Abstract
Objective
We evaluated the association between inflammation and oxidative stress with carotid intima media thickness (cIMT) and elasticity increment module (Einc) in pediatric patients with chronic kidney disease (CKD).
Methods
This analytical, cross-sectional study assessed 134 children aged 6–17 years with CKD. Anthropometric measurements and biochemistry of intact parathyroid hormone (iPTH), high-sensitivity C-reactive protein (CRP), interleukin (IL)-6, IL-1β, reduced glutathione (GSH), malondialdehyde, nitric oxide, and homocysteine were recorded. Bilateral carotid ultrasound (US) was taken. Patients were compared with controls for cIMT and Einc using ≥ 75 percentile (PC).
Results
Mean cIMT was 0.528 ± 0.089 mm; Einc was 0.174 ± 0.121 kPa × 103; cIMT negatively correlated with phosphorus (r −0.19, p = 0.028) and the calcium × phosphorus (Ca × P) product (r −0.26, p = 0.002), and positively with iPTH (r 0.19,p = 0.024). After adjusting for potential confounders, hemodialysis (HD) (β = 0.111, p = <0.001), automated peritoneal dialysis (APD) (β = 0.064, p = 0.026), and Ca x P product (β = −0.002, p = 0.015) predicted cIMT (R 2 = 0.296). In patients on dialysis, HD (β = 0.068, p = 0.010), low-density lipoprotein cholesterol (LDL-C) (β = 0.001, p = 0.048), and GSH (β = −0.0001, p = 0.041) independently predicted cIMT (R 2 = 0.204); HD, hypoalbuminemia, and high iPTH increased the risk of increased cIMT. In dialysis, Einc was inversely associated with GSH, and in predialysis, Ca × P correlated with/predicted Einc (β = 0.001, p = 0.009).
Conclusions
cIMT and Einc strongly associate with several biochemical parameters and GSH but not with other oxidative stress or inflammation markers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with chronic kidney disease (CKD) are more susceptible to atherosclerosis than the general population of the same age and gender. In addition to the traditional cardiovascular risk (CVR) factors, there is growing interest in knowing the effects of nontraditional risk factors, such as inflammation, oxidative stress, and hyperhomocysteinemia. Traditional CVR factors include age, male sex, hypertension (HTA), diabetes mellitus (DM), dyslipidemia, and physical inactivity. Other risk factors in CKD are anemia, hypervolemia, hyperparathyroidism, among others, as well as factors from dialysis modality [1, 2]. Nontraditional risk factors include oxidative stress and inflammation [3, 4]. Vascular Doppler ultrasound (US) is a noninvasive tool that is relatively inexpensive and has the potential to identify populations at high risk for CVD, including in the early stages, through the measurement of intima media thickness of the carotid arteries and different measurements of arterial stiffness [5–7]. It is noteworthy that, given the common state of malnutrition presented by CKD patients as a consequence of both the imbalance between anabolism and catabolism imposed by the disease, and dietary restrictions that are part of the treatment, weight and body mass index (BMI) are quite different in patients compared with healthy children. One of the gaps in current knowledge is to establish precisely the correlation between size, growth, and race in carotid intima media thickness (cIMT).
A more global evaluation of the physical properties of the arterial system can be obtained by measuring arterial stiffness derived from the complex interactions between ventricular output, physical properties of the system, and hematological characteristics of the blood [8]. Arterial stiffness is a dynamic property and is dependent of vascular structure and function and systolic (SBP) and diastolic (DBP) blood pressure. Regardless of the technique used to measure arterial stiffness, experience in children is limited. Arterial distension measured by US is altered in children with a family history of myocardial infarction, in children with high levels of low-density-lipoprotein cholesterol (LDL-C), with obesity, with hypertension, with hyperinsulinemia, and with type 1 DM [5, 7].
There are various ways to evaluate vascular elasticity. Pulse wave velocity (PWV) is defined by the equation by Moens-Korteweg, where PWV = √(Eh/2pR), where E is the Young module of the arterial wall, h is wall thickening, R is the arterial radius at end diastole, and p is blood density [9]. In order to measure other parameters of arterial stiffness, the formulas originally described by Isnard et al. are usually applied [10]. Although PWV is the most convenient method for epidemiological studies, local measurements of arterial stiffness, such as elasticity increment module (Einc), are the most convenient for analyzing physiopathological, pharmacological, and therapeutic bases [11].
The scarcity of data on vascular damage in the early stages of CKD, measured with high-resolution US, is a concern for nephrologists who care for such children [12–15]. In one study, Chavarría et al. evaluated 60 pediatric patients on any dialysis modality and found that 29 had increased cIMT, which was associated with time on dialysis of >2 years, hypercalcemia, greater intake of calcitriol (CTR), and being on HD [16]. To our knowledge, no study to date has evaluated both traditional and nontraditional CVR factors on cIMT and included patients from both dialysis modalities and those in the early stages of the disease (stages 2–4). The object of our study was to measure the magnitude of association between concentrations of mediators of inflammation, oxidative stress, and antioxidation with cIMT and Einc in pediatric patients with CKD, where a timely, adequate intervention might contribute to delaying the appearance of CVD.
Methods
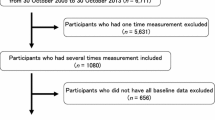
Consecutive cases of children ages 2 years to 16 years, 11 months of age with a diagnosis of CKD in stages 2–5 were obtained from a reference center (Pediatric Nephrology Services of UMAE Hospital, General Centro Médico La Raza; and UMAE Pediatric Hospital, CMN SXXI del IMSS) and were invited to participate, with the following inclusion criteria: either without treatment (predialysis) or with at least 1 month of treatment on automated peritoneal dialysis (APD) or hemodialysis (HD). In addition, parents and children >8 years gave written consent to participate in the study, which was approved by the National Ethics and Research Committee. Excluded were patients with CKD as a consequence of a rheumatic disease with vasculitis, such as lupus erythematosus, acute vascular purpura, or Wegner’s granulomatosis; with clinical evidence of some infection either at the time of taking laboratory samples and/or US or in the week prior, as evaluated by the authors, or who had undergone surgery during the previous month; those with a family history of dyslipidemia or who did not cooperate in the US; and patients taking treatment with corticosteroids or any other immunosuppressor.
Medical history, anthropometric measurements (age, weight, height, systolic and diastolic BP and biochemistry were recorded. Total cholesterol (TC), high-density-lipoprotein cholesterol (HDL-C), triglycerides (TG), albumin (Alb), calcium (Ca), and phosphorus (P) were measured using the Synchron CX analyzer (Beckman Systems, Fullerton, CA, USA), according to standard protocols. Coefficients of variation for TC and HDL-C were 3.3 % and 2.5 %, respectively. Plasma interleukin (IL)-6, IL1-b, and tumor necrosis factor (TNF)-α concentrations were determined using the enzyme-linked immunosorbent assay (ELISA) (Quantike HS Human Immunoassay Kits, R&D Systems, Minneapolis, MN, USA), plasma C-reactive protein (CRP) was measured using a highly sensitive human CRP (hsCRP) ELISA kit (Alpha Diagnostic, San Antonio, TX, USA ) according to the manufacturer’s instructions, and results were read by an ELISA reader (Sunrise, Tecan USA, Durham, NC, USA). Reduced glutathione (GSH) was measured by lambda 25 spectrophotometry (Perkins Elmer, USA). Nitric oxide (NO) was measured with ELISA KontrolLab Eliread (RT-2100C) using the Greiss method. Homocysteine was measured by chemoluminescence on Immulite 1000 equipment (Siemens, Germany). BMI was calculated as kilograms per square meter of body surface, and the z-score was calculated.
All studies were performed by a single, trained radiologist with a high-resolution US scanner (Sonosite Micromaxx Fuji FilmTM, Japan), with imaging on B mode (real time), Doppler color, and Doppler duplex spectral equipped with a 7–12-MHz linear array transducer. Doppler and real-time US studies were performed after patients underwent an overnight fast. Patients were placed in the supine position with the neck in hyperextension. The cIMT was defined by the border between the echolucent vessel lumen and the echogenic intima and the border between the echolucent media and echogenic adventitia. The measurement was done during diastole, according to American Heart Association (AHA) 2009 recommendations [7]. All scans were digitally photographed and stored in the US hard disk and via Ethernet. Images were subsequently analyzed by the same radiologist using QLAB 4.2.1 Advanced Ultrasound Quantification software developed for automatic analysis of US images, with the computerized standardized intima media measurement. Mean value of cIMT for the right and left carotid arteries were calculated.
The formulas originally described by Isnard et al. were used to measure arterial stiffness: Distensibility (DC) = 2(ΔD/D)/(SBP−DBP), where D is diastolic diameter and ΔD the change in artery diameter during systole. Rigidity, defined by the module Einc. Einc, is a marker of intrinsic properties of arterial wall material independent of its geometry and is calculated using the light cut section area (LCSA) = π(D/2)2 and the wall cut section area (WCSA) = π(D/2 + cIMT)2−π(D/2)2; therefore, Einc = 3(1 + [LCSA/WCSA])/DC) [10].
Analysis was done using Student’s t, Mann–Whitney U, χ2, or Fisher exact test and multiple logistic regressions. Among the variables, BP >95 percentile according to sex, age, and height was considered hypertension [17]; malnutrition was considered as height <2 z-scores [18]; anemia was based on hemoglobin levels, as indicated by the World Health Organization, and adjusted by age and sex [19]. Kidney Disease Outcomes Quality Initiative (KDOQI) and Kidney Disease/Improving Global Outcomes (KDIGO) guidelines, adjusted for age and CKD stage, were used to determine normal, high, and low levels of intact parathyroid hormone (iPTH) and P. cIMT in the patient group was compared with a normal control group, as presented by Rabago et al. [5], and Einc ≤ or > 75 percentile (PC). A value of p < 0.05 was considered significant. Analysis was done with software package SPSS 16.0.
Results
Of the 134 children who participated in the study, 66 (49.3 %) were girls; 39 (29.1 %) were in stages 2–4 CKD and receiving only medical treatment (predialysis patients), 42 (31.3 %) were on HD, and 53 (39.6 %) were on APD. The median time from diagnosis was 26 (range 1–205) months. Mean patient cIMT was 0.528 ± 0.089 mm and Einc 0.174 ± 0.121 kPa × 103. Table 1 shows the differences among the values for each variable in the three groups (predialysis, APD, HD). Significant differences were observed regarding months in therapy; BMI z-score (zs), mean BP in mmHg, hemoglobin, and serum Alb (sAlb). In regards to lipid profile, there were significant differences in values for triglycerides, although not so for HDL-C (mg/dl). There were significant differences in corrected values for Ca, P, Ca x P product, and iPTH; however, patients on APD had greater concentrations than those on HD, with an effect size of 0.35.
Regarding inflammation markers, oxidative stress, and antioxidation, there were significant differences among treatment groups in GSH and NO levels, as well as in homocysteine concentrations. Likewise, average values of cIMT among treatment groups were significantly higher in patients on HD than on APD and, in turn, greater in patients on APD than in predialysis, although the same was not true for Einc (Table 1).
In the patient group, malnourishment was 64.2 %, overweight or obese 9 %, hypertension 48.5 %, anemia 60.4 %, Alb < 4 g/dl 27.6 %, hypertriglyceridemia 75 %, reduced HDL-C 44 %, high LDL-C 29.1 %, hypocalcemia 49.3 %, hypercalcemia 14.2 %, hypophosphatemia 62.7 %, hyperphosphatemia 29.1 %, elevated Ca x P product 9.7 %, low iPTH 12.7 %, and high iPTH 47 %. In the analysis of predialysis patients by stage, malnutrition was more frequent in stage 4 patients than the other stages (data not shown). According to treatment modality, there were statistically significant differences in the proportion of adolescents, there being more patients on HD (p = 0.005); likewise regarding replacement therapy time and proportion of patients overweight or obese, which was greater in predialysis patients (p = 0.036); the proportion of hypertensives was lower in predialysis patients (p = 0.010). Proportion of patients with anemia was lower in APD patients. A greater proportion in the APD group had hypertriglyceridemia and hypoalbuminemia whereas a greater proportion in the HD group had hypocalcemia. There was a greater proportion of patients with normal GSH in the APD than the HD group, and in the HD than the predialysis group (p = 0.002). A greater proportion of patients in HD and APD groups had abnormal cIMT than in predialysis patients, with significant difference between HD and APD patients (data not shown). There were significant differences in some mediators of inflammation but not IL-6, IL-1β, TNF-α, hsCRP, and oxidative stress [malondialdehyde (MDA)] (Table 1).
To evaluate the association of cIMT (mm) with study variables, we performed an analysis of correlations and found an inverse significant association with concentrations of P (r −0.19, p = 0.028), Ca × P product (r −0.26, p = 0.002), and positive for iPTH (r 0.19, p = 0.024). There was no significant correlation of cIMT with any of the other variables, including levels of inflammation markers, oxidative stress, antioxidation, and homocysteine (data not shown). However, in patients on either dialysis modality, there was a negative correlation of cIMT with P and Ca × P product (r −0.28, p = 0.006).
Given that no normal values have been established for cIMT in children with CKD, patients were evaluated according to the values established as normal by Rabago et al. [5]. Patients with abnormal cIMT had significantly higher concentrations of iPTH [1,150 (33–2,419) vs 405 (3.7–5,572); p = 0.016)], and lower Ca × P product (40.96 ± 10.95 vs 45.31 ± 10.97; p = 0.050) and GSH (432.37 ± 130.17 vs 509.29 ± 211.65; p = 0.015) than those with abnormal cIMT. Patients with abnormal cIMT also had a lower BMIzs (−1.35 ± 1.37 vs −0.79 ± 1.59; p = 0.069). For patients on either dialysis modality, no significant difference was found in concentrations of variables between those with normal or abnormal cIMT. However, patients on dialysis with abnormal cIMT had lower GSH concentrations (p = 0.167); effect size was 0.33 (data not shown). The proportion of patients in stage 5 CKD and on HD was higher in those with abnormal cIMT compared with those in any other stage, whereas in patients in stage 5 and on APD, this relation was inverse with those in stages 2, 3, and 4 (data not shown). Given that the clinical characteristics of our patients are complex—and inflammation markers, oxidative stress, and antioxidation with cIMT may be influenced by factors such as time of disease evolution, nutritional status, hypertension, anemia, hypoalbuminemia, blood lipids, and Ca-P metabolic status—logistic regression was performed to adjust for the effect of potentially confounding variables on the associations sought. As shown in Table 2, when the total group of patients was analyzed adjusting for potentially confounding variables, stage 5 CKD in both APD and HD and Ca × P product were independent predictors of cIMT.
For patients on dialysis, those on HD, those with hypoalbuminemia, and those with high iPTH had greater probability of having abnormal cIMT (Tables 3 and 4).
Comparing predialysis patients according to CKD stage, we found no significant differences in cIMT values (0.474 ± 0.072 mm) or in Einc (0.173 ± 0.115 kPa × 103) (data not shown); however, P and Ca × P product showed a significant correlation with Einc (r = 0.44, p = 0.005). Of the 134 patients, the proportion with low concentrations of iPTH was significantly greater in those with Einc ≥75 PC (21.2 % vs 9.9 %, p = 0.023). On the other hand, in patents on dialysis, a greater proportion in those with Einc ≥75 PC (50.0 %, p = 0.036) had lower GSH (Tables 5 and 6).
Logistic regression showed that both high and low iPTH represent greater probability of having Einc ≥75 PC. In patients on dialysis, logistic regression showed that none of the variables was associated with a greater probability of having Einc ≥75 PC.
Discussion
Primary findings of this study were that the average cIMT of all patients was 0.528 ± 0.089 and that 70.9 % had cIMT >0.470 mm, the value reported as normal in a group of healthy Mexican children [5]. Patients in predialysis already presented high cIMT. Chavarría et al. [16] reported a prevalence of high cIMT of 48 %, but these authors took as the cutoff value the normal values reported by Jourdan et al. in German patients that only included individuals 10–20 years old [20]. Our study includes children from 6 years of age, so it was necessary to take a cutoff of 0.470 mm. Canpolat et al. [21] reported a prevalence of increased cIMT of 15 % in predialysis patients and of 74 % in HD patients. Most studies did not use a cutoff point to consider high or normal cIMT but analyzed it as a continuous variable. Ethnic differences could be a reason for such varied findings, which suggests future efforts to create tables for children with CKD in various populations. In our study, we found an association of cIMT with the following risk factors:
-
1.
Levels of blood P and Ca × P: Other studies have demonstrated significant positive correlation of cIMT with P [22–25], Ca × P product [21, 24, 25], and historic Ca × P products [15], as well as the dose of P chelates based on Ca [15, 24], and CTR dosage [14, 15, 25]. It is possible that we are indicating especially high doses of P chelates based on Ca, which could explain both the low prevalence of hyperphosphatemia and, indirectly, its negative correlation (and consequently that of Ca × P product) with cIMT. The study by Mitsnefes et al. [24] is particularly interesting in this regard, as they found that whereas in patients in predialysis cIMT correlated with Ca × P product, in patients on dialysis it associated more so with the dose of P chelates based on Ca and CTR dose, rather than Ca × P product. In our predialysis patients, there was a positive association between cIMT and Ca × P product, which might reflect the less strict and longer treatment regime with P chelates for bone metabolism disease.
On the other hand, the high prevalence of undernourished patients is noteworthy because, added to the high prevalence of patients with low and normal blood P, it may reflect the association between malnutrition, secondary hypophosphatemia and CVD risk. This merits further study.
-
2.
Hypoalbuminemia: Our findings agree with those reported by other authors [15, 21, 26, 27]. The mechanism of vascular damage in hypoalbuminemia is not completely known, but it is known that low levels of albumin, one of the main determinants of malnutrition–inflammation–atherosclerosis (MIA) syndrome, is a strong predictor of mortality in patients on dialysis [28, 29]. A longitudinal study in adults demonstrated that hsCRP, cIMT, and albumin were predictors of mortality in patients with CKD over the long term [29]. Interestingly, in our overall patient group and in patients on dialysis, BMIzs was lower among patients with abnormal cIMT, and although the p value was >0.05, the sizes of effect were 0.37 and 0.30, respectively. Therefore, taking into account that having albuminemia represented a greater probability of abnormal cIMT, it is probable that the negative correlation of cIMT with P and Ca × P product translates into an association between cIMT and a deteriorated nutritional status.
-
3.
High blood levels of iPTH: Positive association of cIMT with iPTH is consistent with that reported previously [21, 25, 30]. PTH can, in itself, contribute to vascular damage through different mechanisms, through alterations to CA-P metabolism, allowing thickening of the vascular wall [31] or favoring a chronic increase in BP.
-
4.
Low blood concentrations of GSH: Characteristics of patients with CKD, such as hypertension and a restricted diet of fresh fruits and vegetables to avoid hyperkalemia, with the corresponding reduction in vitamin C levels, predispose them to greater levels of oxidative stress than healthy people [29]. Every HD session induces oxidative stress, with the generation of reactive oxygen species (ROS) on the surface of the dialysate membrane through the activation of polymorphonuclear neutrophiles due to bioincompatibility, whereas a concomitant loss of antioxidant vitamins is produced through the process of dialysis itself.
-
5.
LDL-C: Briese et al. [32] found a positive correlation between LDL-C and cIMT. Oxidized LDL-C is transported to the subendothelial space of the vessels, where it provides phagocytes for macrophages, giving way to the formation of foamy cells that liberate cytokines (IL-β, TNF-α), matrix metalloproteinase-9 (MMP-9), ROS, and other tissue factors into the interior of the intima and media layers of the vessel, which leads to thickening and later atherosclerosis [33].
-
6
HD treatment: Chavarría et al. [16] found similar results to those found in our study. Higher cIMT in patients on HD compared with those on APD has not been completely analyzed, although it has been reported previously [26, 34]. Patients on HD may have a greater risk of cardiovascular damage for various reasons, the most feasible being contact of blood cells with the complementary systems of a foreign surface (the membrane), which would lead to increased liberation by leukocytes of ROS, IL-1β, IL-6, IL-8, IL-12, IL-13, TNF-α, tactile chemical peptide of type 1 monocytes, and interferon (IFN). This contact between blood and the membrane also activates the complement through alternate means, and the subsequent inflammatory process may be the cause of greater vascular damage [35].
We found no difference in Einc among different stages of CKD, which coincides with the results by Rinat et al. [36] but contrasts with Mitsnefes et al. [24], who found that patients on dialysis have significantly higher Einc than predialysis patients. In our study, analysis in predialysis patients of Ca × P product showed significant positive correlation with Einc, an association not found previously. As with the association with cIMT, in analysis of patients in either dialysis modality, the proportion of patients with concentrations of GSH < 75 PC was greater in those with Einc ≥75 PC; however, this relationship became inverted when analyzing the total group. We attribute this to the fact that, as explained previously, patients on dialysis—particularly those on HD—have a greater risk of reduced antioxidant mechanisms, leading to greater vascular damage. On the other hand, the proportion of patients with low iPTH was greater in patients with Einc ≥ 75 PC, and in logistic regression of all patients, those with low and high iPTH showed greater probability of Einc ≥75 PC. Nonetheless, only 17 patients had iPTH below recommended values, and the lower limits of 95 % confidence intervals (CI) in both cases were very close to 1 (1.01 for hypoparathyroidism and 1.04 for hyperparathyroidism). Mitsnefes et al. [24] found correlation between Einc and iPTH, and this turned out to be an independent predictor of the same. Likewise, with the use of high dosage of Ca-based P chelates and aggressive treatment with vitamin D analogs for hyperparathyroidism, hypoparathyroidism is another possible complication of bone metabolism disease in the CKD patient. As a consequence of hypoparathyroidism, adynamic bone cannot properly deposit calcium in its interior, which leads to poor regulation of the same in the blood. In this context, Ca load, be it in dialysis or P chelates, leads to hypercalcemia, which causes other tissues aside from bone, such as blood vessels, to deposit calcium in their walls. An increase in the probability of vascular calcifications in patients with hypoparathyroidism has been demonstrated by previous authors [37]. Galassi et al. [38], in an analysis of 109 adult patients on HD, of whom 64 had DM, found that patients treated with Ca-based P chelates had a greater probability of developing hypoparathyroidism and greater values of coronary arterial calcium (measured by computed electron-beam tomography) than patients treated with Sevelamer. Likewise, Toussaint et al. [39], in a longitudinal study of 48 patients with glomerular filtration rate between 17 and 55 ml/min, found that the values of vascular calcifications correlated positively with PWV values and that Ca × P product correlated positively with PWV. Although we did not measure the presence of calcifications in our patients, it is possible that this is the mechanism by which patients with either hypoparathyroidism or hyperparathyroidism have a greater risk of having Einc ≥75 PC. Adding the presence of vascular calcifications would be useful in future studies.
In summary, the prevalence of cIMT above normal ranges in healthy Mexican children reported previously [5] was high among the patients we studied, including those with CKD in predialysis stages of the disease. According to our results and the findings of various authors, the reason may be associated patients’ with reduced antioxidant capacity, especially those who have begun some dialysis modality, as a consequence of lower levels of GSH. This reduction in antioxidant mechanisms favors circulating particles of LDL-C undergoing oxidation and, by being transported to the subendothelial spaces of the vessels, they become phagocytes for macrophages, giving way to the formation of foamy cells that liberate cytokines (IL-β, TNF-α), MMP-9, ROS, and other tissue factors into the interior of the intima and media layers of the vessel, which leads to thickening and later atherosclerosis [33]. If we add to this a precarious nutritional status, particularly in patients on dialysis, and an environment of Ca-P imbalance due to using high doses of Ca-based P chelates and vitamin D analogs—that provoked in our cross-sectional study hypophosphatemia with lowered values of Ca × P product—vascular calcification could be favored and with it an increase in vascular stiffness.
We recognize the limitations of our study, among them being its cross-sectional design, which does not allow associations that intend to demonstrate causality, only association. We only once measured the variables of interest, which are changing and dynamic. The number of patients by group might not be sufficient to demonstrate real associations within each one. We could not precisely measure adherence to treatments with P chelates and CTR. Also, despite intending to evaluate patients without fluid overload, evaluation of nutritional status was not exact due to the use of weight, height, BMIzs, and height for age, and not of other, more precise, methods (dual-energy X-ray absorptiometry). We did not have an automated method to validate the methodology for later use as a substitute marker. In addition, it was not possible to evaluate adherence to treatment. Given that in practice in Mexico few pediatric patients enter replacement therapy directly with HD instead of PD, it is probable that patients in HD had an unevaluated previous time on APD.
In conclusion, in our pediatric patients with CKD, cIMT, and Einc as markers of vascular risk were associated not only with traditional risk factors such as Ca × P product, iPTH, hypoalbuminemia, and increased LDL-C, but also with reduction in antioxidant mechanisms (GSH) and HD.
References
Longeneker JC, Coresh J, Powe NR, Levey AS, Fink NE, Martin A, Klag MJ (2002) Traditional cardiovascular disease risk factors in dialysis patients compared with the general population: the CHOICE study. J Am Soc Nephrol 13:1918–1927
Goicoechea M, García de Vinuesa S, Gómez-Campderá F, Luño J (2005) Predictive cardiovascular risk factors in patients with chronic kidney disease. Kidney Int 67(Suppl 93):S35–S38
Bayes B, Pastor MC, Bonal J, Juncà J, Hernandez JM, Riutort N, Foraster A, Romero R (2003) Homocysteine, C reactive protein, lipid peroxidation and mortality in hemodialysis patients. Nephrol Dial Transplant 18:106–112
Bayes B, Pastor MC, Bonal J, Romero R (2005) New cardiovascular risk factors in patients with chronic kidney disease: role of folic acid treatment. Kidney Int 67(Suppl 93):S39–S43
Rabago R, Gómez-Díaz RA, Tanus Haj J, Avelar Garnica FJ, Ramirez Soriano E, Nishimura Meguro E, Aguilar-Salinas CA, Wacher NH (2007) Carotid intima media thickness in pediatric type 1 diabetic patients. Diabetes Care 30:2599–2602
De Groot E, Hovingh K, Wiegman A, Duriez P, Smit AJ, Fruchart JC, Kastelein JJ (2004). Measurement of arterial wall thickness as a surrogate marker for atherosclerosis. Circulation 109: III-3 a III-38.
Urbina EM, Williams RV, Alpert BS, Collins RT, Daniels SR, Hayman L, Jacobson M, Mahoney L, Mietus-Snyder M, Rocchini A, Steinberger J, McCrindle B, American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young (2009) Noninvasive assessment of subclinical atherosclerosis in children and adolescents: Recommendations for standard assessment for clinical research: A Scientific statement from the American Heart Association. Hypertension 54:919–950
Davies JI, Struthers AD (2003) Pulse wave analysis and pulse wave velocity: a critical review of their strengths and weakness. J Hypertens 21:463–472
Aggoun Y, Szezepanski I, Bonnet D (2005) Noninvasive assessment of arterial stiffness and risk of atherosclerosis events in children. Pediatr Res 58:173–178
Isnard RN, Pannier BM, Laurent S, London GM, Diebold B, Safar ME (1989) Pulsatile diameter and elastic modulus of the aortic arch in essential hypertension: a noninvasive study. J Am Coll Cardol 13:399–405
Laurent S, Cockcroft J, van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H, European Network for Non-invasive Investigation of Large Arteries (2006) Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 27:2588–2605
Lilien MR, Koemans HA, Schröeder CH (2005) Hemodialysis acutely impairs endothelial function in children. Pediatr Nephrol 20:200–204
Poyrazoglu HM, Düsünsel R, Yikilmaz A, Narin N, Anarat R, Gündüz Z, Coşkun A, Baykan A, Oztürk A (2007) Carotid artery thickness in children and young adults with end stage renal disease. Pediatric Nephrol 22:109–116
Civilibal M, Caliskan S, Oflaz H, Sever L, Candan C, Canpolat N, Kasapcopur O, Bugra Z, Arisoy N (2007) Traditional and new cardiovascular risk markers and factors in pediatric dialysis patients. Pediatr Nephrol 22:1021–1029
Litwin M, Wühl E, Jourdan C, Trelewicz J, Niemirska A, Fahr K, Jobs K, Grenda R, Wawer ZT, Rajszys P, Tröger J, Mehls O, Schaefer F (2005) Altered morphologic properties of large arteries in children with chronic renal failure and after renal transplantation. J Am Soc Nephrol 16:1494–1500
Chavarría LA, Aguilar-Kitsu A, Rosas P, Fajardo A, Mendoza-Guevara L, Sanchez L, Zepeda C, Ibarra P, Luna A, Lindholm B, García-López E (2012) Intima media thickness in children undergoing dialysis. Pediatr Nephrol 27:1557–1564
National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents (1996). Update on the 1987 Task Force on High Blood Pressure in children and adolescents: A working group report from the National High Blood Pressure Education Program. Pediatrics 98:649–658
http://ensanut.insp.mx/informes/ENSANUT2012ResultadosNacionales.pdf, consulted November 8, 2012.
http://www.who.int/vmnis/indicators/haemoglobin_es.pdf, consulted November 8, 2012.
Jourdan C, Wühl E, Litwin M, Fahr K, Trelewicz J, Jobs K, Schenk JP, Grenda R, Mehls O, Tröger J, Schaefer F (2005) Normative values for intima media thickness and distensibility for large arteries in healthy adolescents. J Hypertens 23:1707–1715
Canpolat N, Caliskan S, Sever L, Guzeltas A, Kantarci F, Candan C, Civilibal M, Kasapcopur O, Arisoy N (2012) Glucose intolerance: is it a risk factor for cardiovascular disease in children with chronic kidney disease? Pediatr Nephrol 27:627–35
Ziolkowska H, Brzewski M, Roszkowska-Blaim M (2008) Determinants of the intima media thickness in children and adolescents with chronic kidney disease. Pediatr Nephrol 23:805–11
Litwin M, Wühl E, Jourdan C, Niemirska A, Schenk JP, Jobs K, Grenda R, Wawer ZT, Rajszys P, Mehls O, Schaefer F (2008) Evolution of large-vessel arteriopathy in paediatric patients with chronic kidney disease. Nephrol Dial Transplant 23:2552–7
Mitsnefes MM, Kimball TR, Kartal J, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2005) Cardiac and vascular adaptation in pediatric patients with chronic kidney disease: role of calcium-phosphorus metabolism. J Am Soc Nephrol 16:2803–2805
Shroff RC, Donald AE, Hiorns MP, Watson A, Feather S, Milford D, Ellins EA, Storry C, Ridout D, Deanfield J, Rees L (2007) Mineral metabolism and vascular damage in children on dialysis. J Am Soc Nephrol 18:2996–3003
Dursun I, Poyrazoglu HM, Gunduz Z, Ulger H, Yykylmaz A, Dusunsel R, Patyroglu T, Gurgoze M (2009) The relationship between circulating endothelial microparticles and arterial stiffness and atherosclerosis in children with chronic kidney disease. Nephrol Dial Transplant 24(8):2511–8
Bakkaloglu SA, Saygili A, Sever L, Noyan A, Akman S, Ekim M, Aksu N, Doganay B, Yildiz N, Duzova A, Soylu A, Alpay H, Sonmez F, Civilibal M, Erdem S, Kardelen F (2009) Assessment of cardiovascular risk in paediatric peritoneal dialysis patients: a Turkish Pediatric Peritoneal Dialysis Study Group (TUPEPD) report. Nephrol Dial Transplant 24:3525–3532
Spiegel DM, Raggi P, Smits G, Block GA (2007) Factors associated with mortality in patients new to haemodialysis. Nephrol Dial Transplant 22:3568–3572
Akdag I, Yilmaz Y, Kahvecioglu S, Bolca N, Ercan I, Ersoy A, Gullulu M (2008) Clinical value of the malnutrition-inflammation-atherosclerosis syndrome for long-term prediction of cardiovascular mortality in patients with end-stage renal disease: a 5-year prospective study. Nephron Clin Pract 108:c99–c105
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, Mehls O, Schaefer F (2002) Advanced coronary and carotid arteriopathy in young adult with childhood onset chronic renal failure. Circulation 106:100–105
Rostand SG, Drueke TB (1999) Parathyroid hormone, vitamin D, and cardiovascular disease in chronic renal failure. Kidney Int 56:383–392
Briese S, Wiesner S, Will JC, Lembcke A, Opgen-Rhein B, Nissel R, Wernecke KD, Andreae J, Haffner D, Querfeld U (2006) Arterial and cardiac disease in young adults with childhood-onset end-stage renal disease-impact of calcium and vitamin D therapy. Nephrol Dial Transplant 21:1906–14
Packard RS, Libby P (2008) Inflammation in aterosclerosis: from vascular biology to biomarker discovery and risk prediction. Clin Chem 54:24–38
Sozeri B, Mir S, Kara OD, Levent E (2010) When does the cardiovascular disease appear in patients with chronic kidney disease? Pediatr Cardiol 31:821–828
Mutluay R, Degertekin CK, Poyraz F, Yılmaz MI, Yücel C, Turfan M, Tavil Y, Derici Ü, Arınsoy T, Sindel S (2012) Dialysis type may predict carotid intima media thickness and plaque presence in end stage renal disease patients. Adv Ther 29:370–382
Rinat C, Becker-Cohen R, Nir A, Feinstein S, Shemesh D, Algur N, Ben Shalom E, Farber B, Frishberg Y (2010) A comprehensive study of cardiovascular risk factors, cardiac function and vascular disease in children with chronic renal failure. Nephrol Dial Transplant 25:785–793
London GM, Marty C, Marchais SJ, Guerin AP, Metivier F, de Vernejoul MC (2004) Arterial calcifications and bone histomorphometry in end-stage renal disease. J Am Soc Nephrol 15:1943–1951
Galassi A, Spiegel DM, Bellasi A, Block GA, Raggi P (2006) Accelerated vascular calcification and relative hypoparathyroidism in incident haemodialysis diabetic patients receiving calcium binders. Nephrol Dial Transplant 21:3215–3222
Toussaint ND, Lau KK, Strauss BJ, Polkinghorne KR (2008) Associations between vascular calcification, arterial stiffness and bone mineral density in chronic kidney disease. Nephrol Dial Transplant 23:586–593
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Garcia-Bello, J.A., Gómez-Díaz, R.A., Contreras-Rodríguez, A. et al. Carotid intima media thickness, oxidative stress, and inflammation in children with chronic kidney disease. Pediatr Nephrol 29, 273–281 (2014). https://doi.org/10.1007/s00467-013-2626-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-013-2626-1