedure superficialization of direct autogenous forearm radial-cephalic arteriovenous accesses for hemodialysis. J Vasc Surg 50:369–374 374.e361
Bourquelot P, Karam L, Robert-Ebadi H, Pirozzi N (2015) Transposition, elevation, lipectomy and V-wing for easy needling. J Vasc Access 16(Suppl 9):S108–S113
Sidawy AN, Gray R, Besarab A, Henry M, Ascher E, Silva M Jr, Miller A, Scher L, Trerotola S, Gregory RT, Rutherford RB, Kent KC (2002) Recommended standards for reports dealing with arteriovenous hemodialysis accesses. J Vasc Surg 35:603–610
Rutherford RB, Baker JD, Ernst C, Johnston KW, Porter JM, Ahn S, Jones DN (1997) Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg 26:517–538
Bourquelot P, Gaudric J, Turmel-Rodrigues L, Franco G, Van Laere O, Raynaud A (2010) Proximal radial artery ligation (PRAL) for reduction of flow in autogenous radial cephalic accesses for haemodialysis. Eur J Vasc Endovasc Surg 40:94–99
Bourquelot P, Gaudric J, Turmel-Rodrigues L, Franco G, Van Laere O, Raynaud A (2009) Transposition of radial artery for reduction of excessive high-flow in autogenous arm accesses for hemodialysis. J Vasc Surg 49:424-428, 428.e421
Kovalski Y, Cleper R, Krause I, Davidovits M (2007) Hemodialysis in children weighing less than 15 kg: a single-center experience. Pediatr Nephrol 22:2105–2110
Novljan G, Rus RR, Premru V, Ponikvar R, Battelino N (2016) Chronic Hemodialysis in small children. Ther Apher Dial 20:302–307
Quinlan C, Bates M, Sheils A, Dolan N, Riordan M, Awan A (2013) Chronic hemodialysis in children weighing less than 10 kg. Pediatr Nephrol 28:803–809
Paglialonga F, Consolo S, Pecoraro C, Vidal E, Gianoglio B, Puteo F, Picca S, Saravo MT, Edefonti A, Verrina E (2016) Chronic haemodialysis in small children: a retrospective study of the Italian Pediatric dialysis registry. Pediatr Nephrol 31:833–841
Shroff R, Wright E, Ledermann S, Hutchinson C, Rees L (2003) Chronic hemodialysis in infants and children under 2 years of age. Pediatr Nephrol 18:378–383
Al-Hermi BE, Al-Saran K, Secker D, Geary DF (1999) Hemodialysis for end-stage renal disease in children weighing less than 10 kg. Pediatr Nephrol 13:401–403
Chand DH, Valentini RP (2008) International pediatric fistula first initiative: a call to action. Am J Kidney Dis 51:1016–1024
Sheth RD, Brandt ML, Brewer ED, Nuchtern JG, Kale AS, Goldstein SL (2002) Permanent hemodialysis vascular access survival in children and adolescents with end-stage renal disease. Kidney Int 62:1864–1869
Souza RA, Oliveira EA, Silva JM, Lima EM (2011) Hemodialysis vascular access in children and adolescents: a ten-year retrospective cohort study. J Bras Nefrol 33:422–430
Wartman SM, Rosen D, Woo K, Gradman WS, Weaver FA, Rowe V (2014) Outcomes with arteriovenous fistulas in a pediatric population. J Vasc Surg 60:170–174
Shroff R, Sterenborg RB, Kuchta A, Arnold A, Thomas N, Stronach L, Padayachee S, Calder F (2016) A dedicated vascular access clinic for children on haemodialysis: two years' experience. Pediatr Nephrol 31:2337–2344
Bagolan P, Spagnoli A, Ciprandi G, Picca S, Leozappa G, Nahom A, Trucchi A, Rizzoni G, Fabbrini G (1998) A ten-year experience of Brescia-Cimino arteriovenous fistula in children: technical evolution and refinements. J Vasc Surg 27:640–644
Briones L, Diaz Moreno A, Sierre S, Lopez L, Lipsich J, Adragna M (2010) Permanent vascular access survival in children on long-term chronic hemodialysis. Pediatr Nephrol 25:1731–1738
Kim SM, Min SK, Ahn S, Min SI, Ha J (2016) Outcomes of Arteriovenous fistula for Hemodialysis in Pediatric and adolescent patients. Vasc Specialist Int 32:113–118
Ramage IJ, Bailie A, Tyerman KS, McColl JH, Pollard SG, Fitzpatrick MM (2005) Vascular access survival in children and young adults receiving long-term hemodialysis. Am J Kidney Dis 45:708–714
Chand DH, Bednarz D, Eagleton M, Krajewski L (2009) A vascular access team can increase AV fistula creation in pediatric ESRD patients: a single center experience. Semin Dial 22:679–683
Gradman WS, Lerner G, Mentser M, Rodriguez H, Kamil ES (2005) Experience with autogenous arteriovenous access for hemodialysis in children and adolescents. Ann Vasc Surg 19:609–612
Bourquelot P (2006) Vascular access in children:the importance of microsurgery for creation of autologous arteriovenous fistulae. Eur J Vasc Endovasc Surg 32:696–700
Chand DH, Geary D, Patel H, Greenbaum LA, Nailescu C, Brier ME, Valentini RP (2015) Barriers, biases, and beliefs about arteriovenous fistula placement in children: a survey of the international Pediatric fistula first initiative (IPFFI) within the Midwest Pediatric nephrology consortium (MWPNC). Hemodial Int 19:100–107
Hayes WN, Watson AR, Callaghan N, Wright E, Stefanidis CJ (2012) Vascular access: choice and complications in European paediatric haemodialysis units. Pediatr Nephrol 27:999–1004
Harambat J, van Stralen KJ, Schaefer F, Grenda R, Jankauskiene A, Kostic M, Macher MA, Maxwell H, Puretic Z, Raes A, Rubik J, Sorensen SS, Toots U, Topaloglu R, Tonshoff B, Verrina E, Jager KJ (2013) Disparities in policies, practices and rates of pediatric kidney transplantation in Europe. Am J Transplant 13:2066–2074
Merouani A, Lallier M, Paquet J, Gagnon J, Lapeyraque AL (2014) Vascular access for chronic hemodialysis in children: arteriovenous fistula or central venous catheter? Pediatr Nephrol 29:2395–2401
Jordan CL, Taber DJ, Kyle MO, Connelly J, Pilch NW, Fleming J, Meadows HB, Bratton CF, Nadig SN, McGillicuddy JW, Chavin KD, Baliga PK, Shatat IF, Twombley K (2013) Incidence, risk factors, and outcomes of opportunistic infections in pediatric renal transplant recipients. Pediatr Transplant 20:44–48
Rocha A, Rocha L, Malheiro J, Azevedo P, Tavares T, Faria MS, Mota C, Dias L, Henriques AC (2014) Predictive factors of graft-censored failure in pediatric kidney transplantation. Transplant Proc 46:1723–1726
Almasi-Sperling V, Galiano M, Lang W, Rother U, Rascher W, Regus S (2016) Timing of first arteriovenous fistula cannulation in children on hemodialysis. Pediatr Nephrol 31:1647–1657
Acknowledgements
Special thanks from Pierre Bourquelot to Pr. Chantal Loirat for her constant support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the local ethics committee. Patient formal consent was not required.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Karava, V., Jehanno, P., Kwon, T. et al. Autologous arteriovenous fistulas for hemodialysis using microsurgery techniques in children weighing less than 20 kg. Pediatr Nephrol 33, 855–862 (2018). https://doi.org/10.1007/s00467-017-3854-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3854-6