Abstract
Current data demonstrate pediatric patients who remain on hemodialysis (HD) therapy are more likely to be dialyzed via central venous catheters (CVCs) than arteriovenous grafts (AVGs) and fistulae (AVFs). We retrospectively compared complications and health-related quality of life (HRQOL) associated with different vascular access types at two large centers over a 1-year period. Patients included in the study were younger than 25 years of age, weighed >20 kg, and had received HD for at least 3 months. Thirty CVC patients and 21 AVG/AVF patients received a total of 2,393 and 3,506 HD treatments, respectively. The infectious complication rate was higher for CVC patients, who were hospitalized 3.7 days for each 100 HD treatments versus 0.2 days for AVG/AVF patients (p < 0.01). CVC patients also had a much higher rate of access revision, needing 2.7 hospital days every 100 HD treatments compared with 0.2 days for AVG/AVF patients (p < 0.01). HRQOL scores did not differ between groups. Thus, despite similar HRQOL, CVCs were associated with more complications and greater morbidity when compared with AVG/AVFs. These findings further emphasize the need to use AVG/AVFs as primary HD access for pediatric patients expected to receive a long course of maintenance HD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
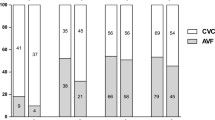
The increased recognition of central venous catheter (CVC)-associated morbidity and mortality in adult patients receiving maintenance hemodialysis has led to an emphasis on permanent vascular access establishment, known as the Fistula First Initiative [1]. Recently, a similar emphasis occurred in the pediatric hemodialysis population with the first published pediatric Kidney Disease Outcome Quality Initiative (K-DOQI) vascular access guidelines, which recommend permanent vascular access placement in children >20 kg who are expected to require hemodialysis for >1 year [2]. Despite this recommendation, CVCs continue to serve as the most prevalent vascular access in the pediatric population, with close to 80% of pediatric maintenance hemodialysis patients using CVCs as vascular access [3]. Permanent access prevalence rates in the form of an AVF or AVG are only 5%, 13.5%, and 21.5% at 1, 2, and 3 years, respectively [3]. Prevalence rates are somewhat better in adolescent patients, although data from the Center for Medicare & Medicaid Clinical Performance Measures Project demonstrate 56% of adolescents receive hemodialysis via CVCs for at least 2 consecutive years [4].
The potential rationale for increased relative CVC prevalence includes perceived difficulties in creating and using permanent access in children and shortened time spent on dialysis therapy as a bridge to transplantation [5]. An additional factor that may influence selection of CVCs over permanent access is the reluctance of children to endure the pain associated with access cannulation, which in turn may negatively influence the patients overall health related quality of life (HRQOL). A recent study in adult patients, however, revealed patients dialyzed persistently via an AVF actually reported better HRQOL [6]. Although there is consistent evidence showing hemodialysis CVC use is associated with greater morbidity and mortality risk in the adult population [7, 8], there is limited information with respect to the complication rate between access types in pediatric hemodialysis patients [9–12]. Moreover, the implications of access-related complications on HRQOL in children have not been described.
The aims of this study were to (1) compare complications associated with different vascular access types and (2) compare-patient reported vascular-access-associated HRQOL in children receiving maintenance hemodialysis.
Methods
A retrospective analysis was completed using a patient sample comprising children receiving maintenance hemodialysis at Mattel Children’s Hospital at the University of California Los Angeles (UCLA), Los Angeles, CA, USA, between 1 May 2005 and 30 April 2006 and Texas Children’s Hospital, Houston, TX, USA, from 1 January through 31 December 2003. Patients received maintenance hemodialysis for at least 3 consecutive months and were ≤25 years of age and >20 kg. Patients with a previously failed AVG/AVF were excluded from study. The Institutional Review Boards at UCLA and Baylor College of Medicine approved the study. Patient data included age, gender, ethnicity, disease leading to end-stage renal disease (ESRD), and vascular access type. During the 1-year study period, the numbers of dialysis sessions were recorded, along with any access-related complications. These were subdivided into infectious or access-related complications (see definitions below) and included number and duration of hospitalizations. In addition, outpatient administration of antibiotics due to infections complications and alteplase treatments given before, during, or after hemodialysis treatments were recorded.
Definitions
Infectious complications were defined as any hospitalization that occurred for fever or other signs and symptoms of infection that could be attributed to the presence of an indwelling CVC or AVG/AVF. Access complications were defined as any hospitalization that resulted from a malfunction of hemodialysis vascular access. This included catheter stripping, replacement, and AVG/AVF thrombectomy.
Completion of Pediatric Quality-of-Life Inventory
Patients and their parents were asked to complete the Pediatric Quality-of-Life Inventory (PedsQL™ Generic 4.0) [13] at the end of the study period or when they stopped hemodialysis therapy due to a modality change or renal transplantation. The PedsQL™ has been validated as a reliable HRQOL assessment instrument in pediatric patients with ESRD [14]. After introductory instructions from a study coordinator, parents and patients >8 years of age self-administered the PedsQL™. For patients <8 years of age or in cases in which patients were unable to self-administer the survey, the study coordinator read the PedsQL™ questions aloud and recorded the patients’ answers. The patient and parents completed the questionnaires independently of one another.
Statistical methods
As there were no significant differences seen between the two medical centers with respect to demographics, complication rates, or HRQOL scores, data were pooled together. Data are presented as means ± standard deviations. Statistically significant differences between demographics or complications were determined by chi-square analysis. The unpaired t test was used to determine differences in HRQOL scores between groups. A p value <0.05 was considered significant.
Results
Demographics
Demographic information for the 51 patients included in this study is listed in Table 1. There were 30 CVC patients (12 from UCLA and 18 from Baylor) and 21 AVG/AVF patients (10 from UCLA and 11 from Baylor). Mean CVC patient age (13.6 ± 4.2 years) was lower than AVG/AVF patient age (17.4 ± 2.1 years, p < 0.05). Only one patient was older than 21 years. There were no significant differences noted with respect to other demographic variables for CVC patients versus AVG/AVF patients.
Over the 1-year study period, CVC and AVG/AVF patients received a total of 2,393 and 3,506 hemodialysis treatments, respectively. During the study period, one patient who received a majority of hemodialysis treatments through an AVG was transitioned to a CVC due to infectious complications (see below). None of the CVC patients were transitioned to AVG/AVF access. Three patients (two CVC and one AVG/AVF) transitioned off dialysis due to renal transplantation.
Complications
Complication rates due to infection or access malfunction are shown in Table 2. Eighteen out of 30 CVC patients were hospitalized at least once during the study period, with nine patients hospitalized multiple times for CVC-related issues. In CVC patients, complications due to infection resulted in 86 hospital days, whereas access revisions resulted in 64 hospital days (p=NS). Five out of 21 AVG/AVF patients were hospitalized during the study period, with only one patient hospitalized multiple times. In AVG/AVF patients, complications due to infection resulted in 7 hospital days, whereas access revisions resulted in 6 hospital days (p=NS).
When normalized to the number of hemodialysis treatments, the complication rate due to infection was higher in CVC patients, who were hospitalized 3.7 days for every 100 hemodialysis treatment days, versus AVG/AVF patients, who were hospitalized 0.2 days for each 100 hemodialysis treatment days (p < 0.01). Similarly CVC patients had a much higher rate of access revision, needing 2.7 hospital days for every 100 hemodialysis treatments compared with 0.2 days for every 100 hemodialysis treatments in AVG/AVF patients (p < 0.01). Outpatient interventions due to infection complication and access malfunction included the administration of antibiotics and alteplase. CVC patients received 216 separate antibiotic administrations and 542 alteplase treatments (22.6 treatments for every 100 hemodialysis treatments) over the study period. AVG/AVF patients underwent only two antibiotic administrations and no alteplase treatments. CVC patients had a significantly higher rate of outpatient antibiotic administrations (9.1 for every 100 hemodialysis treatments) versus AVG/AVF patients (0.06 for every 100 hemodialysis treatments), (p < 0.01).
Health-related quality of life
HRQOL testing was performed on all 51 patients. Mean HRQOL scores from the PedsQL™ for both CVC and AVG/AVF patients and their parents are presented in Table 3. No significant differences were observed in any specific HRQOL domain between the CVC and AVG/AVF patients/parents or in the total HRQOL domain.
Discussion
Previous reports of access-related complications in pediatric hemodialysis patients have been sparse, and no study has compared overall complications, hospitalizations, outpatient access complications and HRQOL between patients dialyzed via a CVC or permanent access. Data from this study demonstrate that CVC use is associated with a much higher rate complication rate. Hospitalization rates associated with CVCs were more than ten times greater than those associated with AVG/AVFs. Hospitalization days (normalized to number of hemodialysis treatments) of CVC patients were nearly 20 times that of AVG/AVF patients. However, there were no differences in reported HRQOL between the two groups. In sharp contrast to the magnitude of hospitalizations seen in CVC patients due to access malfunction, AVG/AVF patients spent only 0.2 days in hospital for every 100 hemodialysis treatments. Considering the perceived difficulties in creating and maintaining permanent access in children, this result is surprising but not inconsistent with previous reports. One-year survival rates for CVCs range from 27% to 62% [11, 15, 16], whereas those of AVG/AVF range from 74% to 96% [9].
A commonly used argument against the placement of AVG/AVFs is the relatively short waiting times for renal transplantation in the pediatric population. Whereas renal transplantation remains the therapy of choice for pediatric ESRD patients, several subpopulations require long-term hemodialysis access [17]. For example, patients at risk for recurrent disease or highly sensitized patients often require hemodialysis for extended periods. These patients require particular attention when hemodialysis access is placed, to ensure that such access will remain available for their entire lifetime. In fact, due to the finite lifespan of a renal allograft, planning for vascular access poses a unique challenge in the pediatric population. Children with renal failure may be facing 40–50 years on dialysis. As a result, any intervention that could compromise future vascular access must be avoided at all costs. Catheters frequently lead to stenosis or thrombosis of the host vessel or the central veins [18]. This is particularly true in children, who have smaller diameter veins than adults. Venous stenosis of the central veins creates outflow obstruction for future fistula formation and may negatively alter the outcome of ESRD therapy in children.
Although many of the items tested in the PedsQL™ favored the use the AVG/AVGs, there were no significant differences seen between the two groups. Even though this study is relatively large for a pediatric hemodialysis study, we recognize that given the nature of HRQOL testing, it is underpowered. Thus, it would take a much larger sample size to adequately address individual items of HRQOL.
One particular issue that needs further study is the concern that the repeated needle sticks associated with the use of AVG/AVFs negatively influences patients HRQOL. This concern plays a major role when vascular access is considered in younger children, where pain could be a prohibitive factor in access cannulation. Although the HRQOL survey administered did not specifically address the impact of cannulation on HRQOL, the PedsQL™ data do not support a negative impact of cannulation on general HRQOL. We speculate that the negative stigma associated with needle sticks may not be as profound as previously thought, although this area requires more direct assessment.
A final consideration is the economic and social burden that CVC use appears to have over the use of AVG/AVFs. We observed a hospitalization rate an order of magnitude higher with CVCs. Although not directly measured in this study, this hospitalization rate unquestionably drives up the cost of medical care and disrupts normal work, school, and family schedules. The outpatient burden with the use of CVCs, which has not been addressed in any other study, appears just as significant. Using a conservative estimate of 1.5 h for medication preparation and administration, CVC patients increased use of outpatient antibiotic and atelplase treatments required an additional 48 h of care per 100 hemodialysis treatments. Thus, use of AVG/AVFs over CVCs in pediatric patients may lead to substantial financial savings.
One potential confounding factor when interpreting the results of this study is the younger average age seen in the CVC group. This may be a reflection of physician bias to place CVCs in younger and smaller patients. However, the age differences seen would not be expected to influence the rate of complications, as the youngest patient in the CVC group was 9 years old. Likely, the weight cutoff of 20 kg used in this study eliminated age as a potential confounding factor for infectious complications.
The choice of vascular access in pediatric patients undergoing hemodialysis remains a controversial subject. However, our study results support the recommendations of the Fistula First Initiative and the K-DOQI Pediatric Vascular Access Clinical Practice Recommendation, as AVG/AVF were associated with a significantly lower complication rate without any negative influence on HRQOL. We would recommend that AVG/AVFs should be the primary form of hemodialysis access for children requiring long-term maintenance hemodialysis.
References
D’Cunha PT, Besarab A (2004) Vascular access for hemodialysis: 2004 and beyond. Curr Opin Nephrol Hypertens 13:623–629
National Kidney Foundation (2006). KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for 2006 Updates: Hemodialysis Adequacy, Peritoneal Dialysis Adequacy, and Vascular Access. Am J Kidney Dis 48(Suppl 1):S1–S322
Neu AM, Ho PL, McDonald RA, Warady BA (2002) Chronic dialysis in children and adolescents. The 2001 NAPRTCS Annual Report. Pediatr Nephrol 17:656–663
Neu AM, Fivush BA, Warady BA, Watkins SL, Friedman AL, Brem AS, Goldstein S, Frankenfield DL (2003) Longitudinal analysis of intermediate outcomes in adolescent hemodialysis patients. Pediatr Nephrol 18:1172–1176
Fischbach M, Edefonti A, Schroder C, Watson A, The European Pediatric Dialysis Working Group (2005) Hemodialysis in children: general practical guidelines. Pediatr Nephrol 20:1054–1066
Wasse H, Kutner N, Zhang R, Huang Y (2007) Association of initial hemodialysis vascular access with patient-reported health status and quality of life. Clin J Am Soc Nephrol 2:708–714
Feldman HI, Kobrin S, Wasserstein A (1996) Hemodialysis vascular access morbidity. J Am Soc Nephrol 7:523–535
Stevenson KB, Hannah EL, Lowder CA, Adcox MJ, Davidson RL, Mallea MC, Narasimban N, Waguild JP (2002) Epidemiology of hemodialysis vascular access infections from longitudinal infection surveillance data: predicting the impact of NKF-DOQI clinical practice guidelines for vascular access. Am J Kidney Dis 39:549–555
Sheth RD, Brandt ML, Brewer ED, Nuchtern JG, Kale AS, Goildstein SL (2002) Permanent hemodialysis vascular access survival in children and adolescents with end-stage renal disease. Kidney Int 62:1864–1869
Brittinger WD, Walker G, Twittenhoff WD, Konrad N (1997) Vascular access for hemodialysis in children. Pediatr Nephrol 11:87–95
Ramage IJ, Bailie A, Tyerman KS, McColl JH, Pollard SG, Fitzpatrick MM (2005) Vascular access survival in children and young adults receiving long-term hemodialysis. Am J Kidney Dis 45:708–714
Fadrowski JJ, Hwang W, Frankenfield DL, Fivush BA, Neu AM, Furth SL (2006) Clinical course associated with vascular access type in a national cohort of adolescents who receive hemodialysis: findings from the Clinical Performance Measures and US Renal Data System projects. Clin J Am Soc Nephrol 1:987–992
Varni JW, Seid M, Kurtin PS (2001) PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 39:800–812
Goldstein SL, Graham N, Burwinkle T, Warady B, Farrah R, Varni JW (2006) Health-related quality of life in pediatric patients with ESRD. Pediatr Nephrol 21:846–850
Goldstein SL, Macierowski CT, Jabs K (1997) Hemodialysis catheter survival and complications in children and adolescents. Pediatr Nephrol 11:74–77
Sheth RD, Kale AS, Brewer ED, Brandt ML, Nuchtern JG, Goldstein SL (2001) Successful use of Tesio catheters in pediatric patients receiving chronic hemodialysis. Am J Kidney Dis 38:553–559
Goldstein SL (2007) Advances in renal replacement therapy as a bridge to renal transplantation. Pediatr Transplant 11:463–470
Agarwal AK, Patel BM, Haddad NJ (2007) Central vein stenosis: a nephrologist’s perspective. Semin Dial 20:53–62
Acknowledgments
This work was supported in part by USPHS grants DK-35423 and DK-67563 and funds from the Casey Lee Ball Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zaritsky, J.J., Salusky, I.B., Gales, B. et al. Vascular access complications in long-term pediatric hemodialysis patients. Pediatr Nephrol 23, 2061–2065 (2008). https://doi.org/10.1007/s00467-008-0956-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-008-0956-1