Abstract
Cardiovascular disease is a leading cause of long-term morbidity and mortality among children with chronic kidney disease (CKD). At which stage of CKD these appear in children is unknown. This study aimed to determine the prevalence of cardiovascular disease in pediatric CKD patients and to explore the relationship of these changes and treatment methods. The study enrolled pediatric patients with stages 1–5 CKD including 20 patients receiving predialysis (PreD), 8 receiving peritoneal dialysis, and 14 receiving hemodialysis. Aortic stiffness, defined as decreased aortic strain (S) and increased pressure strain normalized by diastolic pressure (Ep*), was described. Sonography of the common carotid artery and left ventricle was performed. The mean age of the children was 13.3 ± 5.3 years. The patients had lower S values (0.35 ± 0.23) than the control subjects (0.44 ± 0.2) (P < 0.05) but higher Ep* (2.46 ± 1.31 vs. 1.32 ± 0.09; P < 0.05). Aortic stiffness was found in 13 patients. The PreD group had lower As levels than the dialysis group but higher levels than the control group. The patients (n = 32) had greater carotid intima-media thickness than the control subjects (0.58 ± 0.14 vs. 0.35 ± 0.12; P < 0.05). The intima-media thickness was greatest in the PreD group (P < 0.05). The patients had a higher left ventricular mass index (LVMI; 42.4 ± 15.6) than the control subjects (28.8 ± 8.47) (P < 0.05) and a larger left ventricle end diastolic diameter (LVEDD; 3.44 ± 0.76 vs. 2.59 ± 0.34; P < 0.05). Left ventricular hypertrophy was found in 32 patients. Both LVMI and LVEDD were higher in the groups receiving hemodialysis and lower in the PreD group. Increased carotid-intima media thickness and left ventricle hypertrophy appeared without hypertension in the PreD group. The indications and timing of dialysis should be reevaluated for children with CKD. In the dialysis groups, fewer cardiovascular changes were found with peritoneal dialysis than with hemodialysis. Therefore, peritoneal dialysis should be preferable to hemodialysis for children with CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chronic kidney disease (CKD) in the pediatric population has become an important issue. The mortality rate for CKD patients is higher than for the general population [46]. Children with CKD have a greater risk of death, particularly from cardiovascular disease (CVD), than the general pediatric population [26]. The risk for CVD seems increased even with incipient renal failure. Weiner et al. [44] showed that moderate renal insufficiency is associated with a 19% excess risk for cardiovascular complications.
Cardiovascular disease is associated with a number of risk factors such as malnutrition, diabetes, hyperlipidemia, hypertension, smoking, male gender, uremia, and anemia [10, 27, 39, 40, 42, 45]. Childhood-onset CKD has a high incidence of arteriopathy, even in the absence of traditional atherogenic risk factors [39, 45]. Progressive renal dysfunction is associated with multiple biochemical and hemodynamic alterations that profoundly affect the cardiovascular system.
The pathologic basis for CVD is arterial damage in the form of arteriosclerosis and atherosclerosis. Arteriosclerosis is described as diffuse thickening and stiffening of mainly large and medium-sized arteries [22]. Atherosclerosis is a form of arteriosclerosis that causes focal lesions in the intima of large and medium-sized arteries. This atherosclerotic process produces changes in the structure and function of the arterial tree [38]. Cardiovascular disease is characterized by functional (aortic stiffness) and morphologic abnormalities such as increased intima-media thickness of the carotid artery (c-IMT) and left ventricular hypertrophy (LVH) [27].
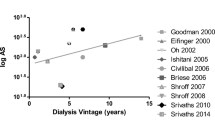
Arterial stiffness is an important mechanical property because it is related to vascular impedance and in turn to the afterload presented to the left ventricle [32]. Stiffness of the abdominal aorta increases with age, and its usefulness as a noninvasive method of assessment has been demonstrated [17, 19, 20, 32]. The presence of vascular calcifications in adult patients with end-stage renal disease (ESRD) has been associated with increased stiffness of large, capacitive, elastic-type arteries such as the aorta and the common carotid artery [14], but only a few studies have evaluated arterial stiffness in children with chronic renal disease [2, 13, 24, 30, 37].
Increased intima-media thickness (IMT) of the large arteries also is an early marker of atherosclerotic changes and a predictor of cardiovascular events in adult dialysis patients. Previous studies have noted an elevation in IMT as early as in stage 2 CKD, with c-IMT most marked in children receiving dialysis [23, 24].
Left ventricular hypertrophy occurs when renal insufficiency is mild or moderate in children and progresses as renal sufficiency deteriorates. Approximately one-third of children with mild to moderate renal insufficiency have increased LVM [16, 29, 31].
Based on these observations, we hypothesized that pathologic changes in the cardiovascular system may give rise to early-stage CKD. This study aimed to describe the prevalence of functional and morphologic changes in the cardiovascular system of pediatric CKD patients and to explore the relationship of these changes and treatment methods.
Patients and Methods
This cross-sectional and observational study included pediatric patients with stages 1–5 CKD followed by predialysis (PreD), peritoneal dialysis (PD), and hemodialysis (HD) at Ege University Faculty of Medicine, Department of Pediatric Nephrology in Turkey and selected from October 2007 to May 2008.
The study enrolled 42 children (23 boys and 19 girls) and 29 healthy children matched for age and gender. These patients included 20 PreD patients (5 stage 1, 9 stage 2, 2 stage 3, and 4 stage 4 patients). Of the 22 stage 5 CKD patients with ESRD, 8 were treated with PD, and 14 were treated with HD. The duration of renal replacement therapy (RRT) ranged from 6 to 139 months (average, 50.6 ± 36 months). The criteria for exclusion from the study specified any clinically overinflammatory disease and overdehydration at the time of screening. The study was approved by the local ethical committees at Izmir.
All the subjects’ weights and heights were measured and their standard deviation scores calculated. The body mass index (BMI) of each subject also was calculated. Nutrition status was evaluated by calculation of the weight–height index. Blood pressure was evaluated by manual and ambulatory 24-h blood pressure monitoring. Hypertension was defined as an average systolic or diastolic blood pressure greater than or equal to the 95th percentile for age, sex, and height. Patients’ clinical characteristics and concomitant medications (phosphate binder, vitamin D, antihypertensive drugs) were retrieved from a medical interview, physical examination, and careful analysis of the patients’ records.
Chronic kidney disease was defined in terms of an estimated glomerular filtration rate (eGFR) (Schwartz formula). Stage 1 (renal injury) was defined by an eGFR greater than 90 ml/min per 1.73 m2, stage 2 (mild) by an eGFR of 60–89 ml/min per 1.73 m2, stage 3 (moderate) by an eGFR of 30–59 ml/min per 1.73 m2, stage 4 (severe) by an eGFR of 15–29 ml/min per 1.73 m2, and stage 5 (ESRD) by an eGFR of less than 15 ml/min per 1.73 m2.
Blood samples were collected from all the patients after a 12-h fast in a standardized manner. The lipid parameters of the patients were evaluated including total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL) and triglycerides, hemoglobin, hematocrit, creatinine clearance (blood plus peritoneal fluid in the dialysis group), serum albumin, calcium (Ca), phosphorus (P), parathyroid hormone, Ca × P, lipid levels, and high sensitive C-reactive protein.
Echocardiographic evaluation was performed with the Hewlett-Packard Sonos-1000 system (Hewlett-Packard, Izmir, Turkey) using a 3.5-mHz transducer by the same cardiologist, who did not know the clinical situation of the patients. Functional changes were defined as aortic stiffness.
Aortic stiffness involves decreased aortic strain (S) and increased pressure strain normalized by diastolic pressure (Ep*). These were measured using a sphygmomanometer with cuff and transthoracic echocardiography. The aortic diameter was measured at the systolic phase (D s) and the diastolic phase (D d). All aortic measurements were performed as previously described by Okubo et al. [34] and Lacombe et al. [17]. The aortic strain was calculated from the changes in aortic diameter as measured by echocardiography using the formula
Pressure strain elastic modulus (Ep) was calculated from S and the changes in brachial artery pressure using the formula
The pressure strain normalized by diastolic pressure (Ep*) was calculated using the formula
where S represents distensibility or elasticity of the aortic wall and Ep* is the mean stiffness of the aorta. Whereas S and Ep* are dimensionless ratios, Ep has the dimension and is represented as N/m2 (force/unit area).
Morphologic changes were defined as increased c-IMT and LVH. Evaluation of c-IMT was performed by carotid artery ultrasound. Measurements in B-mode were performed on both common carotid arteries.
Intima-media thickness was defined as the distance between the leading edges of the lumen–intima interface and the media adventitia interface of the far wall. Left ventricular hypertrophy was defined as increased left ventricular mass index (LVMI) and increased left ventricle end diastolic diameter (LVEDD).
The measurements were determined using standard techniques in accordance with the recommendations of the American Society of Echocardiography. Both LVM and LVMI were calculated using the following standard formulas [7, 8]:
Statistical Analysis
Normality of the data distribution was assessed using the Kolmogorov–Smirnov test, and the values are presented as mean ± standard deviation or as median (interquartile range) unless otherwise specified. Student’s t test, analysis of variance (ANOVA), and Wilcoxon signed ranked test were used to compare differences between numeric values in different groups. Correlations between numeric values were assessed by Pearson analysis. The chi-square test was used to compare prevalence between different groups. Calculations were performed with SPSS version 11.0 for Windows (SPSS, Chicago, IL, USA), and a P value less than 0.05 was determined to be significant.
Results
The study investigated 42 patients. As treatment, 20 patients (F/M: 8/12) received PreD, 8 patients (F/M:3/5) received PD, and 14 patients (F/M:8/6) received HD at the nephrology clinic. The mean age of the patients was 12.0 ± 4. 6 years (range, 3.3–19 years). The mean of duration of therapy was 40.7 ± 30.7 months for PD and 31.1 ± 33.5 months for HD. The mean of weight–height index of the patients (104.3 ± 19.1) was found to be lower than that of the control subjects (113.1 ± 27.1) (P = 0.08). Seven patients (1 receiving PreD, 2 receiving PD, and 4 receiving HD) were found to have malnutrition compared with the control subjects. The systolic and diastolic blood pressures in the patient groups were found to be significantly higher than in the control group. The mean levels of serum lipids were higher in the patients than in the control subjects. The mean high sensitive C-reactive protein (HsCRP) concentration was 1.07 ± 1.86 mg/dl (range, 0.1–8.41 mg/dl). The 16 patients (45.7%) who presented HsCRP levels above 0.3 mg/dl were considered to be inflamed. A larger proportion of HD patients (59%) were inflamed. The main clinical and laboratory characteristics are given in Table 1.
All the children receiving dialysis were administered calcium-based P-binders and calcitriol, whereas the 13 predialysis patients (65%) were given P-binders and 14 (70%) were given calcitriol. A total of 26 patients (9 PreD, 5 PD, and 12 HD patients) (61.9%) were taking antihypertensive drugs.
Of the 42 study patients, 19 (45.2%) had glomerulopathy, 1 (2.3%) had Alport syndrome, 13 (31%) had reflux nephropathy, 4 (9.5%) had neurogenic bladder, 3 (7.1%) had obstructive uropathy, and 2 (4.8%) had hereditary conditions.
Both strain (S) and stiffness (Ep, Ep*) values showed significant differences between the patient and the control groups. The mean S value for the patients (0.27 ± 0.13) was lower than for the control subjects (0.44 ± 0.2) (P = 0.00), whereas the patient Ep (N/m2) and Ep* values were higher than the corresponding control values (respectively, 175 ± 98 and 119 ± 27; P = 0.00 vs. 2.44 ± 1.37 and 1.32 ± 0.09; P = 0.00). Aortic stiffness was found in 35 (69%) of the 42 patients (15 PreD, 8 PD, and 12 HD patients; P = 0,167). The S values were higher in the PreD group (0.30 ± 0.13) than in the PD group (0.24 ± 0.13) or the HD group (0.23 ± 0.09), but the difference was not statistically significant (P = 0.31). The mean Ep* value was lower in the PreD group (2.36 ± 1.61) than in either the PD group (2.46 ± 1.36) or the HD group (2.59 ± 0.89) (P = 0.9) (Table 2).
The mean c-IMT for the patients (0.58 ± 0.14) was higher than for the control subjects (0.35 ± 0.12) (P = 0.01). Increased c-IMT was found in 36 patients (17 PreD, 8 PD, and 14 HD patients). The mean c-IMT was higher in the PreD group (0.58 ± 0.10) than in either the PD group (0.5 ± 0.13) or the HD group (0.52 ± 0.19) (P = 0.25) (Table 2).
In the PreD group, factors affecting increased IMT of the carotid were examined using Pearson’s correlation test, and the results are presented in Table 3. In this group, c-IMT correlated positively with systolic blood pressure (r = 0.700; P = 0.001) and cholesterol (r = 0.669; P = 0.001), whereas it showed no correlation with gender or duration of disease.
We found that the patients had higher values than the control subjects for LVMI (87.5 ± 58.3 vs. 28.8 ± 8.47 g/m2.7; P = 0.00) and LVEDD (3.29 ± 0.60 vs. 2.59 ± 0.34 cm; P = 0.00). Left ventricular hypertrophy was found in 36 patients (18 PreD, 4 PD, and 14 HD patients). The LVMI values were higher in the HD group (103 ± 55.6) than in the PD group (41.01 ± 22.7) or the PreD group (95.2 ± 62.5) (P = 0.03). The LVEDD values were higher in HD group (3.62 ± 0.51) than in the PD group (2.98 ± 0.57) or the PreD group (3.18 ± 0.58) (P = 0.02) (Table 2). In all the patient groups, LVMI was found to be correlated with systolic blood pressure (r = 0.54; P = 0.00), pulse pressure (r = 0.45; P = 0.003), BMI (r = 0.40; P = 0.009), and age (r = 0.67; P = 0.00), but not with male gender (P = 0.39).
Functional and morphologic disorders increased more among the patients than among the control subjects (P < 0.05). The duration of CKD, underlying renal disease, and concomitant medications (vitamin D, phosphate binders, and antihypertensive drugs) were not significantly associated with cardiovascular changes in the CKD patients (data not shown). The PreD group had as many functional and morphologic changes in the cardiovascular system as the RRT group.
Discussion
Clinical and epidemiologic studies have shown that structural and functional changes in large arteries are a major contributing factor to the high mortality rate recorded for adult uremic patients [45]. However, the data on such changes in children with ESRD are limited.
This cross-sectional and observational study assessed cardiovascular parameters in pediatric CKD patients. The patients were classified according to treatment methods, namely, conservative treatment (PreD), peritoneal dialysis, and hemodialysis. The cardiovascular findings of the patients were identified as functional and morphologic changes.
Measurement of aortic distensibility is shown to be a noninvasive method for early detection of atherosclerosis in adults. Increased stiffness causes an increase in systolic blood and pulse pressures and a decrease in diastolic blood pressure, thereby causing increased left ventricle afterload and altered coronary perfusion [32]. Lacombe et al. [17] demonstrated that S, Ep, and Ep* in subjects are related to atherosclerosis. Arterial stiffness is observed already in the early stages of adult CKD [43].
The few studies investigating stiffness of the aorta in children have found increased aortic stiffness in children receiving hemodialysis [2, 5, 6]. Although carotid stiffness could be used to predict cardiovascular events of patients with ESRD [3], this was less evident for patients with manifest arterial disease [9]. However, the abdominal aorta could be examined more easily than the carotid artery in childhood. In this study, we measured the aorta and calculated the aortic wall strain (S), the stiffness (Ep), and the incremental modulus of elasticity (Ep*), then compared these values in our patients with those in healthy control subjects.
Aortic stiffness was determined for 35 patients (69%) with CKD. We also found that children in both the predialysis and dialysis periods already had significant arterial functional abnormalities and that their S values were lower than in control subjects whereas their Ep* values were greater. However, compared with the predialysis and dialysis groups, the strain and stiffness of the aortic wall were better in the PreD group, but the differences were not statistically significant (P = 0.31 and P = 0.9, respectively).
On the other hand, most of the patients in Pre-D group (n = 15) had aortic stiffness. This result supports the conclusion that functional changes in the cardiovascular system are beginning when kidney function is mildly impaired. Among the dialysis groups, the stiffness of the aortic wall was better in the PD group than in the HD group, but the difference was not statistically significant (P > 0.05). Therefore, the indications and timing of dialysis should be reevaluated, and peritoneal dialysis should be preferred over hemodialysis for children with CKD.
Previous studies have shown that increased stiffness of a large artery usually is associated with older age [15, 33]. Our results demonstrated that arterial abnormalities become apparent even in children at a young age.
Increased c-IMT was first observed in a group of young adults with childhood-onset, end-stage renal disease and found to be correlated negatively with glomerular filtration rate [22, 24, 33]. The findings showed that IMT is already increased in children with stage 2 CKD [23] and that young adults who experienced CKD in childhood had increased carotid IMT compared with a healthy control group [33].
In our study, the mean age-related IMT values were significantly higher in the patients than in the control subjects (P = 0.01). The PreD patients had higher values of cIMT than the PD and HD groups (P > 0.05). In the PreD group, c-IMT correlated positively with systolic blood pressure and cholesterol but not with gender or duration of disease. In the PreD period, 17 of 20 patients presented with increased c-IMT values, especially patients with stage 2 CKD. These findings showed that CVD appears at an early stage for CKD patients and can be prevented with RRT.
Two comparable studies investigated young adults receiving dialysis treatment who had experienced childhood-onset ESRD and adults who had undergone renal transplantation. The findings showed significantly elevated and normal IMT values of the carotid artery compared with age- and gender-matched controls, respectively [30, 33]. Litwin et al. [24] investigated IMT and vascular structure in pediatric CKD patients receiving conservative treatment or dialysis and in patients who had undergone renal transplantation. The authors observed increased mean IMT values in all the patient groups, with the most marked changes in the dialysis patients. In the current study, the c-IMT values among dialysis patients were lower in the PD group (0.5 ± 0.13) than in the HD group (0.52 ± 0.19) (P = 0.71).
Because symptomatic CVD is rare in children, the focus of research has been on identifying it in children with CKD early markers or intermediate cardiovascular outcomes. Echocardiographically detected abnormalities of the left ventricle such as LVH have been accepted as early markers of cardiomyopathy [36]. One-third of adults with preterminal CKD have LVH, and its frequency increases with worsening of dialysis [11, 12, 21]. Prior studies have shown that about one-third of children with CKD have an increased LVMI [16, 25]. The mean LVMI was significantly increased in CKD patients, and 50% of the patients showed LVH. In 31% of patients, significant LVH must be considered.
Recently, a correlation between LVH and hypertension in pediatric CKD patients has been shown [30]. Mitsnefes et al. [29] showed that 31% of patients with CKD (stages 2 to 4) had a significant increase in LVMI, with LVH developing in many of the children. Also, Chavers and Herzog [4] reported a 70% prevalence of LVH among stage 5 CKD patients. At initiation of maintenance dialysis, 69–82% of pediatric patients had evidence of LVH [28, 41]. In addition, 70–90% of patients had LVH during dialysis treatment [35].
Continuous ambulatory peritoneal dialysis (CAPD) often leads to better control of hypertension, a higher intake of calories, and less anemia than hemodialysis. In addition, continuous dialysis treatment provides good clearance of uremic toxins. Alpert et al. [1] showed that mean blood pressure, left ventricle end systolic and diastolic volumes, left ventricle stroke index, and cardiac index were significantly lower and the mean velocity of LV circumferential fiber shortening significantly higher in CAPD patients than in HD patients. Also, Leenen et al. [18] showed that left ventricle systolic function returned to normal in patients undergoing CAPD for CKD.
Left ventricular hypertrophy was found in 31 the study patients (13 PreD, 4 PD, and 14 HD patients). Also, we determined that 24 (77.4%) of the 31 patients had hypertension. In all the patient groups, LVMI was found to be correlated with systolic blood pressure (r = 0.54; P = 0.00), pulse pressure (r = 0.45; P = 0.003), BMI (r = 0.40; P = 0.009), and age (r = 0.67; P = 0.00), but not with male gender (P = 0.39).
In the predialysis period, 13 (65%) of 20 patients had hypertrophy of the left ventricle. However, we observed that the LVMI and LVEDD values were significantly higher in the HD group (P = 0.03) than in the PD or PreD group (P = 0.02). The patients receiving hemodialysis appeared to have a higher prevalence of LVMI and LVH (82.3%) than the patients receiving peritoneal dialysis (40%). This is possibility related to poorer blood pressure control. These results suggest that morphologic changes occur in patients with early-stage CKD and that dialysis should be maintained with these patients.
In conclusion, functional and morphologic abnormalities were found to be greater in patients with CKD than in control subjects. Functional changes were determined to be fewer in patients with early-stage CKD (PreD patients) than in dialysis patients. In contrast, c-IMT values were found to be higher in the PreD group than in the other groups. We also found that most of the PreD patients had LVH. In the dialysis groups, either functional or morphologic abnormalities were found to be fewer in patients receiving peritoneal dialysis. Therefore, the indications and timing of dialysis should be reevaluated, and peritoneal dialysis should be preferred over hemodialysis for children with CKD.
This study was limited by a small number of patients in each group. More research with large populations is required to clarify the reported issue.
References
Alpert MA (1986) Cardiac performance during different renal replacement methods: hemodialysis and continuous ambulatory peritoneal dialysis. Contrib Nephrol 52:86–96
Bakiler AR, Yavascan O, Harputluoglu N, Kara OD, Aksu N (2007) Evaluation of aortic stiffness in children with chronic renal failure. Pediat Nephrol 22:1911–1919
Blacher J, Pannier B, Guerin AP, Marchais SJ, Safar ME, London GM (1998) Carotid arterial stiffness as a predictor of cardiovascular and all-cause mortality in end-stage renal disease. Hypertension 32:570–574
Chavers BM, Herzog CA (2004) The spectrum of cardiovascular disease in children with PreDialysis chronic kidney disease. Adv Chronic Kidney Dis 11:319–327
Covic A, Gusbeth-Tatomir P, Goldsmith DJA (2005) Arterial stiffness in renal patients: an update. Am J Kidney Dis 45:965–977
Covic A, Mardare N, Gusbeth-Tatomir P, Brumaru O, Gavrilovici C, Munteanu M, Prisada O, Goldsmith DJ (2006) Increased arterial stiffness in children on hemodialysis. Nephrol Dial Transplant 21:729–735
Devereux RB, Reichek N (1977) Echocardiographic determination of left ventricular mass in man: anatomic validation of the method. Circulation 55:613–618
De Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Divitiis O, Alderman MH (1992) Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and the impact of overweight. J Am Coll Cardiol 20:1251–1260
Dijk JM, Algra A, van der GY, Grobbee DE, Bots ML (2005) Carotid stiffness and the risk of new vascular events in patients with manifest cardiovascular disease: the SMART study. Eur Heart J 26:1213–1220
Fagot-Campagna A (2000) Emergence of type 2 diabetes mellitus in children: epidemiological evidence. J Pediatr Endocrinol Metab 13(Suppl 6):1395–1402
Foley RN, Parfrey PS, Harnett JD, Kent GM, martin CJ, Murray DC, Barre PE (1995) Clinical and echocardiographic disease in patients starting end-stage renal disease therapy. Kidney Int 47:186–192
Graves SC, Gamble GD, Collins JF, Whalley GA, Sharpe DN (1994) Determinants of left ventricular hypertrophy and systolic dysfunction in chronic renal failure. Am J Kidney Dis 24:768–776
Groothoff JW, Lilien MR, van de Kar NC, Wolff ED, Davin JC (2005) Cardiovascular disease as a late complication of end-stage renal disease in children. Pediatr Nephrol 20:374–379
Guérin AP, London GM, Marchais SJ, Metivier F (2000) Arterial stiffening and vascular calcifications in end-stage renal disease. Nephrol Dial Transpl 15:1014–1021
Hayashi T, Nakayama Y, Tsumura K, Yoshimaru K, Ueda H (2002) Reflection in the arterial system and the risk of coronary heart disease. Am J Hypertens 15:405–409
Johnstone LM, Jones CL, Grigg LE, Wilkinson JL, Walker RG, Powell HR (1996) Left ventricular abnormalities in children, adolescents, and young adults with renal disease. Kidney Int 50:998–1006
Lacombe F, Dart A, Dewar E, Jennings G, Cameron J, Laufer E (1992) Arterial elastic properties in man: a comparison of echo-Doppler indices of aortic stiffness. Eur Heart J 13:1040–1045
Leenen FH, Smith DL, Khanna R, Oreopoulos DG (1985) Changes in left ventricular hypertrophy and function in hypertensive patients started on continuous ambulatory peritoneal dialysis. Am Heart J 110:102–106
Levent E, Goksen D, Ozyurek AR, Darcan S, Coker M (2002) Stiffness of the abdominal aorta in obese children. J Pediatr Endocrinol Metab 15:405–409
Levent E, Ozyurek AR, Ulger Z (2004) Evaluation of aortic stiffness in tobacco-smoking adolescents. J Adolesc Health 34:339–343
Levin A, Thompson CR, Ethier J, Carlisle EJ, Tobe S, Mendelssohn D, Burgess E, Jindal K, Barrett B, Singer J, Djurdjev O (1999) Left ventricular mass index increase in early renal disease: impact of decline in hemoglobin. Am J Kidney Dis 34:125–134
Litwin M, Niemirska A (2009) Intima-media thickness measurements in children with cardiovascular risk factors. Pediatr Nephrol 24:707–719
Litwin M, Wühl E, Jourdan C, Niemirska A, Schenk JP, Jobs K, Grenda R, Wawer ZT, Rajszys P, Mehls O, Schaefer F (2008) Evaluation of large-vessel arteriopathy in pediatric patients with chronic kidney disease. Nephrol Dial Transplant 23:2552–2557
Litwin M, Wühl E, Jourdan C, Trelewicz J, Niemirska A, Fahr K, Jobs K, Grenda R, Wawer ZT, Rajszys P, Troger J, Mehls O, Schaefer F (2005) Altered morphologic properties of large arteries in children with chronic renal failure and after renal transplantation. J Am Soc Nephrol 16:1494–1500
Matteucci MC, Wuhl E, Picca S, Mastrostefano A, Rinelli G, Romano C, Rizzoni G, Mehls O, de Simone G, Schaefer F, ESCAPE Trial Group (2006) Left ventricular geometry in children with mild to moderate chronic renal insufficiency. J Am Soc Nephrol 17:218–226
Mitsnefes MM (2005) Cardiovascular morbidity and mortality in children with chronic kidney disease in North America: lessons from the USRDS and NAPRTCS databases. Perit Dial Int 25(Suppl 3):120–122
Mitsnefes MM (2008) Cardiovascular complications of pediatric chronic kidney disease. Pediatr Nephrol 23:27–39
Mitsnefes MM, Daniel SR, Scwartz SM, Khoury P, Strife CF (2001) Changes in left ventricular mass in children and adolescent during chronic dialysis. Pediatr Nephrol 16:318–323
Mitsnefes MM, Kimball TR, Kartal J, Witt SA, Glascock BJ, Khoury PR, Daniels S (2006) Progression of left ventricular hypertrophy in children with early chronic kidney disease: 2-year follow-up study. J Pediatr 149:671–675
Mitsnefes MM, Kimball TR, Kartal J, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2005) Cardiac and vascular adaptation in pediatric patients with chronic kidney disease: role of calcium-phosphorus metabolism. J Am Soc Nephrol 16:2796–2803
Mitsnefes MM, Kimball TR, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2003) Left ventricular mass and systolic performance in pediatric patients with chronic renal failure. Circulation 107:864–868
Nichols WW, O’Rourke MF (1998) Vascular impedance. In: McDonalds’s blood flow in arteries: theoretical, experimental, and clinical principles. 4th edn. Edward Arnold, London, UK, pp 243–293
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Qerfeld U, Mels O, Schaefer F (2002) Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation 106:100–105
Okubo M, Ino T, Tkahashi K, Kishiro M, Akimoto K, Yamashiro Y (2001) Age dependency of stiffness of the abdominal aorta and the mechanical properties of the aorta in Kawasaki disease in children. Pediatr Cardiol 22:198–203
Palcoux JB, Palcoux MC, Jouan JP, Gourgand JM, Cassagness J, Malpuech G (1982) Echocardiographic patterns in infants and children with chronic renal failure. Int J Pediatr Nephrol 3:311–314
Querfeld U, Mitsnefes M (2008) Cardiovascular disease in pediatric chronic kidney disease. In: Geary DF, Schaefer F (eds) Comprehensive pediatric nephrology, 1st edn. Mosby, Philadelphia, pp 793–810
Robinson RF, Nahata MC, Sparks E, Daniels C, Batisky DL, Hayes JR, Mahan JD (2005) Abnormal left ventricular mass and aortic strain in pediatric dialysis patients. Pediatr Nephrol 20:64–68
Ross R (1999) Atherosclerosis: an inflammatory disease. N Engl J Med 340:115–116
Rucker R, Tonelli M (2009) Cardiovascular risk and management in chronic kidney disease. Nat Rev Nephrol 5:287–296
Staruss RS, Pollack HA (2001) Epidemic increase in childhood overweight, 1986–1998. JAMA 286:2845–2848
Ulinski T, Genty J, Viau C, Tillous-Borde I, Deschenes G (2006) Reduction of left ventricular hypertrophy in children undergoing hemodialysis. Pediatr Nephrol 21:1171–1178
Urbina EM, Williams RV, Alpert BS, Collins RT, Daniels SR, Hayman L, Jacobson M, Mahoney L, Mietus-Snyder M, Rocchini A, Steinberger J, McCrindle B, American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young (2009) Noninvasive assessment of subclinical atherosclerosis in children and adolescent: recommendations for standard assessment for clinical research: a scientific statement from the American Heart Association. Hypertension 54:919–950
Wang MC, Tsai WC, Chen JY, Huang JJ (2005) Stepwise increase in arterial stiffness corresponding with the stages of chronic kidney disease. Am J Kidney Dis 45:494–501
Weiner DE, Tighiouart H, Amin MG, Stark PC, Macleod B, Griffith JL, Salem DN, Levey AS, Sarnak MJ (2004) Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: a pooled analysis of community-based studies. J Am Soc Nephrol 15:1307–1315
Wessels S, Amman K, Toring J, Ritz E (1999) Cardiovascular structural changes in uremia: implications for cardiovascular function. Semin Dial 12:288–292
Wong CS, Gipson DS, Gillen DL, Emerson S, Koepsell T, Sherrard DJ, Watkins SL, Stehman-Breen C (2000) Anthropometric measures and risk of death in children with end-stage renal disease. Am J Kidney Dis 36:811–819
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sozeri, B., Mir, S., Kara, O.D. et al. When Does the Cardiovascular Disease Appear in Patients With Chronic Kidney Disease?. Pediatr Cardiol 31, 821–828 (2010). https://doi.org/10.1007/s00246-010-9710-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-010-9710-0