Abstract
Objective
Short-term, noncuffed, percutaneously inserted central venous catheters (CVCs) are widely used and cause more than 250,000 bloodstream infections (BSIs) in hospitals each year in the United States. We report a prospective study undertaken to determine the pathogenesis of CVC-related BSI.
Design and setting
Prospective cohort study in a university hospital 24-bed medical-surgical intensive care unit.
Patients and participants
Patients participating in two randomized trials during 1998–2000—one studying the efficacy of a 1% chlorhexidine–75% alcohol solution for cutaneous antisepsis and the other a novel chlorhexidine-impregnated sponge dressing—formed the study population; CVC-related BSIs were considered to be extraluminally acquired if concordance was identified solely between isolates from catheter segments, skin, and blood cultures and intraluminally acquired if concordance was demonstrated only between hub or infusate and blood culture isolates, as confirmed by DNA subtyping of isolates from blood and catheter sites or infusate.
Results
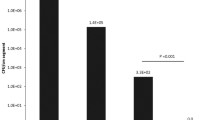
Of 1,263 catheters (6075 CVC days) prospectively studied, 35 (2.7%) caused BSI (5.9 per 1000 CVC days); 27 were caused by coagulase-negative staphylococci. Overall, 45% of infections were extraluminally acquired, 26% were intraluminally derived, and the mechanism of infection was indeterminate in 29%. In the pooled control groups of the two trials, 25 CVC-related BSIs occurred (7.0 per 1000 CVC days), of which 60% of infections were extraluminally acquired, 12% were intraluminally derived and 28% were indeterminate. In contrast, CVC-related BSIs in the treatment groups were most often intraluminally derived (60%, p=0.006).
Conclusions
Most catheter-related BSIs with short-term percutaneously inserted, noncuffed CVCs were extraluminally acquired and derived from the cutaneous microflora. Strategies achieving successful suppression of cutaneous colonization can substantially reduce the risk of catheter-related BSI with short-term CVCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reliable and safe vascular access is one of the most essential features of modern medical care. Unfortunately, the intravascular devices needed to establish stable access are associated with significant potential for producing iatrogenic disease, most often catheter-related bacteremia or candidemia [1, 2, 3]. More than 250,000 intravascular device-related bloodstream infections (BSIs) occur in the United States each year [1]; the majority are related to short-term noncuffed, percutaneously placed central venous catheters (CVCs). CVC-related BSIs are associated with 12–25% attributable mortality [4, 5, 6, 7], and prolongation of hospital stay [5, 6, 7, 8] and marginal cost to the health system of $33,000–35,000 per episode [5, 6, 8].
Understanding the pathogenesis of CVC-related BSIs is essential to devising strategies for prevention of these infections; however, few studies have determined the mechanism of CVC-related colonization and infection, particularly using molecular techniques to verify potential routes of infection [9, 10, 11, 12, 13, 14, 15]. We report a prospective study which employed molecular epidemiology to determine the pathogenesis of CVC-related BSI with short-term, noncuffed CVCs placed percutaneously in the internal jugular, subclavian, or femoral veins.
Patients
A total of 1,098 patients participating in two randomized trials during 1998–2000 [16, 17] formed the study population. One trial studied the effect of a 1% chlorhexidine–75% alcohol solution for cutaneous antisepsis for intravascular catheters [17], and the other evaluated the efficacy of a novel chlorhexidine-impregnated sponge dressing for prevention of catheter-related BSI [16]. The two trials were very similar in overall design and studied common patient populations (Table 1). The majority of patients studied were elderly and had one or more underlying diseases; the mean severity of illness score (Acute Physiology and Chronic Health Evaluation II) was 22. Most patients had a urinary catheter and were mechanically ventilated during the period in which they had a study CVC. Complete data were obtained for 1,263 CVCs, a total of 6,075 CVC days. Data were collected prospectively on study patients with newly inserted short-term, noncuffed and nontunneled central venous catheters, including demographic features, underlying diseases, Acute Physiology and Chronic Health Evaluation II [18], reason for placement of the catheter, service, antibiotic use, length of hospital stay, number of days the catheter remained in place, presence of other invasive devices (urinary catheters and endotracheal tubes), and all clinical and laboratory data pertaining to infection. Both studies were approved by the institutional review board, and written informed consent was obtained from all subjects prior to enrollment.
Microbiological methods
At the time of catheter removal, skin of the insertion site was cultured quantitatively, as previously described [19]. For each catheter two 5-cm segments, the intracutaneous segment and the tip, each transported in a sterile container, were cultured semiquantitatively; each hub and fluid aspirated aseptically from the most distal injection port of the line were also cultured quantitatively, as previously described [19]. Micro-organisms were identified according to standard criteria [20]. When catheter-associated BSI occurred, isolates recovered from the insertion site, catheter segments, infusate or hubs, and blood cultures that appeared similar phenotypically were subtyped by pulsed-field gel electrophoresis after digestion of genomic DNA with restriction endonucleases [21], using a computerized system and Centers for Disease Control criteria [22] for determining the relatedness of isolates (Gel Doc 2000, Bio-Rad Laboratories, Hercules, Calif., USA).
Definitions
Catheter-tip colonization was defined as a positive semiquantitative culture of an intravascular catheter segment (>15 colony-forming units) and is considered synonymous with local infection of the catheter [19]. Catheter-related BSI was defined as isolation of the same strain from the catheter segment, a hub, or infusate and from one or more blood cultures, as confirmed by restriction-fragment subtyping, with no other clearcut source for the BSI [19]. BSIs were considered to be extraluminally acquired if concordance was demonstrated solely between isolates from catheter segments, skin, and blood cultures and intraluminally acquired if concordance was demonstrated only between isolates from a hub or infusate and blood cultures; if the findings suggested that both routes or neither might be operative, the pathogenesis of infection was designated as indeterminate.
Statistical methods
The significance of differences between groups was calculated by χ2 or Fisher’s exact test. We considered two-tailed p values less than 0.05 as statistically significant.
Results
Of the 1263 CVCs 333 (26.3%) were colonized at removal and 35 (2.7%) caused CVC-related BSI, an incidence density of 5.9 per 1000 CVC days. BSIs were caused by coagulase- negative staphylococci (n=27), enterococci (n=4), enteric Gram-negative bacilli (n=3), or Candida (n=1; Table 2).
Recognizing that the database is comprised of patients who were participating in two randomized trials of novel strategies for prevention of CVC and arterial catheter-related BSI, and that both strategies were found to reduce the incidence of catheter colonization and CVC- and arterial catheter-related BSI [16, 17], the rate of CVC-related BSI was also calculated for the pooled data from the control groups [700 CVCs, 3,626 catheter days, 25 CVC-related BSI (3.6%), 7 per 1000 catheter days] and the treatment groups of the two trials [563 CVCs, 2,449 catheter-days, 10 CVC-related BSIs (1.7%), 4.0 per 1000 catheter days].
In the overall population studied 45% of CVC-related BSIs were extraluminally acquired, 26% appear to have had an intraluminal origin, and the mechanism of infection was indeterminate in 29% (Table 2). In a separate analysis of BSIs from the pooled data of the treatment and control groups (Table 3) it can be seen that the extraluminal route was most important (60%) for the catheters in the control groups, but with successful suppression of cutaneous colonization by the two strategies studied the CVC-related BSIs that occurred in the treatment groups were much more likely to be intraluminal (60%) or indeterminate (30%) in origin (p=0.006). A representative pulsed-field gel electrophoresis gel showing the pathogenesis of a CVC-related BSI is shown in Fig. 1.
The pathogenetic mechanisms were also analyzed according to the method of insertion: first catheter in a de novo site and second catheter inserted in an old site over a guidewire; there were no differences between the two groups (Table 4).
Discussion
There are two major sources of intravascular-device-related BSI: (a) colonization of the device, catheter-related infection, and (b) contamination of the fluid administered through the device, infusate-related infection [23]. Contaminated infusate is the cause of most epidemic intravascular device-related BSIs [1]. In contrast, catheter-related infections are responsible for most endemic device-related BSIs. In order for micro-organisms to cause catheter-related infection they must first gain access to the extraluminal or intraluminal surface of the device where they can adhere and become incorporated into a biofilm that allows sustained infection and hematogenous dissemination [11]. Micro-organisms gain access by one of three mechanisms: skin organisms invade the percutaneous tract, probably facilitated by capillary action [24], at the time of insertion or in the days following; micro-organisms contaminate the catheter hub (and lumen) when the catheter is inserted over a percutaneous guidewire or later manipulated [25]; or organisms are carried hematogenously to the implanted device from remote sources of local infection, such as a pneumonia [26, 27] (Fig. 2). With short-term devices (in place <10 days) [28]—peripheral IV catheters, arterial catheters and noncuffed, nontunneled CVCs—the limited studies that have been carried out suggest that most catheter-related BSIs are of cutaneous origin, from the insertion site, and gain access extraluminally, occasionally intraluminally [12, 29, 30]. For long-term devices (in place >10 days) [28]—cuffed and tunneled central venous catheters, subcutaneous ports or peripherally inserted central venous catheters—luminal colonization appears to be the major mechanism of device-related BSI [10, 13, 31, 32].
Potential sources of infection of a percutaneous intravascular device: extraluminally, from the contiguous skin flora; intraluminally, by contamination of the catheter hub and lumen or contamination of infusate; and hematogenously, from distant, unrelated sites of infection. (From [28])
In our large, prospective study of short-term, noncuffed CVCs used in patients in an ICU, the extraluminal route appears to have been the major (or a contributory) mechanism of infection of nearly two-thirds of CVC-related BSIs; however, in 26%, BSIs appeared to have derived from intraluminal contaminants, suggesting that both extra- and intraluminal routes are important with short-term noncuffed CVCs. Studies from Europe [15, 25, 33], where noncuffed, nontunneled CVCs are commonly left in place for longer than the 4–7 days representative of most centers in the United States (Table 1) [19, 34, 35], have found the intraluminal route to be more important, and we believe that the intraluminal route begins to predominate when a noncuffed and nontunneled catheter is left in place for much longer than 1–2 weeks.
Numerous studies performed in the United States have found heavy cutaneous colonization to be a powerful risk factor for CVC-related BSI [36, 37, 38, 39, 40]. Catheter insertion into the femoral vein [41] or internal jugular vein [42] rather than the subclavian vein also carries a higher risk of CVC-related BSI, probably because of heavier cutaneous colonization present at femoral or internal jugular insertion sites [43].
A number of measures have been found to be effective in prevention of CVC-related BSI. Foremost among these is education of personnel regarding catheter insertion technique and catheter care practices. Several large prospective studies have shown a 30–70% relative risk reduction with focused education programs [44, 45]. Tunneling a CVC also appears to reduce the risk of catheter-related BSI, both with catheters placed in the internal jugular or femoral veins [46, 47], and might be considered if circumstances favor cannulation of an internal jugular or femoral vein rather than a subclavian vein (e.g., severe coagulopathy or a hemodialysis catheter). Novel technologies which can reduce cutaneous colonization at the insertion site are most likely to be effective for preventing infection originating by the extraluminal route but can also provide benefit for intraluminally derived infections and have shown efficacy with short-term noncuffed CVCs, such as chlorhexidine for cutaneous antisepsis, chlorhexidine-impregnated sponge dressing, and anti-infective coated catheters [16, 17, 19, 48]. Our findings demonstrate, as presented in Table 3, that preventive strategies that effectively reduce cutaneous colonization markedly reduced the risk of CVC-related BSI with short-term noncuffed CVCs but shifted the pathogenesis of those CVC-related BSIs that still occur in treated patients to the intraluminal route.
In conclusion, in our study the majority of CVC-related BSIs with short-term noncuffed CVCs were extraluminally derived (45%), although 26% appeared to have had an intraluminal origin, and in 29% of catheters the mechanism of infection was indeterminate, suggesting that both routes may have been operative. The mechanism of infection with CVCs inserted in old sites over a guidewire did not differ materially from that seen with catheters inserted in de novo sites. This study points up the importance of a multifaceted approach for prevention of CVC-related BSI with short-term noncuffed CVCs: strategies designed to prevent extraluminally derived BSIs but also strategies to prevent infection that originates from intraluminal contaminants.
References
Maki DG, Mermel LA (1998) Infections due to infusion therapy. In: Bennet JV, Brachman PS, editors. Hospital Infections. Lippincott-Raven, Philadelphia, pp 689–724
Raad I (1998) Intravascular catheter-related infections. Lancet 351:893–898
Mermel LA (2000) Prevention of intravascular catheter-related infections. Ann Intern Med 132:391–402
Smith RL, Meixler SM, Simberkoff MS (1991) Excess mortality in critically ill patients with nosocomial bloodstream infections. Chest 100:164–167
Arnow PM, Quimosing EM, Beach M (1993) Consequences of intravascular catheter sepsis. Clin Infect Dis 16:778–784
Pittet D, Tarara D, Wenzel RP (1994) Nosocomial bloodstream infection in critically ill patients: excess length of stay, extra costs and attributable mortality. JAMA 271:1598–1601
Collignon PJ (1994) Intravascular catheter associated sepsis: a common problem. The Australian Study on Intravascular Catheter Associated Sepsis. Med J Aust 161:374–378
Rello J, Ochagavia A, Sabanes E, Roque M, Mariscal D, Reynaga E, Valles J (2000) Evaluation of outcome of intravenous catheter-related infections in critically ill patients. Am J Respir Crit Care Med 162:1027–1030
Maki DG (1988) Sources of infection with central venous catheters in an ICU: a prospective study. In: Program and abstracts of the 28th Interscience Conference on Antimicrobial Agents and Chemotherapy, Los Angeles
Raad I, Costerton W, Sabharwal U, Sacilowski M, Anaissie E, Bodey GP (1993) Ultrastructural analysis of indwelling vascular catheters: a quantitative relationship between luminal colonization and duration of placement. J Infect Dis 168:400–407
Marrie TJ, Costerton JW (1984) Scanning and transmission electron microscopy of in situ bacterial colonization of intravenous and intraarterial catheters. J Clin Microbiol 19:687–693
Cooper GL, Hopkins CC (1985) Rapid diagnosis of intravascular catheter-associated infection by direct Gram staining of catheter segments. N Engl J Med 312:1142–1147
Sitges-Serra A, Puig P, Linares J, Perez JL, Farrero N, Jaurrieta E, Garau J (1984) Hub colonization as the initial step in an outbreak of catheter-related sepsis due to coagulase negative staphylococci during parenteral nutrition. JPEN J Parenter Enteral Nutr 8:668–672
Sitges-Serra A, Linares J, Perez JL, Jaurrieta E, Lorente L (1985) A randomized trial on the effect of tubing changes on hub contamination and catheter sepsis during parenteral nutrition. JPEN J Parenter Enteral Nutr 9:322–325
Linares J, Sitges-Serra A, Garau J, Perez JL, Martin R (1985) Pathogenesis of catheter sepsis: a prospective study with quantitative and semiquantitative cultures of catheter hub and segments. J Clin Microbiol 21:357–360
Maki DG, Narans LL, Knasinski V, Kluger DM (2000) Prospective randomised, investigator-masked trial of a novel chlorhexidine-impregnated disk (Biopatch) on central venous and arterial catheters. In: Proceedings and Abstracts of the Fourth International Decennial Conference on Nosocomial and Healthcare-Associated Infections, Atlanta
Maki DG, Knasinski V, Narans LL, Gordon BJ (2001) A randomized trial of a novel 1% chlorhexidine-75% alcohol tincture versus 10% povidone-iodine for cutaneous disinfection with vascular catheters. In: Proceedings and Abstracts of the 31st Annual Society for Healthcare Epidemiology of America Meeting, Toronto
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Maki DG, Stolz SM, Wheeler S, Mermel LA (1997) Prevention of central venous catheter-related bloodstream infection by use of an antiseptic-impregnated catheter. A randomized, controlled trial. Ann Intern Med 127:257–266
Balows LE, Hausler W, Shadomy H (1991). Manual of clinical microbiology, 5th edn. American Society for Microbiology, Washington
Alvarado CJ, Stolz SM, Maki DG (1991) Nosocomial infection from contaminated endoscopes: a flawed automated endoscope washer. An investigation using molecular epidemiology. Am J Med 91 [Suppl 3B]:S725–S805
Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Persing DH, Swaminathan B (1995) Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 33:2233–2239
Maki DG, Goldman DA, Rhame FS (1973) Infection control in intravenous therapy. Ann Intern Med 79:867–887
Cooper GL, Schiller AL, Hopkins CC (1988) Possible role of capillary action in pathogenesis of experimental catheter-associated dermal tunnel infections. J Clin Microbiol 26:8–12
Sitges-Serra A, Linares J, Garau J (1985) Catheter sepsis: the clue is the hub. Surgery 97:355–357
Maki DG, Jarrett F, Sarafin HW (1977) A semiquantitative culture method for identification of catheter-related infection in the burn patient. J Surg Res 22:513–520
Maki DG, Hassemer CA (1981) Endemic rate of fluid contamination and related septicemia in arterial pressure monitoring. Am J Med 70:733–738
Crnich CJ, Maki DG (2002) The promise of novel technology for the prevention of intravascular device-related bloodstream infection. I. Pathogenesis and short-term devices. Clin Infect Dis 34:1232–1242
Mermel LA, McCormick RD, Springman SR, Maki DG (1991) The pathogenesis and epidemiology of catheter-related infection with pulmonary artery Swan-Ganz catheters: a prospective study utilizing molecular subtyping. Am J Med 91 [Suppl 3B]:1897–1205
Bjornson HS, Colley R, Bower RH, Duty VP, Schwartz-Fulton JT, Fischer JE (1982) Association between microorganism growth at the catheter insertion site and colonization of the catheter in patients receiving total parenteral nutrition. Surgery 92:720-72-7
Cheesbrough JS, Finch RG, Burden RP (1986) A prospective study of the mechanisms of infection associated with hemodialysis catheters. J Infect Dis 154:579–589
Maki DG (1998) A prospective study of the pathogenesis of PICC-related BSI. In: Proceedings and Abstracts of the 38th Interscience Conference of Antimicrobial Agents and Chemotherapy, San Diego
Mahieu LM, De Dooy JJ, Lenaerts AE, Leven MM, De Muynck AO (2001) Catheter manipulations and the risk of catheter-associated bloodstream infection in neonatal intensive care unit patients. J Hosp Infect 48:20–26
Maki DG, Ringer M, Alvarado CJ (1991) Prospective randomised trial of povidone-iodine, alcohol, and chlorhexidine for prevention of infection associated with central venous and arterial catheters. Lancet 338:339–343
Garland JS, Alex CP, Mueller CD, Otten D, Shivpuri C, Harris MC, Naples M, Pellegrini J, Buck RK, McAuliffe TL, Goldmann DA, Maki DG (2001) A randomized trial comparing povidone-iodine to a chlorhexidine gluconate-impregnated dressing for prevention of central venous catheter infections in neonates. Pediatrics 107:1431–1436
Safdar N, Kluger DM, Maki DG (2002) A review of risk factors for catheter-related bloodstream infection caused by percutaneously inserted, noncuffed central venous catheters: implications for preventive strategies. Medicine (Baltimore) 81:466–479
Moro ML, Vigano EF, Cozzi Lepri A (1994) Risk factors for central venous catheter-related infections in surgical and intensive care units. The Central Venous Catheter-Related Infections Study Group. Infect Control Hosp Epidemiol 15:253–264
Mahieu LM, De Muynck AO, Leven MM, De Dooy JJ, Goossens HJ, Van Reempts PJ (2001) Risk factors for central vascular catheter-associated bloodstream infections among patients in a neonatal intensive care unit. J Hosp Infect 48:108–116
Franceschi D, Gerding RL, Phillips G, Fratianne RB (1989) Risk factors associated with intravascular catheter infections in burned patients: a prospective, randomized study. J Trauma 29:811–816
Almirall J, Gonzalez J, Rello J, Campistol JM, Montoliu J, Puig de la Bellacasa J, Revert L, Gatell JM (1989) Infection of hemodialysis catheters: incidence and mechanisms. Am J Nephrol 9:454–459
Merrer J, De Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, Rigaud JP, Casciani D, Misset B, Bosquet C, Outin H, Brun-Buisson C, Nitenberg G (2001) Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA 286:700–707
Charalambous C, Swoboda SM, Dick J, Perl T, Lipsett PA (1998) Risk factors and clinical impact of central line infections in the surgical intensive care unit. Arch Surg 133:1241–1246
Maki DG (1990) Marked differences in skin colonization of insertion sites for central venous, arterial, and peripheral IV catheters: the major reason for differing risks of catheter-related infection? In: Programs and Abstracts of the Third International Conference on Nosocomial Infections, Atlanta
Eggimann P, Harbarth S, Constantin MN, Touveneau S, Chevrolet JC, Pittet D (2000) Impact of a prevention strategy targeted at vascular-access care on incidence of infections acquired in intensive care. Lancet 355:1864–1868
Sherertz RJ, Ely EW, Westbrook DM, Gledhill KS, Streed SA, Kiger B, Flynn L, Hayes S, Strong S, Cruz J, Bowton DL, Hulgan T, Haponik EF (2000) Education of physicians-in-training can decrease the risk for vascular catheter infection. Ann Intern Med 132:641–648
Timsit JF, Sebille V, Farkas JC, Misset B, Martin JB, Chevret S, Carlet J (1996) Effect of subcutaneous tunneling on internal jugular catheter-related sepsis in critically ill patients: a prospective randomized multicenter study. JAMA 276:1416–1420
Timsit JF, Bruneel F, Cheval C, Mamzer MF, Garrouste-Orgeas M, Wolff M, Misset B, Chevret S, Regnier B, Carlet J (1999) Use of tunneled femoral catheters to prevent catheter-related infection. A randomized, controlled trial. Ann Intern Med 130:729–735
Darouiche RO, Raad, II, Heard SO, Thornby JI, Wenker OC, Gabrielli A, Berg J, Khardori N, Hanna H, Hachem R, Harris RL, Mayhall G (1999) A comparison of two antimicrobial-impregnated central venous catheters. Catheter Study Group. N Engl J Med 340:1–348
Acknowledgements
This research was presented in part at the 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy, 2002 and the 13th Annual Meeting of the Society for Healthcare Epidemiology of America, 2003.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by an unrestricted gift for research from the Oscar Rennebohm Foundation of Madison, Wisconsin
Rights and permissions
About this article
Cite this article
Safdar, N., Maki, D.G. The pathogenesis of catheter-related bloodstream infection with noncuffed short-term central venous catheters. Intensive Care Med 30, 62–67 (2004). https://doi.org/10.1007/s00134-003-2045-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-2045-z