Abstract
The aim of this retrospective study was to investigate if the application of chlorhexidine-based solutions (ChloraPrep®) to the exit site and the hub of long-term hemodialysis catheters could prevent catheter-related bacteremia (CRB) and prolong catheter survival when compared with povidone–iodine solutions. There were 20,784 catheter days observed. Povidone–iodine solutions (Betadine®) were used in the first half of the study and ChloraPrep® was used in the second half for all the patients. Both groups received chlorhexidine-impregnated dressings at the exit sites. The use of Chloraprep® significantly decreased the incidence of CRB (1.0 vs 2.2/1,000 catheter days, respectively, P = 0.0415), and hospitalization due to CRB (1.8 days vs 4.1 days/1,000 catheter days, respectively, P = 0.0416). The incidence of exit site infection was similar for the two groups. Both the period of overall catheter survival (207.6 days vs 161.1 days, P = 0.0535) and that of infection-free catheter survival (122.0 days vs 106.9 days, P = 0.1100) tended to be longer for the catheters cleansed with ChloraPrep®, with no statistical significance. In conclusion, chlorhexidine-based solutions are more effective for the prevention of CRB than povidone–iodine solutions. This positive impact cannot be explained by decreased number of exit site infections. This study supports the notion that the catheter hub is the entry site for CRB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Catheter-related bacteremia (CRB) and catheter malfunction are the two common complications of tunneled-cuffed hemodialysis catheters (TCCs) [1, 2]. CRB strongly contributes to patient morbidity, death and loss of vascular access [3]. In our previous report, we found that CRB was the most important risk factor for shorter catheter survival [4]. The reported incidence of CRB varies from 1.1–4.2/1000 catheter days, with a mortality rate of 5% for the adult hemodialysis population [5–7]. For the cuffed catheters, the colonization of the intraluminal space through the catheter hub or following a bacteremia episode is accepted as the more likely pathogenesis of CRB (intraluminal hypothesis) [8]. For the temporary catheters, the entry of the pathogen to the catheter can be through the exit site and the tunnel around the catheter (extraluminal hypothesis) [9–11]. Among the well-known preventive measures for CRB are the use of strict hygiene measures during placement and maintenance of the catheters, the application of preventive antimicrobial ointments/solutions at the exit site, the eradication of a Staphylococcus aureus nasal/skin carrier state, the cleansing of catheter hubs with antimicrobial solutions, the use of antimicrobial-coated catheters, and the intraluminal application of antibiotic lock solutions (ABLs) [5, 11–16].
ChloraPrep® (Enturia, Inc., Leawood, KS, USA) is a local cleansing agent with a mixture of chlorhexidine gluconate 2% and isopropyl alcohol 70%. The use of chlorhexidine-based solutions for the care of catheter exit sites has successfully decreased the incidence of CRB for the non-cuffed temporary catheters [17–21]. Although the importance of meticulous catheter care is emphasized in several guideline papers, there are still unsettled debates about which antiseptic solution would be the best choice [22–24]. Povidone–iodine solutions (Betadine®, Bruce Medical Supply, Waltham, MA, USA), on the other hand, have historically been used as the standard of exit site and hub care for TCCs [25–27].
The aim of this study was to investigate if the application of chlorhexidine-based solutions (ChloraPrep®) to the exit site and the hub of tunneled-cuffed hemodialysis catheters would have any beneficial impact on the prevention of CRB and catheter survival times when compared with the use of povidone–iodine solutions. Since both treatment groups received chlorhexidine-impregnated dressings at the exit sites, and prophylaxis with tobramycin–tissue plasminogen activator (TPA) antibiotic locks was used for the population at high risk for CRB, the major differentiating intervention between the two groups was the catheter hub care. The tested hypothesis was that the catheter hubs are the major entry site for CRB-causing microorganisms for long-term catheters. With strict surveillance using a broad-spectrum antiseptic at the hub, CRB may be prevented more effectively. It was unclear whether this would translate into longer catheter survival times, since none of the previous studies had focused on catheter survival times. The study was designed as a retrospective chart review.
Patients and methods
This study was approved by the University of Miami, School of Medicine Institutional Review Board (IRB). A retrospective review was performed on the charts of 59 children on long-term hemodialysis in the pediatric dialysis unit at the University of Miami/Holtz Children’s Hospital, USA, from September 2004 to June 2006. All consecutive patients were included in the study. During this period, 51/59 (86%) children were using tunneled–cuffed catheters as vascular access, at least for some portion of the study. Standard tunneled–cuffed, silicone, double-lumen, hemodialysis catheters (Hemocath®; Medcomp, Harleysville, PA, USA) were used for vascular access and were placed percutaneously by the interventional radiologist or by the pediatric surgeon in children weighing fewer than 15 kg. Two pediatric surgeons and three interventional radiologists were involved in the placement and exchange of the catheters. The sizes and lengths of the catheters were based on the patient’s size and ranged from 8 French, 18 cm, to 14 French , 40 cm. The right internal jugular vein was used whenever possible.
Hemodialysis protocol and catheter care
Patients underwent dialysis three to four times per week, with hollow-fiber dialyzers appropriate for body size, on Cobe® (Gambro Inc., Lakewood, Colorado, USA) or Baxter® (Deerfield, Illinois, USA) hemodialysis machines. A standard bicarbonate bath was used as dialysate. Antibiotics, vitamin D analogs, erythropoietin, and iron supplements were infused towards the end of dialysis as needed, through the catheter. Hemodialysis catheters were handled only during dialysis, with no intervention between treatments. The exit site was cleaned with chlorhexidine-based solution or povidone–iodine solution, and a chlorhexidine-impregnated dressing was applied weekly. At the end of each hemodialysis session, each port of the catheter was filled with 5,000 units/ml of heparin solution, according to the volume of the ports. Patients with high-risk for recurrent CRB were treated with tobramycin–tissue plasminogen activator (5 mg/dl tobramycin, 2 mg/2 ml TPA) antibiotic lock solutions 1–3 times per week (definition F, see below). Catheter malfunction was diagnosed when goal blood flow rate could not be maintained or when urea reduction rate (URR) was less than 65%. Catheter malfunction was initially treated by the instillation of 2 mg/2 ml TPA into each lumen for 1–2 h.
Definitions
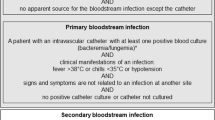
-
(A)
Catheter-related bacteremia (CRB) was defined as the occurrence of a positive blood culture from the catheter with or without a positive peripheral blood culture in a child with systemic symptoms (fever, chills, vomiting, hypotension) and no other source of infection identified. There were no surveillance blood cultures obtained from the catheters during the study period.
-
(B)
Exit site infection was defined as the presence of purulent discharge, swelling, erythema and tenderness at the exit site with or without a positive swab culture.
-
(C)
Polymicrobial CRB was defined as the documented growth of at least two or more microorganisms in the first or sequential blood cultures during the index CRB.
-
(D)
Infection-free survival of a catheter was defined as the period between the placement of the catheter and the first positive blood culture obtained from that catheter. All blood cultures were obtained when CRB was clinically suspected. Censored events were removal of that catheter for malfunction, obstruction, transfer to another facility, elective removal of the catheter [arteriovenous (AV) fistula, AV graft, kidney transplantation] or end of study with a functional non-infected catheter.
-
(E)
Overall survival of a catheter was defined as the period between the insertion of the catheter and its removal. Censored events were the same as the ones for infection-free survival.
-
(F)
High-risk for recurrent CRB was defined in children who had a previous history of more than ten episodes of CRB per 1,000 catheter days or life-threatening CRB with septic shock. In order to fulfill the criterion for high-risk, the new-onset hemodialysis children had to have experienced either two episodes of CRB in their first 200 catheter days or one episode of CRB with septic shock. Long-term hemodialysis patients were evaluated by their cumulative CRB history to qualify for high risk.
The povidone–iodine (Betadine®) era
During this era, all the patients in the unit had their exit sites cleansed with 10% povidone–iodine solution (Betadine®) at each hemodialysis session. The chlorhexidine-impregnated dressing (Biopatch®; Johnson&Johnson Medical Inc., Arlington, Tx, USA) was applied to the exit site once a week after cleansing with Betadine® and was then covered with a transparent dressing by the sterile technique. The exit site was not disturbed in-between hemodialysis treatments. The catheter hubs were immersed in 10% povidone–iodine soaked sterile gauze for 5 min prior to connection to the hemodialysis lines. Before all interventions, and at the end of the treatment sessions, the hubs were again cleansed with 10% povidone–iodine solution.
The chlorhexidine-based solution (Chloraprep®) era
In this era the exit sites were cleansed with chlorhexidine-based solution (chlorhexidine gluconate 2% and isopropyl alcohol 70%, ChloraPrep®). The chlorhexidine-impregnated dressing (Biopatch®) was applied to the exit site once a week after cleansing with chlorhexidine-based solution and was then covered with transparent dressing by the sterile technique. The exit site was not disturbed in-between hemodialysis treatments. The catheter hubs were cleansed with chlorhexidine-based solution for 1–3 min prior to connection to the hemodialysis lines. Before all interventions, and at the end of the treatment session, the hubs were again cleansed with chlorhexidine-based solution.
The diagnosis and management of CRB
Blood was obtained for culture from both ports of the catheter when children presented with fever, chills, hypotension or emesis during treatment. Peripheral blood was cultured whenever possible. All symptomatic children were examined for a clear source of infection, and, if none was found, they were presumed to have CRB. Urine for culture and chest X-rays were obtained whenever indicated. The initial empiric treatment was systemic levofloxacin and vancomycin along with tobramycin–TPA locks or tobramycin–heparin locks. The systemic antibiotics and the locks were tailored according to the sensitivities of the CRB. Symptomatic CRB after 48–72 h of protocol was treated by wire-guided exchange of catheter. Non-symptomatic CRB was treated for 2 weeks until two consecutive blood cultures 1 week apart showed no growth.
Outcome parameters
The primary end point was the occurrence of CRB. Secondary end points were infection-free catheter survival and overall catheter survival.
Data were obtained on serum albumin, ferritin and hemoglobin levels from the samples collected for monthly laboratory tests without underlying CRB for all children during the protocol period. Each patient’s age, gender, etiology of end-stage renal disease, cumulative catheter days when entering the protocol, previous CRB incidence and oral treatment with methylprednisolone (Medrol®) were also documented. Type of CRB/exit site infection (Gram-positive, Gram-negative or polymicrobial) and specific microorganisms causing infections were recorded.
Statistical methods
Mean, standard deviation (SD) and percentage values were used to summarize baseline characteristics and outcome data. All results were expressed as mean ± SD. P values of less than 0.05 were considered significant. Chi-square tests were used to compare proportions. Paired t test and Fischer exact test were used to compare outcomes in the two groups. Survival analysis for the catheter outcomes were performed with Kaplan–Meier curves. Graphpad® software (San Diego, CA, USA) was used to generate the survival curves. SAS 9.1 (SAS institute, Cary, NC, USA) was used for statistical analysis.
Results
There were 59 children on hemodialysis in our center during this study. Fifty-one (86%) of these children underwent hemodialysis using a long-term catheter for at least for part of the study period. Eight patients were using an arteriovenous graft/fistula as their vascular access throughout the study. There were 24 male patients (41%) and 35 female patients (59%). Their mean age was 13.4 ± 8.2 years (range 2–21 years). Their racial distribution was 31 African-American, 22 Hispanic and six Caucasian. The primary etiology for end-stage renal disease was obstructive nephropathy/renal dysplasia–hypoplasia/neurogenic bladder in 21 patients, chronic glomerulonephritis in 14 patients, lupus nephritis/vasculitis in 12 patients, human immunodeficiency virus (HIV) nephropathy in eight patients, and unknown/other in four patients.
Table 1 describes the patients’ comparative demographic characteristics during the Betadine® era and the ChloraPrep® era. There was no statistically significant difference when the two groups were compared for age, gender, primary etiology, the use of immunosuppressive agents, previous catheter days prior to the study or the previous CRB rates. Serum hemoglobin levels were higher in the ChloraPrep® group (10.6 g/dl vs 10.8 g/dl, P = 0.0281). The ChloraPrep® group also had significantly lower serum ferritin levels than the Betadine® group (509.9 mg/dl vs 664.4 mg/dl, P = 0.0034). Serum albumin concentrations were not statistically different between the two groups.
There were 116 catheters used in the study period. Ninety-six were in the right internal jugular, 18 in the left internal jugular, and two were in the right subclavian. Fourteen of the catheters were first time catheters for patients with newly diagnosed end-stage renal disease (six in the Betadine® era and eight in the Chloraprep® era).
This study involved a total of 20,784 catheter days. There were 34 episodes of CRB in 51 children. The overall incidence of CRB was 1.6/1,000 catheter days during this period. Sixteen were Gram-positive, 12 were Gram-negative and six were polymicrobial. Coagulase-negative Staphylococcus species were the most common Gram-positive isolates (38%). The most frequent Gram-negative isolate was Klebsiella pneumoniae (25%). There was no difference in the prevalence of Gram-positive, Gram-negative and polymicrobial CRB between the two groups. There was a statistically significant difference in the incidence of CRB between the Betadine® era and the ChloraPrep® era (2.2 vs 1.0/1,000 catheter days, P = 0.0415). Table 2 provides information on the distribution of CRB types.
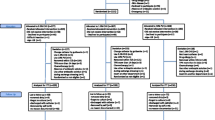
The most common reason for patients to lose their catheters was CRB (47/116; 41%). Thirteen catheters were replaced by wire-guided exchange in the first 48–72 h of the CRB (8/64 for the Betadine® and 5/52 for the Chloraprep® eras, P > 0.05). The mean overall period of catheter survival was longer for the Chloraprep® era, without reaching statistical significance (207.6 days for Chloraprep® vs 161.1 days for Betadine®; P = 0.0535). There was no difference in infection-free survival time between the two groups. The comparative infection-free and overall catheter survival times for the two eras are demonstrated by Kaplan–Meier survival analysis curves in Figs. 1 and 2, respectively. The two groups had very similar incidences of exit-site infections (ESI), but CRB rate was lower for the Chloraprep® group. The Chloraprep® group had fewer hospitalization days due to CRB than did the Betadine® group (1.8 days vs 4.1 days/1,000 catheter days; P = 0.0416). The incidence of catheter malfunction and breakdown requiring catheter exchange were similar for the two eras. Table 3 compares the two eras for the primary and secondary end-points of the study.
Kaplan–Meier curves for infection-free survival times of the catheters in the chlorhexidine-based (Chloraprep®) and povidone–iodine based (Betadine®) cleansing eras. The infection-free survival periods were not statistically different, even though the chlorhexidine group’s survival time tended to be longer than that of the Betadine® group (122.0 ± 54.3 days vs 106.9 ± 56.7 days, P = 0.1100 by the log-rank test)
Kaplan–Meier curves for the overall survival time of the catheters in the chlorhexidine-based (Chloraprep®) and povidone–iodine based (Betadine®) cleansing eras. The overall survival times of the catheters used in the Chloraprep® group were longer than those used in the Betadine® group, but it did not reach statistical significance (207.6 ± 136.0 days vs 161.1 ± 107.2 days, P = 0.0535 by the log-rank test)
There were no allergic reactions/contact dermatitis with either Betadine® or Chloraprep® application during this study period.
Discussion
To our knowledge, this retrospective study was the first to investigate the effect of catheter cleansing method on overall and infection-free catheter survival times for tunneled-cuffed hemodialysis catheters. Our study demonstrated that the application of ChloraPrep® significantly decreased the incidence of CRB in long-term catheter use. There was no difference in the distribution of the types of CRB. ChloraPrep® improved the overall survival period of the catheters, not reaching statistical significance. If there had been more catheters involved in this study and a longer observation period, statistical differences might have been observed for both overall and infection-free survival of the catheters. These positive effects cannot be explained by the use of ChloraPrep® at the exit site, since there was no difference in the incidence of exit site infection between the two groups.
The success of chlorhexidine-based solutions can be explained by some of its characteristics. It is a purely topical agent, with minimal to no absorption by the skin, and without any reported systemic toxic effects. After its initial application, the residual antimicrobial effect of chlorhexidine is longer than that of povidone–iodine [28]. Moreover, chlorhexidine gluconate is a cationic biguanide with a broad spectrum of antimicrobial activity. When it is combined with an alcohol solution, it is shown to be active against most of the pathogens that are known to be responsible for ESI and CRB in long-term catheter usage for hemodialysis patients [18–20, 29]. As a last point, different body solutions can deactivate povidone–iodine solutions, which has not been described in chlorhexidine [30, 31]. There have been very few reports for the resistance patterns for chlorhexidine gluconate [32].
The overall CRB rate in this study period was lower than that reported in the literature. It was also the lowest CRB rate reported from our institution. The beneficial effects of the use of prophylactic antibiotic locks for patients at high-risk for CRB, the treatment of all CRB episodes with appropriate systemic antibiotics and antibiotic lock solutions, the use of chlorhexidine-impregnated dressings at the exit site and the appropriate length of catheter hub care at every treatment all contributed to this decreased CRB rate. This made the task of reaching statistical significance between the two groups even harder. Therefore, if the use of chlorhexidine can decrease the CRB rate for a population with an already low CRB incidence, it potentially may have more significant impact in hemodialysis units with higher baseline CRB rates.
The overall and infection-free survival times of the catheters during this study period seemed shorter than those in our previous reports [2, 4]. The two major differences in the current periods were the aggressive use of prophylactic antibiotic locks and then the use of Chloraprep®. But surprisingly, the significant improvement in CRB incidence did not generate its expected impact on the catheter survival times. When we re-analyzed our data, one important factor was the increased number of catheters that were censored from the statistical analysis because their use had been terminated while they were functioning. More patients underwent kidney transplantation, more patients went through AV fistula surgeries, unfortunately with primary or secondary failures, and, lastly, many functioning catheters were censored because they had been functional at the end of the study. During the period reported here, there were also more children less than 10 years old. The advantage of a study that involves a longer observation period is that more catheters reach their natural endpoints, be it because of CRB, thrombosis or malfunction. In fact, when we analyzed all the catheter survival times within the study period without any censorship, we observed longer survival times in both groups and both eras. Furthermore, the difference in overall survival time was statistically significant, and the difference in infection-free survival was with a smaller P value. Therefore, we speculate that, with longer observation periods, not only would we observe longer survival periods but also we might be able to demonstrate the survival advantage of aggressive surveillance against CRB.
There are no clear data on whether the antimicrobial effect of chlorhexidine is more prominent in certain microorganisms/CRB types than in others. In this study there was a slight increase in the percentage of Gram-negative CRB during the ChloraPrep® era. It did not reach statistical significance, but, in larger numbers and with longer observation periods, this finding or similar other findings might reach statistical significance. An alternative explanation could be a more pronounced decrease in Gram-positive CRB. This was previously demonstrated in adult intensive care patients with uncuffed central venous catheters [20]. This selection characteristic of any antimicrobial/disinfectant would be an unwanted effect. This point is a very important one that needs to be investigated in a prospective trial.
This study, surprisingly, demonstrated improved serum hemoglobin levels and decreased serum ferritin levels during the ChloraPrep® era. We do not have the values for total iron infusion doses or the Epogen doses during the two periods to check if there is another explanation for this finding. However, that is unlikely, because, during the study time, both the approach to anemia and the methods of treating it were literally the same in the two eras. This improvement could also be an indirect sign of better controlled inflammation, which is now considered to be a hidden component of end-stage renal disease/chronic renal replacement therapy. The less frequent hospitalization during this era gives further support to the idea that the micro-inflammation might have been better controlled. One simple explanation for this impact may be less incidence of CRB.
There are several short-comings to our study. The retrospective nature and the overlapping patient populations are the two main limitations. There might have been unique and unaccounted for characteristics of either of the treatment periods that might have affected the outcomes, other than the cleansing methods used. Despite the fact that there was no study protocol, the daily practice in the hemodialysis unit was strictly followed by the nurses and the clinicians for each of the eras. Limited surveillance data from the monthly laboratory reports is another limitation of our study. If it were possible to assess the level of micro-inflammation by the conventional inflammatory markers, the effect of cleansing technique to control the inflammation could be assessed more precisely.
In conclusion, chlorhexidine-based solutions are more effective for the prevention of CRB than are povidone–iodine solutions. This positive impact cannot be explained by decreased number of exit site infections. The use of chlorhexidine as the hub cleanser has the potential to offer longer catheter survival times. Improved serum hemoglobin concentrations and ferritin levels may suggest better controlled inflammation. This study supports the hypothesis that the catheter hub is the more likely entry site in CRB during long-term catheter usage. Persistent and more effective surveillance at the catheter hub may offer decreased CRB rates and even longer catheter survival.
References
Hoen B, Paul-Dauphin A, Hestin D, Kessler M (1998) EPIBACDIAL: a multicenter prospective study of risk factors for bacteremia in chronic hemodialysis patients. J Am Soc Nephrol 9:869–876
Onder AM, Chandar J, Coakley S, Abitbol C, Montane B, Zilleruelo G (2006) Predictors and outcome of catheter-related bacteremia in children on chronic hemodialysis. Pediatr Nephrol 21:1452–1458
Powe NR, Jaar B, Furth SL, Hermann J, Briggs W (1999) Septicemia in dialysis patients: incidence, risk factors and prognosis. Kidney Int 55:1081–1090
Onder AM, Chandar J, Saint-Vil M, Lopez-Mitnik G, Abitbol C, Zilleruelo G (2007) Catheter survival and comparison of catheter exchange methods in children on hemodialysis. Pediatr Nephrol 22:1355–1361
Dogra GK, Herson H, Hutchison B, Irish AB, Heath CH, Golledge C, Luxton G, Moody H (2002) Prevention of tunneled hemodialysis catheter related infections using catheter-restricted filling with gentamicin and citrate: a randomized controlled study. J Am Soc Nephrol 13:2133–2139
Klevens RM, Tokars JI, Andrus M (2005) Electronic reporting of infections associated with hemodialysis. Nephrol News Issues 19:37–39
Weijmer MC, Van den Dorpel MA, Van de Ven PJ, Wee PM, van Geelen J, Groeneveld JO, van Jaarsveld BC, Koopmans MG, le Poole CY, Schrander-Van der Meer AM, Siegert CEH, Stas KJF, for the CITRATE Study Group (2005) Randomized, clinical trial comparison of trisodium citrate 30% and heparin as catheter-locking solution in hemodialysis patients. J Am Soc Nephrol 16:2769–2777
Cheesbrough JS, Finch RG, Burden RP (1986) A prospective study of the mechanisms of infection associated with hemodialysis catheters. J Infect Dis 154:579–589
Linares J, Sitges-Serra A, Garau J, Perez JL, Martin R (1985) Pathogenesis of catheter sepsis: a prospective study with quantitative and semiquantitative cultures of catheter hub and segments. J Clin Microbiol 21:357–360
Raad I, Costerton W, Sabharwal, Sacilowski M, Anaissie E, Bodey G (1993) Ultrastructural analysis of indwelling vascular catheters: a quantitative relationship between luminal colonization and duration of placement. J Infect Dis 168:400–407
Safdar N, Maki DG (2004) The pathogenesis of catheter-related bloodstream infection with noncuffed short-term central venous catheters. Intensive Care Med 30:62–67
Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, Sexton B, Hyzy R, Welsh R, Roth G, Bander J, Kepros J, Goeschel C (2006) An intervention to decrease catheter-related blood stream infections in the ICU. N Engl J Med 355:2725–2732
Sesso R, Barbosa D, Leme IL, Sader H, Canziani ME, Manfredi S, Draibe S, Pignatari AC (1998) Staphylococcus aureus prophylaxis in hemodialysis patients using central venous catheter: effect of mupirocin ointment. J Am Soc Nephrol 9:1085–1092
Lok CE, Stanley KE, Hux JE, Richardson R, Tobe SW, Conly J (2003) Hemodialysis infection prevention with Polysporin ointment. J Am Soc Nephrol 14:169–179
Segura M, Alvarez-Lerma F, Tellado JM, Jimenez-Ferreres J, Oms L, Rello J, Baro T, Sanchez R, Morera A, Mariscal D, Marrugat J, Sitges-Serra A (1996) A clinical trial on the prevention of catheter-related sepsis using a new hub model. Ann Surg 223:363–369
Luna J, Masdeu G, Perez M, Claramonte R, Forcadell I, Barrachina F, Panisello M (2000) Clinical trial evaluating a new hub device designate to prevent catheter-related sepsis. Eur J Clin Microbiol Infect Dis 19:655–662
Langgartner J, Linde HJ, Lehn N, Reng M, Scholmerich J, Gluck T (2004) Combined skin disinfection with chlorhexidine/propanol and aqueous povidone-iodine reduces bacterial colonization of central venous catheters. Intensive Care Med 30:1081–1088
Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA (2007) Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Arch Intern Med 167:2073–2079
Chaiyakunapruk N, Veenstra DL, Lipsky BA, Saint S (2002) Chlorhexidine compared with povidone-iodine solution for vascular catheter-site care: a meta-analysis. Ann Intern Med 136:792–801
Mimoz O, Villeminey S, Ragot S, Dahyot-Fizelier C, Laksiri L, Petitpas F, Debaene B (2007) Chlorhexidine-based antiseptic solution vs alcohol-based povidone-iodine for central venous catheter care. Arch Intern Med 167:2066–2072
Carson SM (2004) Chlorhexidine versus povidone-iodine for central venous catheter site care in children. J Pediatr Nurs 19:74–80
NKF K/DOQI Guidelines. Clinical Practice Guidelines for Vascular Access, 2006 Update. Available at https://doi.org/www.kidney.org
O’Grady NP, Alexander M, Dellinger EP, Gerberding JL, Heard SO, Maki DG, Masur H, McCormick RD, Mermel LA, Pearson ML, Raad II, Randolph A, Weinstein RA; Healthcare Infection Control Practices Advisory Committee (2002) Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control 30:476–489
Centers for Disease Control and Prevention (2001) Issues in healthcare settings: CDC’s 7 healthcare safety challenges. Atlanta, GA. US Department of Health and Human Services, Centers for Disease Control and Prevention. https://doi.org/www.cdc.gov/ncidod/dhqp/about_challenges.html. Accessed June 28, 2008
Levin A, Mason AJ, Jindal KK, Fong IW, Goldstein MB (1991) Prevention of hemodialysis subclavian vein catheter infections by topical povidone-iodine. Kidney Int 40:934–938
Kessler M, Hoen B, Mayeux D, Hestin D, Fontenaille C (1993) Bacteremia in patients on chronic hemodialysis. A multicenter prospective survey. Nephron 64:95–100
Krein SL, Hofer TP, Kowalski CP, Olmsted RN, Kauffman CA, Forman JH, Banaszak-Holl J, Saint S (2007) Use of central venous catheter-related bloodstream infection prevention practices by US hospitals. Mayo Clin Proc 82:672–678
Smylie HG, Logie JR, Smith G (1973) From Phisohex to Hibiscrub. Br Med J 4:586–589
Mimoz O, Pieroni L, Lawrence C (1996) Prospective, randomized trial of two antiseptic solutions for prevention of central venous or arterial catheter colonization and infection in intensive care unit patients. Crit Care Med 24:1818–1823
Zamora JL, Price MF, Chuang P, Gentry LO (1985) Inhibition of povidone-iodine’s bactericidal activity by common organic substances: an experimental study. Surgery 98:25–29
Lowbury EJ, Lilly HA (1974) The effect of blood on disinfection of surgeons’ hands. Br J Surg 61:19–21
Sticker DJ, Thomas B, Clayton CL (1985) Studies of the genetic basis of chlorhexidine resistance. Br J Clin Prac 25 (Suppl):23–30
Acknowledgments
This study is dedicated to the living memory of Mrs. Cherry Charlton, RN, whose singing voice will always be recalled in the Pediatric Hemodialysis Unit at the University of Miami/Holtz Children’s Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Onder, A.M., Chandar, J., Billings, A. et al. Chlorhexidine-based antiseptic solutions effectively reduce catheter-related bacteremia. Pediatr Nephrol 24, 1741–1747 (2009). https://doi.org/10.1007/s00467-009-1154-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-009-1154-5