Abstract
Background
Uremic vasculopathy, including vascular calcification, increases the risk for cardiovascular disease and mortality in chronic kidney disease (CKD) patients. We have investigated the prevalence and factors associated with vasculopathy in children undergoing peritoneal dialysis (PD) or hemodialysis (HD) in a single center.
Methods
Common carotid intima media thickness (cIMT) and its relation with demographics, biochemical parameters and medication was analyzed in 60 patients (mean age 12.9 ± 3.4 years; 27 girls) treated with PD (n = 31) or HD (n = 29) for 34 ± 34 months. Patients were divided into two groups: normal cIMT and increased cIMT.
Results
Mean levels of calcium, phosphate and calcium/phosphate product were in the normal range, the but parathyroid hormone level, 729 ± 670 pg/mL, was higher than the National Kidney Foundation Kidney Disease Outcome Quality Iniative (K/DOQI) recommendations. Twenty-nine patients had increased cIMT, which was associated with time on dialysis of >2 years, hypercalcemia, higher daily dose of calcitriol and HD (vs. PD). In the multivariate analysis, accounting for time on dialysis, HD persisted as a risk for increased cIMT.
Conclusions
The prevalence of increased cIMT in children on dialysis is similar to that reported in adults with CKD and increased with time on dialysis. HD was associated with increased cIMT, independently of time on dialysis; however, the results should be interpreted with caution due to the possible impact of confounding factors. These results underline the need to monitor and, if possible, prevent and treat increased cIMT in children on dialysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several studies in children with chronic kidney disease (CKD) have shown a considerable and consistent association between mineral and bone metabolism disorders, including abnormal levels of calcium (Ca), phosphorous (PO4), vitamin D and parathyroid hormone (PTH), and deteriorating measures of vascular function [1–8]. These alterations occur early in the course of CKD, and some therapies designed to treat these disorders can further affect the progression of vascular pathology [9–11]. These conditions are important risk factors for the development of vascular calcification (VC) and cardiovascular disease (CVD). CVD is the leading cause of morbidity and mortality in both adults and children with CKD [12–16].
Among the factors contributing to CVD in CKD are the traditional risk factors, especially hypertension which is present in 50–75 % of pediatric patients with CKD [17]. In this group of patients, other traditional risk factors, such as dyslipidemia, insulin resistance, obesity and malnutrition, are less frequent [18]. However, uremia-related factors, such as dysregulation of the Ca–PO4–PTH and vitamin D axis are common and thought to increase carotid intima-media thickness (cIMT) [1–6], vascular stiffness [6, 7, 19], coronary calcification [2, 3, 5, 6] and left ventricular mass [20]. CKD patients have a net positive Ca balance as a result of iatrogenic Ca loading from Ca-based phosphate binders, vitamin D therapy and, in dialysis patients, Ca absorbed from the dialysate. Vascular calcification has been found to be associated with the use of calcium-containing phosphate binders and calcitriol [1,25-dihydroxycholecalciferol, 1,25(OH)2D] [1, 2, 6, 21], as well as with longer time on dialysis, older age, and high Ca × PO4 product [2, 3, 5]. In addition to its systemic effects on Ca and PO4 homeostasis, PTH has a direct action on vascular smooth muscle cells and cardiac fibroblasts, causing arteriolar thickening and myocardial fibrosis, respectively [18, 22]. The use of vitamin D analogs to treat secondary hyperparathyroidism can result in high circulating levels of 1,25(OH)2D, and pediatric studies have consistently shown that a high vitamin D dose adversely affects cIMT and calcification [23–25]. Fibroblast growth factor 23 is a potent phosphaturic hormone that increases the rate of urinary excretion of phosphate and inhibits renal production of 1,25(OH)2D and helps to mitigate hyperphosphatemia in CKD patients; high levels of FGF-23 have been found in children with CKD stage 3 and 4 [26]. Inflammation and oxidative stress are common findings in CKD patients and are associated with increased atherosclerosis and cardiovascular morbidity and mortality [27, 28].
New drugs, such as non-calcium-based phosphate binders, other vitamin D analogues and calcimimetics may be better choices for the treatment of mineral disorders present in CKD patients and may possibly attenuate the progression of the vascular complications [9, 29]; however, in Mexico these drugs are not generally available. The aim of this study was to investigate the prevalence and factors associated with vasculopathy, as measured by cIMT, in children with CKD treated with peritoneal dialysis (PD) or hemodialysis (HD).
Material and methods
A cross-sectional study of prevalence and factors associated with uremic vasculopathy in children was performed in a single center and included all patients under the age of 17 years who had been treated with PD or HD for at least 6 months between February 2008 to October 2008. From the files of these patients we collected information on demographics, previous and current renal replacement therapy (RRT), serum values for albumin, Ca, PO4, hemoglobin, alkaline phosphatase and intact PTH (iPTH; measured by radioimmunoanalysis; Diagnostic Systems, Webster, TX), as well as daily doses of calcium carbonate and calcitriol (1,25(OH)2D). The corrected calcium level was calculated using the following formula: [(4 − albumin) (0.8) + serum Ca]; the Ca × PO4 product was also calculated. The average laboratory values from the last 6 or 12 months for those patients who were on dialysis for more than 1 year were taken into account.
The patients were investigated using an M-mode ultrasound (US) with a 7.5-MHz linear transductor (Aloka SSD-1700 DynaView instrument; Hitachi Aloka Medical Ltd, Tokyo, Japan). A single well-trained person performed the US scanning. After at least 10 min of rest, with the patients in a supine position and the neck hyper-extended and rotated, the cIMT was explored at 10 mm from the bifurcation in the right and left common carotid arteries; intima-media thickness was also explored in both abdominal aorta (10 cm) and in iliac arteries after their bifurcation until the inguinal ligament. All of the arteries were explored longitudinally and transversally to identify the presence of plaques. cIMT was classified as normal or increased according to the normative values for cIMT in pediatric populations suggested by Jourdan et al. [30].
Statistical analysis
For the descriptive statistics, the frequencies and percentages of the variables were calculated. Patients were divided into two groups: normal cIMT and increased cIMT, and the percentage and the means were compared with chi-square and Student´s t-test respectively. For the factors associated with vascular calcification, an odds ratio (OR) was calculated. Patients were stratified according to the total time on RRT and on current therapy (PD or HD) respectively. A multivariate post-hoc analysis was performed to identify if modality was an independent factor for increased cIMT, i.e. not related to time on RRT.
Results
Demographics
Among the 88 patients on dialysis eligible for enrollment in the study, all the measurements required for participation were available for only 60 patients, who were then included in the study. Of these 60 patients, 27 (45 %) were girls, the age range was 2–16 years; 42 (70 %) of the patients were between 13 and 16 years old. The etiology of CKD was: chronic glomerulonephritis (52 %), obstructive uropathy (25 %), renal hypoplasia/dysplasia (10 %), familial nephritis (7 %), and others (6 %). Eleven patients had undergone kidney transplantation before being included in the study. Thirty-one patients were on PD and 29 on HD at the time of the investigation, with a median of 22 months of PD/HD treatment (range 6–156 months, mean 34 ± 34 months) dialysis. Twenty-six patients had been only on PD and six only on HD.
Laboratory parameters
Among the 60 patients, hypoalbuminemia was present in 18 %, anemia with hemoglobin below the National Kidney Foundation Kidney Disease Outcome Quality Initiative (K/DOQI) recommendation in 93 % (Table 1), hypertriglyceridemia in 82 % and hypercholesterolemia in 23 %. Ca–PO4 metabolism was evaluated by obtaining the average of Ca and PO4 and calculating the Ca × PO4 product during the 6 months (for incident) or 12 months (for prevalent patients) prior to the study. The mean corrected Ca for all patients was 9.1 ± 0.7 mg/dL; however, when dividing the results according to the K/DOQI guideline recommendation [31] we found that 50 % of the patients were in normal range (9.5–10.2 mg/dL), 42 % had low levels and 8 % had high levels (Table 1). PO4 was 5.6 ± 1.0 mg/dL and the Ca × PO4 product 50.3 ± 10.3 mg2/dL2. Levels of PO4 and Ca × PO4 product were higher than the recommended values in 80 and 31 % of the patients, respectively [31]. Intact PTH (n = 56) was 729 ± 670 pg/mL; 70 % of the patients had secondary hyperparathyroidism (iPTH ≥300 pg/mL [31]) and 54 % had severe hyperparathyroidism (iPTH ≥500 pg/mL).
The average dose of calcium carbonate was 5.4 ± 3. 0 g/day, and the dose was higher than the recommended dose (<2.5 g/day) in 65 % of the patients (Table 1). The average dose of calcitriol was 0.33 ± 0.31 μg/day.
There were no significant differences in the levels of Ca, PO4, iPTH, Ca × PO4 product or the intake of calcium carbonate and calcitriol between PD and HD patients (Table 2).
Intima-media thickness
Thirty-one patients (52 %) had normal cIMT, and 29 (48 %) patients had an increased cIMT. Among the 11 children with a previous kidney transplant, seven had increased cIMT. IMT in the aorta was increased only in two patients with increased cIMT. Iliac artery IMT was normal in all patients. (Note: the results of IMT were reported as categorical variables; i.e. as normal cIMT or increased cIMT; therefore, we are unable to report them as continuous variables).
Factors associated with increased cIMT
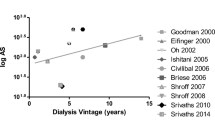
Patients were divided into two groups: normal cIMT and increased cIMT (Table 3). There were no statistically significant differences in age, gender or etiology of CKD between the two groups. Of the patients with increased cIMT, 80 % were on HD and 20 % were on PD (p < 0.001). The total time on RRT was significantly higher in the group with increased cIMT [42 vs. 26 months (normal cIMT); p = 0.027]. The prevalence of increased cIMT in patients who had been on dialysis for 1 year was 46 %, and increased to 60 % in the second year of dialysis, 57 % the third year, and 66 % after the fourth year. Chi-square analysis for trends showed that the risk for changes to cIMT increased over time [odds ratio (OR) 4.47; p = 0.03].
Increased cIMT was not associated with albumin values, PO4 >6 mg/dL, Ca × PO4 >57.4 mg2/dL2, PTH >500 pg/mL or daily calcium carbonate intake (Table 5).
Of the patients with increased cIMT, 72 % had abnormal Ca compared and 39 % had normal cIMT [OR 4.1, 95 % confidence interval (CI) 1.3–12.3, p = 0.009] (Table 4). Increased cIMT was associated with higher doses of calcitriol (OR 2.1, 95 % CI 1.6–2.9; p = 0.06).
Patients with hemoglobin of <9.2 g/dL had a higher risk for increased cIMT (OR 4.7, 95 % CI 1.56–14.13; p = 0.009) (Table 5).
Patients on HD had a higher risk for increased cIMT than those on PD (OR 15.97, 95 % CI 4.5–56.6; p < 0.0001) (Table 5). Considering that in our unit, as in most pediatric units, the first therapy of choice is PD, and that patients on HD in general had been transferred to this therapy after experiencing some problems with PD, one can assume that the total time on dialysis was higher among the HD patients. To account for this confounding factor as well as other confounding factors which could be linked to time on dialysis and dialysis modality, we performed three additional sub-analyses. However, due to the low number of patients in the different subgroups, the results below should be interpreted with caution.
First, we calculated the risk for increased cIMT in patients who had been on dialysis for <2 years (HD, n = 10; PD, n = 3). This analysis showed that HD was associated with increased risk (OR 15, 95 % CI 2.7–80.6). We then compared patients who had been on dialysis for >2 years (HD, n = 13; PD, n = 3); the risk associated with HD versus that with PD was similar to that in the first subanalysis (OR 15.1, 95 % CI 2.0–113.3). Whereas the number of patients on PD was much smaller than those on HD, these findings suggest an association of HD with an increased risk for increased cIMT, both in patients with <2 years or >2 years of dialysis treatment.
The analysis above did not take into consideration whether the patients had been on a different therapy before the current one; therefore, in the second sub-analysis, we included patients who had been on the same therapy all the time. This group comprised 32 patients, 26 on PD and six on HD. Increased cIMT was present in four (15 %) patients on PD and in five (83 %) patients on HD (p = 0.001). Again, there was an increased risk in the HD group (OR 27.5, 95 % CI 2.5–302).
Finally, in a multivariate analysis including both hypercalcemia and total time on RRT, the risk for increased cIMT in patients treated with HD remained at the same high level (OR 14.9, 95 % CI 1.3–164.1) (Table 5). For hypercalcemia, we used the Haldane method because there were no patients on PD with hypercalcemia; the four patients who had hypercalcemia were all on HD and had a higher risk for increased cIMT than those patients with normal Ca for age (OR 20.6 Haldane method, p = 0.016, Fisher’s exact test).
Discussion
In the general population, the prevalence of vascular calcification (VC) is determined by age and comorbidities and may also vary depending on exploration method and the explored site. Whereas VC has not been described in healthy subjects under the age of 20 years, it is present in up to 5 % of young adults (20–30 years old) [3], and in up to 11 % of subjects aged 30–40 years [32]. In CKD patients, the prevalence of VC has been reported to be 15–64 % in teenagers [2, 3, 33], 87 % in adults between 20 and 30 years [3], and 50–66 % in patients older than 30 years [32, 34]. In our study, increased cIMT was present in 48 % of the children who had been on dialysis for an average 34 of months, and the prevalence was as high as 66 % in the patients who had been on dialysis for more than 4 years.
Key factors in preventing mineral dysregulation include the prevention of hyperphosphatemia and maintenance of adequate levels of vitamin D so that the normal control mechanisms of the parathyroid glands are maintained and hyperparathyroidism does not develop [35]. Administration of phosphate binder and vitamin D supplementation are recommended if levels of 25-hydroxyvitamin D are low or hypocalcemia develops. Unfortunately, in our unit, we do not have access to measurements of vitamin D levels, and sometimes we cannot measure iPTH regularly; therefore, it is not easy to adjust doses of calcium-based phosphate binder or calcitriol.
The time on dialysis has been identified as the principal risk factor for vascular dysfunction. The presence of VC in children with CKD, which in different reports varies from 15 to 87 %, has a strong association with the duration of dialysis treatment [1–6]. In our study, patients with increased cIMT had been on dialysis for >2 years (OR 3; 95 % CI 1.03–8.73), and the risk was even higher in patients after 48 months on dialysis (OR 4.51; 95 % CI 1.01–20.1).
Thickening and stiffness of the vessel wall have both been associated with abnormal levels of calcium, phosphorus [1–5, 7, 23, 25, 36], and PTH [1, 2, 5, 6], as have therapeutic dosages of calcium-based phosphate binders and vitamin D compounds [2, 3, 6, 7, 11, 23, 33].
Dialysis patients may have a positive Ca balance as a result of several factors, including the uptake of Ca from the dialysate, oral intake of Ca with the diet, use of Ca-based phosphate binders, and vitamin D therapy [1, 29, 31, 37] and reduced or absent Ca removal via the kidneys [18]. In this study, Ca levels higher than the recommended levels (>10.2 mg/dL)[31] were associated with increased cIMT (Table 5).
Hyperphosphatemia was present in 67 % of the patients; however, this was not associated with increased cIMT. One explanation could be that the serum PO4 level was, on average, not higher than values reported by other groups [2, 11, 32, 38].
Secondary hyperparathyroidism (sHPT) is a frequent complication in children with CKD [39]. In our study, sHPT was present in 70 % of the patients, and 54 % of these patients had severe sHTP, i.e. iPTH >500 pg/mL. There was, however, no linear association between sHTP and the presence of increased cIMT, which is in agreement with previously reported results [3, 33, 34, 40].
In general, our patients received daily doses of calcium carbonate that were higher than the recommended doses [31], but Ca intake was not associated with increased cIMT. There are several reports [2, 11, 33] of children who received higher doses of calcitriol having a higher risk for increased cIMT; the results of our study are in agreement with these earlier studies (OR 2.19; 95 % CI 1.65–2.91). In pediatric patients with CKD, several studies have noted an association between the cumulative doses of calcium-based phosphate binders and calcitriol with the presence of vasculopathy [3, 4, 6, 36]. Unfortunately, we do not have this information in our patients, who usually come to us at a late stage, when dialysis is needed, after previously receiving calcium-based phosphate binders and calcitriol for different time periods.
The modality of RRT has previously been reported to be associated to VC. A recent publication showed that pediatric PD patients had fewer cardiovascular abnormalities, either functional or morphologic, than pediatric HD patients [41]. Civilbal et al. reported that the presence of coronary artery calcification in 15 % of children on PD/HD and following a kidney transplant was strongly associated with time on dialysis and tended to be higher in patients on HD than in those treated with PD or having had a renal transplant, but this difference was not statistically significant [2].
In our study, patients on HD had a higher risk of increased cIMT (OR 15.97; 95 % CI 4.5–56.6). Children on HD are generally those who for various reasons require discontinuation of PD. As this latter group of patients could have had CKD, or had been on dialysis therapy for a longer period time, and were probably sicker, the association between cIMT and HD found in our study could have been confounded by these conditions. Therefore, we also analyzed patients who had been on the same dialysis modality all the time separately (see Results section). The prevalence of a Ca level higher than that recommended was significantly higher in those children who were on HD and had increased cIMT (OR 27.5, 95 % CI 2.5–302). When we adjusted both for hypercalcemia and time on RRT, the risk of HD still remained higher (OR 14.9, 95 % CI 1.3–164.1) compared to the risk with PD. To the best of our knowledge, this is the first report of the modality of dialysis appearing to be closely associated with increased cIMT.
Possible reasons why HD is associated with increased cIMT could be: (1) exposure to hemodynamic changes during the treatment and (2) induction of inflammatory substances by the dialysis procedure, i.e. high levels of C-reactive protein [9, 34] and homocysteine [9, 34]. Elevated levels of homocysteine have also been associated with endothelial dysfunction, increased intima media thickness and left ventricular hypertrophy in children [23, 28]. Chronic inflammation is common in CKD patients and may cause malnutrition and progressive CVD by several pathological mechanisms [28, 42, 43]. Finally, the residual renal function is better preserved in PD and can help to maintain elimination of β2 microglobulin and homocysteine, among other molecules.
Several limitations of the study should be noted. This is a cross-sectional study of patients who had been dialyzed for relatively short time periods prior to the study and the time of appearance of changes in the cIMT is not known. Moreover, the results of IMT were reported as a categorical variable and, therefore, we could not present them as a continuous variable. Due to the cross-sectional design, causal relationships cannot be established. We were not able to retrieve information on the cumulative doses of calcium-containing oral phosphate binders and calcitriol, and we did not measure several other relevant molecules, such as inflammatory markers and promoters and inhibitors of VC. Finally, the US method used to measure cIMT is not the best method for assessing vascular calcification and, therefore, conclusions regarding vascular calcification cannot be made. Nevertheless, we believe that this report provides valuable new information about the high prevalence of uremic vasculopathy in the pediatric dialysis population that will hopefully stimulate the design of new studies and possibly new regimens for follow-up, treatment and prevention of factors linked to vasculopathy in pediatric dialysis patients.
In summary, the prevalence of uremic vasculopathy among this group of dialyzed Mexican children was found to be very high: 48–66 % depending on the time on dialysis therapy. The identified factors associated to increased cIMT were time on dialysis >2 years, high daily dose of calcitriol and exposure to HD treatment. Whereas the method used to measure IMT, namely, M-mode US, has limitations, it is not expensive, does not require exposure to contrast, radiation or sedation and it is available in most hospitals. Based on these results, it seems prudent to recommend that carotid artery investigation, or other types of investigations which could reveal vasculopathy, should be performed in children at the start of dialysis with annual or bi-annual follow-up thereafter.
References
Mitsnefes MM, Kimball TR, Kartal J, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2005) Cardiac and vascular adaptation in pediatric patients with chronic kidney disease: role of calcium-phosphorus metabolism. J Am Soc Nephrol 16:2796–2803
Civilibal M, Caliskan S, Adaletli I, Oflaz H, Sever L, Candan C, Canpolat N, Kasapcopur O, Kuruoglu S, Arisoy N (2006) Coronary artery calcifications in children with end-stage renal disease. Pediatr Nephrol 21:1426–1433
Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D, Wang Y, Chung J, Emerick A, Greaser L, Elashoff RM, Salusky IB (2000) Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med 342:1478–1483
Litwin M, Wuhl E, Jourdan C, Trelewicz J, Niemirska A, Fahr K, Jobs K, Grenda R, Wawer ZT, Rajszys P, Troger J, Mehls O, Schaefer F (2005) Altered morphologic properties of large arteries in children with chronic renal failure and after renal transplantation. J Am Soc Nephrol 16:1494–1500
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, Mehls O, Schaefer F (2002) Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation 106:100–105
Shroff RC, Donald AE, Hiorns MP, Watson A, Feather S, Milford D, Ellins EA, Storry C, Ridout D, Deanfield J, Rees L (2007) Mineral metabolism and vascular damage in children on dialysis. J Am Soc Nephrol 18:2996–3003
Covic A, Mardare N, Gusbeth-Tatomir P, Brumaru O, Gavrilovici C, Munteanu M, Prisada O, Goldsmith DJ (2006) Increased arterial stiffness in children on haemodialysis. Nephrol Dial Transplant 21:729–735
Wesseling K, Bakkaloglu S, Salusky I (2008) Chronic kidney disease mineral and bone disorder in children. Pediatr Nephrol 23:195–207
Querfeld U (2004) The clinical significance of vascular calcification in young patients with end-stage renal disease. Pediatr Nephrol 19:478–484
Moe SM, Chen NX (2003) Calciphylaxis and vascular calcification: a continuum of extra-skeletal osteogenesis. Pediatr Nephrol 18:969–975
Sheth RD, Perez MD, Goldstein SL (2003) Cardiovascular calcifications in pediatric patients receiving maintenance dialysis. Pediatr Nephrol 18:810–813
Foley RN, Parfrey PS, Sarnak MJ (1998) Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis 32:S112–S119
McDonald SP, Craig JC (2004) Long-term survival of children with end-stage renal disease. N Engl J Med 350:2654–2662
Parekh RS, Carroll CE, Wolfe RA, Port FK (2002) Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr 141:191–197
Lilien MR, Groothoff JW (2009) Cardiovascular disease in children with CKD or ESRD. Nat Rev Nephrol 5:229–235
Groothoff JW, Gruppen MP, Offringa M, Hutten J, Lilien MR, Van De Kar NJ, Wolff ED, Davin JC, Heymans HS (2002) Mortality and causes of death of end-stage renal disease in children: a Dutch cohort study. Kidney Int 61:621–629
Mitsnefes M, Stablein D (2005) Hypertension in pediatric patients on long-term dialysis: a report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS). Am J Kidney Dis 45:309–315
Shroff R, Quinlan C, Mitsnefes M (2011) Uraemic vasculopathy in children with chronic kidney disease: prevention or damage limitation? Pediatr Nephrol 26:853–865
Kis E, Cseprekal O, Biro E, Kelen K, Ferenczi D, Kerti A, Szabo AJ, Szabo A, Reusz GS (2009) Effects of bone and mineral metabolism on arterial elasticity in chronic renal failure. Pediatr Nephrol 24:2413–2420
Saab G, Whooley MA, Schiller NB, Ix JH (2010) Association of serum phosphorus with left ventricular mass in men and women with stable cardiovascular disease: data from the Heart and Soul Study. Am J Kidney Dis 56:496–505
Milliner DS, Zinsmeister AR, Lieberman E, Landing B (1990) Soft tissue calcification in pediatric patients with end-stage renal disease. Kidney Int 38:931–936
Rostand SG, Drüeke TB (1999) Parathyroid hormone, vitamin D, and cardiovascular disease in chronic renal failure. Kidney Int 56:383–392
Civilibal M, Caliskan S, Oflaz H, Sever L, Candan C, Canpolat N, Kasapcopur O, Bugra Z, Arisoy N (2007) Traditional and "new" cardiovascular risk markers and factors in pediatric dialysis patients. Pediatr Nephrol 22:1021–1029
Litwin M, Wühl E, Jourdan C, Niemirska A, Schenk JP, Jobs K, Grenda R, Wawer ZT, Rajszys P, Mehls O, Schaefer F (2008) Evolution of large-vessel arteriopathy in paediatric patients with chronic kidney disease. Nephrol Dial Transplant 23:2552–2557
Shroff R, Egerton M, Bridel M, Shah V, Donald AE, Cole TJ, Hiorns MP, Deanfield JE, Rees L (2008) A bimodal association of vitamin D levels and vascular disease in children on dialysis. J Am Soc Nephrol 19:1239–1246
van Husen M, Fischer AK, Lehnhardt A, Klaassen I, Möller K, Müller-Wiefel DE, Kemper MJ (2010) Fibroblast growth factor 23 and bone metabolism in children with chronic kidney disease. Kidney Int 78:200–206
Pecoits-Filho R, Sylvestre LC, Stenvinkel P (2005) Chronic kidney disease and inflammation in pediatric patients: from bench to playground. Pediatr Nephrol 20:714–720
Bakkaloglu SA, Saygili A, Sever L, Noyan A, Akman S, Ekim M, Aksu N, Doganay B, Yildiz N, Duzova A, Soylu A, Alpay H, Sonmez F, Civilibal M, Erdem S, Kardelen F (2009) Assessment of cardiovascular risk in paediatric peritoneal dialysis patients: a Turkish Pediatric Peritoneal Dialysis Study Group (TUPEPD) report. Nephrol Dial Transplant 24:3525–3532
Cunningham J (2004) Achieving therapeutic targets in the treatment of secondary hyperparathyroidism. Nephrol Dial Transplant 19[Suppl 5]:V9–V14
Jourdan C, Wühl E, Litwin M, Fahr K, Trelewicz J, Jobs K, Schenk JP, Grenda R, Mehls O, Tröger J, Schaefer F (2005) Normative values for intima-media thickness and distensibility of large arteries in healthy adolescents. J Hypertens 23:1707–1715
National Kidney Foundation (2005) K/DOQI Clinical practice guidelines for bone metabolism and disease in children with chronic kidney cisease. Am J Kidney Dis 46[Suppl 1]:S1-S122
Savage T, Clarke AL, Giles M, Tomson CR, Raine AE (1998) Calcified plaque is common in the carotid and femoral arteries of dialysis patients without clinical vascular disease. Nephrol Dial Transplant 13:2004–2012
Lumpaopong A, Mathew AV, John E, Jelnin V, Benedetti E, Testa G, Oberholzer J, Sankary H, Ruiz C (2007) Early coronary calcification in children and young adults with end-stage renal disease. Transplant Proc 39:37–39
Guerin AP, London GM, Marchais SJ, Metivier F (2000) Arterial stiffening and vascular calcifications in end-stage renal disease. Nephrol Dial Transplant 15:1014–1021
Rees L (2008) What parathyroid hormone levels should we aim for in children with stage 5 chronic kidney disease; what is the evidence? Pediatr Nephrol 23:179–184
Briese S, Wiesner S, Will JC, Lembcke A, Opgen-Rhein B, Nissel R, Wernecke KD, Andreae J, Haffner D, Querfeld U (2006) Arterial and cardiac disease in young adults with childhood-onset end-stage renal disease-impact of calcium and vitamin D therapy. Nephrol Dial Transplant 21:1906–1914
K/DOQI Workgroup (2005) K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis 45:S1-153
Takebayashi S, Hidai H, Chiba T, Takagi Y, Nagatani Y, Matsubara S (1999) Hyperfunctional parathyroid glands with 99mTc-MIBI scan: semiquantitative analysis correlated with histologic findings. J Nucl Med 40:1792–1797
Evenepoel P, Claes K, Kuypers D, Maes B, Bammens B, Vanrenterghem Y (2004) Natural history of parathyroid function and calcium metabolism after kidney transplantation: a single-centre study. Nephrol Dial Transplant 19:1281–1287
Penalba A, Neme G, Tirado S (2003) Vascular and tissue calcifications of hemodialysis patients. Nefrologia 23[Suppl 2]:112–116
Sozeri B, Mir S, Kara OD, Levent E (2010) When does the cardiovascular disease appear in patients with chronic kidney disease? Pediatr Cardiol 31:821–828
Stenvinkel P, Heimburger O, Paultre F, Diczfalusy U, Wang T, Berglund L, Jogestrand T (1999) Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int 55:1899–1911
Aguilera A, Sanchez-Tomero JA, Bajo MA, Ruiz-Caravaca ML, Alvarez V, del Peso G, Herranz A, Cuesta MV, Castro MJ, Selgas R (2003) Malnutrition-inflammation syndrome is associated with endothelial dysfunction in peritoneal dialysis patients. Adv Perit Dial 19:240–245
Acknowledgement
We would like to thank the patients and personnel involved in the creation of these cohorts. Baxter Novum is the result of a grant to the Karolinska Institute from Baxter Healthcare Corporation. Bengt Lindholm is employed by Baxter Healthcare Corporation. None of the other authors declare any conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chavarria, L.A., Aguilar-Kitsu, A., Rosas, P. et al. Intima media thickness in children undergoing dialysis. Pediatr Nephrol 27, 1557–1564 (2012). https://doi.org/10.1007/s00467-012-2173-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-012-2173-1